Background
Clinical experience with online adaptive radiotherapy (oART) for head-and-neck (H&N) cancer is still limited, and an improved understanding of the process, risks, and benefits is needed to move forward [Citation1]. Added complexity is introduced to the treatment workflow, including deformable image registration (DIR) processes, automated contouring and online re-optimization, and quality assessment (QA) methods [Citation2]. Rapid online dose calculation is required and is in the presented clinical workflow based on the DIR of the planning CT to the anatomy of daily CBCTs. Dosimetric uncertainty as a result of suboptimal DIR should be quantified as part of safety assessment, and challenges are expected to be diagnosis/site-specific [Citation3]. In the current work, our institution’s first clinical experience with oART for H&N cancer is presented. The focus is on the dosimetric effect of uncertainty in the DIR/synthetic CT generation, as well as the dosimetric difference between the daily adapted plans and the original plan.
Material and methods
Patients and treatment
Four patients with H&N cancer were referred to CBCT-based oART on an Ethos linear accelerator (Varian Medical Systems, Palo Alto, CA USA). Treatment intent was palliative, with a prescription of 52 Gy in 13 fractions, 2 fractions/week.
Patient #1: Oropharyngeal cancer T1N2bM0, gross tumor volume (GTV) of 9.1 cc, treated with 7-field unilateral IMRT.
Patient #2: Oropharyngeal cancer T2N0M0, GTV 7.5 cc, treated with 9-field IMRT. Due to claustrophobia positioned in vac-fix instead of the standard immobilization of a five-point mask.
Patient #3: Hypopharyngeal cancer T2N0M0, GTV 13.2 cc, treated with 9-field IMRT.
Patient #4: Oral cavity cancer T4aN2bMx, GTV of 16.7 cc, treated with 9-field IMRT.
Standard planning treatment volume (PTV) margins of 3 mm (AP and LR) and 4 mm (CC) were applied, cropped 3 mm from the body surface. The treatment plans aimed to fulfill the following clinical goals: PTV: V95%>95%, V107%<1.8 cc, SpinalCord: Dmax<33.9 Gy (PRV_4mm <37.2 Gy), BrainStem: Dmax<39.9 Gy (PRV_4mm < 44 Gy), Parotid: Dmean<16Gy, Submandibularis Dmean<27Gy, Larynx: Dmean<31Gy, OralCavity minus PTV: Dmean<24Gy. QA was performed in Mobius (Varian Medical Systems, Palo Alto, USA) (all plans) and with ArcCHECK (Sun Nuclear, Melbourne, Australia) (first adaptive plan for each patient). Patients were assigned 45 min time slots.
Imaging and synthetic CT
Pre-treatment CT scans were performed in the treatment position on a Siemens Somatom scanner (Siemens Healthcare GmbH, Erlangen, Germany) with a 512 × 512 image matrix and 2 mm slice thickness (except 1 mm for patient #4). An iterative metal artifact reduction (iMAR) algorithm was applied. In the Ethos treatment planning system (TPS), image voxels with Hounsfield units (HU) above 2800 were automatically assigned to a so-called technical structure with either water or titanium as material. Technical structures were manually reviewed and changed if necessary. Larger areas with image artifacts around dental implants were manually contoured and overridden with HU = 0 (water).
Daily CBCTs were acquired with protocol Head (100 kV, 138 mAs). The CBCT was used for contouring (automatic, with or without daily corrections), while dose calculation was performed on a synthetic CT (sCT). The sCT was generated in Ethos by deformation of the planning CT to the anatomy of the daily CBCT; sCT was not visualized for the user online. The deformation algorithm used in Ethos is the VelocityTM deformable image registration, with an elastic deformation model (B-spline) [Citation4].
Visually guided correction of synthetic CT
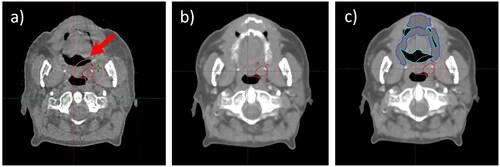
The sCTs from all treatment sessions were imported into the Eclipse TPS together with their corresponding CBCTs. Each sCT/CBCT pair was reviewed slice by slice, and discrepancies in anatomy/density were addressed by manual corrections (). Corrections were performed by one author (EG) and reviewed by another (KH). Correction structures were assigned one of the following materials/densities: air, water, bone, or titanium. The resulting corrected sCT (sCTcorr) was used for a second re-calculation to estimate the dosimetric effect of sCT/deformation uncertainty.
Figure 1. CBCT (a), synthetic CT (sCT) (b) and corrected sCT (sCTcorr) (c) of patient #1. GTV and CTV are displayed in red and Pink, respectively, and added water and air structures are displayed in blue and turquoise on c). the red arrow points at a part of the CTV that was contoured in air on the CBCT (a). the corresponding area on the sCT presents with tissue instead of air (b), which is corrected on the sCTcorr (c).
Re-calculation of plans and dosimetric analysis
Treatment plans were re-calculated with Acurox XB16.1.0 in Eclipse, where beam data for the Ethos/Halcyon accelerator was available. Two dosimetric comparisons were performed:
Original plan vs daily adapted plan, both calculated on the sCT, to illustrate the difference between adapting and not adapting.
Plan used for treatment (original or daily adapted), calculated on the sCT vs calculated on the sCTcorr, to illustrate the uncertainty in dose that can be assigned to sCT/deformation errors.
Dose metrics as reported above (section Patients and treatment) were compared by Wilcoxon signed rank test, but with CTV D99.9% analyzed instead of PTV V95%. p < 0.05 was considered statistically significant. Metrics were reported per fraction, i.e., no dose accumulation was performed. The structures used for dose reporting were the daily structures (targets and organs at risk (OARs)), which had been automatically deformed and online reviewed/modified by an oncologist.
Results
Three out of four patients completed the full course of oART. Patient #4 chose to refrain from the adaptive treatments after two fractions referring to too-long treatments and was thereafter treated non-adaptively. Results are presented for the remaining three patients.
Online adapted vs. original plan
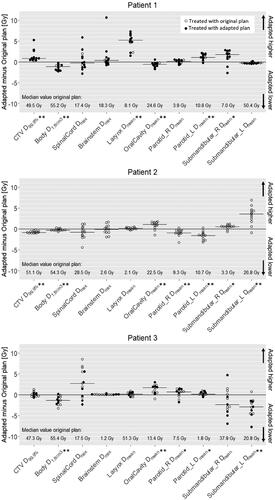
The daily adapted plan was chosen in 11/13 fractions for patient #1, in 0/13 fractions for patient #2, and in 6/13 fractions for patient #3. An overview of reasons for choosing/not choosing the adapted plan is available as supplementary material (Figure S1).
The difference in dose between the adapted and original plans is shown in . The CTV D99.9% was significantly higher in the adapted plans for patient #1 (median 50.4 Gy vs 49.5 Gy, p < 0.001), while it was lower for patient #2 (median 50.3 Gy vs 51.1 Gy, p < 0.001) and no significant difference for patient #3. The dose to 1.8 cc of the Body structure was significantly lower in the adapted plans for all three patients. The mean doses to OARs were significantly higher for some structures/patients and lower for some; the significant differences are marked with stars in . The most pronounced difference was for the larynx Dmean of patient #1 (median 13.6 Gy in the adapted plans vs 8.3 Gy in the original, p < 0.001).
Figure 2. Difference in dose metrics between the adapted and original plans obtained at each treatment fraction. The median dose difference for each patient and dose metric is represented by short horizontal lines in the graph, and significant differences are displayed at the x-axis labels with * for p < 0.05 and ** for p < 0.001. Treatment fractions where the adapted plan was chosen for treatment are shown with filled black dots.
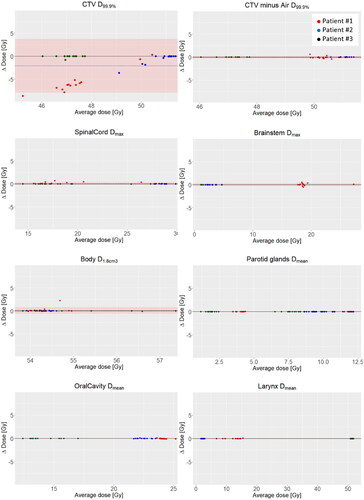
Dosimetric effect of synthetic CT correction
At visual assessment, the largest discrepancies between the CBCT and sCT anatomy occurred in areas of air cavities (). Corrections to the sCTs (to form the sCTcorr) were required, of varying extent, for 38/39 treatment fractions. Metal artifacts, which were pronounced in the CBCTs of patients #1 and #2, did not to the same extent appear in the sCTs (supplementary Figure S2).
The dose recalculated on sCTcorr affected the dose metrics for CTV to a larger extent than for the OARs. The mean dose differences and 95% confidence intervals (±1.96 sd) lay within ±0.4 Gy for all OAR metrics when all patients/fractions were analyzed combined (). The mean dose difference to the CTV (D99.9%) was −2.1 Gy (CI: −7.9–3.8 Gy), with the largest difference for patient #1. As CTV underdosage was found in areas of air, a secondary analysis was performed where parts of the CTV contoured in areas with air on the CBCT (example, see ) were excluded (boolean structure “CTV” minus “air_corrected”). For this structure, the mean dose difference was 0.00 Gy (CI: −0.3–0.3 Gy) ().
Discussion
Adaptive radiotherapy is one of the possible routes to improve treatment for future H&N cancer patients [Citation5]. In the current work, our clinic’s first experience with daily oART for this patient group was presented. Similar studies have previously been published for other treatment sites [Citation6–8]. Here, an investigation of the dosimetric effect of sCT uncertainty was added to the analysis. Data from three patients were analyzed, and results should therefore not be extrapolated to a general population. The results may nevertheless give valuable insight before starting up oART for H&N cancer.
The difference between the daily adapted plans and the original plans, when applied to the sCT of the day, showed different results for the individual patients (). Patient #1 had higher CTV coverage in the caudal parts of the target with the adapted plans, which came at a cost of a significantly higher larynx dose. This effect may be further mitigated if more IMRT angles or a VMAT technique were used. It should be noted that the larynx doses were not displayed for the oncologist at the online session, as the Ethos online TPS currently only shows clinical goals/constraints with a planning priority of 2 or higher, which was not the case for the larynx. For all three patients, a mixed image of OAR benefit of oART was seen (). This indicates that it may be necessary with a PTV margin reduction for a clear clinical benefit of oART. There is certainly a need for larger clinical studies of oART in H&N, where outcome, toxicity, and quality of life are measured.
For a margin reduction to be safe, CBCT image quality should be optimal in the whole extent of the target, and protocols preferably optimized for the specific task[Citation1]. The basis for dose calculation, i.e., the HU map, needs to be correct. In the current work, the dosimetric effect of sCT uncertainty was studied, based on the assumption that the difference between the sCT and the sCTcorr would be a good estimation of such uncertainty. It was found that the DIR did not always perform well around air cavities. It is known that regularization of DIR algorithms can cause problems when mass is not conserved, e.g., mass that “appear” or “disappears” from one image to the other. On the other hand, too little regularization can cause algorithms to produce false/unanatomical solutions [Citation9]. Even though there were target volumes close to air cavities in the current work, no concerning dosimetric effects of DIR/sCT errors were seen. Initial concerns were raised for the CTV coverage, which was lower when calculated on sCTcorr. At a closer look, it was found that the CTV had sometimes been contoured in the air (for example, see ). In the secondary analysis, where areas of air were removed from the CTV contours, a reassuringly good CTV dose agreement was seen (). If, on the other hand, the opposite was to happen – that the sCT presented air where there was CTV tissue on the CBCT – it would be more concerning, as this would lead to underdosage in what was actually part of the target. This points to a need for an individual QA procedure for sCT quality, as also suggested by Delaby et al. [Citation1].
The field of oART is rapidly evolving, and there are other options for defining the HU map for daily reoptimization/calculation. Direct calculation on the CBCT is already available [Citation10], avoiding the step of DIR. For the head and neck anatomy, however, authors have reported DIR or deep-learning-based sCT to be the best solution for CBCT-based dose calculation [Citation11,Citation12]. Dental metal artifacts are a challenge in this setting, which we found was less pronounced on the sCT than on the CBCT (supplementary Figure S2). Implementation of metal artifact reduction algorithms for CBCT may change the mentioned superiority of DIR. In any case, the results of the current study can serve as an estimation of what we should be able to expect in terms of dosimetric accuracy of the sCT in this anatomical region.
The patients of the current study were treated in a palliative setting. If this influenced the choice for one of the patients to refrain from adaptive treatment is impossible to know, but it is worth noting that the extra treatment time required for oART can be a challenge when patients are positioned with masks. To apply oART for H&N cancer in a curative setting also presents additional challenges of a larger treatment volume and additional OARs to consider.
In conclusion, the dosimetric effect of uncertainty in sCT generation was small in the three patients of the study. The DIR algorithm struggles around air cavities, and an individual QA strategy for the sCT may be recommended. OAR dose metrics were a mix of higher and lower in the adapted plans when compared to the original plans. This suggests that the possible clinical gain of oART in H&N cancer may require a margin reduction.
Supplemental Material
Download JPEG Image (259.7 KB)Supplemental Material
Download GIF Image (480.2 KB)Disclosure statement
The study was funded by a research grant from Varian Medical Systems.
Data availability statement
Data not available due to ethical/legal restrictions
Additional information
Funding
References
- Delaby N, Barateau A, Chiavassa S, et al. Practical and technical key challenges in head and neck adaptive radiotherapy: the GORTEC point of view. Phys Med. 2023;109:102568. doi: 10.1016/j.ejmp.2023.102568.
- Lim-Reinders S, Keller BM, Al-Ward S, et al. Online adaptive radiation therapy. Int J Radiat Oncol Biol Phys. 2017;99(4):994–1003. doi: 10.1016/j.ijrobp.2017.04.023.
- Glide-Hurst CK, Lee P, Yock AD, et al. Adaptive radiation therapy (ART) strategies and technical considerations: a state of the ART review from NRG oncology HHS public access. Int J Radiat Oncol Biol Phys. 2021;109(4):1054–1075. doi: 10.1016/j.ijrobp.2020.10.021.
- Varian Medical Systems. Ethos Algorithms Reference Guide Ethos Treatment Management Ethos Treatment Planning. 2019.
- Grégoire V, Langendijk J A, Nuyts S. Advances in radiotherapy for head and neck cancer. J Clin Oncol. 2015;33(29):3277–3284. doi: 10.1200/JCO.2015.61.2994.
- Åström LM, Behrens CP, Calmels L, et al. Online adaptive radiotherapy of urinary bladder cancer with full re-optimization to the anatomy of the day: initial experience and dosimetric benefits. Radiother Oncol. 2022;171:37–42. doi: 10.1016/j.radonc.2022.03.014.
- Byrne M, Archibald-Heeren B, Hu Y, et al. Varian ethos online adaptive radiotherapy for prostate cancer: early results of contouring accuracy, treatment plan quality, and treatment time. J Appl Clin Med Phys. 2022;23:e13479.
- Åström LM, Behrens CP, Storm KS, et al. Online adaptive radiotherapy of anal cancer: normal tissue sparing, target propagation methods, and first clinical experience. Radiother Oncol. 2022;176:92–98. doi: 10.1016/j.radonc.2022.09.015.
- Brock KK, Mutic S, McNutt TR, et al. Use of image registration and fusion algorithms and techniques in radiotherapy: report of the AAPM radiation therapy committee task group no. 132: report. Med Phys. 2017;44(7):e43–76–e76. doi: 10.1002/mp.12256.
- Salerno M, Haertter A, Koger B, et al. Characterization of a Novel High Performance kV CBCT System on a Ring-Gantry Linac. In: ESTRO 2023. Wienna; 2023.
- Barateau A, De Crevoisier R, Largent A, et al. Comparison of CBCT-based dose calculation methods in head and neck cancer radiotherapy: from hounsfield unit to density calibration curve to deep learning. Med Phys. 2020;47(10):4683–4693. doi: 10.1002/mp.14387.
- Giacometti V, King RB, Agnew CE, et al. An evaluation of techniques for dose calculation on cone beam computed tomography. Br J Radiol. 2019;92(1096):20180383. doi: 10.1259/bjr.20180383.