Abstract
Purpose: People with cerebral palsy (CP) or spina bifida (SB) often struggle to perform everyday-life activities. Both groups frequently also have difficulties in creating and using strategies effectively when performing tasks. The cognitive orientation to daily occupational performance (CO-OP) Approach combines the learning of cognitive strategies with task-specific approaches through a client-centred procedure. The aim of this study was to investigate whether the CO-OP Approach is feasible for and potentially beneficial to adolescents and young adults with CP or SB in Sweden by analysing four areas of feasibility (acceptability, efficacy, adaptation, and expansion).
Methods: Exploratory multiple-case study using mixed methods. Ten persons aged 16–28, five with each condition, participated in an intervention period. Assessments were performed on three occasions: baseline, post-intervention, and six-month follow-up.
Results: The result demonstrates that the CO-OP Approach has the potential to enable adolescents and young adults with either condition to achieve personal goals and to enhance their planning skills and their ability to use strategies when performing activities. This approach is also compatible with the core values of habilitation in Sweden and was found by the participants to be highly meaningful and useful.
Conclusions: The CO-OP Approach is feasible for adolescents and young adults with SB or CP in Sweden.
The Cognitive Orientation to daily Occupational Performance
• is a feasible approach for adolescents and young adults with spina bifida and with cerebral palsy.
• is a promising approach when it comes to enabling the achievement of personal goals.
• might have potential to enhance executive functioning through strategy use.
• is in line with the fundamental core values of disability rights of inclusion, empowerment, and participation.
Implications for rehabilitation
Introduction
People with a diagnosis of cerebral palsy (CP) or spina bifida (SB) often struggle to perform everyday-life activities [Citation1–4]. This can restrict their participation in everyday life and cause low self-efficacy [Citation5,Citation6]. Traditionally, this has been studied mainly with regard to motor disability [Citation7] or environmental barriers [Citation8]. However, recent research shows that both groups often also have executive dysfunctions, such as difficulties with planning and problem-solving, which implies that they also have difficulties in creating and using strategies effectively [Citation9–12].
Purposeful doing in general can be seen as a process, in which we take action to transform an idea into an accomplished goal [Citation13,Citation14]. To do so, we use strategies (i.e., behaviours and thoughts that we use actively) to plan the action and then use our body in accordance with those strategies [Citation15,Citation16]. The use of strategies is often implicit – we may even be unaware that we use them [Citation16]. However, a need to use strategies more explicitly can occur when a person has difficulties either with motor performance, such as spasticity, or with process-based performance, owning to memory loss, and executive dysfunctions. A systematic review of contemporary intervention methods for children with CP [Citation17] has shown that, when it comes to enhancing performance in everyday activities, there is better evidence of effectiveness for task-oriented treatment methods than for component-based ones. The goal-setting in itself and the client-centred approach have been suggested as the operating element of task-oriented methods [Citation5,Citation18–20]. For the SB group, a few studies have been published about different intervention methods aiming to enhance performance in everyday activities. One study [Citation21] showed promising results in adults for goal management training, i.e., learning in a group setting how to use a strategy and another by Donlau et al. [Citation22] showed that a goal-focused approach helps children with SB to accomplish specific goals in self-care.
The cognitive orientation to daily occupational performance (CO-OP) ApproachTM [Citation23] combines the learning of cognitive strategy use with task-specific and goal-focused approaches through a client-centred procedure. Hence this approach might help make persons with both CP and SB better at achieving self-identified goals in everyday life. It was originally designed for children with developmental co-ordination disorder, and for that group, there is strong evidence of effectiveness in goal achievement [Citation24–26]. There is also evidence for CO-OP in adults with neurological disability after stroke [Citation27–29] or traumatic brain injury [Citation30] as well as in children with neurodevelopmental disabilities, such as attention deficit hyperactive disorder [Citation31] and, recently, in children with CP [Citation5,Citation32]. However, we have found no studies evaluating the use of CO-OP in adults with CP or in persons with SB, and nor has CO-OP, to the best of our knowledge, been used or tested in a Swedish context.
When an intervention method designed for a certain population is expanded to a new population, diagnosis or cultural context, there may be barriers requiring adaptation [Citation33]. Since CO-OP has not previously been used either in adults with CP or SB or in a Swedish context, prior to performing a large, randomised control study there is an initial need to study the feasibility of the method. The aim of this study was to investigate whether the CO-OP approach is feasible for and potentially beneficial to adolescents and young adults with CP or SB in Sweden by analysing four areas of feasibility (acceptability, efficacy, adaptation, and expansion) proposed by Bowen et al. [Citation34].
Method
Design
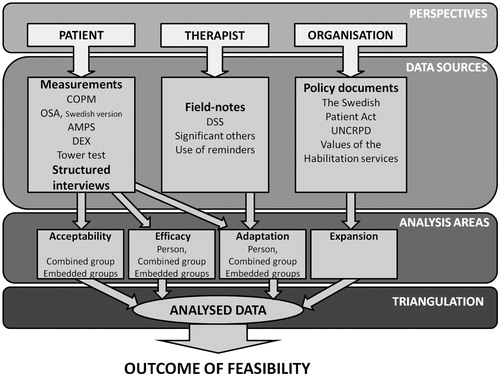
This feasibility study was designed as an exploratory multiple-case study with what Yin [Citation35] refers to as an “embedded design”. The study investigated the feasibility of CO-OP in a Swedish context for the two embedded sub-groups of adolescents/young adults with CP and SB, respectively. Four of the focus areas useful for feasibility studies according to Bowen et al. [Citation34] were chosen – acceptability (to what extent is a new approach judged as satisfying for recipients of the approach), efficacy (does a new approach show promise of being successful), adaptation (to what extent does an approach need adaptation to be appropriate for a new populations), and expansion (to what extent does an approach fit with a new context) as they applied to the design of this pilot study ().
The data used in the study were collected from different perspectives and sources (). The analysed data were triangulated to confirm different types of data and to present an overall picture of the feasibility of CO-OP for these groups in a Swedish context [Citation36] ().
The study was approved by the Regional Ethical Review Board of Gothenburg, Sweden (Ref. No. 736–13).
The cognitive orientation to daily occupational performance (CO-OP) approachTM
CO-OP is described in the manual [Citation23] as a client-centred and performance-based approach to problem-solving which enables individuals to identify cognitive strategies to improve their skill acquisition through an interactive process [Citation23,Citation37]. The client identifies the skills to be learned, sets his or her own goals and is actively involved throughout the process of solving problems and evaluating the performance of activities. There are four basic objectives: skill acquisition, cognitive-strategy use, generalisation of the activity learned to new situations, and transfer of a global strategy learned to solve new performance problems. The approach is based on theories of learning and focuses on client-centeredness and meta-cognitive learning [Citation23,Citation38].
CO-OP uses an eleven-session design. During the first session, the method is introduced with a focus on the global strategy (“Goal-Plan-Do-Check”). The client identifies three activity goals that he or she wants to achieve and rates his or her present level of performance and satisfaction with performance for those goals using the Canadian occupational performance measure (COPM) [Citation39]. In addition, the therapist establishes the baseline level of the client’s performance of the activities using the performance quality rating scale [Citation40]. The subsequent ten sessions focus on interactive use of the global strategy and on helping the client, by guided discovery, to discover his or her own plan. The client is constantly encouraged to evaluate his or her performance and to decide whether the plan has been successful or needs revision. The therapist also guides discovery of “domain-specific strategies” to help the client find ways to revise the plan [Citation23]. The domain-specific strategies are specific to the task, person, and situation, they can be grouped into seven types, and they are “nested” in the therapist’s verbal guidance during the intervention as part of the Goal-Plan-Do-Check procedure. The client is encouraged to use his or her plans at home between training sessions; with the support of significant others whom the client has chosen to support him or her during and after the intervention period. At the last session, the client again rates his or her performance and satisfaction with performance for all three goals and the therapist rates performance quality [Citation23].
Participants
A convenience sample was recruited through the habilitation centres of two Swedish regions. In Sweden, all children and adults diagnosed with CP or SB are offered to be in contact with an interdisciplinary out-patient team at a habilitation centre in their region. The inclusion criteria were: (a) diagnosis of CP (classified as levels I–III in the Manual Ability Classification System (MACS) [Citation41]; persons at those levels handle objects in everyday life between “easily” (level I) and “with difficulty” (level III)) or diagnosis of SB; (b) self-reported difficulties in carrying out activities in everyday life; (c) age 16–30 years; (d) nine years of compulsory education in the mainstream school system; and (e) ability to communicate verbally in Swedish. Thirteen persons agreed to participate, but three of them terminated their participation owing to personal circumstances and health conditions. Hence, 10 persons aged 16–28 years, five with SB and five with CP (MACS levels I–II), participated; their demographics are shown in .
Table 1. Participants’ demographics.
Procedure
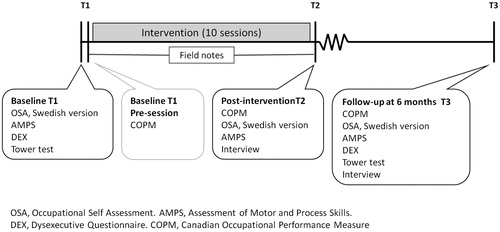
Assessments using different measurements were carried out on three occasions: at baseline (T1), post-intervention (T2), and at follow-up six months after the intervention (T3). Assessments of executive functions were performed at baseline (T1) and at the six-month follow-up (T3). Interviews were carried out post-intervention (T2), and at the six-month follow-up (T3) ().
Intervention
Each participant attended one preparation session and ten treatment sessions, one or two per week, each lasting for approximately one hour. Three of the authors, all occupational therapists and certified CO-OP therapists, delivered the CO-OP intervention sessions in accordance with the CO-OP protocol [Citation23].
Data sources
Data were collected from measurements, structured interviews, field notes, and policy documents.
Outcome measures
Goal attainment. To measure self-rated goal attainment, the Swedish version of the COPM [Citation42] was used. The COPM is part of the CO-OP protocol and was used in accordance with that protocol to identify activity-based goals that were important for each participant to achieve. The COPM is a client-centred, interview-based instrument designed to identify a client’s self-perception of performance in everyday life and to capture change over time. The levels of performance and satisfaction with performance for each goal were rated by the person him- or herself using a ten-point rating scale. The COPM has shown good test–retest reliability and good validity when used in neurological rehabilitation and good responsiveness to change when used in persons with CP [Citation39]. The cutoff representing clinically significant change recommended in the manual [Citation39] is a difference of two points in COPM score.
The outcome measures chosen to capture change owing to the possible transfer of the CO-OP skills to other situations in daily life were based on two components of the International Classification of Functioning, Disability, and Health – Child and Youth version [Citation43], namely the activity/participation and body-function components.
Assessment with regard to activity/participation. The Swedish version of the occupational self-assessment (OSA) [Citation44] was used to evaluate the participants’ perceptions of changes in their overall competence in occupational performance and participation in everyday-life situations. The OSA [Citation45] was designed to capture a client’s perspective on his or her performance competence and participation as well as the importance assigned by the client to a wide range of everyday activities. In this study, only the competence scale was used. The clients rated their self-perceived competence for 21 items on a four-point Likert scale. The raw ordinal scores can be transformed into interval-level scores using the OSA key form, and a statistically significant change is then defined as a case where the values obtained on two occasions do not overlap [Citation45]. Several studies have confirmed that the OSA items and ratings can be used as a valid and reliable measure capable of detecting change [Citation46,Citation47].
The Assessment of Motor and Process Skills (AMPS) [Citation48] is an observation-based method for evaluating the quality of occupational performance. It yields two measures, one for motor skills (i.e., moving oneself and the objects necessary to perform the task) and one for process skills (i.e., actions taken to steer the task from A to Z and to adjust and adapt to any problems that may occur). These two measures are presented as logits. The psychometric properties of the AMPS have been widely tested, and it has been found to be valid and reliable for use in people with congenital developmental disabilities [Citation48,Citation49]. A difference exceeding two standard errors (SE) between two data points is considered statistically significant [Citation48].
Assessment with regard to body function. The Dysexecutive Questionnaire (DEX) scale [Citation50] is a self-report measure of perceived difficulties associated with executive dysfunction. A supplement to the behavioural assessment of dysexecutive syndrome [Citation50], it consists of 20 items and uses a five-point Likert scale ranging from 0 (never) to 4 (very often), with higher scores indicating greater difficulties. The DEX has been psychometrically proven, with good validity and reliability [Citation50]. In a non-clinical sample, the mean was 22.1 out of a maximum of 80 (SD 8.9).
The Tower test from the Delis–Kaplan Executive Function System [Citation51], here used as measure of planning ability, is claimed to capture rule learning, spatial planning, inhibition of perseverative behaviour, and impulsive responses and to have sufficient psychometric properties (although it can be susceptible to practice effects). A clinically significant improvement is defined as a change in results from one ability level to another, based on the descriptive classification given by Wechsler [Citation52], which includes Low (scaled score 1–3), borderline (4–6), low average (7–8), average (9–11), high average (12–13), superior (14–16), and very superior (17–19).
All assessments except the COPM were performed by clinicians (neuropsychologists and occupational therapists) who were not involved in the intervention.
Structured interviews
In the interviews, five structured questions were used. (There was also a semi-structured part this has been analysed using a qualitative approach and the results will be presented in a forthcoming article). Four of them were yes-or-no questions: “Was CO-OP meaningful to you?”, “Were the results worth the effort?”, “Have you continued using the global strategy?” and (fourth question, asked only at the six-month follow-up) “Was there a significant other who supported your continued use of the global strategy? If yes, who?” The fifth question was, “How would you rate the effort involved in the training on a ten-point scale from one (least effort) to ten (most effort)?” The interviewer was one of the three therapists who were CO-OP instructors, but not the one who had conducted the training with the participant concerned.
Field notes
The therapists who conducted the CO-OP training wrote field notes after each session about their use of the approach and any adaptations made to it. These notes were compared with the CO-OP fidelity scale [Citation53]; in particular, the therapists noted the involvement of significant others and their reflections on the domain-specific strategies used by them while guiding the participants.
Policy documents
A number of key policy documents were compared with the CO-OP protocol: the Swedish Patients Act [Citation54], the United Nations Convention on the Rights of Persons with Disabilities [Citation55] and the “core values” statements found on the websites of the habilitation services of the Västra Götaland Region [Citation56] and the habilitation services of Stockholm County Council [Citation57], and the National Network of Swedish Habilitation Services [Citation58].
Data analysis
Because of the study’s exploratory design, its outcome in terms of feasibility was built up through an iterative analysis performed in different areas and in several steps (). The four focus areas described by Yin [Citation35] – acceptability, efficacy, adaptation, and expansion – were used as a framework for the analysis ().
Acceptability (i.e., how meaningful, laborious, useful over time, and worthwhile the method was perceived to be by the participants) was evaluated using the structured-interview questions at post-intervention (T2) and at follow-up (T3). For the yes-and-no questions, proportions of change were calculated; and for the rating of effort, the proportions of answers above five on the ten-point scale were calculated. Such calculations were made for each embedded group separately (CP N = 5 and SB N = 5) and for the combined group (all ten participants). The persons who did not complete the intervention were not interviewed (in line with the ethical guidelines issued by the Regional Ethical Review Board of Gothenburg, Sweden); the information about their reasons for withdrawing come from spontaneous statements made by them when announcing their withdrawal. Because of the case-study design of the study, no intention-to-treat procedure was used.
Efficacy (i.e., goal attainment and functional changes in the participants’ skill levels, societal participation, and executive functions) was evaluated as differences between T1 and T2 and between T1 and T3 in scores on the COPM (self-ratings of performance and satisfaction with performance), on the Swedish version of the OSA and on the AMPS, as well as differences between T1 and T3 in scores on the DEX and the Tower test. The analysis was carried out in four steps: (i) individual calculation of each participant’s results to identify clinically relevant changes for each measurement; (ii) calculation of proportions of clinically relevant changes in the combined group; (iii) calculation of proportions of clinically relevant changes in each embedded group (to explore trends and differences in proportions between the two diagnoses); and (iv) calculation, for the COPM, the DEX, and the Tower test, of medians of the changes in scale score and investigation of changes in statistical significance over time using the Wilcoxson signed-rank test; and, for the Tower test, calculation of differences between groups using the Mann–Whitney U test (the significance level was set to p < 0.05 for all tests). Non-parametric statistical methods were used owing to the small sample size and because all tests used to produce data at an ordinal data level.
Adaptation (i.e., adherence to the CO-OP manual and adaptations needed for use in these new groups of patients) was evaluated by linking the meaningful units in the content of each participant’s three goals to the International Classification of Functioning and Health [Citation43], using the linking rules described by Cieza et al. [Citation59]. The domains and codes identified in the classification were compared with the types of goals described in the CO-OP manual [Citation23]. The field notes written by the therapists were scrutinised to find differences and instances of adaptation of the intervention compared with the CO-OP manual [Citation23] and the CO-OP fidelity scale [Citation53].
Expansion (i.e., how well the intervention matches organisational goals and culture) was evaluated through analysis of the core values expressed in official (policy) documents about care and habilitation in Sweden compared with the CO-OP core values [Citation23,Citation54–58].
Results
Acceptability
Acceptability from the participants’ perspective was high, according to the answers from the structured-interview questions. All participants (10/10) found CO-OP to be meaningful both post-intervention (T2) and six months later (T3). At T2, 56% of the participants (5/9, one answer missing) said that they had used the global strategy in a new situation or new activities. This increased to 80% (8/10) who said that they had applied the strategy to a new situation at T3. CO-OP was deemed strenuous by 4/10 participants at T2 (i.e., effort rated >5 on a 10-point scale ranging from “no effort at all” to “very great effort”). Participants with CP were more likely than those with SB to find the approach strenuous. Further, at T2, participants found that the intervention period was worth the effort for almost all goals (28/30), and at T3 this was so for all goals (30/30) ().
Table 2. Results: structured interviews.
The three persons who did not complete the whole intervention period cited different reasons for this: one of them very quickly (after one/two sessions) reached her two most important goals and so saw no reason to continue, one got a medical condition that prevented him from continuing and one chose to withdraw as the treatment sessions were interfering too much with his schoolwork. Of the three persons who withdrew, one had CP with MACS level III while the other two had demographics corresponding to the study group (one had SB and one had CP with MACS level I).
Efficacy
Goal attainment
A considerable improvement was seen in self-rated performance and satisfaction with performance of the goals for the combined group: 29/30 goals were rated as having improved to a clinically significant extent, i.e., with a difference of ≥2 points, between T1 and T2. At T3, after six months, participants still rated 29/30 goals as having improved in performance and 28/30 as having improved in satisfaction compared with the baseline (). The median difference in performance ratings was a five-point increase on the ten-point COPM scale, both between T1 and T2 and between T1 and T3. The corresponding figure for satisfaction with performance was a six-point increase both between T1 and T2 and between T1 and T3 (). The differences for performance and satisfaction showed statistical significance (p < 0.0001 through-out) between T1 and T2 and between T1 and T3 ().
Table 3. Results: proportions of change in outcome measures.
Table 4. Results: differences in goal attainment and body function, combined group.
Activity and participation
Self-rated participation as measured with the Swedish version of the OSA was higher for 3/9 participants (one rating missing) between T1 and T2 and between T1 and T3. In most cases, there was no change either immediately after the intervention or at follow-up, but one person (in the CP embedded group) had a lower rating at T3 than at T1.
When it comes to activity-performance skills as measured by the AMPS, in 8/10 participants the motor logits did not change by more than 2 SEs between T1 and T2, and 9/10 participants also had motor logits at T3 which were within 2 SEs of what they had at T1. For process skills, 8/10 did not change either from T1 to T2 or from T1 to T3. Two participants (one from each embedded group) had process logits at both T2 and T3 which exceeded their T1 values by more than 2 SEs ().
Body functions
As regards the self-rated amount of executive-function problems measured using the DEX, all participants with SB and 3/5 with CP reported less problems at T3 than at T1 (). Two participants, both with CP, had a higher level of self-rated executive problems at follow-up. The result for the combined group was not statistically significant ( and ). For the combined group, the median total score was 29.0 at baseline (IQR 14.25–31.0) and 22.0 at the six-month follow-up (IQR 12.75–29.5) (lower score meaning less problems) (). At baseline, the SB group had a median total DEX score of 30.0 while the CP group had a median of 15.0. At follow-up, both groups had a median of 22.0 but they still varied in IQR: 16.5–36.5 for the SB group and 8.5–30.0 for the CP group.
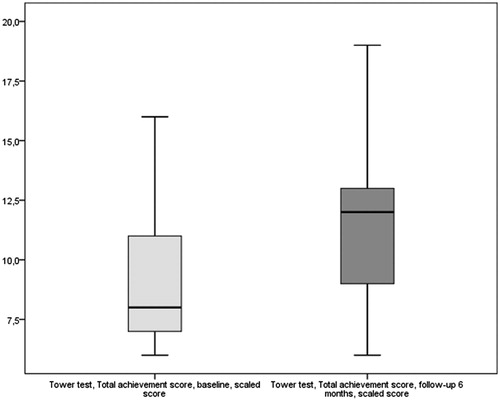
Planning ability measured with the Tower test, 9/10 participants showed improved performance as regards planning ability. One person with a CP diagnosis remained at the same level on both assessments (). The total-achievement scaled score yielded a median of 8.0 (IQR 6.75–11.0) for the combined group at baseline and a median of 12.0 (IQR 9.0–13.0) at follow-up (higher score meaning better planning ability). This difference was statistically significant (, ). At baseline, the median scaled score was 8.0 (IQR 8.0–10.0) for the SB group and 7.0 (IQR 6.0–13.5) for the CP group. At follow-up, both groups had improved: the median scaled score of the SB group was 11.0 (IQR 10.0–13.0) and that of the CP group was 13.0 (IQR 7.5–16.0).
Adaptation
All 30 goals identified by the participants related to the International Classification of Functioning and Health domain of activity and participation. They were in most cases highly complex and did not always involve motor performance – examples include “have good routines at home” and “start my catheterisation procedure on time without anyone reminding me” () – but they did not differ from the goals described in the CO-OP manual. The nature of the goals had an effect on the guiding process during the sessions, as the therapist was often not able to attend the actual performance of an activity, which would frequently be embedded in a daily routine and hence could not be performed during a therapy session. For such goals, guidance was provided through a discussion with the participants, intended to enable them to formulate one or two plans that they could try out between sessions and that would be followed up, again through discussion, at the next session. However, each participant had at least one goal that was more concrete in nature, enabling the therapist to provide guidance during real-time performance. The fact that the performance of many goals was not observable during therapy sessions made it difficult to use the performance quality rating scale as an outcome measure; hence it is not reported in this study. Most of the sessions took place in everyday-life settings, such as the participant’s home or a setting chosen for the purpose (e.g., an urban setting for the goal of “finding my way home from the city”) ().
Table 5. Goals linked to international classification of functioning, disability, and health – child and youth version.
All field notes were found to correspond positively with the CO-OP fidelity scale. The therapists used all of the domain-specific strategies described in the CO-OP manual (i.e., body position, attention to doing, task specification/modification, supplementing task knowledge, feeling the movement, verbal motor mnemonic, and verbal rote script) in their guiding of the participants’ skill acquisition. Further, one of the additional domain-specific strategies used in other adult studies, visualisation, was also used. No new domain-specific strategies emerged in this study. Six out of ten participants in this study involved a significant other during the CO-OP intervention period. Parents, partners, social workers at the habilitation centre, and assistants were chosen as significant others. Three participants with CP and one with SB did not have any significant other involved. As the participants were adults or in their late teens, significant others were not invited to the intervention session until the participants had decided that they should be. Instead, the significant others were informed either in conjunction with the session or during a special meeting also attended by the participant.
Expansion
CO-OP fits well with the culture obtaining in the existing Swedish organisation in that it matches its core values, which stress the importance of involving the client/patient in decision-making and treatment planning and which focus on participation. The habilitation centre of the Västra Götaland Region states on its website that the aim of habilitation is to “strengthen patients, enable them to handle their situation and provide tools and strategies to compensate for their disabilities”. The National Network of Swedish Habilitation Services describes habilitation in Sweden using the same wording, and on the website of the habilitation services of Stockholm County Council it is declared that, “in contacts with the habilitation and health services, children and adults with disabilities should be made to take active part in their habilitation to the widest possible extent”.
The Swedish Patient Act strongly emphasises the patient’s right to participate in all decisions about the care that he or she will be receiving. This is in accordance with CO-OP, for which “the main focus is helping clients to learn to perform the everyday activities (achieve the functional goals) that are important and meaningful to them”. The United Nations Convention on the Rights of Persons with Disabilities, which has been ratified by the Swedish government, also stresses the importance of individual autonomy, including the freedom to make one’s own choices. Article 19 of the convention recognises “the equal right of all persons with disabilities to live in the community, with choices equal to others, and their full inclusion and participation in the community”. CO-OP is compatible with all of the above requirements setting out what should be offered to people with disabilities in Sweden.
Triangulation
Triangulation was performed to corroborate data from different perspectives and hence obtain an overall picture of the feasibility of the CO-OP Approach for young adults with CP or SB in Sweden. This was done for all data and was carried out from different perspectives, using different data sources, within different analysis areas and over time. Triangulation of data from the different outcome measures showed that self-rated goal attainment and executive functions improved significantly and that satisfaction with CO-OP was very high in that the participants found it meaningful and worth the effort. Triangulation of data over time showed that the proportion of participants claiming to use the global strategy was higher at the six-month follow-up (T3) than at post-intervention (T2) and that the high levels of improvement in self-rated performance and satisfaction with performance persisted, indicating that the effects are durable and even evolve over time. Triangulation of different core values and official documents showed that CO-OP was highly compatible with the core values of the Swedish habilitation services. The overall outcome of triangulation from the various perspectives was that CO-OP is a feasible approach for adolescents and young adults with CP or SB in Sweden.
Discussion
This feasibility study shows that CO-OP is a promising approach for enabling adolescents and young adults with CP (MACS levels I–II) or SB to achieve their personal activity goals and to enhance their planning skills and ability to use strategies when performing activities. The approach is compatible with the current habilitation philosophy in Sweden, and the participants found it to be highly meaningful and useful in their everyday lives. The feasibility of CO-OP for the groups in question and in a Swedish context has been shown to be good. While finding evidence of effectiveness was not the primary aim of this pilot study, it is worth noting that the size of the change in the COPM rating, the results from the interviews and the changes seen for executive functions all indicate that CO-OP is a powerful approach for adolescents and young adults both with CP (MACS levels I–II) and with SB.
All 10 participants found CO-OP to be highly meaningful and major changes in self-perceived goal-attainment were achieved. This may be due to the client-centred nature of CO-OP, which places the person’s own goals in focus and gives the person the opportunity to lead the intervention process [Citation23]. Studies have shown that if a person is involved in the intervention process, his or her engagement increases [Citation28], and also that goal-setting in itself enhances the person’s engagement in the intervention [Citation19]. Engagement is seen as closely related to meaningfulness and meaning, purpose, and choice is of essential importance to the value that people assign to different situations in life [Citation60].
In the case of young adults with CP and SB, task-specific models, such as “life-skills training” [Citation61] are mentioned as useful methods to help them gain independence. Many of these models are based on the argument that adolescents/young adults with neurodevelopmental disabilities have had few opportunities to gain experience and practice, meaning that habilitation professionals need to offer them training in the form of more opportunities to learn skills [Citation61]. However, having more opportunities might not always be the whole answer. Indeed, skills training and goal-setting are not always enough when a person has executive difficulties, which may hinder performance [Citation38,Citation62]. A person who is able to do something in one context may not be able to do it in another [Citation4,Citation63]. The meta-cognitive component (the global strategy) of CO-OP adds a crucial dimension to skills training [Citation38] in that it aims to facilitate the generalisation of skills learned in one context and the transfer of the global strategy to new activities in new situations.
The use of the global strategy (Goal-Plan-Do-Check) is assumed to enhance a person’s ability to solve new activity problems [Citation64]. The steps of the CO-OP global strategy greatly resemble key features identified in the literature as crucial for fostering problem-solving through meta-cognitive thinking [Citation65,Citation66], such as planning, monitoring, and evaluating. Eight of 10 participants in this study claimed at the six-month follow-up that they had used the global strategy to overcome new performance problems. This suggests that the approach was effective in its aim to enhance problem-solving, and it also shows that the effect is sustained over time. Indeed, the fact that more participants claimed to use the global strategy at the six-month follow-up than did so post-intervention is noteworthy, suggesting that the participants may need some time to incorporate the new way of thinking into their everyday lives [Citation28]. Another factor that could have contributed to the good results achieved, in terms of the transfer of the global strategy of CO-OP to new activities is that most of the training was provided in a natural setting, familiar to each person, as this is considered to help enhance generalisation and transfer [Citation67].
The positive changes seen in executive functions are encouraging. There was a tendency for persons with SB to experience more dysexecutive problems than the CP group initially; the CP group reported a rather low level of executive problems at baseline. At follow-up, both groups reported problems at the same level. Interestingly, two participants in the CP group rated themselves as having a higher degree of executive problems at follow-up than at baseline. The reason for describing more executive problems after treatment might be a growing awareness of one’s own situation and level of skills for managing various life situations [Citation68]. The difference between the self-ratings on DEX at baseline and at the six-month follow-up was not statistically significant, probably owing to the ratings of those two participants, which exerted a disproportionate impact in the small sample studied.
According to the neuropsychological assessment performed using the Tower test, the participants with CP seemed to improve their planning ability somewhat more than the participants with SB, but even so improvement was a strong common trend for both groups.
Hammel [Citation60] states that the ability to orchestrate activities in everyday life creates a sense of control, and that the individual’s control over his or her performance of activities is central to the experience of quality of life. People who feel that they have a strategy for solving new problems and that they are able to take control over new situations – as the participants in this study claimed that they did – may also have greater self-efficacy [Citation69]. According to van der Slot et al. [Citation6], self-efficacy enables participation. The results from both the interview questions and the test of executive functions do suggest that there may be an effect on self-efficacy, even though this was not measured explicitly. However, the results from the OSA did not show any great improvement in perceived overall participation in everyday life, even though the participants had answered that they used the global strategy to solve new activity problems in their daily lives. This seemingly paradoxical finding is interesting. When asked about their competence to perform (i.e., to participate in different activity-related situations in life), most of the participants did not change their ratings between the baseline and the end of the intervention or the six-month follow-up; one participant even indicated a lower rating. This might be due to a “response shift”, such as described by Schwartz et al. [Citation68] and by Baracaly-Goddard et al. [Citation70]: some of the participants may have rated their participation rather highly at baseline but may then have reconsidered their opinion about themselves after the CO-OP intervention period as they became more aware of their actual abilities and may thus have changed their expectations. On the other hand, it could also be that extended use of the global strategy did not actually enhance the experience of participation for some participants or that it did enhance their experience but the OSA did not capture this change. However, it is intriguing that, at the six-month follow-up, 80% of the participants claimed that they had extended their use of the global strategy and rated their executive function as having improved, whereas only 33% of them rated their participation as having improved. This finding has given the authors reason to reconsider the issue of how to evaluate the effects of CO-OP when it comes to generalisation and transfer in a future randomised controlled study: perhaps evaluation of self-efficacy should be used instead of self-rated participation?
The other outcome measure relating to activity/participation, the AMPS, was hypothesised to show improvements in the quality of performance of well-known, self-chosen tasks as result of transfer, and generalisation of CO-OP skills. However, this outcome measure showed little or no improvements, which is probably due to the operationalisation of the AMPS [Citation48]. In the AMPS, the observer (the occupational therapist) must note any problems that occur during the participant’s performance even if they occur only once. Through the CO-OP, participants develop their ability to change strategies when encountering problems. Accordingly, a person may make several “mistakes” but then correct him- or herself or find a new way of doing things without this being captured by the AMPS. As a result, we have chosen not to use the AMPS in the planned randomised controlled study. The transfer effect is clearly difficult to evaluate. Other CO-OP studies [Citation5,Citation71] have used untrained goals, set at baseline, to capture this effect.
CO-OP, although originally developed for children with developmental co-ordination disorder [Citation23], can be seen as generic in that it does not address any one skill or deficit and also in that it is not carried out according to a fixed manual [Citation37]. However, the approach does have seven key features which have to be used properly, in accordance with the fidelity scale of the CO-OP [Citation53]. The review by Scammell et al. [Citation33] describes how both adaptations and expansions were made when CO-OP was used for new populations (i.e., other than children with developmental coordination disorder. In this study, only a few adaptations were made, and all of them had already been mentioned by Scammell et al. [Citation33]. They were all minor adaptations relating to the participants’ chosen goals or to the involvement of significant others.
Study strengths and limitations
This study has some limitations, such as a small sample size and the lack of a control group. Larger, randomised studies are needed to evaluate the effectiveness of CO-OP compared with existing treatments and to evaluate differences between the CP and SB groups. Even so, the size of the improvements in goal achievement shown in this pilot study and the positive results of the executive-function tests showed that the method is promising for both groups. Further research is warranted to deepen our understanding of how executive difficulties affect the ability of individuals with CP and SB to transfer the global strategy and also to study the issue of generalisation and transfer.
Conclusions
The CO-OP Approach is a feasible approach for adolescents and young adults with SB or CP (MACS levels I–II) in Sweden. It is a promising approach for enabling young people with those congenital diagnoses to achieve their personal goals and to enhance their occupational performance and executive functioning through strategy use. Even though four out of 10 participants found the approach strenuous, all ten participants found the intervention with CO-OP meaningful and worth the effort. The study indicates that CO-OP might improve both planning ability and self-perceived executive functions.
Acknowledgements
The authors would like to thank the 10 persons who participated in the study. The authors gratefully acknowledge this support.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Stubberud J, Riemer G. Problematic psychosocial adaptation and executive dysfunction in women and men with myelomeningocele. Disabil Rehabil. 2012;34:740–746.
- Lindsay S, McPherson AC, Maxwell J. Perspectives of school-work transitions among youth with spina bifida, their parents and health care providers. Disabil Rehabil. 2017;39:641–652.
- Sandstrom K. The lived body: experiences from adults with cerebral palsy. Clin Rehabil. 2007;21:432–441.
- Bergqvist L, Ohrvall AM, Himmelmann K, et al. When I do, I become someone: experiences of occupational performance in young adults with cerebral palsy. Disabil Rehabil. 2017. DOI:10.1080/09638288.2017.1390696
- Cameron D, Craig T, Edwards B, et al. Cognitive orientation to daily occupational performance (CO-OP): a new approach for children with cerebral palsy. Phys Occup Ther Pediatr. 2017;37:183–198.
- van der Slot WMA, Nieuwenhuijsen C, van den Berg-Emons RJG, et al. Participation and health-related quality of life in adults with spastic bilateral cerebral palsy and the role of self-efficacy. J Rehabil Med. 2010;42:528.
- Andren E, Grimby G. Dependence in daily activities and life satisfaction in adult subjects with cerebral palsy or spina bifida: a follow-up study. Disabil Rehabil. 2004;26:528–536.
- Law MC, Darrah J, Pollock N, et al. Focus on function: a cluster, randomized controlled trial comparing child- versus context-focused intervention for young children with cerebral palsy. Dev Med Child Neurol. 2011;53:621–629.
- Bodimeade HL, Whittingham K, Lloyd O, et al. Executive function in children and adolescents with unilateral cerebral palsy. Dev Med Child Neurol. 2013;55:926–933.
- Bottcher L. Children with spastic cerebral palsy, their cognitive functioning, and social participation: a review. Child Neuropsychol. 2010;16:209–228.
- Tuminello ER, Holmbeck GN, Olson R. Executive functions in adolescents with spina bifida: relations with autonomy development and parental intrusiveness. Child Neuropsychol. 2012;18:105–124.
- Dennis M, Barnes MA. The cognitive phenotype of spina bifida meningomyelocele. Dev Disabil Res Rev. 2010;16:31–39.
- Lezak MD, Howieson DB, Bigler ED, Tranel D. Neuropsychological assessment. 5th ed. Oxford: University Press Inc; 2012.
- Peny-Dahlstrand M. A model for the process of task performance to explain difficulties’ in daily life in persons with spina bifida. J Pediatr Rehabil Med. 2017;10:S23–S25.
- Harvey S, Goudvis A. Strategies that work: teaching comprehension for understanding and engagement. 2nd ed. Portland (ME): Stenhouse Publishers; 2007.
- Toglia JP, Rodger SA, Polatajko HJ. Anatomy of cognitive strategies: a therapist’s primer for enabling occupational performance. Can J Occup Ther. 2012;79:225–236.
- Novak I, McIntyre S, Morgan C, et al. A systematic review of interventions for children with cerebral palsy: state of the evidence. Dev Med Child Neurol. 2013;55:885–910.
- Lowing K, Bexelius A, Brogren Carlberg E. Activity focused and goal directed therapy for children with cerebral palsy–do goals make a difference? Disabil Rehabil. 2009;31:1808–1816.
- Miller C, Bauman J. Goal setting: an integral component of effective diabetes care. Curr Diab Rep. 2014;14:509.
- Barker RN, Sealey CJ, Polley ML, et al. Impact of a person-centred community rehabilitation service on outcomes for individuals with a neurological condition. Disabil Rehabil. 2017;39:1136–1142.
- Stubberud J, Langenbahn D, Levine B, et al. Goal Management Training improves everyday executive functioning for persons with spina bifida: self-and informant reports six months post-training. Neuropsychol Rehabil. 2014;24:26–60.
- Donlau M, Mattsson S, Glad-Mattsson G. Children with myelomeningocele and independence in the toilet activity: a pilot study. Scand J Occup Ther. 2013;20:64–70.
- Polatajko HJ, Mandich AD. Enabling occupation in children: the Cognitive Orientation to daily Occupational Performance (CO-OP) approach. Ottawa, Canada: CAOT Publications ACE; 2004.
- Martini R, Polatajko HJ. Verbal self-guidance as a treatment approach for children with developmental coordination disorder: a systematic replication study. OTJR Occup Part Health. 1998;18:157–181.
- Jokic CS, Polatajko H, Whitebread D. Self-regulation as a mediator in motor learning: the effect of the cognitive orientation to occupational performance approach on children with DCD. Adap Phys Act Quart. 2013;30:103–126.
- Thornton A, Licari M, Reid S, et al. Cognitive Orientation to (Daily) Occupational Performance intervention leads to improvements in impairments, activity and participation in children with Developmental Coordination Disorder. Disabil Rehabil. 2016;38:979–986.
- McEwen S, Polatajko H, Baum C, et al. Combined cognitive-strategy and task-specific training improve transfer to untrained activities in subacute stroke: an exploratory randomized controlled trial. Neurorehabil Neural Repair. 2015;29:526–536.
- Poulin V, Korner-Bitensky N, Bherer L, et al. Comparison of two cognitive interventions for adults experiencing executive dysfunction post-stroke: a pilot study. Disabil Rehabil. 2017;39:1–13.
- Wolf TJ, Polatajko H, Baum C, et al. Combined cognitive-strategy and task-specific training affects cognition and upper-extremity function in subacute stroke: an exploratory randomized controlled trial. Am J Occup Ther. 2016;70:7002290010p1–7002290010p1-p10.
- Dawson DR, Binns MA, Hunt A, et al. Occupation-based strategy training for adults with traumatic brain injury: a pilot study. Arch Phys Med Rehabil. 2013;94:1959–1963.
- Gharebaghy S, Rassafiani M, Cameron D. Effect of cognitive intervention on children with ADHD. Phys Occup Ther Pediatr. 2015;35:13–23.
- Jackman M, Novak I, Lannin N, et al. Parents’ experience of undertaking an intensive cognitive orientation to daily occupational performance (CO-OP) group for children with cerebral palsy. Disabil Rehabil. 2017;39:1018–1024.
- Scammell EM, Bates SV, Houldin A, et al. The cognitive orientation to daily occupational performance (CO-OP): a scoping review. Can J Occup Ther. 2016;83:216–225.
- Bowen DJ, Kreuter M, Spring B, et al. How we design feasibility studies. Am J Prev Med. 2009;36:452–457.
- Yin RK. Case study research design and methods. 5th ed. London: SAGE Publications, Inc; 2013.
- Curtin M, Fossey E. Appraising the trustworthiness of qualitative studies: guidelines for occupational therapists. Aust Occ Ther J. 2007;54:88–94.
- Polatajko HJ, Mandich AD, Missiuna C, et al. Cognitive orientation to daily occupational performance (CO-OP): part III–the protocol in brief. Phys Occup Ther Pediatr. 2001;20:107–123.
- Skidmore ER, Holm MB, Whyte EM, et al. The feasibility of meta-cognitive strategy training in acute inpatient stroke rehabilitation: case report. Neuropsychol Rehabil. 2011;21:208–223.
- Law M, Baptiste S, Carswell A, et al. COPM Canadian occupational performance measure. 5th ed. Ottawa, Canada: CAOT Publications ACE; 2014.
- Martini R, Rios J, Polatajko H, et al. The performance quality rating scale (PQRS): reliability, convergent validity, and internal responsiveness for two scoring systems. Disabil Rehabil. 2015;37:231–238.
- Eliasson AC, Krumlinde-Sundholm L, Rosblad B, et al. The Manual Ability Classification System (MACS) for children with cerebral palsy: scale development and evidence of validity and reliability. Dev Med Child Neurol. 2006;48:549–554.
- Law M, Baptiste S, Carswell A, et al. COPM Canadian occupational performance measure. 4th ed. Nacka, Sweden: Förbundet Sveriges Arbetsterapeuter; 2006.
- World Health Organization. International classification of functioning, disability and health: children & youth version: ICF-CY. Geneva: World Health Organization; 2007.
- Baron K, Kielhofner G, Goldhammar V, et al. Min Mening: ett självskattningsinstrument med fokus på aktivitetsförmåga, fysisk och social miljö, värderingar och prioriteringar. 2.2 ed. In: Sjöberg EM, editor. Nacka, Sweden: Förbundet Sveriges Arbetsterapeuter; 2012.
- Baron K, Kielhofner G, Goldhammar V, et al. Occupational self assessment (OSA). Chicago (IL): University of Illinois; 2006.
- Kielhofner G, Forsyth K. Measurement properties of a client self-report for treatment planning and documenting therapy outcomes. Scand J Occup Ther. 2001;8:131–139.
- Kielhofner G, Dobria L, Forsyth K, et al. The occupational self assessment: stability and the ability to detect change over time. OTJR. 2010;30:11–19.
- Fisher AG, K. BJ Assessments of motor and process skills: volume 1 - development, standardization, and administration manual. 7th ed. Fort Collins, Colorado: Three Star Press Inc; 2011.
- Kottorp A, Bernspang B, Fisher AG. Validity of a performance assessment of activities of daily living for people with developmental disabilities. J Intellect Disabil Res. 2003;47:597–605.
- Wilson BA, Alderman N, Burgess PW, et al. Behavioural assessment of the dysexecutive syndrome manual. Bury St Edmunds, England: Thames Valley Test Company; 1996.
- Delis D, Kaplan D, Kramer JH. Delis-kaplan executive function system, D-KEFS, examiners manual. San Antonio (TX): Psychological Corporation; 2001.
- Wechsler D. WAIS-IV technical and interpretive manual. 4 ed. San Antonio (TX): Pearson; 2008.
- McEwen S, Polatajko H, Wolf T, et al. CO-OP fidelity checklist: CO-OP academy; 2012 [updated 2015 Feb; cited 2017 Aug 21]. Available from: http://co-opacademy.ca/wp-content/uploads/2016/03/CO-OPFidelityChecklistApril92015FINAL.pdf
- S. Riksdag Patientlagen (SFS 2014:821) [Internet] Stockholm: Socialdepartementet; 2014 [cited 2017 Nov 02]. Available from: https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/patientlag-2014821_sfs-2014-821
- United Nations. United nations convention on the rights of persons with disabilities: united nations; 2006 [updated 2017 Nov 02]. Available from: https://www.un.org/development/desa/disabilities/convention-on-the-rights-of-persons-with-disabilities.html
- Habilitering-&-Hälsa. Habiliteringen [internet] Göteborg: Habilitering & Hälsa Västra Götalandsregionen; [updated 2017 Oct 18]. Available from: http://www.vgregion.se/f/habilitering-och-halsa/om-habilitering-halsa/verksamhet/habiliteringen/
- Habilitering-&-Hälsa. Habilitering och andra insatser [internet] Stockholm: Habilitering & Hälsa Stockholms läns landsting; 2016 [updated Jun 29]. Available from: http://habilitering.se/habilitering-och-andra-insatser
- Föreningen Sveriges Habiliteringschefer. Habilitering Stockholm: Föreningen Sveriges Habiliteringschefer; [Internet] 2007–2017. Available from: http://habiliteringisverige.se/habilitering/om-hab
- Cieza A, Geyh S, Chatterji S, et al. ICF linking rules: an update based on lessons learned. J Rehabil Med. 2005;37:212–218.
- Hammell KW. Dimensions of meaning in the occupations of daily life. Can J Occup Ther. 2004;71:296–305.
- Kingsnorth S, Healy H, Macarthur C. Preparing for adulthood: a systematic review of life skill programs for youth with physical disabilities. J Adolesc Health. 2007;41:323–332.
- Jacobson LA, Tarazi RA, McCurdy MD, et al. The Kennedy Krieger Independence Scales-Spina Bifida Version: a measure of executive components of self-management. Rehabil Psychol. 2013;58:98–105.
- Toglia J, Johnston MV, Goverover Y, et al. A multicontext approach to promoting transfer of strategy use and self regulation after brain injury: an exploratory study. Brain Inj. 2010;24:664–677.
- McEwen SE, Polatajko HJ, Davis JA, et al. ‘There’s a real plan here, and I am responsible for that plan’: participant experiences with a novel cognitive-based treatment approach for adults living with chronic stroke. Disabil Rehabil. 2010;32:541–550.
- Muir T, Beswick K, Williamson J. Approaches to problem solving: developing an understanding of naive, routine and sophisticated problem solving behaviours, The psychology of problem solving: an interdisciplinary approach. New York (NY): Nova Science Publishers, Inc; 2013.
- Kim YR, Park MS, Moore TJ, et al. Multiple levels of metacognition and their elicitation through complex problem-solving tasks. J Math Behav. 2013;32:377–396.
- Powell J, Heslin J, Greenwood R. Community based rehabilitation after severe traumatic brain injury: a randomised controlled trial. J Neurol Neurosurg Psychiatry. 2002;72:193–202.
- Schwartz CE, Andresen EM, Nosek MA, et al. Response shift theory: important implications for measuring quality of life in people with disability. Arch Phys Med Rehabil. 2007;88:529–536.
- Bandura A. Self-efficacy the exercise of control. New York (NY): W.H Freeman and Company; 1997.
- Barclay-Goddard R, Epstein JD, Mayo NE. Response shift: a brief overview and proposed research priorities. Qual Life Res. 2009;18:335–346.
- Dawson DR, Gaya A, Hunt A, et al. Using the cognitive orientation to occupational performance (CO-OP) with adults with executive dysfunction following traumatic brain injury. Can J Occup Ther. 2009;76:115–127.