Abstract
Background
Out-of-hospital cardiac arrest (OHCA) remains one of the most common causes of death. There is a scarcity of evidence concerning the prevalence of bacteraemia in cardiac arrest patients presenting to the Emergency Department (ED). We aimed to determine the prevalence of bacteraemia in OHCA patients presenting to the ED, as well as study the association between bacteraemia and in-hospital mortality in OHCA patients. In addition, the association between antibiotic use during resuscitation and in-hospital mortality was examined.
Methods and results
This was a study of 200 adult OHCA patients who presented to the ED between 2015 and 2019. Bacteraemia was confirmed if at least one of the blood culture bottles grew a non-skin flora pathogen or if two blood culture bottles grew a skin flora pathogen from two different sites. The prevalence of bacteraemia was 46.5%. Gram positive bacteria, specifically Staphylococcus species, were the most common pathogens isolated from the bacteremic group. 42 patients survived to hospital admission. The multivariate analysis revealed that there was no association between bacteraemia and hospital mortality in OHCA patients (OR = 1.3, 95% CI= 0.2–9.2) with a p-value of .8. There was no association between antibiotic administration during resuscitation and hospital mortality (OR = 0.6, 95% CI= 0.1 − 3.8) with a p-value of .6.
Conclusion
In our study, the prevalence of bacteraemia among OHCA patients presenting to the ED was found to be 46.5%. Bacteremic and non-bacteremic OHCA patients had similar initial baseline characteristics and laboratory parameters except for higher serum creatinine and BUN in the bacteremic group. In OHCA patients who survived their ED stay there was no association between hospital mortality and bacteraemia or antibiotic administration during resuscitation. There is a need for randomised controlled trials with a strong patient oriented primary outcome to better understand the association between in-hospital mortality and bacteraemia or antibiotic administration in OHCA patients.
We aimed to determine the prevalence of bacteraemia in OHCA patients presenting to the Emergency Department. In our study, we found that 46.5% of patients presenting to our ED with OHCA were bacteremic.
Bacteremic and non-bacteremic OHCA patients had similar initial baseline characteristics and laboratory parameters except for higher serum creatinine and BUN in the bacteremic group.
We found no association between bacteraemia and hospital mortality. There was no association between antibiotic administration during resuscitation and hospital mortality.
There is a need for randomised controlled trials with a strong patient oriented primary outcome to better understand the association between in-hospital mortality and bacteraemia or antibiotic administration in OHCA patients.
KEY MESSAGES
Introduction
Despite advances in cardiopulmonary resuscitation (CPR), out-of-hospital cardiac arrest (OHCA) remains one of the most common causes of death globally [Citation1]. A systematic review of the global survivorship of all-cause OHCA reported a weighted Emergency Department (ED) survival rate of 22%, and a weighted in-hospital survival rate of 8.8% [Citation2].
The majority of OHCA cases have a cardiac origin but non-cardiac causes of OHCA do exist [Citation3]. Numerous studies have shown an association between sepsis, bacteraemia and cardiac arrest [Citation4,Citation5]. This association is more prominent in OHCA compared with in-hospital cardiac arrest (IHCA) [Citation5]. A previous study of patients with OHCA presenting to the ED found that 38% were bacteremic; notably, the ED mortality rate was higher in patients with bacteraemia than in patients without bacteremia [Citation6]. The association between bacteraemia and cardiac arrest is topic of active research. Some studies suggest that bacteraemia may be a sequela of the invasive resuscitation measures and potential bacterial translocation from the GI tract secondary to ischemia [Citation6,Citation7]. Other studies suggest that bacteraemia can be a non-cardiac origin of cardiac arrest [Citation3–5].
Despite these findings, there is a scarcity of evidence concerning the prevalence of bacteraemia in cardiac arrest patients presenting to the ED. Examining the association between bacteraemia and OHCA can have significant therapeutic and outcome implications by improving the chain of survival in the post resuscitation period. The aims of our study were to: determine the prevalence of bacteraemia in OHCA patients presenting to the ED and study the association between bacteraemia and in-hospital mortality in OHCA patients. In addition, the association between antibiotic use during resuscitation and in-hospital mortality was examined.
Methods
Setting
In Lebanon (setting of our study), several aspects of the American Heart Association (AHA) chain of survival are absent [Citation8]. Prehospital emergency resources are scarce. In the prehospital setting, the management of OHCA patients by emergency medical services (EMS) is based on quick transport to the hospital and minimal medical care (first aid intervention) [Citation8]. All the OHCA patients receive resuscitation in the Emergency Department where advanced cardiac life support (ACLS) care begins [Citation9] ().
Table 1. Patient characteristics and prehospital variables.
The study was performed at an academic tertiary care centre in Lebanon with greater than 50,000 annual ED patient visits [Citation10].
Inclusion and exclusion criteria
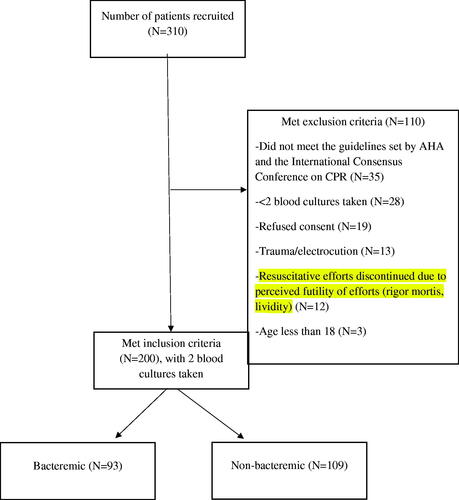
This was a single centre, observational study. All adult patients (≥18 years) who presented to the ED of our tertiary care medical centre with OHCA between October 2015 and August 2019 and underwent resuscitation in the ED were included. Research assistants present in the hospital were informed about eligible patients by the treating team. Patients were recruited 24 h a day, 7 days a week. Patients excluded from our study included: patients who refused consent, patients under the care of any member of the research team (to avoid observer bias), pregnant women, OHCA due to trauma or electrocution, patients with resuscitative efforts that were discontinued due to perceived futility of efforts (rigor mortis, lividity), patients with less than two sets of blood cultures and patients below the age of 18 years. All patients presenting to the ED with OHCA received Cardiopulmonary Resuscitation (CPR). OHCA was diagnosed based on the American Heart Association (AHA) and the International Consensus Conference on Cardiopulmonary Resuscitation (CPR) guidelines [Citation11]. All resuscitations performed by the ED team were in accordance with the advanced cardiac life support (ACLS) guidelines. All patients received the same standard of care provided for all OHCA victims presenting to the ED without involvement of any member of the research team. Patients who were under the care of any member of the research team were not approached to be included in the study to avoid observer bias. The research assistants consented the families of all included patients. The consent was informed, voluntary and written. This study was approved by our hospital Institutional Review Board (IRB# ER.GA.04)
Blood sample collection and patient classification
The study involved drawing blood for analysis and culture (aerobic and anaerobic) on OHCA patients undergoing resuscitation in the ED. Blood withdrawal was performed during active resuscitation by a registered nurse or phlebotomist who was not part of the resuscitation team. Blood cultures were collected during resuscitation from two different sites to decrease the chance of skin flora contamination (aerobic and anaerobic blood cultures from two different sites). In an effort to limit contamination, the individual performing the blood culture collection washed his/her hands and wore clean non-sterile gloves, the caps of the anaerobic and aerobic bottles were removed and the septum disinfected with 70% alcohol swabs, the skin over the venipuncture site was then cleaned with chlorhexidine and allowed to dry. While waiting for the skin to dry the individual collecting the blood culture discarded the non-sterile gloves, washed his/her hands again and wore sterile gloves before finally blood was drawn using disposable sterile syringes and needles. A standard definition of positive blood cultures was used to identify patients with bacteraemiaFootnote1. Patients were then divided into two groups based on culture results: bacteremic OHCA patients and non-bacteremic OHCA patients.
Variables and outcomes
The following information from OHCA patients were collected from the electronic medical records: vital signs upon presentation to ED, medical history, laboratory parameters, two blood cultures, urine analysis and urine cultures, medications used during resuscitation (including use of vasopressors, inotropes, antibiotics and steroids), patient disposition and presence or absence of bacteraemia and mortality at 72 h and 28 days. The primary outcome was the prevalence of bacteraemia. The secondary outcome was in hospital mortality.
Statistical analysis
Student t-test was used to compare the differences in continuous variables, and the χ2 test was used to compare the differences in categorical variables between both groups (Bacteremic vs non-bacteremic). In the bivariate analysis, the statistical association between the independent variables and the dependent variable mortality was assessed. In the multivariate analysis, logistic regression was used to assess the magnitude of association between bacteraemia or antibiotic administration and hospital mortality. The multivariate logistic regression only included the 42 OHCA patients who survived their ED stay. Missing data were not handled through multiple imputations because the percent of missing values in all variables was found to be less than 5%. All the tests were interpreted at a predetermined significance level (α = 0.05). Statistical analyses were performed using SPSS Statistics for Windows V.21.0. (Armonk, New York, USA: IBM Corp).
Results
We recruited a total of 310 OHCA patients from October 2015 to August 2019 (). 110 patients met the exclusion criteria, and 200 patients remained and were followed for a period of one month. Out of the 200, 93 were considered bacteremic. The prevalence of bacteraemia was 46.5% over the 4-year study period.
There were no significant differences in gender, age or medical history between bacteremic and non-bacteremic OHCA patients. The two groups had similar initial laboratory parameters except for higher serum creatinine and BUN in the bacteremic group ().
Table 2. Initial rhythm and lab parameters upon presentation to the ED.
There was no significant difference in CPR duration in the ED between bacteremic and non-bacteremic OHCA patients. Therapeutic interventions, including intravenous (IV) fluid volumes and vasopressor use, were similar between groups ().
Table 3. Therapeutic parameters and outcomes of patients.
Post-return of spontaneous circulation (ROSC) variables did not differ between both groups. ED mortality was higher in the bacteremic patients compared to the non bacteremic patients (86.0% versus 72.9% respectively) with a p-value of .02. However, there was no significant difference in in-hospital or 28-day mortality between the two groups (). The most common pathogen isolated from culture was Staphylococcus (47% of positive cultures), followed by Enterococcus (10.7%) and Escherichia coli (10.7%) ().
Table 4. Organisms found in the blood and in the urine.
Results of the multivariate analysis revealed that there was no association between bacteraemia and hospital mortality in OHCA patients (OR = 1.3, 95% CI= 0.2–9.2) with a p-value of .8. There was no association between antibiotic administration during resuscitation and hospital mortality (OR = 0.6, 95% CI= 0.1 − 3.8) with a p-value of .6 ().
Table 5. Logistic regression for Hospital Mortality.
Discussion
In this single-centre study of patients presenting to the ED following OHCA, we found a 46.5% prevalence of bacteraemia. Gram positive bacteria, specifically Staphylococcus species, were the most common pathogens isolated from the bacteremic group. After adjusting for confounders, the multivariate analysis revealed that there was no association between bacteraemia and hospital mortality in OHCA patients. There was no association between antibiotic administration during resuscitation and hospital mortality.
The impact of bacteraemia
In our study, the prevalence of bacteraemia in OHCA patients was 8.5% higher compared to Coba et al. (38% of 173 OHCA patients) [Citation6]. The association between bacteraemia and OHCA mortality has the potential to carry major therapeutic implications. It has been shown previously that undetected bacteraemia with inadequate treatment is strongly associated with increased mortality and long-term morbidity in septic patients [Citation12]. As well, the administration of early antibiotics in sepsis/septic shock has been definitively shown to be beneficial [Citation13]. Therefore, it is possible that early recognition of sepsis as the cause of OHCA and subsequent antibiotic administration might improve the survival rate in those patients who survive initial emergency department resuscitation.
Several studies examined infections in the post-resuscitation period. Gajic et al. reported that 46% of the OHCA patients admitted to the Intensive care unit (ICU) post CPR developed a new infection [Citation14]. Patients who developed an infection had increased length of mechanical ventilation, ICU length of stay and hospital mortality. In a study by Mongardon et al. 67% of OHCA patients developed infectious complications post resuscitation [Citation15]. ICU mortality was similar between both infected and non-infected patients [Citation15]. These two studies focussed on infectious complications that occurred after resuscitation was successful. They did not address the possible presence of infection prior to the cardiac arrest and that an infection may have potentially contributed to the cardiac arrest itself.
Gaussorgues et al. found that most of the pathogens isolated 12 h post resuscitation were Streptococcus (38.4%) and Gram negatives (46.1%). These findings can be explained by the low cardiac output secondary to the cardiac arrest which led to mesenteric ischaemia causing gut flora to move into the blood leading to sepsis [Citation7]. Contrary to Gaussorgues et al. most of the blood cultures we obtained grew Staphylococcus (47%). Coba et al. had similar results with their most reported pathogens being Staphylococcus (37%) and Streptococcus species (27.5%) [Citation6]. This discrepancy can be due to the time the blood cultures were taken; immediately upon arrival to the ED, the closest time possible to the time of arrest [Citation6].
Factors associated with mortality in OHCA patients
Bacteraemia in OHCA patients
There is controversy on the association between bacteraemia and cardiac arrest. Some studies suggest that bacteraemia is a consequence of the invasive resuscitation measures and potential gastrointestinal bacterial translocation [Citation6,Citation7]. Other studies state that bacteraemia is one of the non-cardiac origins of cardiac arrest [Citation3–5]
Several mechanisms can explain how bacteraemia can be a non-cardiac origin of OHCA. One possible mechanism involves sepsis-induced myocardial injury and hypoxia. Sepsis is a complex process that overwhelms the immune system and triggers an augmented immune response even at sites distant from the original inflammation site. The progression to septic shock is correlated with onset of new fatal arrhythmias like ventricular and atrial fibrillations [Citation16,Citation17]. Sepsis-induced tissue hypoxia combined with the exposure to vasoconstrictors contribute to a decreased myocardial blood supply and gross ischaemia [Citation18]. A prospective post-mortem examination by Schmittinger revealed stress-induced and ischaemic histopathologic changes in the myocardial and coronary arterial tissues of septic shock patients [Citation19].
The second mechanism involves sepsis-induced direct myocardial inflammation and depression. Bacterial endotoxins, as well as pro-inflammatory cytokines and reactive oxygen species, can lead to a decrease in myocardial contractility and a worse cardiac function [Citation20]. Moreover, Cuence et al. described the infiltration of the heart by monocytes and the expression of new extracellular matrix enzymes by the cardiomyocytes in early sepsis, leading to cardiac dysfunction [Citation21].
Antibiotic administration in OHCA patients
We found that 42 patients of the 200 survived in the ED, 88% of which received antibiotics. Coba et al. reported that 69% of OHCA ED survivors received broad-spectrum antibiotics in the ED [Citation10]. Davies et al. showed an early prophylactic treatment of OHCA patients with empiric antibiotics increased survival rate [Citation22], and Hellenkamp et al. demonstrated a longer length of hospital and ICU stay in OHCA patients who received a delayed antibiotic treatment [Citation23]. Gagnon et al. found that prophylactic antibiotic administration in cardiac arrest survivors was associated with less pneumonia and sepsis in the post-resuscitation period (12.6% vs 54.9% and 1.2% vs 5.7% respectively with a p < .001) but both groups had similar functional outcome [Citation24]. On the other hand, Couper et al. showed that prophylactic antibiotic use in cardiac arrest patients was not associated with improved survival, better neurological outcome or decreased hospital length of stay which is in line with our results [Citation25]. Further studies should be done to address the question of antibiotic administration.
Limitations
This was a single centre study which could compromise the generalisability of our results to the entire population. Some of the OHCA patients were taking antibiotics prior to presentation which could have suppressed bacterial growth in culture and lead to underestimation of the prevalence of bacteraemia. Information regarding the antibiotic given during resuscitation was missing. Time to ED arrival after cardiac arrest occurrence was not included in our study which could have affected mortality. In addition, a major confounder of the study was the lack of pre-hospital resuscitation (ACLS). Pre-hospital resuscitation (ACLS) plays a crucial role in achieving ROSC in cardiac arrest patients. The delay in resuscitation due to the lack of pre-hospital ACLS could have reduced the number of patients who survived their ED stay and resulted in a relatively low number of patients included in our multivariate logistic regression (the results obtained in the multivariate analysis were not statistically significant). Although we defined bacteraemia with a common skin-flora organism in an OHCA patient as two blood culture bottles growing a skin flora pathogen from two different sites, the unknown clinical significance of positive cultures with common skin-flora organisms remains a limitation. Repeating blood cultures after the resuscitation to verify the persistence of bacteraemia was not feasible in this study and should be done in future studies. Finally, the treating physicians could have adjusted antibiotics based on the results of the blood cultures and this could have affected the mortality of the bacteremic patients.
Conclusion
In our study, the prevalence of bacteraemia among OHCA patients presenting to the ED was found to be 46.5%. Bacteremic and non-bacteremic OHCA patients had similar initial baseline characteristics and laboratory parameters except for higher serum creatinine and BUN in the bacteremic group. In OHCA patients who survived their ED stay there was no association between hospital mortality and bacteraemia or antibiotic administration during resuscitation. There is a need for randomised controlled trials with a strong patient oriented primary outcome to better understand the association between in-hospital mortality and bacteraemia or antibiotic administration in OHCA patients. In the future we would like to consider collecting blood cultures in OHCA patients, serially at two different times (during resuscitation and after resuscitation). This can help confirm the persistence of bacteraemia with a true pathogen and compare the microorganisms identified by blood culture during and post resuscitation to better understand if bacteraemia can be considered as an origin of cardiac arrest or a consequence of cardiac arrest.
Ethical approval
The research assistants consented the families of all included patients. The consent was informed, voluntary and written. This study was approved by our hospital Institutional Review Board (IRB# ER.GA.04).
Author contributions
All authors have made substantial contributions to the different phases and aspects of the study (conception of the study, design of the study and research funding, data collection, patient recruitment, data analysis and manuscript writing) and all authors endorse the data and conclusion.
Study registration
This study was approved by our hospital Institutional Review Board (IRB# ER.GA.04). This study was registered on the Clinical Research Portal of the American University of Beirut. This can be accessed with the following link: https://eur03.safelinks.protection.outlook.com/?url=https%3A%2F%2Fclinicalresearch.aub.edu.lb%2FClinicalTrials%2FDetails%2F119&data=04%7C01%7Cmelsayed%40aub.edu.lb%7Cbef6325d48f74496f44e08d93714bbfe%7Cc7ba5b1a41b643e9a1206ff654ada137%7C1%7C0%7C637601384452130767%7CUnknown%7CTWFpbGZsb3d8eyJWIjoiMC4wLjAwMDAiLCJQIjoiV2luMzIiLCJBTiI6Ik1haWwiLCJXVCI6Mn0%3D%7C1000&sdata=aJaFLyUKUXmzIVK2i7WtYdq4D67iSe66jJws%2FcRe074%3D&reserved=0
Informed consent
The consent forms signed by consented families of all included patients contained a section stating that the results of the study will be published in a scientific journal. The consent was informed, voluntary and written. All authors endorse the data and conclusion.
| Abbreviations | ||
| OHCA | = | Out-of-hospital cardiac arrest |
| ED | = | Emergency Department |
| CPR | = | Cardiopulmonary Resuscitation |
| IHCA | = | In-Hospital Cardiac Arrest |
| AHA | = | American Heart Association |
| EMS | = | Emergency Medical Services |
| ACLS | = | Advanced Cardiac Life Support |
| AED | = | Automated External Defibrillator |
| ROSC | = | Return of Spontaneous Circulation |
| IV | = | Intravenous |
| ICU | = | Intensive Care Unit |
Acknowledgements
We would like to acknowledge the role of the Emergency Medicine department at the American University of Beirut for their help in the study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
All the data was presented in the form of Tables. Patient information was collected from the electronic medical files of our institution.
The data that support the findings of this study are available from the corresponding author [MES], upon reasonable request.
Additional information
Funding
Notes
1 An OHCA patient was identified as having bacteremia if at least one of the blood culture bottles grew a non-skin flora pathogen or if two blood culture bottles grew a skin flora pathogen from the two different sites [Citation6].
References
- Travers AH, Rea TD, Bobrow BJ, et al. Part 4: CPR overview: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122(18 Suppl 3):S676–S84.
- Yan S, Gan Y, Jiang N, et al. The global survival rate among adult out-of-hospital cardiac arrest patients who received cardiopulmonary resuscitation: a systematic review and meta-analysis. Crit Care. 2020;24(1):61.
- Engdahl J, Holmberg M, Karlson BW, et al. The epidemiology of out-of-hospital ‘sudden’ cardiac arrest. Resuscitation. 2002;52(3):235–245.
- Carr GE, Yuen TC, McConville JF, et al. Early cardiac arrest in patients hospitalized with pneumonia: a report from the American Heart Association’s Get With The Guidelines-Resuscitation Program. Chest. 2012;141(6):1528–1536.
- Leoni D, Rello J. Cardiac arrest among patients with infections: causes, clinical practice and research implications. Clin Microbiol Infect. 2017;23(10):730–735.
- Coba V, Jaehne AK, Suarez A, et al. The incidence and significance of bacteremia in out of hospital cardiac arrest. Resuscitation. 2014;85(2):196–202.
- Gaussorgues P, Gueugniaud PY, Vedrinne JM, et al. Bacteremia following cardiac arrest and cardiopulmonary resuscitation. Intensive Care Med. 1988;14(5):575–577.
- El Sayed MJ, Bayram JD. Prehospital emergency medical services in Lebanon: overview and prospects. Prehosp Disaster Med. 2013;28(2):163–165.
- El Sayed M, Al Assad R, Abi Aad Y, et al. Measuring the impact of emergency medical services (EMS) on out-of-hospital cardiac arrest survival in a developing country: a key metric for EMS systems’ performance. Medicine. 2017;96(29):e7570.
- El Sayed M, Tamim H, Chehadeh AA, et al. Emergency medical services utilization in EMS priority conditions in Beirut, Lebanon. Prehosp Disaster Med. 2016;31(6):621–627.
- Soar J, Maconochie I, Wyckoff MH, et al. 2019 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the basic life support; advanced life support; pediatric life support; neonatal life support; education, implementation, and teams; and first aid task forces. Circulation. 2019;140(24):e826–e880.
- Leibovici L, Shraga I, Drucker M, et al. The benefit of appropriate empirical antibiotic treatment in patients with bloodstream infection. J Intern Med. 1998;244(5):379–386.
- Puskarich MA, Trzeciak S, Shapiro NI, et al. Association between timing of antibiotic administration and mortality from septic shock in patients treated with a quantitative resuscitation protocol. Crit Care Med. 2011;39(9):2066–2071.
- Gajic O, Festic E, Afessa B. Infectious complications in survivors of cardiac arrest admitted to the medical intensive care unit. Resuscitation. 2004;60(1):65–69.
- Mongardon N, Perbet S, Lemiale V, et al. Infectious complications in out-of-hospital cardiac arrest patients in the therapeutic hypothermia era. Crit Care Med. 2011;39(6):1359–1364.
- Dellinger RP, Levy MM, Rhodes A, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41(2):580–637.
- Meierhenrich R, Steinhilber E, Eggermann C, et al. Incidence and prognostic impact of new-onset atrial fibrillation in patients with septic shock: a prospective observational study. Crit Care. 2010;14(3):R108.
- Pulido JN, Afessa B, Masaki M, et al. Clinical spectrum, frequency, and significance of myocardial dysfunction in severe sepsis and septic shock. Mayo Clin Proc. 2012;87(7):620–628.
- Schmittinger CA, Dünser MW, Torgersen C, et al. Histologic pathologies of the myocardium in septic shock: a prospective observational study. Shock. 2013;39(4):329–335.
- Kakihana Y, Ito T, Nakahara M, et al. Sepsis-induced myocardial dysfunction: pathophysiology and management. J Intensive Care. 2016;4:22.
- Cuenca J, Martín-Sanz P, Alvarez-Barrientos AM, et al. Infiltration of inflammatory cells plays an important role in matrix metalloproteinase expression and activation in the heart during sepsis. Am J Pathol. 2006;169(5):1567–1576.
- Davies KJ, Walters JH, Kerslake IM, et al. Early antibiotics improve survival following out-of hospital cardiac arrest. Resuscitation. 2013;84(5):616–619.
- Hellenkamp K, Onimischewski S, Kruppa J, et al. Early pneumonia and timing of antibiotic therapy in patients after nontraumatic out-of-hospital cardiac arrest. Crit Care. 2015;20(1):31.
- Gagnon DJ, Nielsen N, Fraser GL, et al. Prophylactic antibiotics are associated with a lower incidence of pneumonia in cardiac arrest survivors treated with targeted temperature management. Resuscitation. 2015;92:154–159.
- Couper K, Laloo R, Field R, et al. Prophylactic antibiotic use following cardiac arrest: a systematic review and meta-analysis. Resuscitation. 2019;141:166–173.