Abstract
Individuals with multiple disabilities are among the most challenging to serve and AAC teams often lack direction in determining effective interventions. The purpose of this scoping review was to summarize the research evidence on AAC interventions for individuals with complex communication needs and simultaneous motor, and visual impairments as part of their multiple disabilities; to consider implications for practice; and to determine gaps and directions for future research. A total of 27 studies were identified and reviewed, involving 55 unique participants with multiple disabilities. Most studies focused on direct intervention to increase requesting or choice-making, with little focus on social communication. Only two studies focused on training communication partners. Results indicated that AAC interventions can be highly effective to increase communication for individuals with multiple disabilities. However, there is an urgent need for increased rigor and more detailed participant information in future AAC intervention research with this population. Future research should investigate AAC intervention to improve social communication and increase language development, not just expression of needs and wants. Future research should focus on the needs of individuals with multiple disabilities from culturally and linguistically diverse backgrounds and on implementation of AAC within natural environments.
Introduction
Children and young adults who experience simultaneous impairments in both visual and motor functions often have additional complex communication needs due to severe speech impairments (Beukelman & Light, Citation2020; Horn & Kang, Citation2012). The term multiple disabilities is used to encompass individuals who may experience two or more significant concomitant impairments across domains of functioning, which includes combinations of impairments in vision, motor skills, hearing, cognition, and/or communication (IDEA, Citation2018). Specifically, this paper focused on the subset of individuals with concomitant visual, motor, and communication impairments as part of their multiple disabilities. Due to the high risk of additional disabilities in hearing, cognition, and/or other medical conditions in this population (Sigafoos et al., Citation2021), individuals with additional impairments were included if they met the criteria of experiencing simultaneous challenges in vision, motor, and communication. This population have unique and complex needs that necessitate the development and implementation of effective interventions.
Individuals with multiple disabilities can be very challenging to serve for many reasons, including the high prevalence of additional intellectual disabilities, low arousal states, and difficulty with identification of a functional communicative response during service delivery (Sigafoos et al., Citation2021). Furthermore, many individuals with multiple disabilities present with inconsistent methods of communication that are presymbolic (Grove et al., Citation1999), despite being at or above the age at which symbolic communication should develop (Holyfield, Light, et al., Citation2018; Holyfield, Caron, et al., Citation2018b). Augmentative and alternative communication (AAC), including gestures, pictures, signs, or speech-generating devices, may be beneficial to support the effective communication of these children and young adults with multiple disabilities (Beukelman & Light, Citation2020). Individuals with disabilities commonly have increased access to intervention and education services until the age of 21 (CDC, Citation2022). This is an important developmental period, and it is critical that AAC intervention is tailored to meet the unique needs of this complex population. Therefore, the current paper focused on individuals with multiple disabilities between the ages of zero and 21 (i.e. children and young adults).
Individuals with multiple disabilities often experience developmental delays and limitations in participation, activities of daily living, and access to general education (CDC, Citation2020; Jones et al., Citation2006). Additionally, they often require significant supports from caregivers and professionals (Trabacca et al., Citation2016). It is important that AAC is designed to best support increased communication and engagement. These individuals with multiple disabilities may experience severe motor impairments resulting in postural instability, restrictions to independent mobility, and limited engagement with the environment, and may require seating and positioning as well as adaptations to support access to AAC (e.g. eye gaze and microswitch). Additionally, children and young adults with multiple disabilities may experience a range of visual impairments of varying severity such as reduced acuity, astigmatism, nystagmus, blindness, or cortical visual impairment (CVI); these visual impairments may require adaptations to the environment and the AAC system. The possible presence of intellectual disability in individuals with multiple disabilities and communication impairments necessitates careful considerations for assessment, intervention, and AAC system design (Chadwick et al., Citation2019; Maes et al., Citation2021). Furthermore, individuals with multiple disabilities are at risk for hearing impairments (Roush et al., Citation2004), which vary in type (e.g. sensorineural and inner ear) and severity (i.e. mild to severe) and may contribute to language delays. It is imperative that AAC systems and interventions are designed to best meet the needs of those with multiple disabilities and complex communication needs. In particular, motor and vision skills are important for AAC access and must be considered when designing AAC interventions for children and young adults with complex communication needs.
Children and young adults with multiple disabilities are at high risk for speech and language impairments and often require AAC to support effective communication (receptive and/or expressive) (Horn & Kang, Citation2012) and to facilitate participation in meaningful activities of daily living. Successful communication is crucial to support self-advocacy, attain knowledge, express emotions, build social relationships, and enhance education and employment. Unfortunately, many speech-language pathologists report that they are not well prepared to provide AAC interventions generally (ATIA, Citation2020); and they may be especially overwhelmed when providing AAC services to individuals with multiple disabilities (e.g. concomitant motor and vision impairments) given the complexity of their needs. It is imperative that AAC interventions implemented with individuals with multiple disabilities are effective since learning may be slow. It is important to minimize the risk of failure that can lead to long-lasting detrimental effects (Jones et al., Citation2006). A first step in determining effective, evidence-based AAC interventions is to understand the current state of AAC intervention research for individuals with multiple disabilities. Importantly, whilst previous literature reviews have investigated AAC intervention for those with multiple disabilities (e.g. Simacek et al., Citation2018; Stasolla & Perilli, Citation2015), none to date have specifically addressed the needs of children and young adults with concomitant motor, visual, and communication impairments who require AAC, despite the necessity of considering both motor and visual functions when designing and implementing effective AAC systems.
Purpose of this scoping review
A scoping review methodology was used to assess the existing research on AAC intervention for children and young adults (0–21 years) with complex communication needs and simultaneous motor and visual impairments (i.e. multiple disabilities), completed at any point in time up until the present (2023). There was no timeframe set for the search to minimize the chance of missing important early research studies. Similar to a systematic review, a scoping review comprehensively synthesizes the research on a given topic (Munn et al., Citation2018). However, a scoping review is more exploratory in nature than a systematic review and is appropriate for mapping the research on topics that may not be strongly established or may have a scattered literature (Pawliuk et al., Citation2021). Hence a scoping review was deemed appropriate for the topic of AAC intervention research with children and young adults with multiple disabilities. The aims of this scoping review were to identify the current state of the science, determine knowledge gaps, and review research methods (Munn et al., Citation2018). Additionally, a scoping review may provide directions for future research (Colquhoun et al., Citation2014) and suggest clinical implications. This review aimed to explore variables related to the participants, the goals and types of AAC interventions, and outcomes as well as the certainty of evidence.
Method
Guidelines for conducting scoping reviews are still emerging (Pham et al., Citation2014), but this review followed the protocol described by Tricco et al. (Citation2018; see Supplemental Material).
Inclusion criteria
Studies were included in this review if they were (a) published in English; (b) published in a peer-reviewed journal; (c) included at least one participant aged 21 years and below who was reported to have diagnoses of concomitant visual, motor, and communication impairments as part of their multiple disabilities that could also include cognitive, hearing, and/or other medical conditions; (d) included implementation of intervention with unaided and/or aided AAC focused on communication, or communication-partner training; and, (e) provided data on outcomes. Studies were excluded if they did not meet inclusion criteria or if there was insufficient information to determine eligibility criteria of individual participants. Studies that incorporated assistive technology but did not address communication were also excluded (e.g. switch activation to control a toy; Lancioni et al., Citation2004). Individual participants were excluded from data analysis if (a) participants were above 21 years of age; (b) no vision status or functional vision was reported; (c) no motor impairment was reported or no information about motor function was provided; or, (d) no communication challenges were reported.
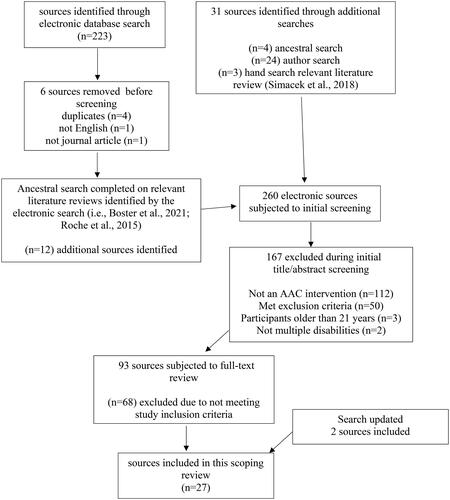
Search methods
This scoping review utilized a combination of search strategies to identify all relevant sources (Tricco et al., Citation2018). presents the flowchart of source identification. The strategy of pearl growing described by Schlosser et al. (Citation2006) for searching the scattered AAC literature was used as a starting point to identify relevant reviews and support identification of relevant search terms and potential citations to explore. An electronic database search was conducted (i.e., ERIC, ProQuest, PsychInfo, PubMed) using the search terms identified in . Then an ancestral search was conducted of sources that qualified for inclusion and existing review studies that were related to the topic or target population (e.g. Boster et al., Citation2021; Roche et al., Citation2015; Simacek et al., Citation2018). In addition, a targeted hand search for studies by authors that frequently populated the electronic database search was completed (e.g. Lancioni, Holyfield, and Stasolla) to identify relevant studies that met the inclusion criteria. Finally, a forward citation search was completed of included sources via title and abstract screening to determine eligibility based on inclusion criteria.
Table 1. Search strategies and yields for electronic database search.
Selection of studies and data extraction
Sources were first screened by reading the title and abstract, using a simple checklist (i.e., multiple disabilities, AAC, intervention) to determine eligibility. Following this, the full text was read, as needed, and the full inclusion criteria were applied. Once all relevant sources were identified, each study was coded by the first author for the following: (a) study design (e.g. single-case experimental research design, group experimental design); (b) participant characteristics (e.g. age, gender, ethnicity, diagnosis, vision, hearing, motor, and communication skills); (c) type of AAC used in intervention (e.g. high-tech, mid-tech, or low-tech); (d) primary intervention purpose (e.g. teach requesting, teach choice-making, and evaluate communicative functions); and (e) primary dependent variable (e.g. percentage correct, number of communication turns). Due to variable information describing participants’ communication abilities, a distinction was not made between presymbolic and symbolic communicators (Grove et al., Citation1999), but this is an important future direction. The coding manual is available upon request.
For the single-case experimental design studies, a gain score was calculated for each participant case and Tau-U was used to calculate the effect size for each participant using an online calculator (Vannest et al., Citation2016). Tau-U estimates nonoverlap between baseline and intervention, can correct for baseline trend, and has high power and sensitivity as an effect size measure for single-case experimental designs (Parker et al., Citation2011). Gain scores (i.e., the difference between the average performance during the final three intervention sessions and the average performance during baseline) are useful as a simple measure of the scope of the improvement overall, especially where learning by participants occurs across multiple sessions (e.g. O'Neill et al., Citation2018). For the one group study included in this review, Cohen’s d was the measure used to determine effect size via an online calculator (Becker, Citation2000).
Additionally, each study was coded for certainty of evidence based on the framework utilized in prior reviews by Schlosser and colleagues (Millar et al., Citation2006; Schlosser & Koul, Citation2015), adapted from Simeonsson and Bailey (Citation1991). This framework was used to assign each source to one of four levels of certainty: conclusive (i.e., strong design such that the outcomes observed were undoubtedly the result of the intervention); preponderant (i.e. only minor flaws in the design such that outcomes were not only possible, but they were more likely to have occurred because of the intervention than not); suggestive (i.e. minor design flaws and inadequate reliability such that the outcomes were plausible as the result of the intervention but uncertainty remains); and inconclusive (i.e., major design flaws and failure to establish experimental control, precluding any conclusions about the outcomes of the intervention). Current research design standards were applied to determine rigor. Existing guidelines for single-case experimental design call for at least five stable baseline measures, interobserver reliability for a minimum of 20% of the data points, and ideally five data points per phase with a minimum of three attempts to show an intervention effect (see Kratochwill et al., Citation2013). However, it is important to note that research standards have continued to evolve over time so many studies included in this review that did not achieve high levels of certainty in this review may have met standards at the time of publication.
Inter-rater reliability of the inclusion and coding of the studies was completed by a trained graduate student in communication sciences and disorders on a randomly selected sample of 18% of the total search results and 20% of the included studies. Inter-rater agreement (i.e. number of agreements divided by the number of agreements plus disagreements, multiplied by 100%) was 100% on the inclusion of studies and 95% on the coding of variables. The original coding, completed by the first author, served as the primary data for the study.
Results
It should be acknowledged that the field of AAC has advanced significantly over time, both in technological advancements as well as in quality of intervention techniques, particularly since the 1980s. There has been increased legislation to protect the rights of individuals with complex communication needs and rapid expansion of clinical AAC assessment and implementation (Hourcade et al., Citation2004). See Hourcade et al. (Citation2004) for a detailed overview of AAC over the decades. Despite these notable clinical advancements, the present review investigated the research on AAC interventions and only found a total of 27 research studies that focused on children and young adults with complex communication needs and simultaneous impairments in vision and motor skills over the years. Of the 27 included studies, 26 were single-case studies and one used a group design. Twenty-five studies reported on direct interventions with participants with multiple disabilities, and two targeted interventions with communication partners. See Appendix C for individual participant characteristics.
AAC interventions implemented with children and young adults with multiple disabilities
summarizes the coded variables across the 25 studies that targeted AAC intervention with children and young adults with multiple disabilities; see Appendix A that presents the coded variables for each of the studies individually. All of the 25 studies that investigated intervention with individuals with multiple disabilities were single case studies and 13 were completed by the same research group with the same first author.
Table 2. Summary of the studies of AAC intervention with individuals with multiple disabilities.
Children and young adults with multiple disabilities and complex communication needs
The 25 studies involved 55 participants with multiple disabilities and complex communication needs. Two participants were involved in multiple studies at different ages (George participated in Lancioni et al. (Citation2007), Lancioni, Singh, et al. (Citation2009), and Lancioni et al. (Citation2011); Joe participated in Lancioni, O'Reilly, Sigafoos, et al. (Citation2006) and Lancioni et al. (Citation2008a), which resulted in 52 unique participants with multiple disabilities that received AAC intervention. Fifteen participants in the 25 studies were not included in the review as they did not meet inclusion criteria.
Participants ranged in age from 3 to 19 years, with the majority between 5 and 17 years (79%; n = 43); only a few studies included individuals 18 years of age or older. The majority of the participants were male (62%; n = 34). Only one study (Ivy et al., Citation2020) reported the race/ethnicity of participants. Cerebral palsy (67%, n = 37) was the most frequent diagnosis reported across participants, with most reporting concomitant seizure disorders and/or neurological disorders (e.g. hydrocephalus and cerebropathy).
Of the 55 participants, 60% (n = 33) were reported to have unspecified visual impairments, 29% (n = 16) were blind, and 11% (n = 6) had cortical visual impairment (CVI). Descriptions of visual function were often vague, ranging from “concerns” with vision (Ivy et al., Citation2020) to “undetermined residual vision” (Lancioni et al., Citation2001) to “severe visual impairment” (e.g. Lancioni, O'Reilly, Sigafoos, et al., Citation2006; Citation2018; Schweigert, Citation1989). Only two studies (Ivy et al., Citation2020; Walker & Wegner, Citation2021), included reports of formal assessment and screening measures for visual impairments.
All participants experienced some level of motor impairment with descriptions suggesting that the vast majority would be categorized at Level 4 and Level 5 on the Gross Motor Function Classification System (Palisano et al., Citation2007). Hearing status was not reported for 62% (n = 36) of participants; of the remaining participants, 20% (n = 11) were reported to have hearing impairments of varying severity, but it was often unclear how hearing status was determined. Only one study reported results of a formal hearing assessment (Lizzy; Ivy et al., Citation2020); and one study reported using informal observation or report (Brianna & Sonja; Cosbey & Johnston, Citation2006).
The majority of participants were reported to have severe to profound cognitive impairments (69%, n = 38); as with vision and hearing, most studies (78%) did not include details of how cognitive status was assessed or determined. All participants were reported to use unaided AAC to express themselves prior to the interventions, including gestures, vocalizations, behaviors, speech approximations, and sign approximations. In addition, 11% (n = 6) of cases used mid-tech AAC (e.g. iTalk2Footnote1 with “yes/no”, Quicktalker SFootnote2), and 4% (n = 2) used high-tech AAC systems (e.g. iPod, NovaChat 8Footnote3) to communicate prior to intervention.
AAC interventions
Of the 25 studies, one targeted unaided AAC (i.e., signs, gestures) during intervention, while six primarily utilized low-tech aided AAC (i.e., adapted Picture Exchange Communication System [PECSFootnote4] with tangible symbols, pictures), three primarily utilized mid-tech AAC speech generating devices (SGDs), and 15 primarily utilized high-tech AAC (i.e., microswitches connected to a computer with speech output; mobile tablet). The majority of the studies provided few, if any, details regarding the characteristics of the AAC systems, such as vocabulary, representations, organization, layout, selection techniques, and output.
Most studies (84%, n = 21) targeted increased requesting or choice-making by participants; only a few (12%, n = 3) targeted social interactions or information sharing. The majority of the AAC interventions were delivered in a highly structured method, often with massed trials outside the context of daily activities. For example, in the study by Lancioni, Singh, et al. (Citation2006), the participant was presented with 30 stimuli per session, across multiple sessions. Very few interventions utilized naturalistic instructional methods within meaningful contexts (16%, n = 4; Cosbey & Johnston, Citation2006, Fleury et al. Citation2019, Holyfield, Caron, et al. Citation2018, Walker & Wegner, Citation2021).
Interventions frequently targeted only a limited number of requests within a single setting and provided access to a very limited range of linguistic concepts. For example, four studies used an adapted PECS to teach participants to request a single preferred item (e.g. beads) when given one adapted tangible symbol (Ali et al., Citation2011; Ivy et al., Citation2014; Citation2020; Snodgrass et al., Citation2013). Nine studies utilized microswitches to teach participants to request preferred items in response to the presentation of stimuli, either with a single switch for a single request (e.g. Schweigert & Rowland, Citation1992) or with more than one microswitch (e.g. Lancioni et al., Citation2007). Microswitches were also utilized in a few studies to teach participants to request social contact or interactions (e.g. Lancioni et al., Citation2008a; Citation2008b; Lancioni, O'Reilly, et al. Citation2009; Mathy-Laikko et al., Citation1989), using a prestored message (e.g. “Please come and play with me,” in Mathy-Laikko; “Can somebody talk to me?” in Lancioni et al., Citation2008b).
Only three studies targeted social functions of communication, sharing information, commenting, or taking turns in interactions (Fleury et al., Citation2019; Holyfield, Caron, et al., Citation2018; Walker & Wegner, Citation2021). Fleury et al. (Citation2019) provided a participant with multiple disabilities with an AAC system with four customized social phrases to share information and ask questions (e.g. “I’m excited,” “Do you like my nails?”) in her natural environments. Holyfield, Caron, et al. (Citation2018) provided participants with mobile technology with visual scene displays (VSDFootnote5) to support social interaction; the researcher followed the participants’ interests and added appropriate vocabulary to the VSDs using just-in-time (JIT) programming to increase the participants’ communicative turns. Walker and Wegner (Citation2021) first taught the participant the necessary visual skills to access an eye-gaze SGD and then taught him to express different communicative functions (e.g. request, make choices, ask questions, comment) using an AAC eye-gaze system.
Dependent variables and outcomes
The intervention studies used a range of measures to evaluate outcomes (e.g. frequency of responses, percentage correct, number of communicative turns), but almost two-thirds (64%; n = 16) of the studies measured frequency of switch activation by participants during the targeted intervention (e.g. requesting, choice-making, respond to preferred stimuli). Gain scores and effect sizes could only be calculated for 13 of the participants across seven different studies. All of these participants demonstrated positive gains as a result of the AAC intervention (e.g. increased frequency of requests in Cosbey & Johnston, Citation2006; increased frequency of communicative turns in Holyfield, Caron, et al., Citation2018; improved accuracy communicating requests via adapted PECS in Ivy et al., Citation2014 and Ivy et al., Citation2020; increased number of switch activations to request caregiver attention in Schweigert, Citation1989). The aggregated mean effect size (Tau U) was calculated by determining the mean effect size across these 13 participants, which was .86 (SD = .23; range = .24–1.0), suggesting that these AAC interventions were highly effective (Vannest & Ninci, Citation2015) with the individuals with multiple disabilities. However, it should be noted that effect sizes could only be calculated for 28% (n = 7) of the intervention studies and there was wide variation as demonstrated by the range of values.
Interventions to train communication partners
Only two studies in this review focused on partner training: a pretest post-test control group design (Holyfield, Light, et al., Citation2018); and a single-case multiple baseline design (Sigafoos et al., Citation1993). Details for these intervention studies can be found in Appendix B.
Children and young adults with multiple disabilities and complex communication needs
A total of three young adults, two male and one female, with multiple disabilities (one in Holyfield, Light, et al., Citation2018, and two in Sigafoos et al., Citation1993) met inclusion criteria in the two studies that provided intervention to train communication partners. Ethnicity of participants was not reported. As with the direct intervention studies, only limited information was provided on the characteristics of these participants. Two had visual impairments that were unspecified, and one was blind; no formal assessments of vision were reported. All three participants were described as “non-ambulatory” (i.e. Level 4 of the GMFCS; Palisano et al., Citation2007). See Appendix B for additional participant details. At the start of the study, all three participants with multiple disabilities utilized unaided AAC to express themselves, including gestures, vocalizations, behaviors, speech approximations, and sign approximations.
Communication partners
In the study by Holyfield, Light, et al. (Citation2018), the communication partners were 24 middle-school peers without disabilities (ages 11–14 years) who attended the same school as the participant with multiple disabilities. In the study by Sigafoos et al. (Citation1993), communication partners were two direct-care staff (age 22–43 years), each paired with one of the two individuals with multiple disabilities in a habilitative program. No additional partner demographics were reported in the studies.
Partner training interventions
Holyfield, Light, et al. (Citation2018) used mobile technology with video VSDs to train the middle school peers to identify and correctly interpret the unaided communicative behaviors of the student with multiple disabilities in order to improve the student’s communication success. Sigafoos et al. (Citation1993) trained the staff in their study to provide increased opportunities for turn-taking and choice-making and evaluated the impact of these strategies during interactions with the two individuals with multiple disabilities.
Intervention outcome measures
Both studies reported positive gains in the use of the targeted strategies by communication partners as a result of partner training. In the study by Holyfield, Light, et al. (Citation2018), the peers in the experimental group who received the training demonstrated increased accuracy identifying the communicative behaviors of the participant with multiple disabilities compared to the control group who did not receive the training. The effect size (Cohen’s d) was large (d=.9), indicating that the partner training was very effective in increasing partner skills. Unfortunately, no measure of any subsequent communication gains from Van (Holyfield, Light, et al., Citation2018) following the partner training was collected to determine changes in communicative behaviors. Both partners in the study by Sigafoos et al. increased the frequency of opportunities that they provided for turn taking and choice making by the participants with multiple disabilities. Tau U was 1.0 for both partners for both skills, suggesting that the partner training was highly effective. The participants with multiple disabilities also demonstrated positive gains in their communication turn taking and choice making as a result of the changes in their communication partners. Tau U for the participants with multiple disabilities ranged from 0.3 to 1.0 across participants and skills, suggesting that the partner training was moderately to highly effective.
Quality of evidence
Of the 25 direct intervention studies in this review, three met the highest standard of certainty; two met the standard of preponderant evidence; 14 provided suggestive evidence; and six studies provided inconclusive evidence, limiting interpretations of the effectiveness of these interventions. Of the two partner training intervention studies, one met the highest standard of evidence and the other was inconclusive.
Discussion
This scoping review provides a number of findings that increase understanding of AAC interventions for children and young adults with multiple disabilities and have important implications for practice and future research. First and most importantly, this review provides evidence that these individuals with multiple disabilities can learn to use AAC to enhance their communication. Furthermore, the evidence indicates that the benefits of AAC extend across a wide range of individuals with multiple disabilities including children as young as three as well as adults, including those with a range of diagnoses (e.g. cerebral palsy and septo-optic dysplasia), and those who present with a wide range of motor, visual, and hearing impairments. Moreover, the evidence shows that those labeled as having severe or profound cognitive impairments who demonstrated limited language and communication prior to intervention also benefited from AAC intervention. Historically, individuals with multiple disabilities have frequently been excluded from AAC and other services and have been isolated from opportunities to participate in society (Mirenda, Citation2015; National Joint Committee for the Communication Needs of Persons with Severe Disabilities, Citation2003). Yet as Brady and colleagues (Citation2016) have argued, everyone has the right to communicate; everyone with complex communication needs can and should have access to appropriate AAC services. This scoping review provides empirical evidence to support these arguments and to debunk the persistent myth that there are prerequisites that must be met for AAC intervention (see Kangas & Lloyd, Citation1988, and Romski & Sevcik, Citation2005, for further arguments debunking these myths). The scoping review also provides encouraging evidence that the benefits of AAC intervention extend to older children, adolescents, and young adults, supporting the argument that “it is never too late” (Beukelman & Light, Citation2020; p. 323) to provide AAC intervention to enhance communication and participation.
These findings of the benefits of AAC intervention are particularly encouraging considering the challenges of service delivery for children and young adults with multiple disabilities. They are at risk of being underestimated (Maes et al., Citation2021) and excluded from social interactions due to severe communication difficulties (Smith et al., Citation2020), which may have negative effects on mental wellbeing and quality of life into adulthood. Furthermore, the presence of intellectual disability may limit comprehension and require adaptations to assessment and intervention techniques to improve outcomes (Chadwick et al., Citation2019). There is a great need for effective AAC intervention that is tailored to their unique and complex needs.
Despite the evidence of the positive benefits of AAC intervention for children and young adults with multiple disabilities, the scoping review also suggests some trends that raise concerns that must be addressed, especially if these trends reflect current practice. First and foremost, it is important to note that only 27 studies were identified over a more than 30-year period, underscoring the overall neglect of the needs of children and young adults with multiple disabilities despite the fact that these individuals face the greatest challenges in communication (Sigafoos et al., Citation2021) and service providers report that they are unsure how to provide effective services (ATIA, Citation2020). Clearly future research is required to determine evidence-based practices.
In addition to the general lack of attention to the needs of children and young adults with multiple disabilities, other trends in the research suggest further problems that must be addressed, including ones related to the age at which AAC interventions are introduced, the goals of these interventions, and the settings. The overwhelming majority of the participants in these studies were over the age of six when AAC intervention was introduced. Communication development begins at birth and AAC intervention should be initiated as early as possible (Cress & Marvin, Citation2003). Early intervention is especially important in the case of children with multiple disabilities as they may require more time and practice to learn communication skills. Since children with multiple disabilities are typically diagnosed at or near birth and are clearly at risk for speech development, these children and their families should immediately be referred for services, especially given the convincing evidence that AAC intervention enhances communication, does not impede speech development, and in fact often enhances speech production for many children, including those with multiple disabilities (e.g. Millar et al., Citation2006; Romski et al., Citation2010). Although this scoping review suggests that it is never too late to provide AAC intervention, by delaying AAC services to age six or later, children with multiple disabilities miss out on many valuable years of language and communication development, negatively impacting long term outcomes. Infants and toddlers with multiple disabilities and their families deserve access to early AAC intervention; future research is required to investigate the effects of this intervention.
The scoping review also revealed that the vast majority of the research with children and young adults with multiple disabilities focused on teaching simple requests or making choices. This result is not surprising as this same tendency has been noted previously with respect to AAC interventions generally (McNaughton & Light, Citation2015). Although learning to express needs and wants is an important communication skill, it is not the only communication skill that should be targeted. According to the first item on the revised Communication Bill of Rights (Brady et al., Citation2016), all individuals with disabilities have the right to interact socially and maintain social relationships. Social communication is especially important because it supports the development of friendships and relationships, and thus has important benefits for overall health and well-being (Cohen, Citation2004). Unfortunately, children with complex communication needs are likely to lack the social experiences necessary to develop these skills (Batorowicz et al., Citation2014). Results of this scoping review suggest that most AAC interventions do not target social interaction to support individuals with multiple disabilities in developing these skills. It is necessary that future interventions focus on improving social communication and experiences.
Interactions that are focused only on expressing needs and wants tend to be highly predictable, are very limited in scope, target a very limited range of vocabulary, and are also limited in duration (Light, Citation1988). If children with multiple disabilities are only taught to make requests, they will lack opportunities to develop reciprocal turn taking, build a rich and varied corpus of language concepts as a foundation for language development, and respond to a wide range of cues in the natural environment; they will lack opportunities to build social relationships and share information with others (Light, Citation1988). It is recommended that AAC interventions with individuals with multiple disabilities extend beyond requesting. Evidence strongly indicates that social interaction skills co-occur with requesting during the very early stages of development for children without disabilities (Crais et al., Citation2004), demonstrating that requesting is not easier to learn than social interaction. Developing skills in both behavior regulation (with a focus on the object or activity) and social interaction (with a focus on the communication partner) are necessary to foster joint attention (coordinating focus on the communication partner and the shared activity) (Prizant et al., Citation2003) required for language development. This scoping review identified few studies that documented effective AAC intervention to increase social interaction and support vocabulary development for individuals with multiple disabilities (e.g. Holyfield, Caron, et al., Citation2018). Although limited in number, these studies provide evidence that children with multiple disabilities can acquire these skills with appropriate supports. Future research is required to investigate the most effective types of AAC interventions to foster these skills.
The scoping review also found that the majority (84%) of the studies with children and young adults with multiple disabilities were conducted by researchers in isolated contexts outside of daily activities. Snell et al. (Citation2010) drew a similar conclusion, noting that most communication intervention research with individuals with severe intellectual and developmental disabilities has been conducted in decontextualized settings, one-on-one with researchers, rather than in natural settings with typical communication partners. Only limited research has been conducted to address the supports that individuals with multiple disabilities require to communicate effectively in their daily lives. Many AAC services are still delivered through “pull out” to isolated settings; there has been limited attention to the supports required in families, schools, and community settings (Foster et al., Citation2023). Future implementation science is required to address effective implementation of AAC in the natural environments of individuals with multiple disabilities.
Although communication is a reciprocal process (where the participants influence each other in the interaction), only two of the 27 studies considered the role of communication partners in the success (or failure) of the communication of children and young adults with multiple disabilities. The lack of attention to partner training is concerning given the repeated calls by AAC users to improve partner competence (Midtlin et al., Citation2015). Prior research has documented the effectiveness of partner training as a means to increase the communication skills of individuals with complex communication needs generally (Kent-Walsh et al., Citation2015). The current scoping review provides specific evidence that interventions to train communication partners of children and young adults with multiple disabilities were both effective and efficient. Furthermore, the scoping review suggests that a range of communication partners may benefit from training, including peers as well as direct-care staff. Unfortunately, none of the studies provided training for parents or siblings despite the central role of families in the lives of individuals with multiple disabilities (Mandak et al., Citation2017). Future research is urgently required to consider supports for families of children with multiple disabilities.
Clinical implications
As evidenced by this scoping review, despite the complexity of supporting children and young adults with multiple disabilities, there is limited information to inform clinical practice for professionals working with those with multiple disabilities and complex communication needs. This review proposes that there are three key clinical takeaways for professionals. Firstly, this review demonstrates that AAC interventions can be very effective for children, adolescents, and young adults with multiple disabilities. Secondly, individuals with multiple disabilities are able to learn several communicative functions. Thirdly, intervention to train communication partners of those with multiple disabilities is highly successful.
Individuals with multiple disabilities and complex communication needs benefit from the provision of AAC and show advantages following intervention. It is important that AAC interventions build functional communication skills for individuals with complex communication needs and teach not just the expression of wants and needs, but also support the development of social communication skills to enable the sharing of information, commenting, and engagement in social etiquette routines (Light & McNaughton, Citation2014). It is recommended that professionals provide AAC intervention to teach children with multiple disabilities effective communication for a range of communicative functions (e.g. express wants and needs, comment, share information, and ask questions) for both current and future needs (Beukelman & Light, Citation2020).
AAC intervention should extend beyond a singular focus on the person with complex communication needs and ought to include communication partners throughout, such as parents, siblings, direct-care staff, and peers (Beukelman & Light, Citation2020). This review illustrates that training communication partners is a strength of intervention and it is recommended that professionals train communication partners to better engage with, and support individuals with complex communication needs.
Limitations
This scoping review is inherently limited by the overall search procedures, databases, and search terms selected, as well as by the inclusion criteria applied. Although this study followed a protocol for conducting scoping reviews (Tricco et al., Citation2018), it is possible that relevant AAC intervention studies were missed if they were not included in the databases searched or unearthed in the ancestral and hand searches, were not available in English, or did not contain the selected search terms. Whilst this study attempted to reduce the chances of missing relevant studies by incorporating multiple search strategies (e.g. electronic database search, ancestral search, and forward citation/author search) it is possible that relevant studies may have still been missed.
The exclusion of grey literature (i.e., unpublished or informally published material that is typically not peer-reviewed; Blackhall & Ker, Citation2007) may have led to publication bias and exaggerated representations of intervention effectiveness (McAuley et al., Citation2000). Despite the acknowledged importance of grey literature, it was excluded from this scoping review because it had not been subjected to rigorous peer-review processes and was not located consistently across online database searches, which can lead to misrepresentation of the grey literature itself. Furthermore, the grey literature that was found in this search was excluded due to limited relevance to the inclusion criteria.
To meet inclusion criteria in this scoping review, studies were required to include at least one participants (0–21 years old) with multiple disabilities and provide sufficient information to determine whether participants had visual, motor, and communication impairments. Of note, only two partner training studies met this inclusion criteria. It is possible that additional communication partner training research studies were not captured by this scoping review due to the focus on AAC intervention, limited age range, and the need for detailed participant description. Studies that may have described individuals with disabilities without utilizing terms such as ‘multiple disabilities’ may have been missed by the search terms in this review. Additionally, partner training studies that focused on interactions or behavior interventions (e.g. Foreman et al., Citation2007) without AAC may have been excluded by the criteria in this review. Future research is needed to investigate the effectiveness of training communication partners of those with multiple disabilities.
Future research considerations
Clearly future research is required to guide practice and improve outcomes for children and young adults with multiple disabilities. The following section outlines some considerations for future research. Specifically, this research should: (a) study the effectiveness of AAC interventions (especially early AAC intervention) not just to request, but also to promote social interaction and build language skills; (b) identify partner supports to enhance the communication of individuals with multiple disabilities; and, (c) investigate barriers and supports for implementing AAC interventions successfully within the natural environments of individuals with multiple disabilities. No single AAC intervention will meet the needs and skills of all individuals with multiple disabilities, across all settings and communication partners, in order to attain communicative competence; rather the challenge is to determine which AAC interventions work best for which individuals to attain which goals under which conditions. In order to meet this challenge, future research must be both rigorous and relevant, and must include robust descriptions of the participants with multiple disabilities, their environments (settings and communication partners), and the AAC intervention.
A number of authors have issued calls for more rigorous scientific methods in AAC research (e.g. Ganz et al., Citation2023; Kent-Walsh & Binger, Citation2018; Romski & Sevcik, Citation2018). Results of this scoping review support these calls: of the 27 studies identified in this scoping review, only six (22%) met current methodological standards such that the certainty of the evidence was either conclusive or preponderant; the majority of the studies (78%) had design flaws (e.g. limitations in treatment fidelity, reliability of the measures, number of observations at baseline or intervention) that made it difficult to draw conclusions with any certainty. Future AAC research must be rigorous in order to advance knowledge and improve practice. Although rigor is necessary, it is by no means sufficient on its own. Future research must also be relevant such that results are useful in the real world lives of individuals with multiple disabilities. In 2008, Granlund and colleagues (Granlund et al., Citation2008) highlighted the lack of research investigating outcomes of AAC intervention in the everyday lives of individuals with complex communication needs, leaving these authors to conclude that, in order to attain successful outcomes, the AAC field needs to focus not just on evidence-based practice, but also on practice-based evidence. Results of this scoping review suggest that this problem persists almost 15 years later.
One key way to ensure relevance is to actively involve individuals with multiple disabilities, their families, and other stakeholders in meaningful ways in all aspects of AAC research (Blackstone et al., Citation2007). AAC users want a voice at the table (Goldman et al., Citation2021). They are valuable sources of input regarding AAC intervention research and implementation (Rackensperger et al., Citation2005) and their voices should not go unheard (Klein, Citation2017). Researchers should seek input from families and other stakeholders at all steps of the research and intervention process through focus groups, interviews, surveys, and informal discussions (Heiden & Saia, Citation2021). Researchers also need to explore effective strategies to empower beginning communicators with multiple disabilities to provide input to set priorities; Beukelman and Light (Citation2020) suggested methods such as offering choices, using photographs, and carefully observing the affect of individuals with multiple disabilities to determine their priorities.
As noted earlier, the population of individuals with disabilities is a heterogeneous one that includes individuals of different races and ethnicities with a wide range of needs and skills. Unfortunately, race/ethnicity was not reported for 95% of the participants in this scoping review. This finding is concerning given the general lack of research focused on individuals with complex communication needs from culturally and linguistically diverse backgrounds, and the preliminary evidence of racial disparities in AAC intervention provided to Black children compared to their white peers (Pope et al., Citation2022). This scoping review also found that very few studies provided detailed information on participant needs and skills: for example, specifics regarding visual function were not reported for 60% of participants, hearing status was not reported for 64%, and cognition for 74%. Although, it should be acknowledged that conducting valid and reliable assessments with this population may be challenging due to their sensory, cognitive, and motor impairments (Crawford et al., Citation2018); there is a desperate need for future research to determine effective methods of ascertaining the needs and skills of those with multiple disabilities (Maes et al., Citation2021). Most studies also failed to consider the characteristics of the typical communication partners and environments of the individuals with multiple disabilities, instead electing to implement AAC intervention in isolated settings with the researcher. Finally, the majority of the studies provided limited information regarding the AAC systems implemented (e.g. limited information on vocabulary, representations, organization, layout, selection, and output) and yet the research clearly demonstrates that each of these variables may impact performance. Future research should consider the needs of individuals with multiple disabilities from culturally and linguistically diverse backgrounds to reduce racial disparities in AAC services. Future research should also explore improved assessment techniques to provide better descriptions of the needs and skills of individuals with multiple disabilities and should also provide more detailed descriptions of communication partners and environments as well as the AAC systems and instructional procedures implemented. All of this information is essential to determine which interventions work best for which individuals under which conditions – a question that is critically important to guide clinical practice.
Conclusion
Children and young adults with multiple disabilities present with the most complex communication needs, but there is limited information to guide clinicians in AAC interventions. However, the available research evidence consistently indicates that those with multiple disabilities can successfully learn and use various AAC systems to make simple requests and communicate choices. Unfortunately, little is known about AAC interventions to improve social communication and foster language development in natural contexts with this population. Limited research to date has focused on training communication partners to support the communication of individuals with multiple disabilities, but the existing research indicates that partner training is highly effective and efficient. There is an urgent need for future research to investigate AAC interventions (both direct intervention and partner training) to support social interactions, enhance language development, and maximize participation in daily environments for individuals with multiple disabilities with a wide range of needs and skills, including those from culturally and linguistically diverse backgrounds. Researchers are advised to follow current research reporting guidelines to maximize the certainty of evidence; to involve individuals with multiple disabilities, their families, and other stakeholders to ensure the relevance of their research; and to provide detailed descriptions of participants, environments, communication partners, and AAC interventions to support the translation of research results to practice.
Supplemental Material
Download MS Word (93.9 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
Notes
1 iTalk2 is a mid-tech AAC system with two speech output buttons. Available from AbleNet https://www.ablenetinc.com/italk2/.
2 QuickTalker S is a speech output button available from AbleNet https://www.ablenetinc.com
3 Novachat 8 is a high-tech speech-generating tablet available from Saltillo https://saltillo.com
4 Picture Exchange Communication System (PECS) is a communication system developed in the USA, based on principles of applied behavioral analysis. https://pecsusa.com/pecs/.
5 Visual Scene Displays (VSD) are a type of AAC display that embeds language concepts into photographs. Hotspots are created on the photograph or video and language is embedded. https://play.google.com/store/apps/details?id=invotek.apps.easyvsd&hl=en_US&gl=US
References
- *Asterix denotes studies that were included in the scoping review analysis.
- *Ali, E., MacFarland, S. Z., & Umbreit, J. (2011). Effectiveness of combining tangible symbols with the picture exchange communication system to teach requesting skills to children with multiple disabilities including visual impairment. Education and Training in Autism and Developmental Disabilities, 46(3), 425–435. https://www.jstor.org/stable/23880596
- Assistive Technology Industrial Association and Human Service Institute (ATIA). (2020). 2019 ATIA survey: Training needs in augmentative and alternative communication. https://www.atia.org/wp-content/uploads/2020/10/ATIA-Survey-White-Paper-Final-2020820_508.pdf
- Batorowicz, B., Campbell, F., von Tetzchner, S., King, G., & Missiuna, C. (2014). Social participation of school-aged children who use communication aids: The views of children and parents. Augmentative and Alternative Communication (Baltimore, Md.: 1985), 30(3), 237–251. https://doi.org/10.3109/07434618.2014.940464
- Becker, L. A. (2000). Effect size calculators. University of Colorado, Colorado Springs, CO. https://lbecker.uccs.edu
- Beukelman, D., & Light, J. (2020). Augmentative & alternative communication: Supporting children & adults with complex communication needs (5th ed.). Paul H. Brookes.
- Blackhall, K., & Ker, K. (2007). Finding studies for inclusion in systematic reviews for interventions for injury prevention – importance of grey and unpublished literature. Injury Prevention: Journal of the International Society for Child and Adolescent Injury Prevention, 13(5), 359–359. https://doi.org/10.1136/ip.2007.017020
- Blackstone, S. W., Williams, M. B., & Wilkins, D. P. (2007). Key principles underlying research and practice in AAC. Augmentative and Alternative Communication (Baltimore, Md. : 1985)), 23(3), 191–203. https://doi.org/10.1080/07434610701553684
- Boster, J. B., McCarthy, J. W., Brown, K., Spitzley, A. M., & Blackstone, S. W. (2021). Creating a path for systematic investigation of children with cortical visual impairment who use augmentative and alternative communication. American Journal of Speech-Language Pathology, 30(4), 1880–1893. https://doi.org/10.1044/2021_AJSLP-20-00203
- Brady, N. C., Bruce, S., Goldman, A., Erickson, K., Mineo, B., Ogletree, B. T., Paul, D., Romski, M. A., Sevcik, R., Siegel, E., Schoonover, J., Snell, M., Sylvester, L., & Wilkinson, K. (2016). Communication services and supports for individuals with severe disabilities: Guidance for assessment and intervention. American Journal on Intellectual and Developmental Disabilities, 121(2), 121–138. https://doi.org/10.1352/1944-7558-121.2.121
- Center for Disease Control and Prevention (CDC). (2020, September 16). Common barriers to participation experienced by people with disabilities. https://www.cdc.gov/ncbddd/disabilityandhealth/disability-barriers.html#ref
- Center for Disease Control and Prevention (CDC). (2022, May 2). Individuals with disabilities education act (IDEA) services. https://www.cdc.gov/ncbddd/cp/treatment.html
- Chadwick, D., Buell, S., & Goldbart, J. (2019). Approaches to communication assessment with children and adults with profound intellectual and multiple disabilities. Journal of Applied Research in Intellectual Disabilities: Jarid, 32(2), 336–358. https://doi.org/10.1111/jar.12530
- Cohen, S. (2004). Social Relationships and Health. The American Psychologist, 59(8), 676–684. https://doi.org/10.1037/0003-066X.59.8.676
- Colquhoun, H. L., Levac, D., O'Brien, K. K., Straus, S., Tricco, A. C., Perrier, L., Kastner, M., & Moher, D. (2014). Scoping reviews: Time for clarity in definition, methods, and reporting. Journal of Clinical Epidemiology, 67(12), 1291–1294. https://doi.org/10.1016/j.jclinepi.2014.03.013
- *Cosbey, J. E., & Johnston, S. (2006). Using a single-switch voice output communication aid to increase social access for children with severe disabilities in inclusive classrooms. Research and Practice for Persons with Severe Disabilities, 31(2), 144–156. https://doi.org/10.1177/154079690603100207
- Crais, E., Douglas, D. D., & Campbell, C. C. (2004). The intersection of the development of gestures and intentionality. Journal of Speech, Language, and Hearing Research: Jslhr, 47(3), 678–694. https://doi.org/10.1044/1092-4388(2004/052)
- Crawford, J. R., Parker, D. E., & McKinlay, W. (2018). A handbook of neuropsychological assessment. Routledge.
- Cress, C. J., & Marvin, C. A. (2003). Common questions about AAC services in early intervention. Augmentative and Alternative Communication, 19(4), 254–272. https://doi.org/10.1080/07434610310001598242
- *Fleury, A., Wu, G., & Chau, T. (2019). A wearable fabric-based speech-generating device: System design and case demonstration. Disability and Rehabilitation. Assistive Technology, 14(5), 434–444. https://doi.org/10.1080/17483107.2018.1462860
- Foreman, P., Arthur‐Kelly, M., & Pascoe, S. (2007). The impact of partner training on the communicative involvement of students with multiple and severe disability in special schools. Journal of Intellectual & Developmental Disability, 32(4), 233–247. https://doi.org/10.1080/13668250701654417
- Foster, S. T., Brown, M. T., & Michels, C. M. (2023). The classroom profile for integrated communication supports: A framework to support augmentative and alternative communication coaching services in the school setting. Perspectives of the ASHA Special Interest Groups, 8(2), 358–371. https://doi.org/10.1044/2022_PERSP-22-00005
- Ganz, J. B., Pustejovsky, J. E., Reichle, J., Vannest, K. J., Foster, M., Pierson, L. M., Wattanawongwan, S., Fuller, M. C., Haas, A. N., Sallese, M. R., Smith, S. D., & Yllades, V. (2023). A case for increased rigor in AAC research: A methodological quality review. Education and Training in Autism and Developmental Disabilities, 58(1), 3–21.
- Goldman, A., Jackson, D., Kannan, K., Canter, C., Klein, C., Marshall, S., McNaughton, D., Paul, D., Rackensperger, T., Soto, G., & Zangari, C. (2021). Training needs in augmentative and alternative communication: A virtual roundtable discussion. Assistive Technology Outcomes & Benefits, 15(1), 1–28.
- Granlund, M., Björck-Akesson, E., Wilder, J., & Ylvén, R. (2008). AAC interventions for children in a family environment: Implementing evidence in practice. Augmentative and Alternative Communication (Baltimore, Md.: 1985), 24(3), 207–219. https://doi.org/10.1080/08990220802387935
- Grove, N., Bunning, K., Porter, J., & Olsson, C. (1999). See what I mean: Interpreting the meaning of communication by people with severe and profound intellectual disabilities. Journal of Applied Research in Intellectual Disabilities, 12(3), 190–203. https://doi.org/10.1111/j.1468-3148.1999.tb00076.x
- Harding, C., Lindsay, G., O’Brien, A., Dipper, L., & Wright, J. (2011). Implementing AAC with children with profound and multiple learning disabilities: A study in rationale underpinning intervention. Journal of Research in Special Educational Needs, 11(2), 120–129. https://doi.org/10.1111/j.1471-3802.2010.01184.x
- Heiden, T., Saia, T. (2021). Engaging stakeholders for research impact. American Institutes for Research. https://ktdrr.org/products/KTDRR-Stakeholder-Engagement-Brief-508.pdf
- *Holyfield, C., Light, J., Drager, K., McNaughton, D., & Gormley, J. (2018). Effect of AAC partner training using video on peers’ interpretation of the behaviors of presymbolic middle-schoolers with multiple disabilities. Augmentative and Alternative Communication (Baltimore, Md. : 1985)), 34(4), 301–310. https://doi.org/10.1080/07434618.2018.1508306
- *Holyfield, C., Caron, J. G., Drager, K., & Light, J. (2018). Effect of mobile technology featuring visual scene displays and just-in-time programming on communication turns by preadolescent and adolescent beginning communicators. International Journal of Speech-Language Pathology, 21(2), 201–211. https://doi.org/10.1080/17549507.2018.1441440
- Horn, E., & Kang, J. (2012). Supporting young children with multiple disabilities: What do we know and what do we still need to learn? Topics in Early Childhood Special Education, 31(4), 241–248. https://doi.org/10.1177/0271121411426487
- Hourcade, J., Everhart Pilotte, T., West, E., & Parette, P. (2004). A history of augmentative and alternative communication for individuals with severe and profound disabilities. Focus on Autism and Other Developmental Disabilities, 19(4), 235–244. https://doi.org/10.1177/10883576040190040501
- Individuals with Disabilities Education Act (IDEA). (2018). Sec. 300.8 (c) (7). Retrieved November 25, 2023, from https://sites.ed.gov/idea/regs/b/a/300.8/c/7/
- *Ivy, S., Hatton, D., & Hooper, J. D. (2014). Using the picture exchange communication system with students with visual impairment. Exceptional Children, 80(4), 474–488. https://doi.org/10.1177/0014402914527239
- *Ivy, S., Robbins, A., & Kerr, M. G. (2020). Adapted picture exchange communication system using tangible symbols for young learners with significant multiple disabilities. Augmentative and Alternative Communication, 36(3), 166–178. https://doi.org/10.1080/07434618.2020.1826051
- Jones, T. W., Jones, J. K., & Ewing, K. M. (2006). Students with multiple disabilities. Deaf learners: Developments in curriculum and instruction, 127–143.
- Kangas, K., & Lloyd, L. (1988). Early cognitive skills as prerequisites to augmentative and alternative communication use: What are we waiting for? Augmentative and Alternative Communication, 4(4), 211–221. https://doi.org/10.1080/07434618812331274817
- Kent-Walsh, J., & Binger, C. (2018). Methodological advances, opportunities, and challenges in AAC research. Augmentative and Alternative Communication (Baltimore, Md. : 1985), 34(2), 93–103. https://doi.org/10.1080/07434618.2018.1456560
- Kent-Walsh, J., Murza, K. A., Malani, M. D., & Binger, C. (2015). Effects of communication partner instruction on the communication of individuals using AAC: A meta-analysis. Augmentative and Alternative Communication (Baltimore, Md.: 1985), 31(4), 271–284. https://doi.org/10.3109/07434618.2015.1052153
- Klein, C. (2017). Communication and developing relationships for people who use augmentative and alternative communication. Assistive Technology Outcomes & Benefits, 11(1), 58–65.
- Kratochwill, T., Hitchcock, J., Horner, R., Levin, J., Odom, S., Rindskopf, D., & Shadish, W. (2013). Single-case intervention research design standards. Remedial and Special Education, 34(1), 26–38. https://doi.org/10.1177/0741932512452794
- *Lancioni, G. E., O'Reilly, M. F., Oliva, D., & Coppa, M. M. (2001). Using multiple microswitches to promote different responses in children with multiple disabilities. Research in Developmental Disabilities, 22(4), 309–318. https://doi.org/10.1016/S0891-4222(01)00074-9
- Lancioni, G., Singh, N., O’Reilly, M., & Oliva, D. (2003). Extending microswitch-based programs for people with multiple disabilities: Use of words and choice opportunities. Research in Developmental Disabilities, 24(2), 139–148. https://doi.org/10.1016/S0891-4222(03)00015-5
- *Lancioni, G. E., Singh, N. N., O'Reilly, M. F., & Oliva, D. (2004). A microswitch program including words and choice opportunities for students with multiple disabilities. Perceptual and Motor Skills, 98(1), 214–222. https://doi.org/10.2466/pms.98.1.214-222
- Lancioni, G. E., O'Reilly, M. F., Sigafoos, J., Singh, N. N., Oliva, D., & Basili, G. (2004). Enabling a person with multiple disabilities and minimal motor behaviour to control environmental stimulation with chin movements. Disability and Rehabilitation, 26(21-22), 1291–1294. https://doi.org/10.1080/09638280412331280316
- *Lancioni, G. E., O'Reilly, M. F., Sigafoos, J., Singh, N. N., Oliva, D., & Baccani, S. (2006). Teaching ‘yes’ and ‘no’ responses to children with multiple disabilities through a program including microswitches linked to a vocal output device. Perceptual and Motor Skills, 102(1), 51–61. https://doi.org/10.2466/pms.102.1.51-61
- Lancioni, G. E., O’Reilly, M. F., Singh, N. N., Oliva, D., Baccani, S., Severini, L., & Groeneweg, J. (2006). Micro-switch programmes for students with multiple disabilities and minimal motor behaviour: Assessing response acquisition and choice. Pediatric Rehabilitation, 9(2), 137–143. https://doi.org/10.1080/13638490500235466
- *Lancioni, G. E., Singh, N. N., O'Reilly, M. F., Sigafoos, J., Oliva, D., & Antonucci, M. (2006). A microswitch-based programme to enable a boy with multiple disabilities and minimal motor behaviour to choose among environmental stimuli. Disability and Rehabilitation. Assistive Technology, 1(3), 205–208. https://doi.org/10.1080/17483100612331392934
- *Lancioni, G. E., Singh, N. N., O'Reilly, M. F., Sigafoos, J., Oliva, D., & Baccani, S. (2007). Enabling students with multiple disabilities to request and choose among environmental stimuli through microswitch and computer technology. Research in Developmental Disabilities, 28(1), 50–58. https://doi.org/10.1016/j.ridd.2005.12.001
- *Lancioni, G. E., O'Reilly, M. F., Singh, N. N., Sigafoos, J., Oliva, D., & Severini, L. (2008a). Enabling two persons with multiple disabilities to access environmental stimuli and ask for social contact through microswitches and a VOCA. Research in Developmental Disabilities, 29(1), 21–28. https://doi.org/10.1016/j.ridd.2006.10.001
- *Lancioni, G. E., O'Reilly, M. F., Singh, N. N., Sigafoos, J., Oliva, D., & Severini, L. (2008b). Three persons with multiple disabilities accessing environmental stimuli and asking for social contact through microswitch and VOCA technology. Journal of Intellectual Disability Research: Jidr, 52(Pt 4), 327–336. https://doi.org/10.1111/j.1365-2788.2007.01024.x
- *Lancioni, G. E., O'Reilly, M. F., Singh, N. N., Sigafoos, J., Didden, R., Oliva, D., Campodonico, F., de Pace, C., Chiapparino, C., & Groeneweg, J. (2009). Persons with multiple disabilities accessing stimulation and requesting social contact via microswitch and VOCA devices: New research evaluation and social validation. Research in Developmental Disabilities, 30(5), 1084–1094. https://doi.org/10.1016/j.ridd.2009.03.004
- *Lancioni, G. E., Singh, N. N., O’Reilly, M. F., Sigafoos, J., Oliva, D., & Cingolani, E. (2009). Students with multiple disabilities using technology-based programs to choose and access stimulus events alone or with caregiver participation. Research in Developmental Disabilities, 30(4), 689–701. https://doi.org/10.1016/j.ridd.2008.09.002
- *Lancioni, G., O'Reilly, M., Singh, N., Sigafoos, J., Oliva, D., Smaldone, A., La Martire, M., Navarro, J., Spica, A., & Chirico, M. (2011). Technology-assisted programs for promoting leisure or communication engagement in two persons with pervasive motor or multiple disabilities. Disability and Rehabilitation. Assistive Technology, 6(2), 108–114. https://doi.org/10.3109/17483107.2010.496524
- *Lancioni, G., O’Reilly, M., Sigafoos, J., Campodonico, F., Perilli, V., Alberti, G., Ricci, C., & Miglino, O. (2018). A modified smartphone-based program to support leisure and communication activities in people with multiple disabilities. Advances in Neurodevelopmental Disorders, 2(3), 293–299. https://doi.org/10.1007/s41252-017-0047-z
- Light, J. (1988). Interaction involving individuals using augmentative and alternative communication systems: State of the art and future directions. Augmentative and Alternative Communication, 4(2), 66–82. https://doi.org/10.1080/07434618812331274657
- Light, J., & McNaughton, D. (2014). Communicative competence for individuals who require augmentative and alternative communication: A new definition for a new era of communication? Augmentative and Alternative Communication (Baltimore, Md. : 1985)), 30(1), 1–18. https://doi.org/10.3109/07434618.2014.885080
- Mandak, K., O'Neill, T., Light, J., & Fosco, G. M. (2017). Bridging the gap from values to actions: A family systems framework for family-centered AAC services. Augmentative and Alternative Communication (Baltimore, Md.: 1985)), 33(1), 32–41. https://doi.org/10.1080/07434618.2016.1271453
- Maes, B., Nijs, S., Vandesande, S., Van Keer, I., Arthur‐Kelly, M., Dind, J., Goldbart, J., Petitpierre, G., & Van Der Putten, A. (2021). Looking back, looking forward: Methodological challenges and future directions in research on persons with profound intellectual and multiple disabilities. Journal of Applied Research in Intellectual Disabilities: JARID, 34(1), 250–262. https://doi.org/10.1111/jar.12803
- *Mathy-Laikko, P., Iacono, T., Ratcliff, A., Villarruel, F., Yoder, D., & Vanderheiden, G. (1989). Teaching a child with multiple disabilities to use a tactile augmentative communication device. Augmentative and Alternative Communication, 5(4), 249–256. https://doi.org/10.1080/07434618912331275306
- McAuley, L., Pham, B., Tugwell, P., & Moher, D. (2000). Does the inclusion of grey literature influence estimates of intervention effectiveness reported in meta-analyses? Lancet (London, England), 356(9237), 1228–1231. https://doi.org/10.1016/S0140-6736(00)02786-0
- McNaughton, D., & Light, J. (2015). What We Write about When We Write About AAC: The Past 30 Years of Research and Future Directions. Augmentative and Alternative Communication (Baltimore, Md.: 1985)), 31(4), 261–270. https://doi.org/10.3109/07434618.2015.1099736
- Midtlin, H., Næss, K., Taxt, T., & Karlsen, A. (2015). What communication strategies do AAC users want their communication partners to use? A preliminary study. Disability and Rehabilitation, 37(14), 1260–1267. https://doi.org/10.3109/09638288.2014.961659
- Millar, D., Light, J., & Schlosser, R. (2006). The impact of augmentative and alternative communication intervention on the speech production of individuals with developmental disabilities: A research review. Journal of Speech, Language, and Hearing Research: JSLHR, 49(2), 248–264. https://doi.org/10.1044/1092-4388(2006/021)
- Mirenda, P. (2015). Considerations in developing and acquiring communication aids. In J. Downing, A. Hanreddy, & K. Peckham-Hardin (Eds.). Teaching communication skills to students with severe disabilities (3rd ed.) (pp. 137–162). Paul H. Brookes Publishing Co.
- Munn, Z., Peters, M., Stern, C., Tufanaru, C., McArthur, A., & Aromataris, E. (2018). Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Medical Research Methodology, 18(1), 143. https://doi.org/10.1186/s12874-018-0611-x
- National Joint Committee for the Communication Needs of Persons with Severe Disabilities. (2003). Position statement on access to communication services and supports: Concerns regarding the application of restrictive “eligibility” policies [Position Statement]. Retrieved from www.asha.org/njc
- O'Neill, T., Light, J., & Pope, L. (2018). Effects of interventions that include aided augmentative and alternative communication input on the communication of individuals with complex communication needs: A meta-analysis. Journal of Speech, Language, and Hearing Research: JSLHR, 61(7), 1743–1765. https://doi.org/10.1044/2018_JSLHR-L-17-0132
- Palisano, R., Rosenbaum, P., Bartlett, D., & Livingston, M. (2007). GMFCS-E&R. CanChild Centre for Childhood Disability Research, McMaster University, 200(7).
- Parker, R., Vannest, K., Davis, J., & Sauber, S. (2011). Combining Nonoverlap and Trend for Single-Case Research: Tau-U. Behavior Therapy, 42(2), 284–299. https://doi.org/10.1016/j.beth.2010.08.006
- Pawliuk, C., Brown, H. L., Widger, K., Dewan, T., Hermansen, A.-M., Grégoire, M.-C., Steele, R., & Siden, H., (H.). (2021). Optimising the process for conducting scoping reviews. BMJ Evidence-Based Medicine, 26(6), 312–312. https://doi.org/10.1136/bmjebm-2020-111452
- Pham, M. T., Rajić, A., Greig, J. D., Sargeant, J. M., Papadopoulos, A., & McEwen, S. A. (2014). A scoping review of scoping reviews: Advancing the approach and enhancing the consistency. Research Synthesis Methods, 5(4), 371–385. https://doi.org/10.1002/jrsm.1123
- Pope, L., Light, J., & Franklin, A. (2022). Black children with developmental disabilities receive less augmentative and alternative communication intervention than their white peers: Preliminary evidence of racial disparities from a secondary data analysis. American Journal of Speech-Language Pathology, 31(5), 2159–2174. https://doi.org/10.1044/2022_AJSLP-22-00079
- Prizant, B. M., Wetherby, A. M., Rubin, E., & Laurent, A. C. (2003). The SCERTS model: A transactional, family-centered approach to enhancing communication and socioemotional abilities of children with autism spectrum disorder. Infants & Young Children, 16(4), 296–316. https://doi.org/10.1097/00001163-200310000-00004
- Rackensperger, T., Krezman, C., Mcnaughton, D., Williams, M. B., & D'Silva, K. (2005). When I first got it, I wanted to throw it off a cliff”: The challenges and benefits of learning AAC technologies as described by adults who use AAC. Augmentative and Alternative Communication, 21(3), 165–186. https://doi.org/10.1080/07434610500140360
- Roche, L., Sigafoos, J., Lancioni, G. E., O'Reilly, M. F., & Green, V. A. (2015). Microswitch technology for enabling self-determined responding in children with profound and multiple disabilities: A systematic review. Augmentative and Alternative Communication (Baltimore, Md. : 1985)), 31(3), 246–258. https://doi.org/10.3109/07434618.2015.1024888
- Romski, M. A., & Sevcik, R. (2005). Augmentative communication and early intervention: Myths and realities. Infants & Young Children, 18(3), 174–185. https://doi.org/10.1097/00001163-200507000-00002
- Romski, M. A., Sevcik, R., Adamson, L. B., Cheslock, M., Smith, A., Barker, R. M., & Bakeman, R. (2010). Randomized comparison of augmented and nonaugmented language interventions for toddlers with developmental delays and their parents. Journal of Speech, Language, and Hearing Research: Jslhr, 53(2), 350–364. https://doi.org/10.1044/1092-4388(2009/08-0156)
- Romski, M. A., & Sevcik, R. (2018). The complexities of AAC intervention research: Emerging trends to consider. Augmentative and Alternative Communication (Baltimore, Md.: 1985)), 34(4), 258–264. https://doi.org/10.1080/07434618.2018.1526319
- Roush, J., Holcomb, M. A., Roush, P. A., & Escolar, M. L. (2004). When hearing loss occurs with multiple disabilities. Seminars in Hearing, 25(04), 333–345. https://doi.org/10.1055/s-2004-836135
- Schlosser, R., & Koul, R. (2015). Speech output technologies in interventions for individuals with autism spectrum disorders: A scoping review. Augmentative and Alternative Communication (Baltimore, Md. : 1985), 31(4), 285–309. https://doi.org/10.3109/07434618.2015.1063689
- Schlosser, R., Wendt, O., Bhavnani, S., & Nail-Chiwetalu, B. (2006). Use of information-seeking strategies for developing systematic reviews and engaging in evidence-based practice: The application of traditional and comprehensive Pearl Growing. A review. International Journal of Language & Communication Disorders, 41(5), 567–582. https://doi.org/10.1080/13682820600742190
- *Schweigert, P. (1989). Use of microswitch technology to facilitate social contingency awareness as a basis for early communication skills. Augmentative and Alternative Communication, 5(3), 192–198. https://doi.org/10.1080/07434618912331275196
- *Schweigert, P., & Rowland, C. (1992). Early communication and microtechnology: Instructional sequence and case studies of children with severe multiple disabilities. Augmentative and Alternative Communication, 8(4), 273–286. https://doi.org/10.1080/07434619212331276313
- *Sigafoos, J., Roberts, D., Couzens, D., & Kerr, M. (1993). Providing opportunities for choice-making and turn-taking to adults with multiple disabilities. Journal of Developmental and Physical Disabilities, 5(4), 297–310. https://doi.org/10.1007/BF01046387
- Sigafoos, J., Roche, L., & Tait, K. (2021). Challenges in providing AAC intervention to people with profound intellectual and multiple disabilities. In B. T. Ogletree (Ed.), Augmentative and alternative communication: Challenges and solutions (pp. 229–252). Plural Publishing.
- Simacek, J., Pennington, B., Reichle, J., & Parker-McGowan, Q. (2018). Aided AAC for people with severe to profound and multiple disabilities: A systematic review of interventions and treatment intensity. Advances in Neurodevelopmental Disorders, 2(1), 100–115. https://doi.org/10.1007/s41252-017-0050-4
- Simeonsson, R. J., & Bailey, D. B. (1991). Evaluating programme impact: Levels of certainty. In D. M. Mitchell & R. I. Brown (Eds.), Early Intervention Studies for Young Children with Special Needs. (pp. 280–296). Springer US. https://doi.org/10.1007/978-1-4899-3292-1_11
- Smith, M., Manduchi, B., Burke, É., Carroll, R., McCallion, P., & McCarron, M. (2020). Communication difficulties in adults with Intellectual Disability: Results from a national cross-sectional study. Research in Developmental Disabilities, 97, 103557. https://doi.org/10.1016/j.ridd.2019.103557
- Snell, M., Brady, N., McLean, L., Ogletree, B., Siegel, E., Sylvester, L., Mineo, B., Paul, D., Romski, M., & Sevcik, R. (2010). Twenty years of communication intervention research with individuals who have severe intellectual and developmental disabilities. American Journal on Intellectual and Developmental Disabilities, 115(5), 364–380. https://doi.org/10.1352/1944-7558-115-5.364
- *Snodgrass, M. R., Stoner, J. B., & Angell, M. E. (2013). Teaching conceptually referenced core vocabulary for initial augmentative and alternative communication. Augmentative and Alternative Communication (Baltimore, Md.: 1985), 29(4), 322–333. https://doi.org/10.3109/07434618.2013.848932
- Stasolla, F., & Perilli, V. (2015). Microswitch-based programs (MBP) to promote communication, occupation, and leisure skills for children with multiple disabilities: A literature overview. In Silton, N.R. Recent advances in assistive technologies to support children with developmental disorders. IGI Global. https://doi.org/10.4018/978-1-4666-8395-2.ch009
- Trabacca, A., Vespino, T., Di Liddo, A., & Russo, L. (2016). Multidisciplinary rehabilitation for patients with cerebral palsy: Improving long-term care. Journal of Multidisciplinary Healthcare, 9, 455–462. https://doi.org/10.2147/JMDH.S88782
- Tricco, A. C., Lillie, E., Zarin, W., O'Brien, K. K., Colquhoun, H., Levac, D., Moher, D., Peters, M. D. J., Horsley, T., Weeks, L., Hempel, S., Akl, E. A., Chang, C., McGowan, J., Stewart, L., Hartling, L., Aldcroft, A., Wilson, M. G., Garritty, C., … Straus, S. E. (2018). PRISMA extension for scoping reviews (PRISMAScR): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. https://doi.org/10.7326/M18-0850
- Vannest, K. J., & Ninci, J. (2015). Evaluating intervention effects in single-case research designs. Journal of Counseling & Development, 93 (4), 403–411. https://doi.org/10.1002/jcad.12038
- Vannest, K. J., Parker, R. I., Gonen, O., Adiguzel, T. (2016). Single case research: Web based calculators for SCR analysis. (Version 2.0) [Web-based application]. College Station, TX: Texas A&M University. www.singlecaseresearch.org
- *Walker, C., & Wegner, J. (2021). Eyegaze access and cortical visual impairment: A case study. Assistive Technology Outcomes and Benefits, 15, 24.
Appendix A
Table A1. Summary of coded variables: AAC intervention studies with individuals with multiple disabilities.
Appendix B
Table B1. Summary of coded variables: Partner training intervention studies.
Appendix C
Table C1. Demographic table of all individual participants.