Background
Highly conformal treatment plan using volumetric arc therapy (VMAT) and daily image guidance (IGRT) is standard of care in radiotherapy for prostate cancer. However, there are still risks of severe side effects from radiation dose to the rectum. The largest concerns are risk of diarrhoea, rectal strictures and rectal bleeding [Citation1,Citation2], which cause significant impact on patients’ quality of life [Citation3,Citation4]. We follow local guidelines specifying dose constraints to the rectal lumen (V78Gy<1 cm3, V70Gy<20%). These are based on clinical trials and QUANTEC publications [Citation5]. Since the rectum is a hollow organ, dose to the rectal wall is of special concern [Citation6,Citation7]. A number of studies [Citation7,Citation8] have focused on dose to the anterior part of the rectal wall, which often overlaps with planning target volumes. The dose to this sub-volume of the rectum is already controlled in our clinic using local standard optimization. A recent study has shown that the dose to the posterior part of the rectal wall is also of concern [Citation9]. Therefore, our institution has added an extra dose constraint: ‘Not more than 2/3 of the rectal circumference should be covered by the 50 Gy isodose’. The aim of this work was to establish a systematic optimization procedure that reduces the dose to the posterior part of the rectal wall.
Materials and methods
Curative patients with prostate cancer are planned with 78 Gy in 39 fractions to the planning target volume (PTV): PTV-T, consisting of a margin (5 mm LR/AP, 7 mm CC) surrounding the clinical target volumes, i.e., the seminal vesicles (CTVsemves) and the prostate (CTVprostate). There are dose constraints to the PTV-T and to the two sub-PTVs (PTV-semves and PTV-prostate). The treatment is carried out with PTV-T receiving a simultaneous integrated boost while the elective lymph nodes (PTV-E) are planned to 56 Gy in 39 fractions (50 Gy EQD2).
In this retrospective study we have analysed the difference in the coverage of the PTVs as well as the effect of dose to the rectum and rectal wall when planning without (original) or with (re-optimized) an automatically generated optimization structure covering the posterior rectal wall (RW-post). We have re-planned 8 patients with this new optimization technique.
The patients were treated on Varian accelerators (either TrueBeam or Clinac iX) and the plans were made in Eclipse version 16.1 (Varian Medical Systems, Palo Alto, California, USA). The Photon Optimizer algorithm (v. 16.1) was used for optimization and the Anisotropic Analytical Algorithm (v. 16.1) for dose calculation.
The patients are scanned and treated without a spacer (e.g., gel) between rectum and the prostate. The patients are instructed in the use of rectally administered lactavia to keep a comparable rectal filling during treatments.
Optimization strategy
We defined RW-post as an optimization structure to be used in addition to our usual optimization routine. This structure was defined as the rectal wall (3 mm inner margin of the rectum) subtracted from the total PTV with a 5 mm margin. This is consistent with general practice in our clinic, where we use organ-at-risk (OAR) optimization structures that are cropped from the total PTV (PTV-T + PTV-E) with a 5 mm margin. We further defined the intersection between the PTV-T and the bladder and rectum, respectively, to minimize high dose to these organs as dictated by our standard optimization procedure. These overlap structures were optimized to receive a slightly lower minimum dose than the rest of the PTV-T. Finally, we defined a ‘PTV-OAR’ structure (PTV-T minus all OAR) that we optimized towards the full prescribed dose of 78 Gy.
After the first optimization, we balanced the plan to protect the OARs while keeping the desired coverage of all PTVs: V95%≥ 98%. In a third optimization we aimed at removing other imperfections from the plan (e.g., dose spillage, hot spots, or lack of coverage). Our local constraints for coverage and dose to the rectum can be seen in .
Table 1. Local constraints.
When planning without the RW-post, the coverage goal for the PTV-T and each of the sub-volumes was V95%≥99%. With the new method we aim at 98% coverage to the PTV-semves, as we have observed that slightly decreased coverage in this area can substantially lower dose to the rectal wall for most patients. This coverage is within our local constraints ().
Plans were compared based on dose volume histograms (DVH) metrics for targets and rectum/rectal wall (). Further, an experienced radiation oncologist performed blinded comparisons of the two plans for each patient and selected the preferable plan based on dosimetry and patient characteristics. Due to the limited number of patients, no further statistical methods were employed for comparison.
Results
The DVH for especially RW-post showed a notable difference, resulting in a lower mean dose to the RW-post and the rectum. DVHs for one of the patients are shown in . Data for all patients are listed in .
Figure 1. DVHs for patient number 1. The original plan is shown in triangles and the re-optimized plan using RW-post as squares. Brown: rectum, magenta: RW-post, light blue: PTVs, orange: CTVs (CTV-E/56 Gy, CTV-T/78 Gy).
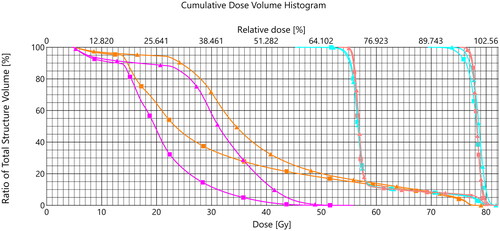
Table 2. Dose statistics and plan selection for the 8 patients in the study.
Only one plan could not be improved in terms of dose to the rectal wall using the new method. In three plans the oncologist preferred higher level of dose coverage to the PTV-semves (V95% ≥99%) due to the position of the tumour and therefore chose the original plan.
The largest reduction in V50Gy was −7,7% and the patient that had the best original plan had an increase of 6,6%. The mean dose to the rectum was lowered by maximum −8,0 Gy and for the patient that could not have an improved plan the mean dose changed with 3,3 Gy. Dose to the remaining OARs, especially bladder and intestine, did not change due to the new optimization method. There may be a small increase in dose to volumes that are not outlined (for example the os pubis).
The coverage of PTV-T changed less than 1% point for six of eight patients; only one patient (patient 2) approached the lower dose constraint. Patients 2 and 3 were the only two patients where the coverage of PTV-semves differed more than 1% point between the two plans (). Patient 3 showed one of the largest reductions in dose to the rectum and the oncologist preferred the re-optimized plan, whereas patient number 2 showed a minor reduction in dose to the rectum and the oncologist preferred the original plan.
Discussion
As shown in this letter, the dose to the rectum and the dose to the posterior rectal wall were consistently lowered when using the optimization structure RW-post at the cost of only small, often clinically acceptable, coverage decrease. The planning procedure described in this letter is easily implemented in daily clinical work routines and smoothens the workflow.
Using the additional optimization structure has also proved effective in the planning process on the adaptive Ethos platform (Varian Medical Systems). In the Ethos setting, the new workflow can be fully automated, as the RW-post structure is derived from existing delineations and manual delineation of isodose lines overlapping the rectum (as often used in manual optimization) are not necessary.
In connection with another project in our clinic, four additional patients have been re-planned after introducing this procedure and the data from these patients align well with the data shown in this study.
The procedure is being evaluated by expanding the RW-post structure by 7 mm laterally. This ensures that the 50 Gy isodose curve will not affect the rectal wall even though the rectum might be larger in some treatment sessions than in the planning CT.
Whether the oncologist preferred plans with very high (≥99%) or sufficient (≥98%) coverage of the PTV-semves depended on individual patient anatomy and location of primary disease. Our study shows a clear potential for sparing of the posterior rectal wall in patients whose disease location allows for a small decrease in dose to the seminal vesicles. These patients are identified using existing models for probability of seminal vesicle involvement defined by clinical factors.
It has been shown before [Citation10–12] that, in addition to being an efficient optimization structure, the rectal wall also serves as a clinical predictor for risk of side effects to the rectum. Thus, constraints for the rectal wall should be implemented instead of, or in addition to, constraints for the rectal lumen.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The authors confirm that the data supporting the findings of this study are available within the article ().
References
- krol R, McColl GM, Hopman WPM, et al. Anal and rectal function after intensity-modulated prostate radiotherapy with endorectal balloon. Radiother Oncol. 2018;128(2):364–368. doi:10.1016/j.radonc.2018.03.032.
- onjukka E, Fiorino C, Cicchetti A, et al. Patterns in ano-rectal dose maps and the risk of late toxicity after prostate IMRT. Acta Oncol. 2019;58(12) :1757–1764. doi:10.1080/0284186X.2019.1635267.
- petersen SE, Bentzen L, Emmertsen KJ, et al. Development and validation of a scoring system for late anorectal side-effects in patients treated with radiotherapy for prostate cancer. Radiother Oncol. 2014;111(1):94–99. doi:10.1016/j.radonc.2014.01.023.
- nguyen PL, Chen RC, Hoffman KE, et al. Rectal dose–volume histogram parameters are associated with Long-Term Patient-Reported gastrointestinal quality of life after conventional and High-Dose radiation for prostate cancer: a subgroup analysis of a randomized trial. Int J Radiat Oncol Biol Phys. 2010;78(4):1081–1085. doi:10.1016/j.ijrobp.2009.09.015.
- michalski JM, Gay H, Jackson A, et al. Radiation Dose-Volume effects in Radiation-Induced rectal injury. Int J Radiat Oncol Biol Phys. 2010;76(3 Supplement 1):123–129.
- ICRU Report 83: prescribing, recording and reporting intensity-modulated photon beam therapy (IMRT), 2010
- peterson JL, Buskirk SJ, Heckman MG, et al. Image-guided intensity-modulated radiotherapy for prostate cancer: dose constraints for the anterior rectal wall to minimize rectal toxicity. Med Dosim. 2014;39(1):12–17. doi:10.1016/j.meddos.2013.08.007.
- zelefsky MJ, Levin EJ, Hunt M, et al. Incidence of late rectal and urinary toxicities after Three-Dimensional conformal radiotherapy and Intensity-Modulated radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys. 2008;70(4):1124–1129. doi:10.1016/j.ijrobp.2007.11.044.
- casares-Magaz O, Bülow S, Pettersson NJ, et al. High accumulated doses to the inferior rectum are associated with late gastro-intestinal toxicity in a case-control study of prostate cancer patients treated with radiotherapy. Acta Oncol. 2019;58(10):1543–1546. doi:10.1080/0284186X.2019.1632476.
- casares-Magaz O, Muren LP, Mosieenko V, et al. Spatial rectal dose/volume metrics predict patient-reported gastro-intestinal symptoms after radiotherapy for prostate cancer. Acta Oncol. 2017;56(11):1507–1513. doi:10.1080/0284186X.2017.1370130.
- fokdal L, Honore H, Høyer M, et al. Dose-volume histograms associated to long-term colorectal functions in patients receiving pelvic radiotherapy. Radiother Oncol. 2005;74(2):203–210. doi:10.1016/j.radonc.2004.11.001.
- valdagni R, Rancati T. Reducing rectal injury during external bream radiotherapy for prostate cancer. Nat Rev Urol. 2013;10(6):345–357. doi:10.1038/nrurol.2013.96.

