ABSTRACT
Introduction
Wearable technology may provide the possibility to monitor and quantify home exercises, to increase motivation for training and to facilitate cooperation between stroke survivors and physiotherapists. However, little is known about potential users’ opinions about using such systems.
Purpose
To explore stroke survivors’ and physiotherapists’ perspectives on the potential benefit of such wearable technology consisting of a smartphone application and movement sensors.
Methods
Four semi-structured focus group discussions, two with stroke survivors (n = 12) and physiotherapists (n = 11) respectively, were conducted to explore their perceptions on the potential of such technology.
Findings
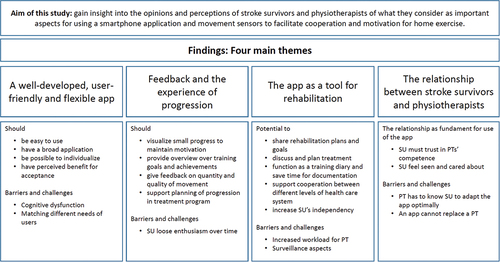
We developed four main themes through the thematic analysis: 1) the app should be well-developed, user-friendly and flexible; 2) the app’s potential for feedback and the experience of progression; 3) the app as a tool for rehabilitation; and 4) the app’s potential to strengthen the relationship between stroke survivors and physiotherapists.
Conclusions
Stroke survivors’ use of wearable technology to promote home exercise will depend as much on their trust in the professional and relational competence of the physiotherapist as the technical issues of an app. The potential benefits of wearable technology for cooperation between stroke survivors and physiotherapists and as a tool for rehabilitation were highlighted.
Introduction
The level of physical activity among stroke survivors is less than in the general population (Vahlberg, Bring, Hellström, and Zetterberg, Citation2019). Several studies indicate that people with stroke are physically inactive and spend most of their time sedentary during in-patient rehabilitation (Barrett et al., Citation2018; Sjöholm et al., Citation2014) and the frequency and intensity of therapy sessions do not reach recommended levels (Barrett et al., Citation2018). Similarly, stroke survivors living at home spend less time in activity and more time sitting compared with age-matched peers (English et al., Citation2016; Hassett et al., Citation2020). However, staying active and exercising is important to maintain independence in daily living.
To increase physical activity, as well as to improve motor function and to optimize recovery, home exercises are often prescribed by physiotherapists; however, adherence to home exercise seems to be less than ideal (Mahmood et al., Citation2020; Miller et al., Citation2017). A qualitative study concluded that interventions should be individualized and take into account social and environmental influences to enable stroke survivors to participate in physical activity (Morris et al., Citation2015). Similarly, van Dongen et al. (Citation2021) emphasized the importance of social aspects of exercising and the feeling of being connected to others. Lack of motivation and support was reported to be the most important reason for not to begin or continue exercising (van Dongen et al., Citation2021). In addition, the lack of professional support after the stroke survivors’ discharge from the hospital was regarded as an important barrier to physical activity (Nicholson et al., Citation2014).
New promising ways for interaction between patient and physiotherapist such as telerehabilitation (Sarfo, Ulasavets, Opare-Sem, and Ovbiagele, Citation2018) and the use of wearables evolved during the last decades, intending to track the activities of stroke survivors with the aim to motivate and to increase the amount of physical activity and specific training (Lynch et al., Citation2018). Wearable devices are electronic devices that can be worn on the body, like smart watches or fitness trackers and can be used in stroke rehabilitation to continuously monitor physical activities and activities of daily living (Dobkin and Martinez, Citation2018). The most frequent application of wearable devices in neurology is giving feedback on walking; and step counting is the most common function of commercial wearable devices (Dobkin and Martinez, Citation2018). Inertial movement units (IMUs) and accelerometers are the most frequently used sensors for the evaluation of physical activity in the stroke survivors’ natural environment (Jung et al., Citation2020), as for example during home exercise. A survey showed that 27% of the responding physiotherapists were using activity monitoring in day-to-day stroke care (Braakhuis, Bussmann, Ribbers, and Berger, Citation2021). Even if they considered remote wearable activity monitoring as useful, the technology was not widely adopted, mostly because they regarded the lack of stroke survivors’ knowledge and skills as an important barrier to implementation.
Unfortunately, commercially available wearables do not capture the slow and asymmetric movement patterns of stroke survivors reliably (Dobkin and Martinez, Citation2018). Furthermore, they are designed to give feedback about gait related activities, most often step counting (Dobkin and Martinez, Citation2018), and are not able to give feedback on various activities that are performed commonly during home exercise. In addition, a Cochrane review (Lynch et al., Citation2018) concluded that there is too little evidence to support the use of commercial wearables to increase physical activity after stroke, moreover little is known about the effectiveness of digital health technologies in at-home settings (Mura et al., Citation2022). However, smartphone applications (apps) in combination with movement sensors and machine learning algorithms, designed to recognize stroke survivors’ individual movement patterns, can be used to develop systems that can quantify the performance during home exercise (Boukhennoufa et al., Citation2021; Marwaa, Guidetti, Ytterberg, and Kristensen, Citation2022; O’Brien et al., Citation2017).
This study is part of an ongoing project that intends to develop a wearable system that can recognize the asymmetrical movement patterns in the lower limbs of stroke survivors. As the movement patterns of stroke survivors are asymmetrical, differ from person to person and are slower compared to healthy people, an option is to train the system to recognize individual movement patterns of stroke survivors. When the system has learnt the movement patterns under controlled conditions and has created a model of the recorded activities, it should be able to recognize the activities and exercises while the stroke survivor is performing them at home. This could make it possible to track not only activities related to walking, but also exercises typical performed at home, like sit-to-stand or stepping exercises. There is a rapid development in the field of human activity recognition, and such a system that reliably and accurately monitors the activities and home exercises might be available in the near future.
The perceived benefits of using new technologies seem to predict the acceptance of wearable devices (Brouns et al., Citation2019). Therefore, it might be crucial to include the potential users into the development of such a wearable system (Wentink et al., Citation2019). In order to get insight into stroke survivors’ and physiotherapists’ opinions about expected benefits or potential barriers for using this kind of wearable technology, we conducted focus group discussions. The aim of this study is to gain insight into the opinions and perceptions of stroke survivors and physiotherapists of what they consider as important aspects for using a smartphone application and movement sensors to facilitate cooperation and motivation for home exercise.
Methods
Design
The study was designed within the perspectives of social constructivism, using an interpretive framework to develop knowledge about peoples’ opinions and experiences (Creswell and Poth, Citation2018). Focus group discussions give the possibility to rapidly generate information and gather in-depth insights into participants’ opinions and perceptions, and were regarded as an appropriate method in the initial phase when developing a new product (Krueger and Casey, Citation2015). The interaction between the participants is essential, as it creates an environment for exchanging ideas and perspectives on a topic (Barbour, Citation2018). See to get an overview over the study design.
Participants
Purposeful sampling was used to recruit participants that were believed to have relevant background to inform the study (Creswell and Poth, Citation2018). Stroke survivors were recruited among people that had been to in-patient rehabilitation at a local center. The participants were included if they were more than 18 years old, had a stroke more than two months ago, were potential users of wearable technology, were able to walk independently and to perform home exercise without supervision. People with minor speech difficulties were included, as long as they were able to follow and participate in a conversation.
The physiotherapists were recruited among therapists working in the community, private practice and at a rehabilitation center. The inclusion criteria were that they should have experience with stroke rehabilitation. We recruited 12 stroke survivors and 11 therapists (). These sample sizes were considered to have enough information power (Malterud, Siersma, and Guassora, Citation2016) to elucidate the purpose of the study, both in sense of the participants’ characteristics and that we intended to generate opinions and ideas in the initial phase of developing a wearable device to support home training for stroke survivors. All participants received oral and written information about the study, and signed an informed written consent before participating. The regional ethics committee (REK Midt 2020/199756) approved the study.
Table 1. Participant characteristics.
Data generation
Two focus group discussions with six persons in each group were conducted with stroke survivors, and two focus groups with six and five physiotherapists, respectively, during November 2021. The discussions lasted about 90 min each, including a short break for the stroke survivors. The discussions took place in a quiet meeting room at a local rehabilitation center. A skilled focus group moderator (EL) and a co-moderator (RS) facilitated the group discussions. In addition, an observer (AG) took notes.
After the aim of the focus group discussion was presented and all participants had introduced themselves, the interviewees got a short introduction about how a smartphone app in combination with movement sensors could be used to record activities and home exercises. In addition,they were informed about the general capabilities of such a wearable device. Open questions were used to facilitate the discussion and to minimize the influence of the moderator (Ryan, Gandha, Culbertson, and Carlson, Citation2014). The moderator used a semi-structured thematic interview guide to assure that the following topics were covered: immediate comments after the presentation, the potential usefulness of the app to facilitate activity and promote home exercise, how such an app could influence the cooperation between stroke survivor and physiotherapist, and how such an app could contribute to increase motivation for home exercise. In addition, we were interested in issues such as design of the user interface, advantages and disadvantages of the wearable technology, as well as the willingness to test and use such an app. As our main interest was to have a wider perspective on the potential of such devices, we wanted to guide the participants as little as possible during the discussions. The role of the moderator was to facilitate the discussion, introduce relevant issues and to ensure that relevant topics were addressed (Krueger and Casey, Citation2015). The focus group discussions were audio recorded with consent from the participants, transcribed verbatim, anonymized and checked for accuracy, prior to analysis (AG).
Data analysis
Guidelines for thematic analysis as described by Braun and Clarke (Citation2022) were used in the active and interpretative process of making meaning of the dataset. A mainly inductive orientation was chosen for exploring the transcripts. After familiarizing with the data material as a whole, the text was given codes to name the immediate semantic meaning. Initial codes were collated and grouped together into potential themes bearing more of the latent meaning of the material. Initial themes were then reviewed and refined to final themes. Combining findings from the two informant groups made it possible to compare and to contrast perceptions and opinions. The coding work was mainly done by two of the researchers (EL, RS). All authors discussed and agreed on the final themes. Data was structured using Nvivo 12 (QSR International, Doncaster, Victoria, Australia).
Findings
The potential and the constraints of an app to facilitate cooperation and motivation for home exercise was an important topic for both stroke survivors and therapists. We developed four main themes through the analysis of the discussions: 1) the user-friendliness and flexibility of the app; 2) the app’s potential for providing feedback; 3) the app as a tool for rehabilitation; and finally 4) the app’s potential to strengthen the relationship between stroke survivors and physiotherapists. Details about the main findings are presented in .
Figure 2. Main themes and summary of the stroke survivors’ (SU) and physiotherapists’ (PT) opinions and perceptions.
The app should be well-developed, user-friendly and flexible
The therapists questioned the need for “just another app” as there already are many apps and wearables on the market. Both stroke survivors and physiotherapists agreed that user-friendliness and a fully developed system is a basic precondition for them to consider using such a system. The physiotherapists stressed that there should be some evidence that the system actually works and stimulates the stroke survivor to be more active. The first meeting with the app should not be negative for the stroke survivor. Often such technology, especially if it is not well developed, could be a frustrating experience.
Also they [stroke survivors] must feel a sense of accomplishment from the first time they use it, so that it does not become a burden or something negative (Marcus, PTFootnote1)
The stroke survivors and the physiotherapists highlighted the importance of the user-friendliness of such an app; the app and sensors should be easy to use, otherwise it can be an additional burden for the users. It should be a smooth log in and connection process with fewest possible keystrokes (i.e. not more than 2–3) otherwise it will not be used over time and will end up being just another app with limited benefit. In addition, there should be as little as possible text on the display. Both groups were concerned that for some stroke survivors cognitive dysfunction might be a barrier to use such an app.
The physiotherapists and most of the stroke survivors agreed that the recording of exercises to create a model of the movement patterns is too complicated for most stroke survivors and should be a task for the physiotherapist. However, two of the survivors with technical skills and interests would like to have access to advanced features to be able to create their own exercise program.
Well, I don’t train with a physiotherapist at the moment so I could, if I were to use something like that [the app], make my own model with activities or movements or exercises (Adam, SU)
The participants expressed that it could be an advantage to have two versions of such an app: one very simple for the stroke survivors and one more advanced for the physiotherapists. If it is not possible for the app to recognize and register complex exercises automatically with help from movement sensors, there should be a possibility to record activities like dancing and climbing manually in the same app. Further, they mentioned that it should be possible to register activities that involve the upper limb as well.
If I were to use such an app, it would have to be able to record all types of activities I have done. I don’t want to have one app that checks when I get up from my chair and another app that checks when I ride my bicycle, like. Then it isn’t appealing. (…) And then it is not used (Eskil, SU)
The app’s potential for feedback and the experience of progression
Another theme that was prominent in the discussion was feedback and how an app could support the stroke survivors’ experience of progression. The physiotherapists stated that stroke survivors often are very motivated for exercise in the beginning, but lose some of their enthusiasm over time because they are unable to see their progress. In that case, such an app could visualize even small progress. Compared to paper-based exercise diaries, it will be easier for the stroke survivors to recognize progression over time through diagrams, statistics and the history of the results, and thus, to maintain long-term motivation.
Very often, regardless of the issues they have, the patients don’t notice their own progress because it takes such a long time. It is much easier to point out when you have the numbers, “you managed so and so much less three weeks ago” (Nils, PT)
As the stroke survivors and physiotherapists tend to rely more on the objective data from the movement sensors than on self-reported exercise or activity registration, it could be valuable for the physiotherapist to adjust the treatment program based on objective registrations. It might also have the potential to show goal attainment:
Is it perhaps nice to have an overview of which goals you have achieved and which rewards you have got, sort of, just to be able to go back and see “oh look at everything I have managed here” and have a sort of overview. I think that might be useful to have in an app like that (Ina, PT)
One stroke survivor suggested building in an expected progression into the app, where physiotherapists and stroke survivors plan the progression in the exercise program together. In addition, the participants mentioned the possibility to express goal achievement in percent to make it possible to compare themselves with peers with higher functional capacity, here illuminated by the stroke survivor Eskil:
(…)… then I could set myself a training goal expressed only in percentages, so you then see how much of that you achieve. To share percentages with people can be impressive because you can do something with that (Eskil, SU)
Both stroke survivors and physiotherapists wished that such a system could give feedback not only on the quantity of the home exercise program, but also on the quality of performance (i.e. how exercises were performed). Most participants agreed that rewards in the form of notifications, short messages, emojis and signs, should be included into the feedback system of the app in order to facilitate motivation. Altogether, there was a huge variation on what the stroke survivors would prefer as feedback from such an app. Some mentioned that it would be more motivating if the voice of their own physiotherapist gave feedback via the app, compared to the voice of an unknown person. However, not all stroke survivors felt motivated by rewarding comments, and they expressed that they were very sensitive to verbal comments like a “well done” that does not correspond with how they experienced their performance.
Both groups had concerns about how stroke survivors with cognitive dysfunction could remember to do their exercises. The participants discussed the possibility of getting a notification to remind the survivors to start exercising. However, it should be possible to adjust the frequency of such reminders to the survivor’s needs, as too frequent notifications were regarded as annoying by some of the stroke survivors.
The app as a tool for rehabilitation
The participants emphasized that data from the app would be relevant for discussing and planning treatment. An app that makes it possible to share the recordings of what the stroke survivors have done during home exercise, could give both stroke survivors and therapists an overview to which degree the survivors performed their planned home exercise. Some physiotherapists stated that compared to self-report, this would provide them with objective feedback about the stroke survivors’ activities and the specific exercises they trained. Information from the app could be a useful tool in planning the next consultation.
To be able to follow up, well I think we’re in the blind when regulating the training quantity when we don’t have any figures on what has actually been done. Self-reporting is an inaccurate thing. (…) and we also have a few patients where we can’t say that “nothing has been done here because we don’t see any effect,” it may still have occurred. With a [digital] training diary, we would know what’s going on. Then it’s possible to practice actual training planning (Nils, PT)
Both physiotherapists and stroke survivors believed that the app could facilitate motivation to practice via the feedback function and through the possibility to communicate directly. If the therapists have the possibility to give direct feedback and to show the stroke survivors when they have done less than intended, they can ask about possible reasons and adapt the exercise program and goals accordingly, also between the consultations.
Regarding their workload, the physiotherapists see advantages and disadvantages of a system that allows the stroke survivors to share movement data. They would appreciate that the exercise data were transferred directly to the journal; this could save some of the time they have to spend on documentation. Often physiotherapists’ resources are restricted and they have limited capacity to follow up the stroke survivors. Such an app could help them to prioritize stroke survivors based on the objective registrations from the movement sensors. It could enable them to decide if they should spend less time on stroke survivors who are compliant to their training recommendations and who, via the app, get sufficient feedback and contact with their physiotherapist. Instead, they could prioritize stroke survivors who struggle to exercise without having a physiotherapist at their side. The app could also help to reduce the number of consultations for some stroke survivors and give them more responsibility to train on their own, still with the opportunity to have contact with the physiotherapist. Some therapists believed that the stroke survivors could to a higher degree use the app between the consultations and the app could possibly replace some visits at the stroke survivors’ home.
…if the idea is that you can also cut down the patient visits by using the app, you know, for exercising, because it’s the idea with consultations, that you check “oh have you done your exercises.” It might be great now through an app (haha). But yes, that this is part of the idea, that the app should also be used instead of going home to the patient (Trude, PT)
One physiotherapist expressed that if such an app would end up as a well working digital training diary that is used by both stroke survivors and physiotherapists, this would “revolutionize” their work. However, the physiotherapists were also concerned that an app that provided continuous information about each stroke survivor’s compliance could also lead to more work and stress, like “a pop-up-hell,” as (Jarl, PT) expressed, and Ina (PT) added later:
Yes, you can choose if you want feedback the other way too. But then it quickly becomes a lot of communication in a channel you might not want that much, you might not have the time for it. But at least being able to give such small motivational boosts is probably what I want most (Ina, PT)
Stroke survivors and physiotherapists discussed the positive and negative sides of sharing the survivors’ training log. Both groups worried about the surveillance aspect of the app. Especially the physiotherapists worried about privacy, whereas the stroke survivors tended to see more of the positive sides and told that it is their decision with whom they want to share their data. Knowing that their physiotherapist possibly could follow them from distance would in their opinion be highly motivating, like the stroke survivor Maja said: “It’s rather committing, if you feel like the devil is on your shoulders watching.”
The app could also be used to promote cooperation between levels of the health care system if the same journal system was being used. The participants imagined that the app could facilitate a smoother transfer between the levels and increase communication between a stroke specialist and the local physiotherapist. One survivor expressed that such a smooth transfer gives the physiotherapist insight in the stroke physiotherapist’s work. A physiotherapist talked about the communication loop between stroke specialist, municipal and private physiotherapist and the stroke survivor and that there could be feedback both ways.
So if the app helps to share important information whether it’s the hospital using it or whether we’re using it, in a shared profile, to inform each other about what to do and what’s been done, then absolutely (Ole, PT)
In the therapists’ focus groups, they discussed that feedback via the app could enable stroke survivors, who have been followed over long time periods, to participate more actively in their rehabilitation process. The app could be regarded as an “exercise buddy” (Didrik, PT) that may increase the stroke survivors’ responsibility for training and self-efficacy, and make them more independent of the therapist:
To make yourself less dependent on someone (…) it can be a bit difficult finishing [treatment]. So there’s something about finding something that might be useful to further independence maybe mostly in relation to training. Because it’s something about taking responsibility, and to show them that it’s ok to take that responsibility, that it will work and you will manage it. And maybe there will be a sense of accomplishment in that (Cecilie, PT)
The stroke survivors and the physiotherapists discussed the potential of the app to be part of a wider system that takes into account the rehabilitation perspective. They suggested that treatment goals or a rehabilitation plan could be accessible in the app. Several stroke survivors talked about how setting goals motivates them to exercise and that achieving goals gives them a motivational boost.
If it had been possible to set a goal, or maybe an updated six-month goal, so that you have worked for six months toward a goal in collaboration with a therapist (…) … because I am motivated to go without a wheelchair on the next flight. We have moved from a house to a flat with very nice stairs with railings on both sides, so I call it climbing the flight stairs. I take a walk every day on the flight stairs. Because the [main] goal is to go back to a warm and nice place (Maja, SU)
The physiotherapists agreed that the app would be particularly useful if it is not restricted to stroke survivors, but could also be applied on other user groups, like frail elderly people, people with orthopedic problems, or other neurological conditions.
The app’s potential to strengthen the relationship between stroke survivors and physiotherapists
The personal relation between physiotherapists and stroke survivors was a recurrent theme in the focus group discussions with the stroke survivors. They talked about “my physiotherapist” and highlighted the importance that their physiotherapist cared about them as a person. The importance of the personal contact and “being seen” by their physiotherapist was considered as essential to motivate for home exercise. However, they stressed that an app could not replace the personal contact with the physiotherapist. In order to adapt the training and to motivate and challenge the stroke survivors in an optimal manner, the physiotherapist has to know them.
Important that there are people who knows you (…) then it can be very motivating because it is easy to set up the goals and a final goal. So I really believe in that (Finn, SU)
The personal relation was also mentioned by the physiotherapists, however, their main focus was on organizational aspects like planning the treatment, giving more specific feedback.
I also think that some people will feel more taken care of when they have the app in between consultations. That it is a bit more stimulating, a bit more active follow-up than that piece of paper [exercise program] (Didrik, PT)
Several of the stroke survivors questioned how early after stroke the app should be introduced. They were concerned that feedback from an app in the early phase after stroke should be given with care as they remembered this as a vulnerable phase when feedback on training was interpreted differently compared to years after the stroke. Their physiotherapist’s sensitivity and the relationship with their physiotherapist would be essential to how they could react to comments.
Also, it is a very vulnerable time. So they [physiotherapists] should have compassion in addition to the technical skills, I think that’s very important (Finn, SU)
The app will not do better than the physiotherapist as some stroke survivors mentioned. The app will only be useful if it is used as a supplement to facilitate the cooperation between stroke survivors and physiotherapists. Eskil (SU) put it like “But I like the interpersonal aspect, that it is a person”, Hans (SU) replied “You don’t get that with an app”.
Likewise, the physiotherapists stressed that their competence cannot be replaced by an app, they still would have to interact with the stroke survivors, and their “professional gaze” would be better than a digital app. One stroke survivor expressed that the competent physiotherapist who knows them is best suited to start up with the app.
The stroke survivors experienced it as positive if their regular physiotherapist was open and interested in cooperation with the stroke physiotherapists at the hospital. One stroke survivor stated that physiotherapists who treat few stroke survivors could benefit using the app in cooperation with physiotherapists specialized on stroke rehabilitation to learn what exercises and activities could be most beneficial. The competence and engagement of the physiotherapist is an important precondition for trust as Finn stated:
The therapist must have a high level of expertise, otherwise it does not work. (…) So one must have human qualities in addition to the technical (Finn, SU)
Some of the stroke survivors exercised in a group with other survivors, which they found highly motivating. They felt safe and supported by their peers as they understood each others’ situation. Some of the stroke survivors could even imagine sharing exercise data from the app with their peers in such a safe and trusting environment. Sharing information and experience about exercises via the app could help them to see what others have done, get feedback and get “pushed” further by peers. This could possibly increase “self-motivation,” as one stroke survivor (Eskil) expressed it. In addition, sharing activity and exercise data via the app can facilitate discussion with like-minded people with similar problems.
And then that with the group is a factor, because they have an understanding of the fact that other people have ailments, I notice that in the group we belong to. They understand why you are not always doing so good. The physiotherapists don’t always do that (Finn, SU)
Being seen by physiotherapists and peers seem to be especially important during episodes when “everything gets hard” and they “don’t get on.” This was also experienced during the covid pandemic when group training was not possible. One stroke survivor believed that an app that makes it possible to share training data and experiences could have helped in that situation.
I think so, because then I’ve got the focus back on it, through that app, that now I have to pull myself together. Otherwise, there were no one to take a hold of this, just me. (…) I would guess that maybe one of those [apps], I don’t just guess, I think and I know that those would have been very motivating for me (Anne, SU)
Discussion
The purpose of this study was to investigate the perceptions of stroke survivors and physiotherapists about the potential of a wearable system consisting of a smartphone app and movement sensors to facilitate cooperation and motivation for home exercise. We wanted to get insight into what they consider as important aspects for using such an app. The analysis from the focus group discussions indicates that the apps’ possibility to give feedback about home exercises and to improve the communication and cooperation between stroke survivors and physiotherapists could facilitate motivation for use. Such an app could also improve goal setting and treatment planning, and thus work as a tool in the rehabilitation process. The user-friendliness, the system’s flexibility to adapt to the individual needs of the stroke survivor and to monitor progression were regarded as important preconditions for users to be willing to adopt such a system. The survivors emphasized the potential of the app to promote the personal relation to “their” physiotherapist and the support from their peers, while the physiotherapists focused more on the organizational benefits of the app.
The stroke survivors and the therapists emphasized that they are not interested in “just another app” and prefer one app with the possibility to register a variety of activities. Most of the apps that already are developed to support rehabilitation after stroke have a narrow content like exercises to strengthen ankle muscles, to facilitate finger movements, or to support trunk and balance control, as a recent review reports (Marwaa, Guidetti, Ytterberg, and Kristensen, Citation2022). Currently, a single device may not meet the variable needs of the stroke survivors and the physiotherapists (Louie, Bird, Menon, and Eng, Citation2020). However, the field of wearable technology based on inertial measurement unit (IMU) sensors is rapidly developing and new solutions like more advanced sensors and new ways to analyze the signals obtained from the sensors can make it possible to analyze human abnormal locomotion in more detail in the future (Glowinski, Blazejewski, and Krzyzynski, Citation2017). Such future devices will make it possible to track more complex activities related to home exercise. Apps that register activities broadly (i.e. registration of climbing or dancing) may stimulate the stroke survivors to use the app daily, not only when performing home exercises. Daily use may contribute to better adherence to the use of the app and thereby to home exercise.
The possibility to individualize the type of instructions and feedback given on the app was stressed by the participants, such as reminders, statistics, history, notifications, incorporation of goals and rehabilitation plan, as well as the possibility to communicate with peers and health care providers. This is in line with the findings from other studies (Dobkin, Citation2016; Wentink et al., Citation2019). It seems to be a critical factor for successful use that the device matches the individual needs of the users (Chen and Bode, Citation2011).
The participants in our study highlighted the role of feedback on progression as an important aspect. As survivors often do not recognize progress from day-to-day, the possibility to show them their training history might be valuable to facilitate motivation. The participants in our study regarded the app as a useful tool to document progress in a more objective and reliable way compared to paper-based home exercise dairies. As wearable technology may give an opportunity to objectively monitor and quantify motor behavior both inside and outside the clinic, it provides the possibility to give feedback about physical activities (Maceira-Elvira, Popa, Schmid, and Hummel, Citation2019; Porciuncula et al., Citation2018). Providing feedback on physical activity can improve compliance and stimulate self-management; the experience of even small changes in performance can promote motivation and stimulate home exercise (Dimaguila, Batchelor, Merolli, and Gray, Citation2020; Poltawski et al., Citation2015).
If the stroke survivors train mainly without supervision, such an app could make it possible to share data and communicate about their home exercise with their physiotherapist on demand. Access to training data could provide the physiotherapists with an insight into what the stroke survivors were doing and how they understood the home exercises. The regular personalized support could increase adherence to home exercise because the stroke survivors know they are monitored and followed-up. Thus, the app may help to overcome barriers to home exercise adherence, because the physiotherapist is able to identify problems and help the stroke survivors to manage barriers (Miller et al., Citation2017).
The participants in our study suggested, that such an app could be a useful tool in rehabilitation, through facilitating discussion about goals and giving the survivor insight into how exercises are related to their rehabilitation goals. The review from Marwaa, Guidetti, Ytterberg, and Kristensen (Citation2022) concluded that most existing smartphone apps designed to support rehabilitation, have limited usability as they focus on only one aspect of the rehabilitation process, usually assessment or training. Few studies in the review used the app for several purposes, and only one focused on goal setting. The role of patient-centered goal setting was emphasized in previous research (Rosewilliam et al., Citation2016), and an app may help to improve goal-setting practice.
According to our participants, the possibility to cooperate and communicate via the app is essential for using such a system. The interest of stroke survivors to stay connected with their physiotherapist was also highlighted by other studies, which stressed that the use of technology should take into account the importance of the interaction between stroke survivors and professionals (Poltawski et al., Citation2015). Being integrated in the electronic journal system, it also has the potential to be a device to facilitate communication and collaboration between the stakeholders in rehabilitation. One could also imagine that the app could support cooperation and knowledge transfer between experienced stroke physiotherapists and less experienced therapists.
The stroke survivors regarded it as important that their physiotherapist has knowledge and competence about stroke; however, it seemed to be even more important that the physiotherapist was genuinely interested in them as a person. This is similar to the findings of Peiris, Taylor, and Shields (Citation2012) who found that stroke survivors valued the relationship with their therapists as higher than the content of the therapy. The physiotherapist has to know the stroke survivor in order to be able to take the survivors’ goals into account and to utilize and adapt the system to the survivors’ needs and preferences as well as to establish trust in the therapeutic relation. If the physiotherapists know the stroke survivors, they are also able to recognize when the survivor is in a vulnerable phase and can adapt the feedback accordingly, an app cannot do that. The stroke survivors will probably have less benefit from the app if they doubt on the competence of their physiotherapist and if they do not feel that the app supports the relation to their physiotherapist.
According to Luker et al. (Citation2015) motivation requires nurturing and can be affected positively or negatively by the cooperating parts. The benefits of the app depend on the users and the app cannot replace the professional and personal relations, but the relations can be supported by the app. The usefulness of the app will depend on the reflections and recommendations of the physiotherapist. The physiotherapists in our study stressed that they still have to interact with the stroke survivors and expressed that their competence and “knowing-in-practice” cannot be replaced by an app. In addition to physical meetings, the app could provide ongoing support, which seems to be important for sustaining motivation to exercise over time (Poltawski et al., Citation2015). Moreover, the app could help the stroke survivors to get more responsible and less dependent on the physiotherapist; this has the potential to improve their self-efficacy.
Limitations
There was possibly some selection bias since stroke survivors and physiotherapists with experience and interest in wearable technology might be more interested in participating in focus group discussions. However, the participants’ characteristics showed that half of the stroke survivors had no experience with wearables and exercise apps. In contrast, all physiotherapists had at least some experience with wearables and apps.
One stroke survivor was still inpatient when participating in the focus group discussion and might have had limited experience with home exercise. As this participant was very interested in technology and had previous experience with wearable devices, it was expected that he would be able to make relevant contributions to the focus group discussion.
The moderators had met some of the stroke survivors before in earlier in-patient rehabilitation. Likewise, the moderators were known with some of the physiotherapists. Acquaintance to the participants could have influenced them toward suppressing negative opinions. On the other hand, the familiarity might also help them to talk more freely.
Findings regarding the app’s user friendliness, its potential for feedback on progression as well as its relational potential are assumed to have relevance in most rehabilitation contexts. However, its use as a rehabilitation tool might be more dependent on the organization of the specific health care system.
Conclusion
Wearable technology aiming to promote stroke survivors’ home exercise should be highly flexible, as the needs of the stroke survivors and physiotherapists are multifaceted. Their needs relate to different dimensions such as design, user-friendliness, how feedback on progression is provided, and how motivation and cooperation are supported. Most likely it will be difficult to meet all these needs with current technological solutions. However, the mentioned aspects should be regarded when designing new devices.
The stroke survivors’ successful use of the app will not only depend on technical and design issues, but also on the trust in the professional and relational competence of the physiotherapist. If facilitated by a competent physiotherapist with good relational and professional competence and knowledge about stroke rehabilitation, the app has the potential to promote a more direct communication and cooperation about goal setting and treatment planning and thus to increase adherence to home exercise.
Future studies should address the potential of such an app as a tool in rehabilitation in more detail. In addition, they should further investigate how relational aspects and the feeling of “being seen” could be supported by the way the system is designed.
Acknowledgments
We would like to thank the stroke survivors and physiotherapists for their valuable contributions in the focus group discussions. This work was supported by the Norwegian research council under Grant [number 317454] and NTNU Discovery under Grant [number 90427572].
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
Notes
1. Abbreviations for the participants: physiotherapist = PT, stroke survivor = SU. All participants’ names were pseudonymized.
References
- Barbour R 2018 Doing focus groups, 2nd. Los Angeles: SAGE.
- Barrett M, Snow JC, Kirkland MC, Kelly LP, Gehue M, Downer MB, McCarthy J, Ploughman M 2018 Excessive sedentary time during in-patient stroke rehabilitation. Topics in Stroke Rehabilitation 25: 366–374. 10.1080/10749357.2018.1458461
- Boukhennoufa I, Zhai X, Utti V, Jackson J, McDonald-Maier K 2021 A comprehensive evaluation of state-of-the-art time-series deep learning models for activity-recognition in post-stroke rehabilitation assessment. Annual International Conference of the IEEE Engineering in Medicine and Biology Society 2021 Mexico: 2242–2247.
- Braun V, Clarke V 2022 Thematic analysis: A practical guide. Los Angeles: SAGE.
- Brouns B, Meesters JJ, Wentink MM, de Kloet AJ, Arwert HJ, Boyce LW, Vliet Vlieland TP, van Bodegom-Vos L 2019 Factors associated with willingness to use eRehabilitation after stroke: A cross-sectional study among patients, informal caregivers and healthcare professionals. Journal of Rehabilitation Medicine 51: 665–674. 10.2340/16501977-2586
- Braakhuis HE, Bussmann JB, Ribbers GM, Berger MA 2021 Wearable activity monitoring in day-to-day stroke care: A promising tool but not widely used. Sensors 21: 4066. 10.3390/s21124066
- Chen CC, Bode RK 2011 Factors influencing therapists’ decision-making in the acceptance of new technology devices in stroke rehabilitation. American Journal of Physical Medicine & Rehabilitation 90: 415–425. 10.1097/PHM.0b013e318214f5d8
- Creswell JW, Poth CN 2018 Qualitative inquiry and research design: Choosing among five approaches, 4th. Los Angeles: Sage.
- Dimaguila GL, Batchelor F, Merolli M, Gray K 2020 ‘We are very individual’: Anticipated effects on stroke survivors of using their person-generated health data. BMJ Health & Care Informatics 27: e100149. 10.1136/bmjhci-2020-100149
- Dobkin BH 2016 Behavioral self-management strategies for practice and exercise should be included in neurologic rehabilitation trials and care. Current Opinion in Neurology 29: 693–699. 10.1097/WCO.0000000000000380
- Dobkin BH, Martinez C 2018 Wearable sensors to monitor, enable feedback, and measure outcomes of activity and practice. Current Neurology and Neuroscience Reports 18: 87. 10.1007/s11910-018-0896-5
- English C, Healy GN, Coates A, Lewis L, Olds T, Bernhardt J 2016 Sitting and activity time in people with stroke. Physical Therapy 96: 193–201. 10.2522/ptj.20140522
- Glowinski S, Blazejewski A, Krzyzynski T 2017 Inertial sensors and wavelets analysis as a tool for pathological gait identification. In: Gzik M, Tkacz E, Paszenda Z Pietka E (Eds) Innovations in biomedical engineering: advances in intelligent systems and computing, pp. 106–114. Cham, Switzerland: Springer.
- Hassett L, Ada L, Hellweg S, Paul S, Alzahrani M, Dean C 2020 Active and sedentary bouts in people after stroke and healthy controls: An observational study. Physiotherapy Research International 25: e1845. 10.1002/pri.1845
- Jung S, Michaud M, Oudre L, Dorveaux E, Gorintin L, Vayatis N, Ricard D 2020 The use of inertial measurement units for the study of free living environment activity assessment: A literature review. Sensors 20: 5625. 10.3390/s20195625
- Krueger RA, Casey MA 2015 Focus groups: A practical guide for applied research, 5th. Los Angeles: Sage.
- Louie DR, Bird ML, Menon C, Eng JJ 2020 Perspectives on the prospective development of stroke-specific lower extremity wearable monitoring technology: A qualitative focus group study with physical therapists and individuals with stroke. Journal of Neuroengineering and Rehabilitation 17: 31. 10.1186/s12984-020-00666-6
- Luker J, Lynch E, Bernhardsson S, Bennett L, Bernhardt J 2015 Stroke survivors’ experiences of physical rehabilitation: A systematic review of qualitative studies. Archives of Physical Medicine & Rehabilitation 96: 1698–1708. e1610. 10.1016/j.apmr.2015.03.017
- Lynch EA, Jones TM, Simpson DB, Fini NA, Kuys SS, Borschmann K, Kramer S, Johnson L, Callisaya ML, Mahendran N, et al. 2018 Activity monitors for increasing physical activity in adult stroke survivors. Cochrane Database of Systematic Reviews 7: Cd012543. 10.1002/14651858.CD012543.pub2
- Maceira-Elvira P, Popa T, Schmid AC, Hummel FC 2019 Wearable technology in stroke rehabilitation: Towards improved diagnosis and treatment of upper-limb motor impairment. Journal of Neuroengineering and Rehabilitation 16: 142. 10.1186/s12984-019-0612-y
- Mahmood A, Solomon JM, English C, Bhaskaran U, Menon G, Manikandan N 2020 Measurement of adherence to home-based exercises among community-dwelling stroke survivors in India. Physiotherapy Research International 25: e1827. 10.1002/pri.1827
- Malterud K, Siersma VD, Guassora AD 2016 Sample size in qualitative interview studies: Guided by information power. Qualitative Health Research 26: 1753–1760. 10.1177/1049732315617444
- Marwaa MN, Guidetti S, Ytterberg C, Kristensen HK 2022 Use of mobile/tablet and web-based applications to support rehabilitation after stroke: A scoping seview. Journal of Rehabilitation Medicine 54: jrm00269. 10.2340/jrm.v54.452
- Miller KK, Porter RE, DeBaun-Sprague E, Van Puymbroeck M, Schmid AA 2017 Exercise after stroke: Patient adherence and beliefs after discharge from rehabilitation. Topics in Stroke Rehabilitation 24: 142–148. 10.1080/10749357.2016.1200292
- Morris JH, Oliver T, Kroll T, Joice S, Williams B 2015 From physical and functional to continuity with pre-stroke self and participation in valued activities: A qualitative exploration of stroke survivors’, carers’ and physiotherapists’ perceptions of physical activity after stroke. Disability & Rehabilitation 37: 64–77. 10.3109/09638288.2014.907828
- Mura A, Maier M, Ballester BR, De la Torre Costa J, López-Luque J, Gelineau A, Mandigout S, Ghatan PH, Fiorillo R, Antenucci F, et al. 2022 Bringing rehabilitation home with an e-health platform to treat stroke patients: Study protocol of a randomized clinical trial (Rgs@home). Trials 23: 518. 10.1186/s13063-022-06444-0
- Nicholson S, Donaghy M, Johnston M, Sniehotta F, van Wijck F, Johnston D, Greig C, McMurdo ME, Mead G 2014 A qualitative theory guided analysis of stroke survivors’ perceived barriers and facilitators to physical activity. Disability & Rehabilitation 36: 1857–1868. 10.3109/09638288.2013.874506
- O’Brien MK, Shawen N, Mummidisetty C, Kaur S, Bo X, Poellabauer C, Kording K, Jayaraman A 2017 Activity recognition for persons with stroke using mobile phone technology: Toward improved performance in a home setting. Journal of Medical Internet Research 19: e184. 10.2196/jmir.7385
- Peiris CL, Taylor NF, Shields N 2012 Patients value patient-therapist interactions more than the amount or content of therapy during inpatient rehabilitation: A qualitative study. Journal of Physiotherapy 58: 261–268.
- Poltawski L, Boddy K, Forster A, Goodwin VA, Pavey AC, Dean S 2015 Motivators for uptake and maintenance of exercise: Perceptions of long-term stroke survivors and implications for design of exercise programmes. Disability & Rehabilitation 37: 795–801.
- Porciuncula F, Roto AV, Kumar D, Davis I, Roy S, Walsh CJ, Awad LN 2018 Wearable movement sensors for rehabilitation: A focused review of technological and clinical advances. PM&R 10: S220–232.
- Rosewilliam S, Sintler C, Pandyan AD, Skelton J, Roskell CA 2016 Is the practice of goal-setting for patients in acute stroke care patient-centred and what factors influence this? A qualitative study. Clinical Rehabilitation 30: 508–519.
- Ryan KE, Gandha T, Culbertson MJ, Carlson C 2014 Focus group evidence: Implications for design and analysis. American Journal of Evaluation 35: 328–345.
- Sarfo F, Ulasavets U, Opare-Sem O, Ovbiagele B 2018 Tele-rehabilitation after stroke: An updated systematic review of the literature. Journal of Stroke & Cerebrovascular Diseases 27: 2306–2318.
- Sjöholm A, Skarin M, Churilov L, Nilsson M, Bernhardt J, Lindén T 2014 Sedentary behaviour and physical activity of people with stroke in rehabilitation hospitals. Stroke Research and Treatment 2014: 591897.
- Vahlberg B, Bring A, Hellström K, Zetterberg L 2019 Level of physical activity in men and women with chronic stroke. Physiotherapy Theory and Practice 35: 947–955.
- van Dongen L, Hafsteinsdottir TB, Parker E, Bjartmarz I, Hjaltadottir I, Jonsdottir H 2021 Stroke survivors’ experiences with rebuilding life in the community and exercising at home: A qualitative study. Nursing Open 8: 2567–2577.
- Wentink M, van Bodegom-Vos L, Brouns B, Arwert H, Houdijk S, Kewalbansing P, Boyce L, Vliet Vlieland T, de Kloet A, Meesters J 2019 How to improve eRehabilitation programs in stroke care? A focus group study to identify requirements of end-users. BMC Medical Informatics & Decision Making 19: 145.