Abstract
Purpose
The aim of this study is to systematically review and critically assess the methodological quality of literature regarding prevalence, characteristics and factors influencing pain, other than phantom limb pain (PLP) in persons with lower limb amputation (LLA).
Materials and methods
A systematic review was performed (PROSPERO CRD42019138018). Literature was searched using PubMed, EMBASE, PsycINFO, and PEDro. Studies were included if describing pain other than PLP at least three months after amputation. For residual limb pain (RLP) and back pain, a meta-regression was performed.
Results
Fifty-one studies were included in which predominantly young males with a unilateral traumatic amputation using a prosthesis were investigated. Pooled prevalence of RLP was 0.51 (95% CI 0.40–0.62) with a positive association with presence of back pain (p = 0.044) in the univariate meta-regression. Pooled prevalence of back pain was 0.55 (95% CI 0.45–0.64), with a positive association of time since amputation (p < 0.001) and co-occurrence of RLP (p = 0.050).
Conclusions
Back pain and RLP are common after LLA. The prevalence of back pain was positively associated with the presence of RLP, and vice versa. Future studies should give more attention to other chronic pain types, to persons with a diabetic or vascular cause of amputation, and to pain-related interference.
Both back pain and residual limb pain occur in more than 50% of persons with lower limb amputation (LLA), and both pain types are positively associated.
Clinicians should be aware that chronic pain is common after LLA and can have a significant impact on the functioning of persons with LLA.
Future research on this topic should give more attention to other chronic pain types, to persons with a diabetic or vascular cause of amputation, and to pain-related interference.
Implications for Rehabilitation
Introduction
Chronic pain, specific and non-specific, is common after lower limb amputation (LLA) [Citation1]. Chronic pain is defined as recurrent or persistent pain which persists past the normal time of healing. Three months is the most common applied division between acute and chronic pain [Citation2]. Most of the post-amputation pain literature has focused on phantom limb pain (PLP), and to a lesser extent on residual limb pain (RLP). Phantom limb pain is defined as painful sensations in the missing part of the limb [Citation2]. Residual limb pain is pain in the part of the amputated limb that is still present [Citation2]. Residual limb pain can be prosthesis-related, neurogenic, arthrogenic, vascular, osteogenic including heterotopic ossification, dermatogenic, sympathogenic, referred, and can be related to wound problems [Citation3]. In literature, these types of pain are seldom distinguished [Citation4,Citation5]. In addition to RLP and PLP, recently more and more attention has been given to other types of pain occurring after LLA. Back pain seems to be occurring more frequently in persons with LLA compared to the general population [Citation6]. The exact cause is unknown, but biomechanical factors like leg length discrepancy, spinal movement during prosthetic gait, prosthesis type, skeletal muscle atrophy, and strength loss may play a role [Citation7–10]. Other, again less investigated pain types are knee pain and hip pain, in both the prosthetic leg and the contralateral leg. All mentioned pain types seem to occur frequently and can have a significant impact on the functioning of persons with LLA [Citation5,Citation6,Citation11]. Pain-related interference seems to vary depending on the type of pain and the number of pain sites [Citation12,Citation13]. Pain can significantly impact the health-related quality of life of persons with LLA [Citation14]. Additionally, experiencing multiple pain conditions can negatively influence the psychosocial adjustment to LLA [Citation15].
To the best of our knowledge, no overview of the literature of pain types other than PLP exists, therefore, the extent of the problem is currently unknown. Such an overview could inform the clinician working with persons with LLA concerning the prevalence and characteristics of the different kind of pain types, and possible influencing factors for these pain types. Furthermore, this overview could reveal possible gaps in knowledge concerning pain in persons with LLA, which in return provides directions for future research.
Therefore, the aim of this study was to systematically review and to critically assess the methodological quality of the literature regarding the prevalence, characteristics and factors influencing pain, other than PLP in persons with LLA, and to perform a meta-regression if sufficient data were present.
Materials and methods
Study identification and selection
This systematic review and meta-analysis was reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (Supplemental file 1) [Citation16]. A systematic literature search was performed in PubMed, EMBASE, PsycINFO, and PEDro from inception to April 2020. The search was performed using database specific keywords and free text words associated with amputation, lower extremity, including all amputation levels, and pain (Supplemental file 2). In PEDro, no database specific keywords were available. Therefore, 12 different combinations of free text words were used (Supplemental file 2). An information specialist has assisted with the preparations of the search. No restrictions to publication year were made. The protocol for this systematic review was registered on PROSPERO (Central Registration Depository: CRD42019138018).
Studies were selected in two rounds. In the first round, titles and abstracts were assessed. In the second round, full-texts were assessed. Two observers (MO, JHBG) assessed independently all studies at each stage of the review according to our predefined inclusion and exclusion criteria. Only studies that were excluded by both observers were removed. If opinions differed, agreement through discussion was reached. When disagreement remained, a third observer (PUD) provided a binding verdict. The reason of exclusion was recorded for the full-text selection. As measure of agreement, Cohen’s kappa was calculated between the two observers for both stages of the selection process.
The adjusted cross-sectional/prevalence checklist of the Agency for Healthcare Research and Quality (AHRQ), was used by two authors independently to assess risk of bias assessment of the included studies (Supplemental file 3) [Citation17,Citation18]. We decided to use this checklist due to its focus on quality assessment of cross-sectional studies.
Inclusion and exclusion criteria
Observational studies were included if the sample size was at least 10 persons with LLA (Syme amputation or more proximal up to hemipelvectomy), and if describing any type of pain (RLP and/or back pain, and/or any other type of pain) present at least three months after amputation, with type and location of pain being specified. The number of 10 persons per study was chosen because studies of this small size would have a great uncertainty in estimated pain prevalence (wide 95% confidence intervals) and would not be of added value to our review. Excluded were experimental or laboratory studies, expert opinions, case reports, case series, letters to the editor, reviews, and studies written in a language other than English, Dutch, or German. Studies were also excluded if containing only data about PLP, and if pain was studied related to the effectiveness of an intervention. Furthermore, studies solely describing amputation due to complex regional pain syndrome (CRPS) were excluded, because these data have been described in a recent systematic review [Citation19].
Summary data extraction
Studies were assessed for design, subject characteristics, and level of functioning. Pain prevalence, pain frequency, pain intensity, and pain impact were grouped according to RLP, back pain, and other types of pain. If data were not presented in the studies, authors were requested by e-mail to provide additional information.
Pain prevalence was grouped by reason for amputation and level of amputation; unilateral above knee amputation including knee-disarticulation and more proximal amputation levels up to hemipelvectomy, unilateral below knee amputation including transtibial amputation and Syme amputation, and bilateral amputation including any bilateral amputation between Syme amputation and hemipelvectomy level.
Descriptive statistics were calculated in IBM SPSS Statistics 23 (Armonk, NY). A meta-analysis, random effects model, was performed with prevalence as outcome variables for RLP and back pain, using Comprehensive Meta-Analysis version 3. We used a random effects model because of clinical and methodological heterogeneity between studies. Studies were included in the meta-analysis when presenting outcome and potential predictors for RLP and/or back pain. Potential predictors of back pain and RLP were explored for the association with the reported prevalence of back pain and RLP univariately. The following potential predictors were explored: mean age of the study population, time since amputation, proportion traumatic amputations, proportion vascular amputations, proportion males, proportion of persons using a prosthesis, proportion below knee amputations, proportion above knee amputations, proportion bilateral amputations, proportion RLP/back pain and publication year. Studies did not need to report all these data to be included in the analyses. Due to lack of data we could not take other potential predictors into account. No within-study data were available for all studies, therefore only between-study data were taken into account. Logit event rates (natural logarithm of (prevalence/1 – prevalence) were used to prevent the disproportionately weighing of proportions at the lower and higher range. Funnel plots were not made because of a clinical and methodological heterogeneity between included studies. Outliers, however, were explored for their impact on reported prevalence using Comprehensive Meta-Analysis version 3. All p values were two-sided, with p ≤ 0.05 considered statistically significant.
Results
Study characteristics
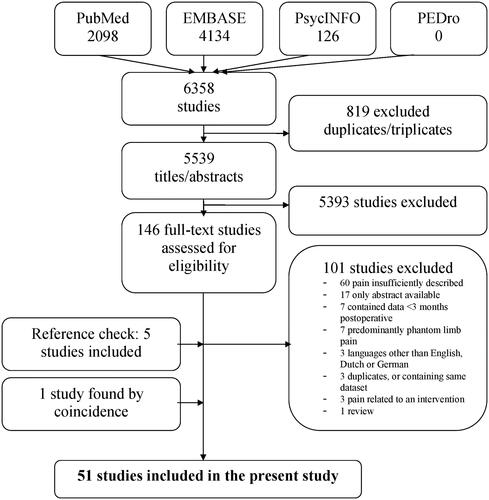
In total, 5539 studies were identified after excluding duplicates and triplicates (). After screening by title and abstract, 5393 studies were excluded (Kappa 0.451, absolute agreement 0.973). After full-text screening, another 101 studies were excluded (Kappa 0.674, absolute agreement 0.844). Five studies were included after a reference check of the included studies. One study was found by coincidence, not stating any keywords in title or abstract. In total, 51 studies were included in this review. Three times two studies used the same dataset. Data per pair were combined in the table and meta-regression [Citation5,Citation6,Citation20–23]. Nine authors were requested to provide additional data [Citation4,Citation5,Citation24–30]. Three authors responded to our request and their data were processed in the analyses [Citation5,Citation26,Citation27]. Five studies used a retrospective cohort design [Citation11,Citation31–34], three studies a prospective cohort design [Citation25,Citation35,Citation36], one study was a secondary analysis of a randomized clinical trial () [Citation25]. All other studies were cross-sectional in design. Persons were most often identified in hospital and rehabilitation center registries, in some studies specific national databases were used. In most studies, questionnaires were sent to participants to gather the necessary data. Two studies used International Classification of Diseases Ninth or Tenth Revision codes (ICD-9 or ICD-10) [Citation33,Citation34].
Table 1. Study and patient characteristics.
Patient characteristics
Regarding RLP and back pain, number of persons ranged from 19 to 1569 per study, in total 10 201 persons. The weighted mean ± SD (standard deviation) age of study persons was 51 ± 10 years, ranging from 23 to 73 years. The weighted mean ± SD time since amputation was 15 ± 7 years, ranging from 0.4 to 32 years. The median proportion prosthesis use was 0.98 (IQR 0.80–1.00), the median proportion male gender 0.82 (IQR 0.70–0.99). Most persons had undergone a traumatic amputation with a weighted mean proportion of 0.68, followed by the proportion vascular cause of 0.20, and a proportion diabetic cause of 0.08. A mean weighted proportion of 0.51 had undergone an above knee amputation, a mean proportion of 0.40 a below knee amputation, and a mean proportion of 0.08 a bilateral amputation.
Risk of bias assessment
Inter observer agreement of the risk of bias assessment expressed as kappa was 0.897 (absolute agreement 0.946). The mean score of the quality assessment was 6.8, ranging from 3 to 11 points out of 12 possible points (Supplemental file 3). In 22 out of the 51 studies, time frame of inclusion was reported. Exclusion criteria were reported in 26 out of 51 studies. Subjects were recruited consecutively or population based in 20 studies. Confounding was assessed and controlled for in 32 out of 51 studies, 12 studies reported missing data.
Residual limb pain
Thirty-three studies reported on RLP in persons with LLA (n = 7062). The reported RLP prevalence in the individual studies ranged from 6% to 92% (). Eighteen studies reported RLP within a certain timeframe, ranging from only actual pain to pain during the last three months (). Residual limb pain was mostly reported as being intermittent in 61–87% of persons and as constant in the remaining persons [Citation5,Citation42,Citation43,Citation49,Citation53]. Residual limb pain episodes occurred four times per week or less in most of the persons; however, a frequency of more than four per week was reported in 30–42% of persons [Citation5,Citation15,Citation49]. If being reported, the episodes of pain lasted mostly less than one to two hours [Citation5,Citation15,Citation43,Citation49,Citation53]. However, several studies reported a considerable amount of persons with longer lasting RLP, varying from a duration of several hours in 18% of persons, more than several hours in 34% of persons, and more than one day in 21% of persons in different studies [Citation5,Citation43,Citation49].
Table 2. Residual limb pain: prevalence, pain characteristics, and causes.
The mean RLP intensity scores ranged from 1.7 to 5.7 on a 10-point NRS between the studies, with the majority of studies reporting intensity scores of 5 or higher [Citation4,Citation5,Citation13,Citation25,Citation26,Citation28,Citation49,Citation59,Citation62]. Severe pain intensity was reported in 30–38% of persons [Citation4,Citation5,Citation41], with 27–33% of persons reporting a severe or extreme bothersome RLP [Citation4,Citation5,Citation15]. One study found a small decrease of intensity in RLP over time, with a mean intensity of 2.5 at six months, 2.5 at 12 months, and 2.1 at 24 months after amputation [Citation25]. Residual limb pain intensity declined by 30% or more for 56% of persons, and increased by 30% or more for 22% of persons during the course of two years. Another study found a greater RLP intensity in the dysvascular group of persons with LLA compared to the traumatic and diabetic groups, and suggested a more proximal arterial disease resulting in ischemic pain as the reason for this difference [Citation49].
Few studies reported about the impact of RLP on the functioning of persons with LLA. Pain-related interference assessed on a 10-point scale was 2.9 for ADL, 2.8 for social life, and 3.9 for ability to work in one study [Citation49]. Comparable results were reported in other studies [Citation5,Citation32,Citation43,Citation53]. Pain-related interference in persons with a knee disarticulation compared to persons with a transfemoral or transtibial amputation did not differ significantly, but groups were small [Citation13].
Few studies evaluated the cause of RLP (). If reported, a neuroma was found in 3–50% of persons [Citation22,Citation23,Citation40,Citation57], a prosthetic problem in 42–52% of persons [Citation26,Citation49], bone overgrowth in 20% of persons [Citation22,Citation23], ulcers and/or scar hypersensitivity in 10–20% of persons [Citation22,Citation23], and foreign bodies in 2.5% of persons [Citation23]. Although several other studies did mention the presence of prosthetic and skin problems, no association with RLP was reported. None of the studies specifically reported ischemic pain as cause of RLP.
Back pain
Twenty-nine studies reported on back pain in persons with LLA (n = 7887). The prevalence of back pain ranged from 34% to 95% (). Twelve studies reported back pain within a certain timeframe, ranging from only actual pain to pain during the last six months (). Some studies reported on back pain in different regions. One study found the highest prevalence of lumbar spine pain (72%), followed by cervical spine pain (45%), thoracic spine pain (32%), and sacral pain (17%) [Citation55]. Another study found that 53% of persons reported lumbosacral spine pain, 18% neck spine pain, and 10% thoracic spine pain [Citation21]. Furthermore, 67% of persons experienced pain in one area, 28% in two areas, and 5% in three areas. The other included studies predominantly reported low back pain [Citation4–6,Citation8,Citation12,Citation13,Citation22,Citation24,Citation27,Citation29,Citation33,Citation37–39,Citation41,Citation44–52,Citation60,Citation62]. Several studies reported data about the experienced pain frequency [Citation6,Citation8,Citation27,Citation45,Citation47,Citation49]. Similar to RLP, back pain was reported as intermittent in 70–91% of persons, constant in the remaining persons [Citation6,Citation8,Citation27,Citation45,Citation47,Citation49]. Frequency of back pain episodes was usually low, often not more than three times a week. The duration of back pain episodes ranged from up to one hour in 66% of persons [Citation49], to several hours or more in 58% of persons in another study [Citation6].
Table 3. Back pain: prevalence, pain characteristics, and causes.
The reported mean back pain intensity of the included studies ranged from NRS 3.0 to 5.3 [Citation5,Citation6,Citation13,Citation46,Citation49,Citation62]. Several studies reported moderate back pain in 5–35% of persons, severe back pain in 14–39% of persons, with one study reporting extreme back pain in 11% of persons [Citation6,Citation27,Citation41,Citation46,Citation47,Citation52]. Three studies reported back pain interference on a 0–10 scale, all reporting scores in the mild range: back pain interference with ADL ranged from 2.9 to 3.9, with social activities 3.4 to 3.8, with work 3.4 to 4.0 [Citation6,Citation13,Citation49].
Few studies evaluated possible causes of back pain related to amputation (). In one study, postural and gait abnormalities were thought to be the possible cause of back pain in 53% of persons [Citation41]. An older study stated that persons with LLA with low back pain had significantly greater leg length discrepancies than those without pain [Citation8]. A more recent study did not find any differences in lumbar range of motion, leg length, body mass index, and magnetic resonance imaging findings, comparing persons with LLA with and without back pain [Citation47]. Some studies did assess the presence of pelvic tilt or a scoliosis, but these findings were not related to the presence of back pain either [Citation37,Citation38].
Other pain
An overview of all the studies reporting other types of chronic pain is presented in Supplemental file 4. Due to the small number of studies, these data were not included in the meta-regression.
Pain in the non-amputated limb
Pain in the non-amputated limb was found in 25–71% of persons [Citation4,Citation5,Citation27,Citation31,Citation39,Citation42,Citation44,Citation50,Citation52,Citation58,Citation61,Citation62]. Seven studies reported contralateral limb pain within a certain timeframe, ranging from only actual pain to pain during the last three months (Supplemental file 4). Two studies reported the presence of vascular and wound problems in the non-amputated limb in some of the persons with LLA, but not specifically related to the presence of pain [Citation31,Citation42]. In general, causes were not specifically stated. Intensity of pain in the non-amputated limb varied from 31% for moderate pain and 19% for severe pain, to 46% moderate or worse severity/reduction in quality of life [Citation4,Citation44].
Hip pain
Hip pain was found in 3–37% of persons [Citation8,Citation22,Citation23,Citation37,Citation55,Citation62]. One study reported hip pain in the last three months (Supplemental file 4). Causes of hip pain were not specifically stated. One study reported hip pain intensity of moderate or more in 30% of persons [Citation37].
Knee pain
Knee pain was found in 9–81% of persons, if stated 9–15% on the ipsilateral side, 19–68% on the contralateral side of the amputation [Citation8,Citation11,Citation12,Citation22–24,Citation37,Citation38,Citation55,Citation62]. Another study found a prevalence of contralateral knee pain in 40% of persons with LLA, compared to 20% knee pain in a control group of persons without an amputation [Citation11]. Three studies reported knee pain within a certain timeframe, ranging from pain during the last week to pain during the last month (Supplemental file 4). The prevalence of symptomatic knee osteoarthritis was 16% in the group of persons with LLA versus 12% in the control group without an amputation. Two studies reported about knee pain intensity, with a moderate knee pain in 32% of persons in the first study, and an average NRS of 4.9 in the second study [Citation11,Citation37].
Meta-analysis
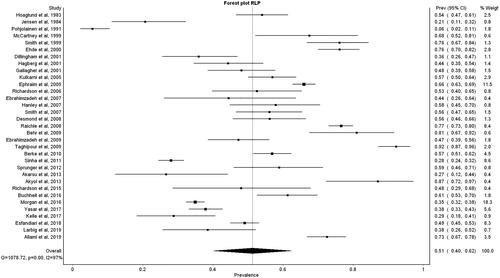
The meta-analysis included 46 studies reporting about back pain or RLP in a total of 10 201 persons with LLA. Not all included studies reported on all predictors explored in meta-regression (). For RLP (33 studies, n = 7062), a pooled mean prevalence of 0.51 (95% CI 0.40–0.62) was found (I2 = 97%) (). In the meta-regression to statistically predict the logit event rate of RLP, only a positive association between the proportion back pain (p = 0.044) was found in the univariate regression model (). Too few studies reported about pain intensity and interference, hence these data could not be included in the meta-regression.
Table 4. Results of meta-regression to explore which study characteristics are associated with the logit of RLP and logit of back pain: random effects model.
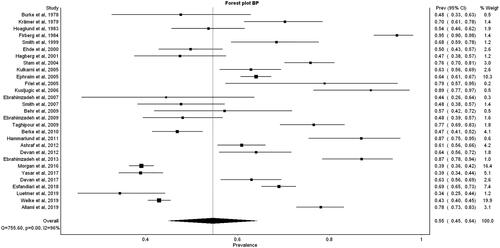
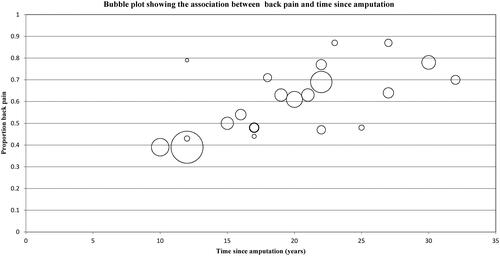
For back pain (29 studies, n = 7887), we found a mean pooled prevalence rate of 0.55 (95% CI 0.45–0.64) (I2=96%) (). The univariate regression model showed a higher prevalence of back pain with a longer time since amputation (p < 0.001), male gender (p = 0.006), and a traumatic cause of amputation (p < 0.001) (; ). Furthermore, we found a borderline significant positive association between the proportion back pain and the co-occurrence of RLP (p = 0.050). Only few studies reported about pain intensity and interference, these data could not be included in the meta-analysis.
In a post hoc analysis, we calculated Pearson’s r between proportion RLP and proportion back pain in the different studies (r = 0.75), indicating a strong correlation between the prevalence of RLP and back pain.
Discussion
The aim of this study was to systematically review and to critically assess the methodological quality of the literature regarding the prevalence, characteristics and factors influencing chronic pain, other than PLP in persons with LLA. We found a pooled prevalence for RLP of 0.51, with a positive association with the presence of back pain in the univariate regression analysis. The cause of RLP was seldom adequately described. For back pain, we found a pooled prevalence of 0.55 with a positive association of the time since amputation, male gender, traumatic cause of amputation and the co-occurrence of RLP in the univariate regression analysis. Only few studies reported about other types of pain, and pain impact in general.
In our RLP meta-regression, we found a significant positive association with the proportion back pain. In the back pain meta-regression, we found a borderline significant positive association with the proportion RLP. We did not find significant outcomes in both directions, possibly explained by the relatively small sample size we had to work with. Our findings however still suggest a strong association between the prevalence of RLP and back pain in LLA, also supported by the strong correlation we demonstrated in our post hoc analysis. The underlying mechanism could be related to the measurement instrument used. Another explanation might be a biomechanical explanation for the association between RLP and back pain in persons with LLA. The presence of RLP might influence the gait pattern, perhaps influencing pelvic and spinal movement, which could lead to back pain in the longer term [Citation9,Citation63]. These alterations in movement patterns could also be explained by fear of pain (fear avoidance or pain driving change in gait) due to changes to functional connectivity and sensorimotor integration, as suggested in chronic low back pain in the general population [Citation64].
Further elaborating on this, sensitization might be an explanation for the correlation between RLP and back pain in our study population. Peripheral sensitization represents a reduction in threshold and an amplification in the responsiveness of nociceptors which occurs when the peripheral terminals of these high-threshold primary sensory neurons are exposed to inflammatory mediators and damaged tissue. Peripheral sensitization is restricted to the primary site of tissue injury [Citation65,Citation66]. Central sensitization is defined as an amplification of neural signaling within the central nervous system that elicits pain hypersensitivity and as an increased responsiveness of nociceptive neurons in the central nervous system to their normal afferent input [Citation67,Citation68]. Peripheral and central sensitization nowadays are well-established neurophysiological mechanisms in chronic pain in general [Citation66]. In literature focusing on pain after LLA, central sensitization is only linked to PLP [Citation69].
Considering the positive association of “time since amputation” in our back pain meta-regression, several explanations are present. Biomechanically, it can be hypothesized that prolonged use of a prosthesis might influence the gait pattern which could increase susceptibility for development of back pain. By contrast, the prevalence of back pain might also increase due to the increase of physical inactivity during the process of aging. The process of aging in general might play the same role in aging adults without LLA. A systematic review focusing on the trends of back pain prevalence with age in the general population indeed stated that most included studies considering severe forms of back pain found an increase of prevalence with increasing age [Citation70]. Further elaborating on this, the question remains in which way LLA influences the risk of experiencing back pain. In the recent history, various surveys have been performed to identify the prevalence of low back pain in the general population, showing an estimated prevalence ranging from 22 to 48%, depending on the study population and definitions applied [Citation71–74]. The age distribution of those studies was relatively comparable to our study population, with the proportion male gender however being overrepresented in our study population. This can be explained by the fact that our study population predominantly consisted of war veterans with a traumatic LLA. Taking this into account, the mean pooled prevalence of back pain in our study turned out to be higher in comparison with the previously reported back pain prevalence in the general population. Four of the included studies in our systematic review retrospectively analyzed the back pain prevalence before LLA. Three studies found that only 10–20% of persons with back pain retrospectively recalled experiencing back pain before their amputation, compared to 50–87% after amputation [Citation6,Citation51,Citation62]. One study focusing on persons with transfemoral amputation found a slightly increased frequency of ICD-9 back pain codes postamputation [Citation33]. This study also found a statistically significant increased frequency of back pain events in persons with a dysvascular transfemoral amputation in comparison with a matched control group. For persons with a non-dysvascular cause of amputation, no significant differences were found, the sample size of this group was small however.
In our back pain meta-regression, we found a positive association with male gender and traumatic cause of amputation. As stated earlier, most of our study database consisted of male persons (median proportion 0.82) with LLA due to traumatic reasons (mean proportion 0.68). For this reason, these findings should be interpreted with great caution. No other associations between back pain and cause of LLA were found. Furthermore, no associations between cause of LLA and presence of RLP were found. The proportion of persons with LLA due to vascular reasons in the reviewed studies turned out to be relatively small. RLP could also be a sign of vascular claudication and therefore might be leading to a re-amputation, which happens relatively frequent in persons with LLA due to vascular reasons [Citation75]. This finding might have further influenced the reported prevalence of RLP in the long term.
No association between amputation level and the prevalence of RLP or back pain was found in this review. Thus, we could not confirm the results of the regression analyses performed in other studies on RLP and on back pain, in which such an association was found [Citation4,Citation41].
A recent systematic review focused on summarizing evidence on physical and social determinants for health-related quality of life in veterans with LLA [Citation14]. It found back pain to be one of the determining factors for quality of life, based on two studies also included in our review [Citation20,Citation50]. RLP did not prove to be a determining factor in that review. A meta-analysis could not be performed in that review. Comparing these findings with our data, we did find a higher prevalence of back pain compared to RLP in our pooled data. Our reported RLP and back pain intensity and impact were similar as well. However that systematic review focused solely on veterans with LLA, and we did not specifically take quality of life data into account.
In an expert review, it was stated that back pain is a frequent and bothersome secondary complaint [Citation9]. Our findings underline that statement. We also found a considerable prevalence of contralateral limb pain; knee and hip pain was indeed reported more at the contralateral side. It has been proposed that persons with LLA tend to favor their intact limb which causes more stress on the contralateral side, which makes persons with LLA twice as likely to develop pain in the intact limb [Citation11]. Due to the low amount of studies reporting hip and knee pain, we were not able to confirm this proposed mechanism. As mentioned before, other factors besides the biomechanical aspect as neurophysiological and personal factors could possibly play a role in the experiencing of pain after LLA [Citation64]. Furthermore, our data concerning the cause of the different pain types turned out to be limited and non-conclusive.
The findings presented in this review provide patient and clinician working with persons with LLA with data about pain characteristics of the different chronic pain types other than PLP, and factors related to these pain types. Besides this, this study also provides insight in areas of the field in which the current available knowledge is lacking.
Future studies on this topic should systematically distinguish different pain intensities, preferably using the same cut-off values. We would also like to suggest that future prevalence studies on this topic include pain-related interference as an outcome variable. More information about pain intensity and pain-related interference would provide more insight in the impact of pain on the functioning of persons with LLA [Citation76]. Apart from the possible moderators studied in the present review, factors like health-related quality of life, coping strategy and psychological well-being could also have an important impact on the experienced RLP and back pain in persons with LLA. Next to this, future studies should also give more attention to other chronic pain types than RLP, back pain and PLP, as those pain types could have a significant impact on the functioning of persons with LLA as well. Also, more attention should be given to pain in persons with LLA due to diabetic and vascular reasons, considering the underrepresentation of these categories in the current literature. Finally, more attention should be given to central sensitization in persons with pain after LLA.
Study limitations
The conclusions of this review are limited by the quality and reporting of the source publications, and should therefore be interpreted with caution. The majority of included studies had a poor methodological quality. As mentioned earlier in our risk of bias assessment, aspects like timeframe of inclusion and exclusion criteria were often poorly reported. Subjects were mostly not recruited consecutively, and missing data were mostly not reported. Many studies did not distinguish pain characteristics per amputation level. The timeframe in which pain had to be present varied widely, which may have impacted negatively on pooling of results in our meta-regression. Furthermore, some studies only reported pain if being frequent or always present, or being of high intensity, while other studies reported any intensity and frequency, and some studies used ICD-9 or ICD-10 codes instead of questionnaires or interviews. Most included studies used a cross-sectional design. A large proportion of the study population of the included studies consisted of relatively young male persons with traumatic LLA. As could be a consequence, the proportion prosthesis use in this systematic review was high. A considerable amount of studies in our review excluded persons not using a prosthesis, or only included persons with LLA in prosthetic clinics. Therefore, caution should be taken to generalize the outcomes of this review to the general population of persons with LLA, especially concerning the elderly patient with LLA due to vascular reasons who does not or seldom uses a prosthesis [Citation77].
Furthermore, a considerable amount of studies did not report every predictor of our regression model, which might have contributed to varying and sometimes contradictory outcomes. Interpreting the results of the meta-regression, the reader should be aware that the meta-regression is based on aggregated data and not on individual patient data, thus influence of confounding variables on the associations found cannot be analyzed on a patient level. Thus, regression coefficients are based on between-study variations and weights of the studies included.
During our last search update, we excluded a study reporting on pain and quality of life after amputation in children. While we did not specifically document this in our study protocol, in previous searches we had always focused on adult persons and wanted to prevent additional heterogeneity within our dataset.
Finally, by excluding all studies reporting only PLP during our study selection, some RLP data may have been lost. More importantly, we did not expect to find an association between RLP and back pain with a central sensitization mechanism as a possible explanation. By excluding studies reporting only PLP, we were not able to investigate if the presence of RLP and back pain was associated with the presence of PLP as well.
Conclusions
Chronic back pain and RLP are common after LLA, back pain being more prevalent than RLP. The presence of back pain is positively associated with the presence of RLP, and vice versa. Furthermore, the prevalence of back pain is positively influenced by the time since amputation. Future studies should give more attention to other chronic pain types such as hip pain, knee pain, and pain in the contralateral limb, and to persons with a diabetic or vascular cause of amputation. Finally, more attention should be given to pain-related interference.
Additional_file_4.docx
Download MS Word (18.4 KB)Additional_file_3.docx
Download MS Word (24.1 KB)Additional_file_2.docx
Download MS Word (17.1 KB)Additional_file_1.doc
Download MS Word (65.5 KB)Acknowledgements
The authors thank all the authors of the studies included in our review. In particular, the authors thank Hemakumar Devan PhD and Kevin J. Gertz MPA, on behalf of Ms KA Raichle, PhD and Professor DM Ehde, PhD, for providing us with additional data.
Part of this study material was presented at the Dutch Congress of Rehabilitation Medicine on Friday April 13th 2018.
Disclosure statement
The authors report no conflicts of interest.
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- Czerniecki JM, Ehde DM. Chronic pain after low extremity amputation. Crit Rev Phys Rehabil Med. 2003;15(3–4):24–332.
- Loeser JD. Classification of chronic pain. 2nd ed. (revised). Descriptions of chronic pain syndromes and definitions of pain terms. Washington, USA: IASP Press. International Association for the Study of Pain; 2011.
- Davis RW. Phantom sensation, phantom pain, and stump pain. Arch Phys Med Rehabil. 1993;74(1):79–91.
- Ephraim PL, Wegener ST, MacKenzie EJ, et al. Phantom pain, residual limb pain, and back pain in amputees: results of a national survey. Arch Phys Med Rehabil. 2005;86(10):1910–1919.
- Ehde DM, Czerniecki JM, Smith DG, et al. Chronic phantom sensations, phantom pain, residual limb pain, and other regional pain after lower limb amputation. Arch Phys Med Rehabil. 2000;81(8):1039–1044.
- Ehde DM, Smith DG, Czerniecki JM, et al. Back pain as a secondary disability in persons with lower limb amputations. Arch Phys Med Rehabil. 2001;82(6):731–734.
- Jaegers SM, Arendzen JH, de Jongh HJ. Prosthetic gait of unilateral transfemoral amputees: a kinematic study. Arch Phys Med Rehabil. 1995;76(8):736–743.
- Friberg O. Biomechanical significance of the correct length of lower limb prostheses: a clinical and radiological study. Prosthet Orthot Int. 1984;8(3):124–129.
- Gailey R, Allen K, Castles J, et al. Review of secondary physical conditions associated with lower-limb amputation and long-term prosthesis use. J Rehabil Res Dev. 2008;45(1):15–29.
- Wasser JG, Vincent KR, Herman DC, et al. Potential lower extremity amputation-induced mechanisms of chronic low back pain: role for focused resistance exercise. Disabil Rehabil. 2019. DOI:https://doi.org/10.1080/09638288.2019.1610507
- Norvell DC, Czerniecki JM, Reiber GE, et al. The prevalence of knee pain and symptomatic knee osteoarthritis among veteran traumatic amputees and nonamputees. Arch Phys Med Rehabil. 2005;86(3):487–493.
- Morgan SJ, Friedly JL, Amtmann D, et al. Cross-sectional assessment of factors related to pain intensity and pain interference in lower limb prosthesis users. Arch Phys Med Rehabil. 2017;98(1):105–113.
- Behr J, Friedly J, Molton I, et al. Pain and pain-related interference in adults with lower-limb amputation: comparison of knee-disarticulation, transtibial, and transfemoral surgical sites. J Rehabil Res Dev. 2009;46(7):963–972.
- Christensen J, Ipsen T, Doherty P, et al. Physical and social factors determining quality of life for veterans with lower-limb amputation(s): a systematic review. Disabil Rehabil. 2016;38(24):2345–2353.
- Desmond D, Gallagher P, Henderson-Slater D, et al. Pain and psychosocial adjustment to lower limb amputation amongst prosthesis users. Prosthet Orthot Int. 2008;32(2):244–252.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
- Rostom A, Dubé C, Cranney A, et al. Appendix D. Quality assessment forms. Cross-sectional/prevalence study quality. Rockville (MD): Agency for Healthcare Research and Quality (US). Celiac disease. Evidence reports/technology assessments, no. 104; 2016. Available from: https://www.ncbi.nlm.nih.gov/books/NBK35156/
- Zeng X, Zhang Y, Kwong JS, et al. The methodological quality assessment tools for preclinical and clinical studies, systematic review and meta-analysis, and clinical practice guideline: a systematic review. J Evid Based Med. 2015;8(1):2–10.
- Bodde MI, Dijkstra PU, den Dunnen WF, et al. Therapy-resistant complex regional pain syndrome type I: to amputate or not? J Bone Joint Surg Am. 2011;93:1799–1805.
- Rahimi A, Mousavi B, Soroush M, et al. Pain and health-related quality of life in war veterans with bilateral lower limb amputations. Trauma Mon. 2012;17(2):282–286.
- Ashraf A, Shojaee H, Mousavi B, et al. Impact of pain in vertebral column on activities of daily living in the Iranian amputees with bilateral lower limb amputation. Disabil Rehabil. 2012;34(10):869–872.
- Ebrahimzadeh MH, Fattahi AS. Long-term clinical outcomes of Iranian veterans with unilateral transfemoral amputation. Disabil Rehabil. 2009;31(22):1873–1877.
- Ebrahimzadeh MH, Hariri S. Long-term outcomes of unilateral transtibial amputations. Mil Med. 2009;174(6):593–597.
- Ebrahimzadeh MH, Rajabi MT. Long-term outcomes of patients undergoing war-related amputations of the foot and ankle. J Foot Ankle Surg. 2007;46(6):429–433.
- Hanley MA, Jensen MP, Smith DG, et al. Preamputation pain and acute pain predict chronic pain after lower extremity amputation. J Pain. 2007;8(2):102–109.
- Raichle KA, Hanley MA, Molton I, et al. Prosthesis use in persons with lower- and upper-limb amputation. J Rehabil Res Dev. 2008;45(7):961–972.
- Devan H, Hendrick P, Hale L, et al. Exploring factors influencing low back pain in people with nondysvascular lower limb amputation: a national survey. Pm R. 2017;9(10):949–959.
- Akyol Y, Tander B, Goktepe AS, et al. Quality of life in patients with lower limb amputation: does it affect post-amputation pain, functional status, emotional status and perception of body image? J Musculoskelet Pain. 2013;21(4):334–340.
- Berke GM, Fergason J, Milani JR, et al. Comparison of satisfaction with current prosthetic care in veterans and servicemembers from Vietnam and OIF/OEF conflicts with major traumatic limb loss. J Rehabil Res Dev. 2010;47(4):361–371.
- Sinha R, van den Heuvel WJ, Arokiasamy P. Factors affecting quality of life in lower limb amputees. Prosthet Orthot Int. 2011;35(1):90–96.
- Pohjolainen T. A clinical evaluation of stumps in lower limb amputees. Prosthet Orthot Int. 1991;15(3):178–184.
- McCartney CJL, Charles DHM, Cooper GG, et al. Pain and disability following lower limb amputation – a quantitative and qualitative study. Pain Clin. 1999;11(4):293–300.
- Luetmer M, Mundell B, Kremers HM, et al. Low back pain in adults with transfemoral amputation: a retrospective population-based study. Pm R. 2019;11(9):926–933.
- Welke B, Jakubowitz E, Seehaus F, et al. The prevalence of osteoarthritis: higher risk after transfemoral amputation? A database analysis with 1,569 amputees and matched controls. PLoS One. 2019;14(1):e0210868.
- Richardson C, Glenn S, Nurmikko T, et al. Incidence of phantom phenomena including phantom limb pain 6 months after major lower limb amputation in patients with peripheral vascular disease. Clin J Pain. 2006;22(4):353–358.
- Larbig W, Andoh J, Huse E, et al. Pre- and postoperative predictors of phantom limb pain. Neurosci Lett. 2019;702:44–50.
- Burke MJ, Roman V, Wright V. Bone and joint changes in lower limb amputees. Ann Rheum Dis. 1978;37(3):252–254.
- Kramer J, Heisel JM, Ullrich CH. Late results of patients with amputation of the thigh (author’s transl). Z Orthop Ihre Grenzgeb. 1979;117(5):801–807.
- Hoaglund FT, Jergesen HE, Wilson L, et al. Evaluation of problems and needs of veteran lower-limb amputees in the San Francisco Bay Area during the period 1977–1980. J Rehabil Res Dev. 1983;20:57–71.
- Jensen TS, Krebs B, Nielsen J, et al. Immediate and long-term phantom limb pain in amputees: incidence, clinical characteristics and relationship to pre-amputation limb pain. Pain. 1985;21(3):267–278.
- Smith DG, Ehde DM, Legro MW, et al. Phantom limb, residual limb, and back pain after lower extremity amputations. Clin Orthop Relat Res. 1999;361:29–38.
- Dillingham TR, Pezzin LE, MacKenzie EJ, et al. Use and satisfaction with prosthetic devices among persons with trauma-related amputations: a long-term outcome study. Am J Phys Med Rehabil. 2001;80(8):563–571.
- Gallagher P, Allen D, Maclachlan M. Phantom limb pain and residual limb pain following lower limb amputation: a descriptive analysis. Disabil Rehabil. 2001;23(12):522–530.
- Hagberg K, Branemark R. Consequences of non-vascular trans-femoral amputation: a survey of quality of life, prosthetic use and problems. Prosthet Orthot Int. 2001;25(3):186–194.
- Stam HJ, Dommisse AM, Bussmann HJ. Prevalence of low back pain after transfemoral amputation related to physical activity and other prosthesis-related parameters. Disabil Rehabil. 2004;26(13):794–797.
- Friel K, Domholdt E, Smith DG. Physical and functional measures related to low back pain in individuals with lower-limb amputation: an exploratory pilot study. J Rehabil Res Dev. 2005;42(2):155–166.
- Kulkarni J, Gaine WJ, Buckley JG, et al. Chronic low back pain in traumatic lower limb amputees. Clin Rehabil. 2005;19(1):81–86.
- Kusljugic A, Kapidzic-Durakovic S, Kudumovic Z, et al. Chronic low back pain in individuals with lower-limb amputation. Bosn J Basic Med Sci. 2006;6:67–70.
- Smith E, Comiskey C, Ryall N. Prevalence and patterns of back pain and residual limb pain in lower limb amputees at the National Rehabilitation Hospital. Ir J Med Sci. 2008;177(1):53–57.
- Taghipour H, Moharamzad Y, Mafi AR, et al. Quality of life among veterans with war-related unilateral lower extremity amputation: a long-term survey in a prosthesis center in Iran. J Orthop Trauma. 2009;23:525–530.
- Hammarlund CS, Carlstrom M, Melchior R, et al. Prevalence of back pain, its effect on functional ability and health-related quality of life in lower limb amputees secondary to trauma or tumour: a comparison across three levels of amputation. Prosthet Orthot Int. 2011;35(1):97–105.
- Devan H, Tumilty S, Smith C. Physical activity and lower-back pain in persons with traumatic transfemoral amputation: a national cross-sectional survey. J Rehabil Res Dev. 2012;49(10):1457–1466.
- Sprunger NM, Laferrier JF, Collins DP, et al. Utilization of prostheses and mobility-related assistive technology among service members and veterans from Vietnam and Operation Iraqi Freedom/Operation Enduring Freedom. J Prosthet Orthot. 2012;24:144–152.
- Akarsu S, Tekin L, Safaz I, et al. Quality of life and functionality after lower limb amputations: comparison between uni- vs. bilateral amputee patients. Prosthet Orthot Int. 2013;37(1):9–13.
- Ebrahimzadeh MH, Kachooei AR, Soroush MR, et al. Long-term clinical outcomes of war-related hip disarticulation and transpelvic amputation. J Bone Joint Surg Am. 2013;95:e114.
- Richardson C, Crawford K, Milnes K, et al. A clinical evaluation of postamputation phenomena including phantom limb pain after lower limb amputation in dysvascular patients. Pain Manag Nurs. 2015;16(4):561–569.
- Buchheit T, Van de Ven T, Hsia HL, et al. Pain phenotypes and associated clinical risk factors following traumatic amputation: results from Veterans Integrated Pain Evaluation Research (VIPER). Pain Med. 2016;17(1):149–161.
- George J, Newman JM, Caravella JW, et al. Predicting functional outcomes after above knee amputation for infected total knee arthroplasty. J Arthroplasty. 2017;32(2):532–536.
- Kelle B, Kozanoğlu E, Biçer ÖS, et al. Association between phantom limb complex and the level of amputation in lower limb amputee. Acta Orthop Traumatol Turc. 2017;51(2):142–145.
- Yaşar E, Tok F, Kesikburun S, et al. Epidemiologic data of trauma-related lower limb amputees: a single center 10-year experience. Injury. 2017;48(2):349–352.
- Esfandiari E, Yavari A, Karimi A, et al. Long-term symptoms and function after war-related lower limb amputation: a national cross-sectional study. Acta Orthop Traumatol Turc. 2018;52(5):348–351.
- Allami M, Faraji E, Mohammadzadeh F, et al. Chronic musculoskeletal pain, phantom sensation, phantom and stump pain in veterans with unilateral below-knee amputation. Scand J Pain. 2019;19(4):779–787.
- Devan H, Carman A, Hendrick P, et al. Spinal, pelvic, and hip movement asymmetries in people with lower-limb amputation: systematic review. J Rehabil Res Dev. 2015;52(1):1–19.
- Nijs J, Clark J, Malfliet A, et al. In the spine or in the brain? Recent advances in pain neuroscience applied in the intervention for low back pain. Clin Exp Rheumatol. 2017;35(5):108–115.
- Hucho T, Levine JD. Signaling pathways in sensitization: toward a nociceptor cell biology. Neuron. 2007;55(3):365–376.
- Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. 2009;10(9):895–926.
- Merskey H, Bogduk N. Part III: pain terms, a current list with definitions and notes on usage. In: Merskey H, Bogduk N, editors. Classification of chronic pain. 2nd ed. Seattle (WA): IASP Press; 1994. p. 209–201.
- Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. Pain. 2011;152(3 Suppl.):S2–S15.
- Ahuja V, Thapa D, Ghai B. Strategies for prevention of lower limb post-amputation pain: a clinical narrative review. J Anaesthesiol Clin Pharmacol. 2018;34(4):439–449.
- Dionne CE, Dunn KM, Croft PR. Does back pain prevalence really decrease with increasing age? A systematic review. Age Ageing. 2006;35(3):229–234.
- Cassidy JD, Carroll LJ, Cote P. The Saskatchewan health and back pain survey. The prevalence of low back pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976). 1998;23(17):1860–1866; discussion 1867.
- Deyo RA, Mirza SK, Martin BI. Back pain prevalence and visit rates: estimates from U.S. national surveys, 2002. Spine (Phila Pa 1976). 2006;31(23):2724–2727.
- Skovron ML, Szpalski M, Nordin M, et al. Sociocultural factors and back pain. A population-based study in Belgian adults. Spine (Phila Pa 1976). 1994;19(2):129–137.
- Papageorgiou AC, Croft PR, Ferry S, et al. Estimating the prevalence of low back pain in the general population. Evidence from the South Manchester Back Pain Survey. Spine (Phila Pa 1976). 1995;20(17):1889–1894.
- Izumi Y, Satterfield K, Lee S, et al. Risk of reamputation in diabetic patients stratified by limb and level of amputation: a 10-year observation. Diabetes Care. 2006;29(3):566–570.
- World Health Organization. International Classification of Functioning, Disability and Health (ICF). Geneva: WHO; 2001.
- Fleury AM, Salih SA, Peel NM. Rehabilitation of the older vascular amputee: a review of the literature. Geriatr Gerontol Int. 2013;13(2):264–273.