Abstract
It is estimated that approximately 97 million people in the world have complex communication needs and may benefit from alternative and augmentative communication (AAC). Although AAC is considered an evidenced-based intervention, device abandonment remains common, and researchers have attempted to analyze the causes of people abandoning devices. These devices have been prescribed following extensive assessment and often a protracted period of negotiation with a funding body. In this paper, we present the process of AAC prescription using a new model called the Communication Capability Approach by adding the Capability Approach from Amartya Sen to the widely used Participation Model. This allows clinicians to see individual daily decision-making as a valid choice of the individual. We propose reframing the concept of device abandonment as the person and their family making a choice to use a full range of multimodal communication to meet their own needs. This changes the tone of the narrative to viewing the person using AAC as competent and able to exercise self-determination and agency in this decision rather than as abandoning the device. AAC choices can be made on a day-to-day basis, according to the context of use so that people do not abandon devices but rather use whichever mode of communication is appropriate to the context.
People with complex communication needs may rely on alternative and augmentative communication (AAC) to communicate. AAC includes a range of paper-based materials as well as complex high tech computerized devices. AAC devices are often expensive and require not only financial investment but also time to learn to use the system. Despite advances in AAC technology (Kent-Walsh & Binger, Citation2018) and acceptance of this (Ripat et al., Citation2020), a significant body of research indicates that device abandonment continues to be common (Johnson et al., Citation2006; Moorcroft et al., Citation2020; Waller, Citation2019).
Johnson et al. (Citation2006) defined rejection of the AAC system as occurring prior to any attempt to use the system, and abandonment when the AAC system is no longer used, despite an ongoing need identified by the professionals involved. They reported that fewer than 40% of participants continue to use their AAC device 12 months after implementation. Reasons for AAC abandonment include poor usability, high learning demands, a lack of professional expertise and difficulty with physical access (Calculator, Citation2013; Ripat et al., Citation2019; Waller, Citation2019). Moorcroft et al. (Citation2021) identified a number of themes relating to device abandonment for child AAC users, including parental lack of emotional readiness and resilience to implement AAC, parents’ perception of the extra work required to implement AAC, parental report of the child not using their AAC system for communication, and a lack of parental satisfaction with the AAC system itself.
Device abandonment is not unique to people with a developmental disability. Individuals with acquired disorders have different AAC challenges, however, they also abandon devices (Pampoulou, Citation2019). Pampoulou identified the length of time since the onset of disability, the person’s acceptance and attitude toward communication facilitators, and perceptions about AAC systems as relevant to device abandonment. Thus, AAC device acceptance or abandonment is an issue for adults with acquired and developmental complex communication needs as well as families of young children new to AAC. Given that continued use of AAC is challenging and the high rate of abandonment of AAC, it is important to consider factors that impact device acceptance. The section that follows considers two factors: choice/preference in AAC and barriers to AAC implementation.
A key issue in understanding device use and abandonment is that of personal choice. Given the multimodal nature of communication, it is common for a person using AAC to use a range of communicative modalities alongside their device. These include facial expression and body language; pointing, gestures, and signing; vocalization or spoken words; alphabet boards; pen and paper; texting on mobile phones; and writing on a computer (Judge & Townend, Citation2013; Waller, Citation2019). Many adults (with either developmental or acquired disorders) using AAC report communicating differently with different communication partners and in different situations (Ripat et al., Citation2019). Some users report using their high-tech device if the content of the message is complex but prefer to use gestures and low-tech methods if the content can be expressed as effectively (Ripat et al., Citation2019). Some parents of children who use AAC report that their child will use low-tech AAC or gestures when the child’s needs are simple (Calculator, Citation2013).
Choice in AAC includes an array of options and devices. Judge & Townsend reported that people using AAC perceive a high-tech device as what they describe as a “minority communication tool” within a spectrum of communication methods (Judge & Townend, Citation2013, p. 378) by which they mean that the person’s high-tech device was used less frequently than other options. One parent of a child in a study by O’Neill and Wilkinson (Citation2020, p. 245) said “At home when it’s just us we use a lot of nonverbal communication, she’s very expressive… We don’t use her talker all the time. It’s our own personal style.” Speed, intelligibility, and the environment also impact the decision on whether to use an AAC device (Wickenden, Citation2011).
Communication style is individual, and for those using AAC, their “voice” is inextricably linked to the mode of AAC used. A person using AAC (with either developmental or acquired disorders) may consider that a synthesized voice does not represent their identity (Wickenden, Citation2011) and personality (Patel & Threats, Citation2016), consequently, people using AAC may choose low tech rather than speech generating devices in situations where their personality is more important to them than the method in which they communicate (Ripat et al., Citation2019). This can be challenging for AAC clinicians. Moorcroft et al. (Citation2019, p. 14) reported that clinicians in their study characterized a person’s preference to use their “limited speech or a different type of AAC” as a barrier to the “provision” of unaided or low-tech AAC rather than a legitimate choice for the person with complex communication needs. The authors imply that this choice - to use their existing speech or some other form of AAC not currently being recommended by this clinician - interferes with the role of the AAC clinician which is to provide an AAC system. This places the burden to overcome this barrier on the professional. Furthermore, Moorcroft et al. (Citation2022, pp. 4260) noted that when faced with a family who abandon AAC, the SLP may “push ahead” with AAC irrespective of the family’s wishes or suggest the family find a different clinician. One SLP in a study by Lynch et al. (Citation2019) expressed concern about the lack of family buy-in, noting that some families are clear that they never intend to use the device. Participants in the Lynch study did not see a lack of buy-in as a deterrent to recommending a device but did state that it would limit their expectations of how it might be used; however, decision making for families is complex. Doak (Citation2021) proposed a model for viewing family implementation of AAC that identified the complexity of managing AAC within the context of all the other pressures on families of a child with complex communication needs. Clinicians need to understand these complexities and balance that with their own frustrations and motivations.
When considering the choices made by the person using AAC, many practitioners and researchers try to ensure that AAC assessment includes the person’s preferences (Murray et al., Citation2019). The concept of preference refers to both device preference and personal preference. Device preferences can be measured be presenting the same task on multiple devices and observing the responses of the person; however, the term preference assessment is also used to determine the personal preferences the person has in their daily life in order to provide motivating activities and to target key vocabulary (Lund et al., Citation2021). While personal preferences are relatively easy to measure directly or via informant report, it may be difficult for a person who has never experienced successful communication using AAC, to express a preference for any particular mode or device. Some studies have compared different AAC options and measured acquisition and preference within structured settings such as which of two options does the child use to request a specific item (Achmadi et al., Citation2014; Couper et al., Citation2014); however, it is not clear whether preferred AAC modes at the time of assessment impact later abandonment of AAC.
In considering device abandonment, it is important to note the range of barriers that can impact the use of high-tech AAC. These include features of the device such as reliability, voice quality, and speed of message generation (Baxter et al., Citation2012; Waller, Citation2019); as well as other barriers such as financial barriers, waiting lists for services, and time and availability of support personnel to create resources (Moorcroft et al., Citation2019). Communication partners need to become skilled in device use (Anderson et al., Citation2014) and this can pose a barrier to successful implementation. For example, parents are expected to develop skills and technical knowledge to manage the device and to teach their child to use it. Furthermore, attitudinal barriers pose a barrier to effective AAC use (Johnston et al., Citation2020).
Given the research about device abandonment, it is important to consider how devices are prescribed and the roles of those involved. AAC clinicians make device recommendations based on the skills of the person across a broad range of domains including cognition, motor skills, vision and hearing, and social communication (Lund et al., Citation2017). Beukelman and Mirenda (Citation2013) suggested that assessment should be guided by the Participation Model, whereby a team of stakeholders consider facilitators and barriers, including environmental barriers, across this range of domains. This process involves individuals’ participation needs being identified alongside a range of barriers they may experience, followed by feature matching, whereby the operational requirements of the person are matched with the features of a device.
To prescribe an AAC device, the assessment process based on the Participation Model involves the team first identifying access and opportunity barriers and then planning intervention to decrease barriers. Intervention is likely to include an AAC device as well as a range of training to overcome skill and knowledge barriers by communication partners as well as to modify policies or practices that limit participation.
Although clinicians perceive that their decision-making is inclusive of people who use AAC and/or parents of young children with complex communication needs, AAC users and families do not always feel included (Mandak et al., Citation2017; McNaughton et al., Citation2019). Parents have reported not feeling supported by SLPs and feeling devalued and ignored by SLPs who see themselves as the experts in AAC (McNaughton et al., Citation2008; Moorcroft et al., Citation2020). In the paper by Moorcroft et al., parents felt that SLPs did not listen to them or their children. Parent voices are very clear in this paper, with direct quotes illustrating the challenges experienced by parents in implementing AAC. “I just felt like all the power was in their hands and I’m the stupid mum who doesn’t know anything about AAC…” Moorcroft et al. further noted that parents felt that they were not given a choice about the use of AAC and that they were pressured or directed toward a particular pathway based on the philosophies of the SLP or organization their child was receiving services from.
Given that successful implementation of AAC relies on the skills and attitudes of a range of people, it is important to clarify the roles of the various stakeholders (Binger et al., Citation2012; Calculator & Black, Citation2009; Ogletree, Citation2012; Ogletree et al., Citation2018; Schlosser & Raghavendra, Citation2004). Stakeholders include parents, communication partners, educators, paid staff, and healthcare professionals (Uthoff et al., Citation2021). Although the involvement of the person themselves is acknowledged, often it is challenging to include the person in a meaningful way. Binger et al. (Citation2012) state that “When possible, the client may serve as his or her own facilitator” and the assessment process should systematically assess the person’s preferences (p. 283). Finding ways to truly value the perspectives of the person for whom the device is being considered is ultimately essential to the success of communication using AAC.
The involvement of families within the AAC process is vital (Binger et al., Citation2012; Goldbart & Marshall, Citation2004; Parette et al., Citation2000) and families need “a voice” in AAC decision making (Parette et al., Citation2000) so their input is at the center of any decisions about AAC. Yet, it is not clear if families feel included in the process (McNaughton et al., Citation2019). More than 20 years ago families specified the supports that they want to implement AAC, including not only that professionals teach them how to use the device, but also that professionals understand that (a) families must meet many competing demands in their day-to-day lives, (b) whole families need to be involved in the AAC process, (c) every child with a disability is unique, (d) information is needed from a range of environments including home and school, (e) families differ in many ways including culturally, and (f) before discussing AAC intervention the professional needs to build rapport with each family member (Parette et al., Citation2000).
One game changer for families is the availability of AAC applications on an iPadFootnote1 (Ogletree et al., Citation2018; Paterson & Carpenter, Citation2015). Increasingly, families are purchasing this device and appropriate apps without an AAC assessment (Caron, Citation2015). iPads are relatively inexpensive and parents can buy apps without consultation with SLPs and trial the AAC that they choose. There is some evidence that apps can be used effectively as AAC alternatives to dedicated devices (Kagohara et al., Citation2013).
Decision making in AAC is challenging. Researchers have attempted to address this by creating a number of decision trees and frameworks that guide assessment, device selection, and intervention to support device learning (Sanders et al., Citation2021; Schlosser & Raghavendra, Citation2004). While the Participation Model (Beukelman & Mirenda, Citation2013) is probably the most familiar to those experienced in AAC, other frameworks can also be used to scaffold reasoning and decision making in AAC, including the SETT framework (Zabala, Citation2020), which considers the Student, Environment, Tasks, and Tools; and the Tri-focus Framework (Siegel-Causey & Bashinski, Citation1997), which considers the Learner, Partner, and Environment as key aspects for communication intervention. Additionally, there is the International Classification of Functioning, Disability, and Health (ICF), a framework from the World Health Organization (World Health Organization, Citation2001). Though it was not intended specifically for AAC or even for those with complex communication needs, it is often used by researchers to support AAC decision making (Bornman & Murphy, Citation2006; Huer & Threats, Citation2016).
The Participation Model identifies the participation needs of the individual and the features of the environment that might present barriers, such as policy, attitudes, and resources. The focus of an assessment within this framework is on how the person participates in their everyday life and what supports might allow them to participate more successfully. Key parameters relate to the participation of the person using AAC compared to that of their peers. Barriers to participation for people using AAC are termed access barriers and opportunity barriers. Access barriers relate to the specific skills of the individual, whereas opportunity barriers relate to environmental factors that result in the person not being afforded the opportunity to participate. Opportunity barriers include policies, knowledge, and skills of communication partners, and a broad range of societal and personal attitudes.
The SETT framework (Zabala, Citation2020) was designed to provide an organizational structure to help students who use AAC to participate more fully in their classes. The aim is for those involved with the student to identify people, the environment, the tasks, and the tools necessary to plan classroom activities for a student who uses AAC. The framework is not a specific protocol or assessment but rather a guiding framework to ensure that all aspects of a student’s needs are considered in AAC planning.
The TriFocus framework, created by Seigel-Causey and Bashinski (Citation1997), encourages those planning intervention for a person using AAC to plan across three different areas: the learner, the communication partner, and the environment. Successful AAC intervention requires changes in not only the person themselves (learner) but also those that interact with them (partner) and in the environments in which the person functions (environment), as each area can impact communicative success.
The World Health Organization’s ICF framework focuses on participation and puts the person with a disability at the center of a network of contextual factors that include environmental and personal factors. The ICF defines disability as “dysfunctioning” (World Health Organization, Citation2002, p. 10) at one or more levels of impairment, activity, and participation and uses qualifiers to record the presence and severity of the problem at the level of body functions and structures, activity limitation, and participation restriction. The qualifiers include the concept of capacity vs. performance. For a person with complex communication needs, that might involve considering how the person would communicate if they had an optimal device in an optimal environment. This would involve imagining that there were no barriers to participation in the environment such as policies, attitudes, or resources.
Both the Participation Model and the ICF are based on the social model of disability, which situates disability as not being due to impairments but to barriers in society (Oliver, Citation2013). Whilst these models provide guidance to clinicians and others about assessment and intervention for people who use AAC, there are limitations to both. Trani et al. (Citation2011) argued that there is a missing element in the ICF, that of beliefs, values, and preferences. Mitra and Shakespeare (Citation2019) proposed that the ICF needs remodeling as it has fallen behind the current understanding of disability. Specifically, the authors argue that the ICF is not person-centered and does not have sufficient focus on quality of life. They also query whether the ICF considers the agency of the individual and the extent to which they can “act, participate or live on behalf of what matters to him/her” (Mitra & Shakespeare, Citation2019, p. 338). Trani et al. proposed that the Capability Approach be considered as an alternate model to the ICF in order to capture individual preferences and choices. In this paper, we present the process of AAC prescription by considering adding the Capability Approach from Amartya Sen to the widely used Participation Model to create a model called the Communication Capability Approach.
Method
In creating a framework for AAC relating to the Capability Approach, we reviewed the literature about the Capability Approach and its use relating to people with a disability. The section that follows introduces the approach with reference to people with a disability and more specifically those who use AAC. The Capability Approach was developed by economist Amartya Sen (Citation1980) and further developed by the philosopher Martha Nussbaum (Citation2000) as a way of conceptualizing individuals whom they describe as being disadvantaged within society. It is described as a conceptual framework of well-being, development, and justice, which has revolutionized modern welfare economics as well as health and development policy (Paraschivoiu et al., Citation2020). The Capability Approach views a person’s achievements and freedoms as based not only on what they are capable of but also on what they value and ultimately choose.
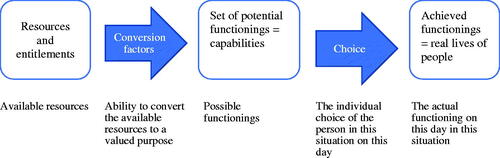
The Capability Approach defines capabilities not as physical or intellectual features but as a set of opportunities and the freedom to choose what the person wants to do or be. These “doings” and “beings” are referred to as functionings. Within the Capability Approach the capability of a person (their potential functioning) is shaped by those around him or her including the individual themselves (age, gender, ethnicity, educational level, disability etc) as well as their family, community, national politics and society. A person uses available resources which they convert into a set of possible functionings, for example, communicating with others. Their final achieved functioning is based on which of the possible functions they ultimately choose as shown in . The term capability within the Capability Approach has a very different meaning compared to the term capability in the Participation Model.
The example of a bike is often used to illustrate the framework. Clearly, a bike is made up of parts, of specific materials and shapes but we view the bike as an object that has value or utility: specifically, it can be used for mobility. Mobility allows us to participate in a range of activities – to get to places faster, and to be independent, which is referred to as valuable functioning. However, a person may not be able to use the bike to achieve that functioning (to participate) if they cannot ride (for example if they have a disability) or if there are no safe pathways for bikes in the location in which the person lives.
Robeyns (Citation2005) explains the bike as a resource (goods or services) that the person can use (conversion) to travel faster and thus it provides them with mobility (capability), which consequently makes it possible (freedom) for the person to visit friends more often (functioning). If we translate this to AAC we can see that some low-tech symbols (resources, goods or services) can be used to communicate with others. As illustrated in , the person needs to be able to convert the resource (the low-tech symbols) to a valued purpose; that of communication. In the Capability Approach, this is referred to as capability.
Table 1. Illustrating the capability approach using a physical example and a communicative example.
Although the Capability Approach is a complex framework, at its core it asks the simple question: What are people able to do and what do they have the potential to be?
Capability Approach and disability
Within the Capability Approach, as with the ICF, the Participation Model and the social model of disability (Oliver, Citation2013), disability is viewed as more than just the skills of the person, it includes consideration of environmental and societal factors, and barriers created in society that limit the person’s opportunities to fully participate in the life of the community. Terzi (Citation2005) argues that the Capability Approach offers two insights to disability that are not evident in other models: First, that Sen views impairment and disability as aspects of human diversity and second, that he places human diversity at the core of evaluation of people’s advantage or disadvantages which results in evaluating disability in relation to relevant freedoms, and ultimately, justice.
Terzi argues that the Capability Approach allows understanding of the relationship between impairment, disability and social arrangements where people with a disability are entitled to effective freedoms, that is, their capabilities for well-being. The Capability Approach reframes impairment and disability in terms of functionings and capabilities. Impairment may affect certain functionings whereas disability is a restriction of functionings. A restriction in functionings results in a restriction of the set of possible functionings available to the person. There it results in a narrower range of capability. Consequently, whether impairments result in disability depends both on the possible overcoming of the impairment itself and on the specific design of the social and physical environment. Therefore, impairment and disability in the Capability Approach imply considering the full sets of capabilities one person can choose from and evaluating the impact of impairment on these sets of freedoms.
Several authors have directly compared the Capability Approach to the ICF (Bickenbach, Citation2014; Morris, Citation2009; Trani et al., Citation2011). Trani et al. suggest that the ICF is missing the dimension of individual identity. They suggest that individual identity that is grounded in the person’s beliefs, values and preferences goes beyond body function and structure, and activities and participation. They suggest that the ICF “completely fails to appreciate this dimension” (Trani et al., Citation2011 p.147) and state that the environment in the ICF is merely a mechanical facilitator or barrier. Considering this through the lens of the Capability Approach, the individual perceives her/his environment through a capability set.
The Capability Approach and AAC device prescription
Using the Capability Approach to guide AAC prescription would involve identifying conversion factors (including a series of social and personal factors) in order to identify a set of possible functionings. This approach would view the choice-making relating to AAC as a choice made by the person not only once but according to different contexts. The person might have a set of possible functionings that might include using a high tech AAC device but also using communication options chosen according to the activity, environment and people that exist in each situation. This might be viewed as a subtle difference, but it moves the choice away from being that of the clinician and places the opportunity for daily choice in the hands of the person using AAC. It would consider using AAC as being one of a range of possible functionings which would validate user choice and move away from the concept of abandonment instead viewing this need to choose as a daily event. For example, a child who is being teased at school by one particular child about using a device, may choose to not use their device when the bully is in the room. An adult who has carers to help with dressing and personal hygiene may use low-tech and gestures to communicate because it is quicker and easier than using their high-tech device.
Proposed model: Communication Capability Approach
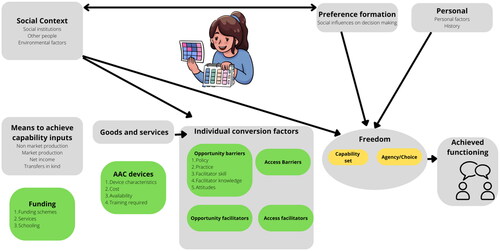
Several authors have created visual models to represent the complex interchange between components of the Capability Approach (Mitra, Citation2006; Morris, Citation2009; Robeyns, Citation2005). We have created a visual representation based on the model by Robeyns (Citation2017) demonstrating where the participation model overlaps with the Capability Approach in relation to AAC and how the participation model could be incorporated into the Capability Approach to create a Communication Capability Approach.
In the Communication Capability Approach () the grey boxes are similar to the Robeyns model, and the green boxes include aspects of the Participation Model. The availability of devices, specialist assessment teams, funding for devices, and device trials will impact available resources. Conversion factors include the skills and attitudes of the person themselves as well as those of a range of people in a range of settings in which the person functions. Ultimately the interaction of resources and conversion factors results in a set of possible behaviors which are capability sets. Social context influences conversion factors and the capability set. Social influences on decision making, personal history and personality influence agency and choice. The combination of agency and capability results in the freedom to choose the actual achieved functioning. In AAC, the achieved functioning is the way in which the person chooses to communicate in any given situation.
The person using AAC may now be able to communicate in several different ways perhaps in different locations. They may use sign language and gesture at home with familiar communication partners; they may use the high-tech device at school in formal educational settings but may also use low tech AAC when chatting with friends at school or on the school bus. These different options are considered capability sets within the Capability Approach and, combined with agency, these create freedom for the person to choose how to communicate. Their decision results in their achieved functioning which may be different in different situations with a range of communication partners. The Capability Approach differs from the ICF or the Participation Model primarily in the concept of choice and agency.
Expected advantages using the Communication Capability Approach for AAC
The Communication Capability Approach (CCA) has the advantage of considering the use of AAC as a daily choice rather than a single preference. While the Participation Model is an established framework in AAC, it does not account for the need for the person to have multiple options to choose from for every situation. Adding the concept of “possible functionings” through the incorporation of the Capability Approach will allow clinicians to focus on multiple possible communication options to meet different functional needs. The concept of multimodality is commonly used in AAC but typically refers to the use of both aided and unaided AAC whereby the person uses AAC but also uses a range of body language, facial expressions and gestures. Here we are proposing that the person may use different AAC systems as part of multimodal communication.
Calculator (Citation2013) noted that children who reject a high-tech device may also reject other forms of electronic communication. Calculator surveyed parents and asked them to judge whether or not their child had accepted or rejected the AAC. The wording posed to parents as a binary choice doesn’t consider that the child may be using it for some things but not others. Our proposed use of the Capability Approach would support clinicians to phrase variable device use as part of the expected multimodal nature of communication rather than a binary choice of accept vs. reject.
Conclusion
AAC research is complex and this is evidenced by the number of models or frameworks that guide the field. There are articles about family and user experience, speech-language pathologist training, the process of assessment, and device abandonment. This paper proposes including a different framework: the Capability Approach by Amartya Sen with one aspect that is not included in the other approaches: that of choice or agency and the freedom to choose. Multimodal is a concept that is often used to describe how a person using AAC communicates. However, the concept of choosing modes does not seem to exist comfortably with device prescription, which views the provision of a device as a specialist skill carried out by experts (clinicians) and that when a person stops using the recommended device, they have abandoned not only the device but also the expert advice.
Donaldson et al. (Citation2021) interviewed adults with autism spectrum disorder who can use speech, but sometimes prefer to use an AAC device. The participants listed choice as a key factor in their relationships:
What makes communication successful for me is when I can use the method that works best for me in the moment, and when the other person just accepts that method” and “I love multimodal communication. My brain loves it. It is so much easier to communicate with multimodal communication. It is hard to try to force myself to one communication method when I can use multiple. Life is easier with multiple. Different methods have different advantage[s] (p. 319).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Notes
1 The iPad© is a product of Apple Computers, Cupertino, CA. www.apple.com
References
- Achmadi, D., Sigafoos, J., van der Meer, L., Sutherland, D., Lancioni, G. E., O’Reilly, M. F., Hodis, F., Green, V. A., McLay, L., & Marschik, P. B. (2014). Acquisition, preference, and follow-up data on the use of three AAC options by four boys with developmental disability/delay. Journal of Developmental and Physical Disabilities, 26(5), 565–583. https://doi.org/10.1007/s10882-014-9379-z
- Anderson, K., Balandin, S., & Stancliffe, R. (2014). Australian parents’ experiences of speech generating device (SGD) service delivery. Developmental Neurorehabilitation, 17(2), 75–83. https://doi.org/10.3109/17518423.2013.857735
- Baxter, S., Enderby, P., Evans, P., & Judge, S. (2012). Barriers and facilitators to the use of high-technology augmentative and alternative communication devices: A systematic review and qualitative synthesis. International Journal of Language & Communication Disorders, 47(2), 115–129. https://doi.org/10.1111/j.1460-6984.2011.00090.x
- Beukelman, D. R., & Mirenda, P. (2013). Augmentative and alternative communication: Supporting children and adults with complex communication needs (4th ed.). Paul H. Brookes Pub.
- Bickenbach, J. (2014). Reconciling the capability approach and the ICF. Alter, 8(1), 10–23. https://doi.org/10.1016/j.alter.2013.08.003
- Binger, C., Ball, L., Dietz, A., Kent-Walsh, J., Lasker, J., Lund, S., McKelvey, M., & Quach, W. (2012). Personnel roles in the AAC assessment process. Augmentative and Alternative Communication, 28(4), 278–288. https://doi.org/10.3109/07434618.2012.716079
- Bornman, J., & Murphy, J. (2006). Using the ICF in goal setting: Clinical application using talking mats. Disability and Rehabilitation Assistive Technology, 1(3), 145–154. https://doi.org/10.1080/17483100612331392745
- Calculator, S. N. (2013). Use and acceptance of AAC systems by children with Angelman syndrome. Journal of Applied Research in Intellectual Disabilities: JARID, 26(6), 557–567. https://doi.org/10.1111/jar.12048
- Calculator, S. N., & Black, T. (2009). Validation of an inventory of best practices in the provision of augmentative and alternative communication services to students with severe disabilities in general education classrooms. American Journal of Speech-Language Pathology, 18(4), 329–342. https://doi.org/10.1044/1058-0360(2009/08-0065)
- Caron, J. G. (2015). We Bought an iPad”: Considering family priorities, needs, and preferences as an aac support provider. Perspectives on Augmentative and Alternative Communication, 24(1), 5–11. https://doi.org/10.1044/aac24.1.5
- Couper, L., van der Meer, L., Schafer, M. C., McKenzie, E., McLay, L., O'Reilly, M. F., Lancioni, G. E., Marschik, P. B., Sigafoos, J., & Sutherland, D. (2014). Comparing acquisition of and preference for manual signs, picture exchange, and speech-generating devices in nine children with autism spectrum disorder. Developmental Neurorehabilitation, 17(2), 99–109. https://doi.org/10.3109/17518423.2013.870244
- Doak, L. (2021). Rethinking family (dis)engagement with augmentative & alternative communication. Journal of Research in Special Educational Needs, 21(3), 198–210. https://doi.org/10.1111/1471-3802.12510
- Donaldson, A. L., Corbin, e., & McCoy, J. (2021). Everyone Deserves AAC”: Preliminary study of the experiences of speaking autistic adults who use augmentative and alternative communication. Perspectives of the ASHA Special Interest Groups, 6(2), 315–326. https://doi.org/10.1044/2021_PERSP-20-00220
- Goldbart, J., & Marshall, J. (2004). Pushes and pulls" on the parents of children who use AAC. Augmentative and Alternative Communication, 20(4), 194–208. https://doi.org/10.1080/07434610400010960
- Huer, M. B., & Threats, T. T. (2016). Shared responsibilities for full participation in society: Planning further integration of the ICF into AAC. Perspectives of the ASHA Special Interest Groups, 1(12), 83–93. https://doi.org/10.1044/persp1.SIG12.83
- Johnson, J. M., Inglebret, E., Jones, C., & Ray, J. (2006). Perspectives of speech language pathologists regarding success versus abandonment of AAC. Augmentative and Alternative Communication (Baltimore, Md. : 1985), 22(2), 85–99. https://doi.org/10.1080/07434610500483588
- Johnston, S. S., Blue, C., Gevarter, C., Ivy, S., & Stegenga, S. (2020). Opportunity barriers and promising practices for supporting individuals with complex communication needs. Current Developmental Disorders Reports, 7(3), 100–108. https://doi.org/10.1007/s40474-020-00195-w
- Judge, S., & Townend, G. (2013). Perceptions of the design of voice output communication aids. International Journal of Language & Communication Disorders, 48(4), 366–381. https://doi.org/10.1111/1460-6984.12012
- Kagohara, D. M., van der Meer, L., Ramdoss, S., O'Reilly, M. F., Lancioni, G. E., Davis, T. N., Rispoli, M., Lang, R., Marschik, P. B., Sutherland, D., Green, V. A., & Sigafoos, J. (2013). Using iPods® and iPads® in teaching programs for individuals with developmental disabilities: A systematic review. Research in Developmental Disabilities, 34(1), 147–156. https://doi.org/10.1016/j.ridd.2012.07.027
- Kent-Walsh, J., & Binger, C. (2018). Methodological advances, opportunities, and challenges in AAC research. Augmentative and Alternative Communication, 34(2), 93–103. https://doi.org/10.1080/07434618.2018.1456560
- Lund, S. K., Quach, W., Weissling, K., McKelvey, M., & Dietz, A. (2017). Assessment with children who need augmentative and alternative communication (AAC): Clinical decisions of AAC specialists. Language, Speech, and Hearing Services in Schools, 48(1), 56–68. https://doi.org/10.1044/2016_LSHSS-15-0086
- Lund, S. K., Weissling, K., Quach, W., & McKelvey, M. (2021). Finding a voice for individuals with ASD who are minimally verbal through comprehensive communication assessment. Perspectives of the ASHA Special Interest Groups, 6(2), 306–314. https://doi.org/10.1044/2021_PERSP-20-00227
- Lynch, Y., Murray, J., Moulam, L., Meredith, S., Goldbart, J., Smith, M., Batorowicz, B., Randall, N., & Judge, S. (2019). Decision-making in communication aid recommendations in the UK: Cultural and contextual influencers. Augmentative and Alternative Communication, 35(3), 180–192. https://doi.org/10.1080/07434618.2019.1599066
- Mandak, K., O'Neill, T., Light, J., & Fosco, G. M. (2017). Bridging the gap from values to actions: A family systems framework for family-centered AAC services. Augmentative and Alternative Communication, 33(1), 32–41. https://doi.org/10.1080/07434618.2016.1271453
- McNaughton, D., Light, J., Beukelman, D. R., Klein, C., Nieder, D., & Nazareth, G. (2019). Building capacity in AAC: A person-centred approach to supporting participation by people with complex communication needs. Augmentative and Alternative Communication, 35(1), 56–68. https://doi.org/10.1080/07434618.2018.1556731
- McNaughton, D., Rackensperger, T., Benedek-Wood, E., Krezman, C., Williams, M. B., & Light, J. (2008). A child needs to be given a chance to succeed”: parents of individuals who use AAC describe the benefits and challenges of learning AAC technologies. Augmentative and Alternative Communication, 24(1), 43–55. https://doi.org/10.1080/07434610701421007
- Mitra, S. (2006). The Capability Approach and disability. Journal of Disability Policy Studies, 16(4), 236–247. https://doi.org/10.1177/10442073060160040501
- Mitra, S., & Shakespeare, T. (2019). Remodeling the ICF. Disability and Health Journal, 12(3), 337–339. https://doi.org/10.1016/j.dhjo.2019.01.008
- Moorcroft, A., Allum, J., & Scarinci, N. (2022). Speech language pathologists’ responses to the rejection or abandonment of AAC systems. Disability and Rehabilitation, 44(16), 4257–4265. https://doi.org/10.1080/09638288.2021.1900412
- Moorcroft, A., Scarinci, N., & Meyer, C. (2019). A systematic review of the barriers and facilitators to the provision and use of low-tech and unaided AAC systems for people with complex communication needs and their families. Disability and Rehabilitation Assistive Technology, 14(7), 710–731. https://doi.org/10.1080/17483107.2018.1499135
- Moorcroft, A., Scarinci, N., & Meyer, C. (2020). We were just kind of handed it and then it was smoke bombed by everyone’: How do external stakeholders contribute to parent rejection and the abandonment of AAC systems? International Journal of Language & Communication Disorders, 55(1), 59–69. https://doi.org/10.1111/1460-6984.12502
- Moorcroft, A., Scarinci, N., & Meyer, C. (2021). I’ve had a love-hate, I mean mostly hate relationship with these PODD books”: parent perceptions of how they and their child contributed to AAC rejection and abandonment. Disability and Rehabilitation Assistive Technology, 16(1), 72–82. https://doi.org/10.1080/17483107.2019.1632944
- Morris, C. (2009). Measuring participation in childhood disability: How does the capability approach improve our understanding? Developmental Medicine and Child Neurology, 51(2), 92–94. https://doi.org/10.1111/j.1469-8749.2008.03248.x
- Murray, J., Lynch, Y., Meredith, S., Moulam, L., Goldbart, J., Smith, M., Randall, N., & Judge, S. (2019). Professionals’ decision-making in recommending communication aids in the UK: Competing considerations. Augmentative and Alternative Communication, 35(3), 167–179. https://doi.org/10.1080/07434618.2019.1597384
- Nussbaum, M. C. (2000). Women and human development: The capabilities approach. (Vol. 3). Cambridge University Press.
- O’Neill, T., & Wilkinson, K. M. (2020). Preliminary investigation of the perspectives of parents of children with cerebral palsy on the supports, challenges, and realities of integrating augmentative and alternative communication into everyday life. American Journal of Speech-Language Pathology, 29(1), 238–254. https://doi.org/10.1044/2019_AJSLP-19-00103
- Ogletree, B. T. (2012). Stakeholders as partners: Making AAC work better. Perspectives on Augmentative and Alternative Communication, 21(4), 151–158. https://doi.org/10.1044/aac21.4.151
- Ogletree, B. T., McMurry, S., Schmidt, M., & Evans, K. (2018). The changing world of augmentative and alternative communication (AAC): examining three realities faced by today’s AAC provider. Perspectives of the ASHA Special Interest Groups, 3(12), 113–122. https://doi.org/10.1044/persp3.SIG12.113
- Oliver, M. (2013). The social model of disability: Thirty years on. Disability & Society, 28(7), 1024–1026. https://doi.org/10.1080/09687599.2013.818773
- Pampoulou, E. (2019). Speech and language therapists’ views about AAC system acceptance by people with acquired communication disorders. Disability and Rehabilitation Assistive Technology, 14(5), 471–478. https://doi.org/10.1080/17483107.2018.1463401
- Paraschivoiu, I., Winkler, A., & Meschtscherjakov, A. (2020). Beyond “assistive” four tensions in the design of AAL based on the capability approach [Paper presentation]. Companion Publication of the 2020 ACM Designing Interactive Systems Conference. https://doi.org/10.1145/3393914.3395859
- Parette, H. P., Brotherson, M. J., & Huer, M. B. (2000). Giving families a voice in augmentative and alternative communication decision- making. Education and Training in Mental Retardation and Developmental Disabilities, 35(2), 177–190.
- Patel, R., & Threats, T. T. (2016). One’s voice: A central component of personal factors in augmentative and alternative communication. Perspectives of the ASHA Special Interest Groups, 1(12), 94–98. https://doi.org/10.1044/persp1.SIG12.94
- Paterson, H., & Carpenter, C. (2015). Using different methods to communicate: How adults with severe acquired communication difficulties make decisions about the communication methods they use and how they experience them. Disability and Rehabilitation, 37(17), 1522–1530. https://doi.org/10.3109/09638288.2015.1052575
- Ripat, J., Verdonck, M., Gacek, C., & McNicol, S. (2019). A qualitative metasynthesis of the meaning of speech-generating devices for people with complex communication needs. Augmentative and Alternative Communication, 35(2), 69–79. https://doi.org/10.1080/07434618.2018.1513071
- Ripat, J., Woodgate, R. L., & Bennett, L. (2020). Attitudes faced by young adults using assistive technology as depicted through photovoice. Disability and Rehabilitation Assistive Technology, 15(3), 314–321. https://doi.org/10.1080/17483107.2019.1571118
- Robeyns, I. (2005). The capability approach: A theoretical survey. Journal of Human Development, 6(1), 93–117. https://doi.org/10.1080/146498805200034266
- Robeyns, I. (2017). Wellbeing, freedom and social justice: The capability approach re-examined. Open Book Publishers.
- Sanders, E. J., Page, T. A., & Lesher, D. (2021). School-based speech-language pathologists: Confidence in augmentative and alternative communication assessment. Language, Speech, and Hearing Services in Schools, 52(2), 512–528. https://doi.org/10.1044/2020_LSHSS-20-00067
- Schlosser, R. W., & Raghavendra, P. (2004). Evidence-based practice in augmentative and alternative communication. Augmentative and Alternative Communication, 20(1), 1–21. https://doi.org/10.1080/07434610310001621083
- Sen, A. (1980). Equality of what? In S. McMurrin (Ed.), The tanner lectures on human values (pp. 196–220). University of Utah Press.
- Siegel-Causey, E., & Bashinski, S. M. (1997). Enhancing initial communication and responsiveness of learners with multiple disabilities. Focus on Autism and Other Developmental Disabilities, 12(2), 105–120. https://doi.org/10.1177/108835769701200206
- Terzi, L. (2005). Beyond the dilemma of difference: The capability approach to disability and special educational needs. Journal of Philosophy of Education, 39(3), 443–459. https://doi.org/10.1111/j.1467-9752.2005.00447.x
- Trani, J.-F., Bakhshi, P., Bellanca, N., Biggeri, M., & Marchetta, F. (2011). Disabilities through the Capability Approach lens: Implications for public policies. Alter, 5(3), 143–157. https://doi.org/10.1016/j.alter.2011.04.001
- Uthoff, S. A. K., Zinkevich, A., Boenisch, J., Sachse, S. K., Bernasconi, T., & Ansmann, L. (2021). Collaboration between stakeholders involved in augmentative and alternative communication (AAC) care of people without natural speech. Journal of Interprofessional Care, 35(6), 821–831. https://doi.org/10.1080/13561820.2020.1860918
- Waller, A. (2019). Telling tales: Unlocking the potential of AAC technologies. International Journal of Language & Communication Disorders, 54(2), 159–169. https://doi.org/10.1111/1460-6984.12449
- Wickenden, M. (2011). Whose voice is that?: Issues of identity, voice and representation arising in an ethnographic study of the lives of disabled teenagers who use Augmentative and Alternative Communication (AAC). Disability Studies Quarterly, 31(4), https://doi.org/10.18061/dsq.v31i4.1724
- World Health Organization (2001). International Classification of Functioning, Disability and Health: (ICF). World Health Organization.
- World Health Organization (2002). Towards a common language for functioning, disability, and health: ICF. The international classification of functioning, disability and health. https://www.who.it/classifications/icf/icfbeginnersguide.pdf
- Zabala, J. S. (2020). The SETT Framework: A model for selection and use of assistive technology tools and more. In D. Chambers (Ed.), Assistive technology to support inclusive education (Vol. 14, pp. 17–36). Emerald Publishing Limited.