Abstract
Background: Physical activity plays an important role in the prevention and treatment of chronic musculoskeletal pain, but chronic pain may implicate a poor rehabilitation outcome. The concept of physical activity on prescription (PAP) is a therapeutic option for various diseases, but there is a lack of knowledge about how patients with chronic musculoskeletal pain experience receiving the prescription.
Objectives: The objective of this study was to describe the experiences of and thoughts about receiving a prescription for physical activity of people with chronic musculoskeletal pain.
Design: Interviews analysed using qualitative content analysis with an inductive approach.
Setting: Three primary healthcare centres in a mixed rural and suburban area in the vicinity of a large city in western Sweden.
Subjects: Fifteen individuals with chronic musculoskeletal pain.
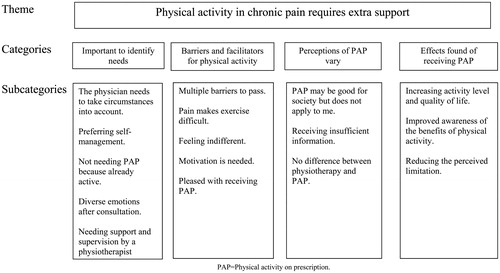
Results: Four categories were identified with the overarching theme “Physical activity in chronic pain requires extra support”. There were several barriers for increasing activity level and these patients suffered from the additional burden of pain. The categories were: “Important to identify needs”, “Barriers and facilitators for physical activity”, “Perceptions of PAP vary” and “Effects found of receiving PAP”.
Conclusions: Despite the many positive experiences of receiving PAP, patients described confusion about the role and execution of PAP. Chronic pain is an additional barrier for increasing activity level, and it is crucial to consider these patients’ circumstances. This study suggests that patients with chronic musculoskeletal pain have a greater need for information and extra support to overcome existing barriers, before or when physical activity is prescribed.
Physical activity is important for prevention and treatment of chronic pain and has earlier been shown to be increased by “physical activity on prescription”.
Patients with chronic musculoskeletal pain required the prescriber to listen and take the patients’ circumstances, context, symptoms and current activity level into account to a greater extent.
Patients with chronic musculoskeletal pain experienced more obstacles to increase their physical activity and, therefore, had a greater need for individually tailored information and support when prescribed physical activity.
Patients with chronic musculoskeletal pain found it difficult to distinguish between physical activity on prescription and physiotherapy and perceived that also the physicians could not tell the difference.
Key Points
Introduction
Musculoskeletal pain is one of the most common reasons to consult either a general practitioner (GP) or a physiotherapist in primary care [Citation1]. In Sweden and in Europe, about 20% of the population is estimated to have severe chronic pain [Citation2]. Chronic pain is often defined as pain lasting more than 12 weeks [Citation3] and has been associated with poorer self-rated health and mobility, depression and social isolation because it affects everyday life and undermines self-efficacy and autonomy [Citation4,Citation5].
Treatment of pain has changed over the past decades. Previously, it was commonly advised to rest, sometimes in combination with passive therapies [Citation6]. Today, the benefits of physical activity are well known and physical activity is emphasised both in prevention and in treatment of chronic pain [Citation7]. Physical activity is, according to the World Health Organization, defined as “any bodily movement produced by skeletal muscles that requires energy expenditure” [Citation8]. Physical activity affects pain in several ways, such as increasing body awareness, reducing secondary muscle tension due to pain, increasing mental and physical performance, and improving sleep quality, mood, and stress tolerance [Citation7]. Furthermore, physical activity can influence the experience of pain. It has been reported that 54% of patients with musculoskeletal pain feature a high degree of kinesiophobia [Citation9] and that the pain affects the level of motivation [Citation10].
Distraction can also change the experience of pain [Citation7,Citation11], and a Norwegian interview study indicated that patients continued to be physically active despite experiencing pain, because the pain signals were reinterpreted to signal activity limitation [Citation12].
The individual's beliefs about the onset and intensity of pain can affect adherence to treatment [Citation13]. Patients with musculoskeletal pain feel they are responsible for their health, but nevertheless expect individually tailored support from the social environment, including health care [Citation14]. It is, therefore, important to identify factors that may affect motivation for physical activity, such as perceptions and experiences of receiving physical activity on prescription (PAP) [Citation15].
Studies in healthy subjects show that the pain threshold is raised during and after physical activity, but for people with chronic pain, such as fibromyalgia, pain can be triggered at a very low level of activity, which may limit the beneficial effects [Citation7,Citation16]. Still, physical activity can yield positive side effects and people who suffer from chronic pain can endure more pain to achieve well-being and health [Citation17].
To exploit the known benefits of physical activity, the healthcare sector initiated PAP, originally in the United Kingdom [Citation18]. The concept was introduced in Sweden in 2001 by the National Institute of Public Health [Citation19] and is today used internationally as either a single intervention or as a complement to other interventions in treating various diseases [Citation18]. Considerable resources have been invested to develop the PAP concept, with the knowledge compilation “Physical activity in the prevention and treatment of disease” (FYSS) as a scientific basis [Citation7]. The key component of the concept, the prescription itself, is a written prescription (similar to a drug prescription), in which one or more physical activities are recommended to the patient, with individual specifications regarding dose and frequency. The concept may also include a consultation based on motivational interviewing. The method is primarily based on the transtheoretical behaviour change model, which describes progress through stages of change [Citation20]. National guidelines for disease prevention methods from Sweden’s National Board of Health and Welfare [Citation21] recommend that healthcare providers give advice and talk with patients about physical activity based on the recommendations of the guidelines. The advice should include individual specifications regarding dose, frequency, and specific follow-up of patients with inadequate physical activity levels [Citation21,Citation22]. Issuing a written prescription has been shown to be more effective in increasing physical activity levels than just giving verbal advice [Citation23].
Patients suffering from chronic pain are often physically inactive because of current symptoms and, therefore, lack motivation [Citation15]. Some may need additional support before they are prescribed physical activity [Citation24]. The prescription should be tailored to the individual's condition to achieve a change in motivational level and behaviour [Citation15]. To stimulate the prescription of physical activity, healthcare facilities in several Swedish counties may receive compensation for each PAP issued. The strategy in different counties varies depending on prescribers, patients and the resources available [Citation25]. Some prescribers refer patients to a training specialist (most often a physiotherapist) who is trained in motivational interviewing. This person may perform fitness tests and helps the patient to identify appropriate physical activities based on the patient’s physical ability and by using FYSS as a guideline for physical activity recommendations. Different forms of support and monitoring exist [Citation25], and in some counties with more scarce resources, PAP might be limited to just a written prescription.
Recommended activities for chronic pain should, according to FYSS, be regular, continuous, last for at least 30 min (which could be divided in 10-min intervals), and be of moderate intensity [Citation7]. The importance of avoiding prolonged sedentary behaviour is also emphasised, since evidence of detrimental effects of this also has become increasingly clear [Citation7,Citation23].
There is a lack of knowledge about how people who suffer from chronic musculoskeletal pain perceive receiving a prescription for physical activity and what their needs related to physical activity are. Most people experience barriers in various forms before an activity change. Suffering from pain is an additional obstacle. A better understanding of these issues is important to be able to tailor routines for prescribing physical activity more effectively. The aim of this study was to describe the experiences of and thoughts about receiving a prescription for physical activity of people with chronic musculoskeletal pain.
Methods
The study included 15 individuals with chronic musculoskeletal non-malignant pain of at least 3 months duration as defined by the International Association for the Study of Pain [Citation26], who had received a prescription for physical activity from their GP. The sample consisted of 12 women and three men with a mean age of 58.4 years (range 35–72). Informant characteristics are presented in .
Table 1 Characteristics of informants.
Data collection
Participants were recruited from three primary healthcare centres in a mixed rural and suburban area in the vicinity of a large city in western Sweden. With authorisation from the head of each clinic, the first author searched electronic medical charts for suitable participants. Criterion sampling was used, which means reviewing and studying all cases that meet the predetermined criteria [Citation27], in this case, all patients identified who had chronic musculoskeletal pain and who had received PAP from their GP during the previous year. In this study, PAP was prescribed by the GP who was supposed to conduct a first motivational interview and then refer the patient directly to an activity or, if deemed necessary to a physiotherapist for an extra motivational interview and follow-up after 3 months. However, the motivational interview was not carried through for all the participants, as this was left to the GP’s discretion. There was no planned contact with a physiotherapist but some patients were advised to contact a physiotherapist if in need of additional support.
There is often co-morbidity in these patients and the primary reason for prescribing PAP was not always the pain. A frequent reason for prescribing was metabolic syndrome. Regardless of reason for prescribing, the purpose of the study was to explore the patients’ thoughts about receiving PAP while having chronic pain.
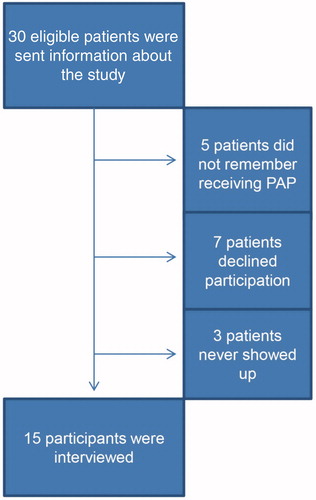
Patients with interpreter needs were excluded because project funds did not allow for compensation to the interpreter. Three to twelve months after the prescription had been issued, 30 patients, who had been identified in the electronic medical chart search, were sent a written invitation to participate in the study, information about the study's purpose, and that participation was voluntary. They were assured that no unauthorised persons would have access to the material and that their participation could be cancelled at any time [Citation28]. The first author then contacted them by telephone and asked if they were interested in participating, and if so scheduled the interview at a location chosen by the patient.
Fifteen of the 30 potentially eligible participants were excluded before the study started. Five of them did not remember receiving PAP, seven declined participation and three never showed up for their interview ().
Prior to the interview, the informants gave their written consent to participate and permission to be quoted from the interviews. All interviews were conducted by the first author. The interviews were semi-structured with open-ended questions and the main question was:
“You received a prescription for physical activity, what do you think about that?”
The informants were encouraged to speak freely in a narrative interview [Citation29,Citation30]. To clarify the individual’s story, additional probing questions were asked. Data on personal characteristics such as age, gender, occupation, and type of musculoskeletal pain were collected in order to describe the group. The interviews lasted for 35–40 min and were recorded and transcribed verbatim by the first author. Ethical approval was not required, according to a statement received by the Regional Ethical Review Board in Gothenburg prior to the study.
Analysis
A qualitative content analysis according to Graneheim and Lundman [Citation29] was performed. The purpose of the interview was to intercept the patient's thoughts and experiences when receiving the prescription for physical activity. Both the manifest and the underlying, latent, content were analysed [Citation29,Citation30]. An inductive approach was used and the unit of analysis was the transcribed text. Each interview was read several times and meaning units were identified – sentences or paragraphs containing information relevant to the aim. The meaning units were condensed, coded and categorised. The codes were sorted based on similarities and differences and organised in subcategories. These were sorted and abstracted into categories and an overall theme was formulated.
The analysis was led by the first author, who is a physiotherapist and previous project coordinator for implementation of PAP in the primary care areas where the participants were recruited. The second and third authors are physiotherapists and researchers with PhD degrees. All three authors have substantial experience from primary care physiotherapy. The first two interviews were coded independently by all three authors and differences were discussed to reach agreement and a common understanding of coding strategy. The remaining 13 interviews were coded by the first author. Content conformity of the categories was verified by the second author. Categories were discussed and revised in an iterative process among all authors. The computer software program NVivo 10 Software 2013 (QSR International Pty Ltd, Doncaster, Victoria, Australia) was used in the process of analysis to organise the data.
Results
Four categories were identified with the overarching theme “Physical activity in chronic pain requires extra support”. There were several barriers for increasing activity level and these patients suffered from the additional burden of the pain. The categories were “Important to identify needs”, “Barriers and facilitators for physical activity”, “Perceptions of PAP vary” and “Effects found of receiving PAP” ().
Figure 2. Theme, categories and subcategories of findings related to the experiences of and thoughts about receiving a prescription for physical activity of people with chronic musculoskeletal pain.
Important to identify needs
The physician needs to take circumstances into account
Various reasons for failing to change physical activity level were described. It was argued that physical activity had no effect at all on their symptoms. Others had realised that there were no other treatment options but they still felt that physical activity was boring, difficult or hard to fulfil. You know that you should, but have not started or even forgot. There were opinions about how and when physical activity should be prescribed. It was expressed that the prescriber should take into account their current health situation, present activities and interests, and previous experience of physical activity. The informants wanted the prescription to be more specific.
“No, it’s just that doctors should listen more to the patients and… and not tar everyone with the same brush1…like now when it comes to me… when we had discussed everything… about exercise and food and stuff like that, so she should have remembered” (IP 3).
Preferring self-management
The informants described that they want to get something concrete to take back home when they contact a physician for medical advice, but that PAP can be enough for well-motivated patients who do not have many or severe symptoms.
“So it’s clear that there are simple exercises that don’t require instruction from a physiotherapist. If the doctor thinks it’s so simple, I can do it myself, it's absolutely a lot easier and cheaper.” (IP 15).
Doing exercises in a gym, with more equipment and a personal trainer, was sometimes perceived as more fun.
Not needing PAP because already active
For those who were already active and had experienced positive effects, it seemed superfluous and unnecessary to receive a prescription. They thought that it was obvious and also expressed that it had been a habit since many years and explained why it is important. The informants appreciated that the physician was interested in them but perceived that it was probably due to a trend or campaign at the moment; that the physician was supposed to give each patient a prescription.
“So I thought that it was a bit unnecessary. Getting it on a piece of paper… Because I’m already quite aware of that message… that one should exercise.” (IP 13).
Diverse emotions after consultation
Within this subcategory there was disappointment about not being listened to, or that the treatment was not in line with what they believed in or needed, for example receiving PAP when they expected analgesics or when they were already very active. The informants used many words to describe the negative feelings that they had; degrading, sad, surprised, disappointed.
It was also perceived as a matter of participation in the decision making. The informants used expressions such as being the underdog, feeling run over and feeling mistrusted. They expressed that the healthcare professionals tried to persuade them but that it is important with own decisions.
“I would have understood if she had sent me to some weight unit, but not this exercise, because… I exercise five days a week. Three days I go to the gym, training strength, and two days, at least, I do spinning. Sometimes it can be on Saturday too, and then I walk the dog every day… maybe 5 km every day. Weekends too. So I didn’t like it because… anyway I'm early retired and I exercise as much as I can, I couldn't endure more. So therefore, I was pissed… (IP 3).
Needing support and supervision by physiotherapist
A need to feel secure was expressed, meaning that the informants wanted to exercise in the presence of a physiotherapist after an initial assessment. They said that the physiotherapist can set limits to prevent mistakes or excessive exercise. They felt more secure when joining a rehabilitation group with other patients with the same condition.
“PAP feels like a slap in the face and almost laughable if it’s not supported at all times” (IP 8).
Barriers and facilitators for physical activity
Multiple barriers to pass
Lack of time was the most common argument when motivation levels were low. The informants pointed out that weather, costs and temporary illness prevent regular physical activity and that it is important to find an activity that suits you. It was argued that PAP should mean subsidised exercise in the same way as for drugs, since poor personal finances were a major obstacle. The recommendation was exclusively gym exercise, despite common protests that this is boring or too expensive, but it is unclear whether this was the informants’ interpretation or the actual recommendation. Furthermore, the importance of self-image was mentioned, for example feeling awkward because of obesity, age or having low self-esteem when it comes to physical activity.
“We have so much going on right now and there is so much else occupying me so I have like no time. I haven’t had any time to think about exercise, but I hope when autumn comes and when everything has settled with the move, the traveling and vacation time and everything has passed on and we have settled at the new place, that I can get started…” (IP 4).
Pain makes exercise difficult
It was described that pain often contributed to inactivity and hampered regular exercise and the informants spoke of easily ending up in a vicious circle. Exercise was not regular because it depended on the shape of the day and exercising entailed a risk for overexertion and increased pain. The informants were not motivated to increase their activity level despite the recommendation and prescription; they did not believe that exercise would hurt but they did not want to risk increased pain. Instead they preferred to eliminate the pain before engaging in an activity and risking to aggravate the pain.
“I’m not forced to the same level of activity since I’m retired now and what prevents me is… I don’t want to be in pain then… I don’t want it to hurt…if I sit perfectly still like this so… I don’t exactly have any pain…” (IP 10).
Feeling indifferent
Some informants denied that physical activity could have an effect on their symptoms, which manifested itself in different ways: from expressing that they forgot, that it was not interesting, that it did not concern them, or that they simply did not believe in it. After having tried many different treatment options, they had low expectations and did not think that PAP would make any difference. Patients with poor experience from physical therapy ignored the prescription since they could not see the difference between PAP and physiotherapy.
“It was the doctor who did it. She was probably thinking that it would help. But… I don’t believe in it! …because I’ve been to physiotherapists before” (IP 7).
Motivation is needed
Getting over the threshold was considered as the main issue by the informants. However, it was described that even if you had experienced feeling better when you were more active, it was difficult to find motivation.
“…my reaction to physical activity on prescription was of course very positive, except that motivation might not always be there. I think not… the idea was great but…. to perform it in reality maybe not always worked” (IP 9).
Pleased with receiving PAP
The interviews revealed that the prescription could be a major contributing factor to initiate a change in activity level. The informants expressed that they had been waiting for a recommendation from a physician and were delighted to have received PAP rather than medication.
“Why haven’t I received it before? I have been in pain for many years.” (IP 1).
Perceptions of PAP vary
PAP may be good for society but does not apply to me
In this subcategory, the informants expressed that the concept of PAP is good for public health and that most people need it, but that it was not always applicable to themselves. Others felt that the prescription of physical activity is better than pharmacological treatment or other passive treatments, but it should be prescribed with care for the patient. It was expressed that PAP can help to get started or facilitate physical activity in everyday life. The need to be pushed was also expressed.
“I do think that it can be very good for many who haven’t thought that they might need this. It could be a kick…. And then… where else can you get it? …otherwise some are not doing it at all. Because I think for health, public health’s sake, it’s great.” (IP 14).
Receiving insufficient information
The informants expressed a need for more information about why they received PAP, what it was, or what to do about it. They tried, in vain, to search online. Someone had been referred to motivational interviewing, but not attended, while others remembered discussing the positive effects of increased physical activity with the physician but could not remember having received PAP.
“I tried to read a little online too about this physical activity of exercise… or on prescription and… it wasn’t so good. I thought it was hard to understand.” (IP 6).
No difference between physiotherapy and PAP
The interviews revealed that there was uncertainty about the distinction between physiotherapy and PAP, since the informants often received exercise programs by the physiotherapist. It was expressed that the physician also might have difficulties with this distinction.
“…he suggested that I should go to either rehab down here but there was nobody left then, or at any other place.” (IP 14)
Effects found of receiving PAP
Increasing activity level and quality of life
The increased activity level provided a sense of pride to have managed something the informants thought themselves incapable of, and an increased awareness of the positive effects that had created a virtuous cycle. They had discovered new forms of exercise and realised that they were capable of exercising, which sometimes had stimulated them to set new goals.
“I will continue as I do now, and my hope is, to later be able to increase resistance and even to have more time… to practice… and then… my goal is actually that I want to ride again as I did when I was young.” (IP 1).
Other benefits of increased activity level were described. Among these were reduced medication, increased energy (both physically and mentally), better quality of life and higher self-esteem when they saw themselves as in better shape than friends and colleagues.
“I think I have a better quality of life! I had a very severe depression during the autumn… And I’ve come outdoors, been able to stop taking medication, just taking my walks and exercise.” (IP 1).
Improved awareness of the benefits of physical activity
The informants had become more aware of their physical activity level and reported thinking more about taking the opportunity to exercise after receiving PAP. It was also expressed that it was good to be reminded because they had put off the idea of exercising.
“Thinking a lot that I should activate me after I had PAP.” (IP 10).
Reducing the perceived limitation
This subcategory contains the experience that the pain remained through exercising but that this did not need to cause concern. Knowing the cause of the pain and that exercise produces other positive effects made the informants feel secure and able to tolerate a slight increase in pain. They had also learned to distinguish between muscle soreness due to exercise and other pain, as well as to focus on other benefits, such as increased mental strength.
“I feel like I’m getting stronger and able to do more, as though…I've constant pain anyway, I feel that. But… you become stronger mentally too, I think… “(IP 1).
Discussion
Principal findings
The present study was a qualitative study of how patients with chronic musculoskeletal pain experienced receiving a prescription for physical activity. Semi-structured interviews were conducted with fifteen patients, recorded and analysed with qualitative content analysis. The results show different views on receiving PAP when suffering from chronic musculoskeletal pain and that it was often insufficient to just hand over a written prescription. Extra support and motivation may be needed and it was apparent that these patients had a great need for being actively listened to, understood and affirmed, implying the importance of the prescriber to seriously consider the patient's previous experience, present physical activity level, needs and individual circumstances. Furthermore, the study shows that the need for support varied. Informants who suffered from functional disability due to pain described being annoyed with receiving PAP without consideration of their situation. Others, who already exercised a lot, experienced that they were not being listened to. Some could do without extra support, while others needed professional supervision and guidance during training, and help with motivational measures and follow-up.
As suggested in the results, it may be important that PAP is prescribed by a physician. The fact that patients waited for a physician’s recommendation for physical activity although they already knew that this was important may imply that the prescription is better adhered to if written by a physician. This finding suggests that the physician still enjoys the highest authority and patients’ confidence to recommend and prescribe physical activity. Awareness of PAP and understanding of the meaning of PAP were limited and some informants were not aware that they had received a prescription, although they had discussed an increase in physical activity with the physician. Still, the prescription needs to be in writing, since this has been shown to increase physical activity levels more effectively [Citation24]. Confusion also existed regarding the difference between PAP and physiotherapy, and whether physiotherapy was part of the PAP concept.
According to the transtheoretical model, change takes place in stages that are not always visible to the environment [Citation20]. The probability of a change in behaviour and good treatment results is likely to increase if the patient takes an active role in decision-making and greater responsibility for their own process [Citation21]. Increased understanding of the benefits of physical activity also affects pain tolerance, functional capacity, self-reliance and commitment to change [Citation7].
The interviews took place 3–12 months after prescribing and it was expressed that even if the informants had not yet started with regular activity, they thought more about that they should. It can, therefore, be assumed that a change had occurred, in that they had moved from precontemplation to contemplation, or even to the preparation stage, according to the transtheoretical model [Citation20].
The PAP concept was considered important for the community and public health, but was not always perceived as applicable to the informants themselves. This might be interpreted as if these informants lacked motivation for physical activity, meaning that they remained in the precontemplation phase.
Strengths and weaknesses of the study
Trustworthiness of the study was achieved by addressing credibility, dependability and transferability of the findings. To meet the requirement of credibility and dependability, consensus about the analysis and the interpretation was continuously strived for and reached among the co-authors. Direct quotes from the interviews are presented, further strengthening credibility of our findings. To facilitate transferability, the selection and characteristics of participants, data collection, and process of analysis are described in both text and in .
The interviewer was not known to the informants prior to the study. However, because she introduced herself as a researcher and, when asked, as a physiotherapist, there is a risk of social desirability bias. A further consideration is her prior knowledge and experience both in the capacity of physiotherapist and of former project coordinator implementing PAP in the area, which likely influenced the formulation of the research question, data collection and interpretation of the data.
The distribution of gender and age in our sample was uneven. More women than men participated in the study, and most participants were more than 50 years of age. However, a similar distribution is also seen in the prevalence of chronic pain in Sweden, in which women and older age groups are over-represented [Citation31].
The study was set in a mixed rural and urban area in the vicinity of a large city. Some participants live in proximity to the city with ample opportunities for organised exercise, while others live in more rural areas, which offer various opportunities for physical activity.
In the area studied, as in several other counties in Sweden, the prescribing unit received financial compensation for each physical activity prescription during the present study. This was intended both as a strategy to restrict the increasing level of pharmaceutical prescriptions and instead focus more on preventive measures such as physical activity, and also to make a contribution to public health. The financial compensation is likely to affect the prescribing patterns, since it may mean that PAP is prescribed to receive the reimbursement without identifying the patient’s motivational level and present activity level so that the prescription can be adapted to the individual. This may in turn have caused the feeling of not having been listened to.
Findings in relation to other studies
The main finding of the study is the need for greater consideration of the patient's context and individual circumstances. This is consistent with previous findings that the need for support is significant when one suffers from chronic pain [Citation7]. Furthermore, needs for information about the PAP concept and about the effects of physical activity, for assistance to increase motivation, for help to find a suitable activity and for continual guidance, were pronounced. Group exercise, often with supervision, was a recurring request. This need is supported by a previous study by Larsson et al [Citation14], where patients with musculoskeletal disorders expressed the need for individually tailored support from the social environment, including health care.
The present study reveals that patients with chronic musculoskeletal pain do not always feel that they receive sufficient support to enable an activity change. According to a study by Bohman et al. [Citation32], in which nurses were interviewed, the PAP concept was perceived as a complex intervention because of lack of experience, knowledge, clear local standards or general guidelines, and insufficient time. Lack of time and routines applies also to the follow-up [Citation33]. Persson et al. [Citation34] reported that physicians believe that motivational interviewing is an art and that they lack sufficient training in giving lifestyle advice. They believe that it is not their responsibility. Discussing patients’ lifestyle may be perceived as challenging by GPs, particularly if the patients themselves consider their lifestyle unproblematic [Citation35]. Nevertheless, a health promotion dialogue can empower the patient but it is important to be sensitive to the patient’s needs and make sure that the dialogue is not perceived as intrusive. Still, as mentioned previously, it was perceived as important that a physician prescribes the activity and it has been suggested that a multidisciplinary approach is necessary and gives the best long-term effect on behavioural change in patients with chronic pain [Citation7,Citation36,Citation37]. It may also be relevant to apply a salutogenic approach when discussing physical activity and other lifestyle changes, as suggested by Miettola and Viljanen [Citation38]. They found that individuals with poorer health awareness are in particular need for professional support in lifestyle changes, while those who perceive practical constraints in their everyday life need more social support and those with a strong sense of coherence may only need encouragement to maintain a healthy lifestyle.
We support that the prescribing GP initiates PAP to supplement or replace pharmacological treatment for patients who are not limited by musculoskeletal pain. However, when it comes to people with more obstacles, such as chronic pain, it seems that PAP is not sufficient and instead a more comprehensive effort is needed. Specialists in physical activity, such as physiotherapists, might contribute with their competence about physical activity and exercise, in preventing impairments and activity limitations, and in providing treatment to restore body functions that are essential for movement. Physiotherapy management also includes continual follow-up [Citation36]. It may be that those patients who need and desire additional support might benefit more from physiotherapy than from PAP.
Meaning of the study
The PAP concept is useful in primary, secondary and tertiary prevention, promoting physical activity that ranges from regular walks to strenuous exercise [Citation7]. The journey from inactivity to regular physical activity is a time consuming process for both the individual and the supporting public and social environment. To guide patients to increase physical activity requires time, while health care strives for efficiency. Clarified and changed routines may also be required if the target is to be achieved. There is also a need for better infrastructure in the community for increased opportunities to choose activity rather than a sedentary lifestyle.
Further research is needed to determine if other patient populations have similar needs and which strategies are most effective and sustainable individually. Boundaries between social and personal responsibility should also be better defined, probably through political decisions.
Acknowledgements
The authors thank the study participants for generously giving of their time and sharing their experiences.
Disclosure statement
The authors are not aware of any conflicts of interest.
Note
Additional information
Funding
Notes
1 To “tar everyone with the same brush” is the English translation of a Swedish expression. It means to treat everyone in the same way.
References
- Jordan KP, Kadam UT, Hayward R, et al. Annual consultation prevalence of regional musculoskeletal problems in primary care: an observational study. BMC Musculoskelet Disord. 2010;11:144.
- Gerdle B, Ghafouri B, Ernberg M, et al. Chronic musculoskeletal pain: review of mechanisms and biochemical biomarkers as assessed by the microdialysis technique. J Pain Res. 2014;7:313–326.
- National Institutes of Health and the Friends of the National Library of Medicine. Chronic Pain: Symptoms, Diagnosis, & Treatment [Internet]. NIH Medline Plus 2011 [cited 2016 Nov 3]. Available from: https://www.nlm.nih.gov/medlineplus/magazine/issues/spring11/articles/spring11pg5-6.html.
- Dysvik E, Lindstrom TC, Eikeland OJ, et al. Health-related quality of life and pain beliefs among people suffering from chronic pain. Pain Manag Nurs. 2004;5:66–74.
- Rapo-Pylkko S, Haanpaa M, Liira H. Chronic pain among community-dwelling elderly: a population-based clinical study. Scand J Prim Health Care. 2016;34:159–164.
- Statens beredning för medicinsk utvärdering. Rehabilitering vid långvarig smärta: en systematisk litteraturöversikt, partiell uppdatering och fördjupning av SBU-rapport nr. 177/1 + 2 [Rehabilitation of chronic pain: a systematic literature review, partial update and elaboration of SBU report no. 177/1 + 2]. Stockholm: Statens beredning för medicinsk utvärdering (SBU) [Swedish agency for health technology assessment]; 2010.
- Professional Associations for Physical Activity/Swedish National Institute of Public Health. Physical activity in the prevention and treatment of disease (FYSS). Stockholm: Swedish National Institute of Public Health; 2015 [cited 2016 Nov 3]. Available from: http://www.fyss.se/fyss-in-english/
- World Health Organization (WHO). Global strategy on diet, physical activity and health. Geneva: World Health Organization; 2015 [cited 2016 Nov 3]. Available from: http:www.who.int/dietphysicalactivity/pa/en/
- Lundberg M, Larsson M, Ostlund H, et al. Kinesiophobia among patients with musculoskeletal pain in primary healthcare. J Rehabil Med. 2006;38:37–43.
- Wittink H. Physical therapy treatment. In: Michel T, Wittink H, editors. Chronic pain management for physical therapists. Boston: Butterworth-Heinemann; 1997.
- Miron D, Duncan GH, Bushnell MC. Effects of attention on the intensity and unpleasantness of thermal pain. Pain 1989;39:345–352.
- Damsgard E, Dewar A, Roe C, et al. Staying active despite pain: pain beliefs and experiences with activity-related pain in patients with chronic musculoskeletal pain. Scand J Caring Sci. 2011;25:108–116.
- Turner JA, Jensen MP, Romano JM. Do beliefs, coping, and catastrophizing independently predict functioning in patients with chronic pain? Pain 2000;85:115–125.
- Larsson ME, Nordholm LA, Ohrn I. Patients' views on responsibility for the management of musculoskeletal disorders – a qualitative study. BMC Musculoskelet Disord. 2009;10:103.
- Biddle S, Mutrie N, Gorely T. Psychology of physical activity: determinants, well-being and interventions. 3rd ed. Routledge: Abingdon, Oxon; 2015.
- O'Connor PJ, Cook DB. Exercise and pain: the neurobiology, measurement, and laboratory study of pain in relation to exercise in humans. Exerc Sport Sci Rev. 1999;27:119–166.
- Mannerkorpi K, Rivano-Fischer M, Ericsson A, et al. Experience of physical activity in patients with fibromyalgia and chronic widespread pain. Disabil Rehabil. 2008;30:213–221.
- Sallis R. Exercise is medicine: a call to action for physicians to assess and prescribe exercise. Phys Sportsmed. 2015;43:22–26.
- Leijon ME, Bendtsen P, Stahle A, et al. Factors associated with patients self-reported adherence to prescribed physical activity in routine primary health care. BMC Fam Pract. 2010;11:38.
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. J Consult Clin Psychol. 1983;51:390–395.
- The National Board of Health and Welfare. National guidelines for methods of preventing disease – English summary. The National Board of Health and Welfare (Socialstyrelsen); 2015 [cited 2016 Nov 3]. Available from: http://www.socialstyrelsen.se/nationalguidelines/nationalguidelinesformethodsofpreventingdisease
- Jansen MJ, Hendriks EJ, Oostendorp RA, et al. Quality indicators indicate good adherence to the clinical practice guideline on “Osteoarthritis of the hip and knee" and few prognostic factors influence outcome indicators: a prospective cohort study”. Eur J Phys Rehabil Med. 2010;46:337–345.
- Statens beredning för medicinsk utvärdering. Methods of promoting physical activity: a systematic review (English summary). Stockholm: Statens beredning för medicinsk utvärdering (SBU) [Swedish agency for health technology assessment]; 2007 [cited 2016 Nov 3]. SBU report No. 181. Available from: http://www.sbu.se/globalassets/publikationer/content1/1/fysisk_sam_eng.pdf
- Leijon ME, Faskunger J, Bendtsen P, et al. Who is not adhering to physical activity referrals, and why? Scand J Prim Health Care. 2011;29:234–240.
- Kallings LV. Fysisk aktivitet på recept – en underutnyttjad resurs. Stora variationer mellan landstingen, visar statistik över förskrivningen [Physical activity on prescription – an underutilized resource. Statistics on prescription shows large variations between counties]. Läkartidningen 2012;109:2348–2350.
- Turk DC, Rudy TE. IASP taxonomy of chronic pain syndromes: preliminary assessment of reliability. Pain 1987;30:177–189.
- Patton M. Qualitative research and evaluation methods. 3rd ed. Thousand Oaks (CA): Sage; 2002.
- World Medical Association. Recommendations guiding medical doctors in biomedical research involving human subjects. Declaration of Helsinki. Helsinki: World Medical Association; 1975.
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24:105–112.
- Granskär M, Höglund-Nielsen B. Tillämpad kvalitativ forskning inom hälso- och sjukvård [Applied qualitative research in health care]. Lund: Studentlitteratur AB; 2012.
- Gerdle B, Bjork J, Coster L, et al. Prevalence of widespread pain and associations with work status: a population study. BMC Musculoskelet Disord. 2008;9:102.
- Bohman DM, Mattsson L, Borglin G. Primary healthcare nurses' experiences of physical activity referrals: an interview study. Prim Health Care Res Dev. 2015;16:270–280.
- Kallings LV. Physical activity on prescription: studies on physical activity level, adherence and cardiovascular risk factors [dissertation]. Stockholm: Karolinska Institutet; 2008.
- Persson G, Brorsson A, Ekvall Hansson E, et al. Physical activity on prescription (PAP) from the general practitioner's perspective – a qualitative study. BMC Fam Pract. 2013;14:128.
- Guassora AD, Nielsen SB, Reventlow S. Deciding if lifestyle is a problem: GP risk assessments or patient evaluations? A conversation analytic study of preventive consultations in general practice. Scand J Prim Health Care. 2015;33:191–198.
- Verhagen E, Engbers L. The physical therapist's role in physical activity promotion. Br J Sports Med. 2009;43:99–101.
- Tulloch H, Fortier M, Hogg W. Physical activity counseling in primary care: who has and who should be counseling? Patient Educ Couns. 2006;64:6–20.
- Miettola J, Viljanen AM. A salutogenic approach to prevention of metabolic syndrome: a mixed methods population study. Scand J Prim Health Care. 2014;32:217–225.