Abstract
Purpose
To appraise and synthesize evidence from previous systematic reviews (SRs) concerning the impacts of goal setting on engagement in the rehabilitation process and on outcomes of participation and occupational performance for individuals with acquired brain injury (ABI).
Materials and methods
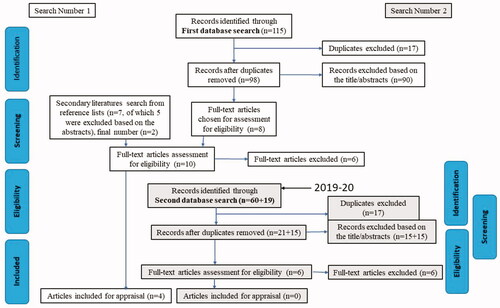
Systematic review of SRs following the preferred reporting items for SRs and meta-analysis guidelines. Sixteen full text articles were assessed for eligibility, from which four were included in the review. The Critical Appraisal Skills Programme checklists for SRs was used to rate quality and risk of bias.
Results
Four SRs of moderate to high quality included a variety of methodologies. Evidence of moderate quality showed clients’ active participation in goal setting had positive impacts on the client and their engagement in the process. Findings suggested that goal-directed interventions, particularly in outpatient rehabilitation, may improve occupational performance. There was some indication that goal setting may support adherence to therapeutic exercises, but relevance to rehabilitation outcomes was less clear. Findings related to participation outcomes were minimal.
Conclusions
Goal setting is a complex and multidimensional process. Goal setting may contribute to improved engagement in rehabilitation although few studies explored occupational performance and participation outcomes for individuals with ABI.
Active goal setting may contribute to improved engagement in rehabilitation, however, including individual clients in the goal setting process requires creativity and flexibility on behalf of professionals.
A model is presented to promote understanding of the personal and environmental barriers and facilitators that may interact with goal setting approaches to promote engagement in rehabilitation.
There is a need for more research exploring impact of active client-centered goal setting on occupational performance and participation outcomes for people with acquired brain injury.
Implications for rehabilitation
Introduction
The willingness and ability of individuals suffering from disability or disease to set goals have been related to his/her need to adapt to the various challenges in their life and thus participate and engage in rehabilitation processes [Citation1]. Engagement is considered vital to rehabilitation processes for more optimal outcomes [Citation2], and should not be viewed as a discrete phase, but rather as a process to be continually renewed in accordance with shifting goals, expectations, and emotional needs [Citation2,Citation3].
Acquired brain injury (ABI) often results in impairments to an individual’s functions and occupational performance and impacts on their performance of activities of daily living (ADL) and participation in meaningful, socio-cultural valued life situations. Following ABI, the outcomes of rehabilitation may be influenced by the level of the individual’s engagement within the therapy process [Citation3]. ABI includes conditions likely comprising a range of cognitive and/or communication disorders which may impact on goal setting markedly. These personal factors are likely to interact with environmental factors and goal setting approaches in differential ways to influence engagement and outcomes. In any intervention, the degree to which a client is ready to engage in rehabilitation (i.e., adheres to therapy protocols) and his/her level of motivation to work toward future goals, is a central issue [Citation4].
Goal-setting has been identified as a critical component contributing to engagement in rehabilitation [Citation2,Citation3]. Rehabilitation goals should be intentionally created, have purpose and be developed with the individuals who will be directly affected by the intervention; reflecting client-centered practice [Citation5]. outlines some key concepts and definitions related to engagement, client-centered practice, ABI, occupational performance, participation, and goal setting used in this study. There are many different approaches to goal setting and the extent of the client involvement varies [Citation5]. However, goal setting is not always explicit or simple [Citation5]. There are challenges in goal setting processes with individuals with ABI because of possible emotional, communication, and cognitive impairments [Citation3,Citation7,Citation8]. Plant et al. explored barriers and facilitators to the goal setting process for people with ABI in a systematic review (SR) [Citation9]. They noted that there were differences in clients’ and staff’s perspectives of goal setting, and client-, staff-, or organization-related barriers [Citation9]. On the other hand, strategies such as individually tailored goal setting processes and strategies promoting communication and understanding, facilitated goal setting [Citation9].
Table 1. Key concepts and definitions.
In a Cochrane review by Levack et al. [Citation5], which included randomized controlled trials (RCTs), there was inconclusive evidence regarding whether goal setting results in improvements in body functions, levels of activity or better engagement in the rehabilitation process in adults with disability. The review however included people with physical impairments and also with mental health conditions. While there are previous SRs exploring both the effects and experiences of goal setting [Citation10–12] or exploring the effectiveness of different interventions where goal setting is a technique amongst other interventions [Citation13], the effects of goal setting on engagement in rehabilitation and influence on outcomes of participation, engagement in ADL and occupational performance have not been highlighted before. Additionally, the populations included in previous studies often include a broad client group [Citation5] or are limited to stroke survivors [Citation10,Citation12] rather than consider individuals with all forms of ABI who are often in similar rehabilitation facilities. This kind of demarcation is important in view of potential varied and complex functional deficits in ABI and especially considering cognitive and/or communication disorders impacting on goal setting, engagement, and subsequent outcomes. Thus, there is a need to identify, evaluate, and synthesize the existing body of completed and recorded research of the impacts of goal setting for individuals with ABI through an SR [Citation14].
The aim of this study therefore is to appraise and synthesize the available evidence from previous SRs concerning the impacts of goal setting on (1) engagement in the rehabilitation process and (2) on rehabilitation outcomes of engagement in ADL, occupational performance, and participation for individuals with ABI. Based on a hypothesis that some positive effects of goal-setting will be identified, a third aim is to consider the barriers and facilitators to the implementation of client-centered goal setting in clinical practice. A model which builds on the theoretical background, previous literature [Citation9], and findings from the SR to consider factors influencing goal setting, engagement, and outcomes of rehabilitation will be proposed to support understanding of the interactions between client and clinical contexts and goal-setting approaches in practice.
Materials and methods
An SR of SRs was undertaken to collate the evidence for goal setting for individuals with ABI. This review follows recommendations for conducting SRs of healthcare interventions [Citation15] and guidelines for reporting of SR of the preferred reporting items for systematic reviews and meta-analysis (PRISMA) checklist [Citation16].
Data collection
The person, intervention, comparison, outcome (PICO) framework was used to focus the research aims and determine the key items and preliminary search terms for data extraction [Citation17]. The Boolean operators AND, OR, NOT, and * (truncations) were used for finding the relevant articles. Search terms thus included ABI or stroke, cerebrovascular accident (CVA), traumatic brain injury (TBI) or brain tumor and goal setting and: engagement or participation, involvement, attendance, adherence, fidelity, or occupational performance.
Comprehensive search of electronic databases MEDLINE (Ebsco), CINAHL (Ebsco), AMED (Ebsco), Cochrane Library, and PsychINFO (ProQuest) was conducted between February and April 2018. The initial searches were carried out for published articles covering the years 1998–2018 following the shift in therapies toward client-centered practice and engagement in intervention [Citation6]. Search terms were adjusted for the different databases (see Supplementary Table S1). The search was conducted in the English language. The search was done in two parts and in the latter one the search strategy was revised, and the terms were expanded to incorporate specific conditions included in ABI (e.g., encephalitis) and terms related to goal setting (e.g., goal planning). However, the second database search, with expanded terms, did not increase the number of included articles. The search was replicated in November 2019 and July 2020 to capture any recent reviews from 2018 to 2020. A further search was undertaken manually based on the reference list of articles selected for the full text review was conducted for any further articles that met the inclusion criteria. The detailed search with search terms is presented in Supplementary Table SI and the search process is presented in .
Inclusion/exclusion criteria
The primary and secondary collection of literature and review of the articles was done by the first author and verified independently by a research expert. Any disagreements regarding study selection were resolved through discussion. The titles, abstracts, or full texts of articles were screened for inclusion reflecting the following criteria: (1) SR as a research design; (2) involved adults 16 years of age or over with acquired brain injuries; (3) explored the impact of goal setting on engagement in rehabilitation and/or on the outcomes of participation and/or occupational performance; (4) the rehabilitation and goal setting were carried out in any settings by any rehabilitation professionals; and, (5) published in peer-reviewed journals.
The studies excluded after full text analysis are presented in the Supplementary Table S2. The studies were excluded if: (1) they did not explicitly examine the impacts of goal setting; (2) they did not separate out the results for goal setting from other interventions in the analysis; (3) the impacts of goal setting for people with ABI were not separated from other populations studied in the SR; and, (4) they related to “if-then” plans upon goals rather than goal setting. “If-then” plans are defined as “implementation intention tools aimed at supporting people to deal more effectively with self-regulatory problems” [Citation18, p.563].
Study selection
From a total of 178 hits in the search, which was conducted in two parts, 16 full text articles were assessed for eligibility (see ). On the full text analysis 12 studies were excluded as 11 [Citation5,Citation9,Citation18–26] of them did not meet the inclusion criteria and one identified SR 27] only included one article related to goal setting and the same article was also included in one of the previously included SRs [Citation11]. Four were selected to be included in the review (). Two of the SRs [Citation10,Citation12] had five studies in common, thus results considered for this review included a total of 47 reported studies. No articles were identified for review from the second part of the search.
Table 2. Overview of reviewed articles.
Assessment of methodological quality
The methodological quality of the included articles was assessed using the Critical Appraisal Skills Programme (CASP) as it enables the systematic assessment of the trustworthiness, results, and relevance of published papers [28]. The main categories in CASP rating for SRs include validity, study inclusion, results, outcomes, and implications. The 10 qualitative claims in the CASP-ratings were converted to points where 0 was equal to “no”, 0,5 “partial/unclear”, and 1 “yes”. The points for each study were summarized and converted to percentages (see ). The quality ratings of 50–74% were considered to be of moderate quality, those of 75% and above strong and with those rated less than 50% considered weak with high risk of bias influencing results [Citation22]. To enhance the reliability of the judgment SRs were independently appraised by three raters (KMK, RC, DG). Consensus in CASP ratings was achieved through discussions.
Table 3. CASP quality rating.
The level of evidence of single SRs was evaluated using the Oxford Centre for Evidence Based Medicine Levels of Evidence (OCEBM) [Citation29] (see and ). It is a ranking system to consider the extent of the evidence according to the quality and results of clinical trials and studies. In the OCEBM, level 1 reflects the most robust studies such as SRs of RCTs of high quality and level 5 refers to the lowest quality such as expert opinion without explicit critical appraisal [Citation29].
Data extraction and synthesis
Considering the aim of this study, relevant information was extracted and highlighted in each single SR. In the SRs with mixed populations only results related to people with ABI were considered. Equally, in SRs where various interventions for people with ABI were explored only results related to goal setting were considered. Based on the aims of this review, the findings from each included SR were grouped in two categories: (1) goal setting in enhancing engagement in rehabilitation and (2) goal setting in improving outcomes of participation and occupational performance (reported based on the definitions set out in ). The findings were then synthetized descriptively. Due to different study designs and diverse reporting of findings in the included SRs, meta-analysis was not possible within the scope of this review.
Results
Study characteristics
The SRs included a variety of methodologies across a total of 98 studies. One consisted of 19 RCTs of which only six studies contained individuals with brain injury [Citation11]. Another SR consisted of 35 studies including four SRs, 10 RCTs, and the remaining 21 quasi-experimental or cohort studies (with one pilot RCT) [Citation13]. Two further SRs consisted of a mix of quantitative and/or qualitative studies. Sugavanam et al. [Citation10] included seven quasi-experimental or cohort studies and two single case studies exploring quantitative outcomes with 11 studies investigating the experiences of goal setting. Rosewilliam et al. [Citation12] contained a mix of one RCT, three cohort studies, one survey, two case reviews and one case series quasi-experimental, one mixed methods study and remaining 18 qualitative studies varying from interviews and conversational analysis to videos, drawings, and focus groups. Participants in the studies reviewed in this SR were predominately adults with stroke, TBI or other acquired brain injuries which were not further specified. Some studies also included health care professionals and carers. Sample sizes within the SR studies varied from 1 to 695 participants, including 44 carers. It was not possible to determine from one of the SRs [Citation11] if participants overlapped between some of the studies and only six of the 19 RCTs involved individuals with brain injuries.
Intervention methods taken to evaluate goal setting approaches or impact of goal setting on rehabilitation differed. Two of the SRs focused on client-centered goal-setting [Citation12] or provision of goals, goal planning or goal management training (GMT) [Citation11] specifically with stroke or TBI populations, with one exploring goal planning across clinical rehabilitation settings and populations [Citation10]. A further SR contrasted rehabilitation outcomes from goal-setting and goal-directed therapy with five other interventions [Citation13]. Outcomes varied across all the studies included in each of the SRs, ranging from length of stay, functional motor skills as well as goal attainment [Citation10]. Goals predominately focused on psychosocial and behavioral outcomes [Citation13] but also included clients’, carers’, and staff’s perceptions of any benefits and experiences [Citation12] or a focus more on adherence and intensity of exercise/therapy practice in additional to goal achievement [Citation11].
The methodological strength varied from weak to strong. The SRs which met the inclusion criteria [Citation10–13] all scored greater than 60% quality rating on the CASP [Citation30], one achieved 75% [Citation13], indicating that the overall quality of the SRs was acceptable. Reasons reducing methodological quality across the SRs were due to: unclear search processes to determine if all relevant articles had been identified; lack of clarity over rationale for combining results across studies (mixed populations in papers or lack of clarity over overlapping samples between studies); insufficient rigor of application of quality appraisal tool, particularly with respect to the validity and reliability of outcome measures; limited precision in reporting of results; and, limited inclusion of all important outcomes (e.g., focus on mobility and self-care rather than participation in domestic life) (see ). The evidence level of included articles was graded at levels 1 and 2 based on OCEBM [Citation29]. Overview of the reviewed articles is presented in .
Findings from the systematic reviews
The findings related to goal setting in enhancing engagement in rehabilitation are reported based on the definition of client engagement set out by Bright et al. [Citation2] as described in . Likewise, the findings related to goal setting in improving outcomes of participation in ADL and occupational performance are based on the definitions explained in .
Goal setting in enhancing engagement in rehabilitation
Goal setting was reported to have either positive or negative impact on therapist-client relationship [Citation10,Citation12]. Two of the SRs reported that there were often discrepancies between individuals with ABI and professionals in perceptions of goal setting [Citation10,Citation12]. For example, situations where clients’ goals were unrealistic in relation to their recovery could lead to conflicts between the client and therapist [Citation12]. The literature from both quantitative and qualitative studies, where the level of evidence was not clearly determined, showed that goal-setting practices were not always client-centered. This means that goals were not set collaboratively between individuals with ABI and professionals, clients’ involvement in the goal setting process was limited or it did not exist [Citation10,Citation12]. This was even though in one qualitative study, included in two of the SRs, professionals reported that client-centered goal setting increased client motivation [Citation10,Citation12]. In three quantitative studies included in one SR, of which two showed moderate and one weak methodologies, and in one qualitative study (lacking confirmability) the clients were often unclear of the purpose of goal setting and their role in the process [Citation10]. This decreased their perception of their participation in goal setting. One speculated reason for this by the authors was that clients were not ready to set goals at the stage (6 months post stroke) [Citation10]. It was reported that in order for clients to be able to be involved in active decision making in goal setting, goals need to be modulated to clients’ participation ability (graded decision making) [Citation12].
Despite the barriers to goal setting, studies suggested that active participation in goal setting was seen as important by clients; particularly as working towards individually customized goals was expected to improve their life situation and helped them feel better psychologically [Citation12]. Within one of the SRs, four high quality RCT studies showed evidence that goal setting improves motivation and adherence to rehabilitation tasks1 [Citation11]. Additionally, there was some quantitative evidence that the use of a formal method in goal setting, such as the Canadian Occupational Performance Measure (COPM), improved individuals’ perception of active participation in goal setting [Citation12] and helped professionals to discern the differences in the goals between professionals and clients [Citation10]. In one quantitative study of weaker methodological quality but within an SR, the participants involved in goal setting were able to recall their treatment goals better and manage more tasks than the comparison group [Citation10].
Goal setting in improving outcomes of participation in ADL and occupational performance
Evidence from two RCTs in a higher quality SR suggests that goal setting, particularly when goal-directed within outpatient rehabilitation after TBI, improves clients’ self-ratings of occupational performance [Citation13]. In the same SR, goal-directed outpatient rehabilitation after TBI is supported by evidence from one RCT, to improve occupational performance and psychosocial reintegration [Citation13]. Additionally, according to a quantitative study within an SR of moderate quality, goal setting improves perceptions of self-care ability [Citation10]. Four high quality RCT studies from an SR rated of moderate quality, suggested that prescribed, specific and difficult goals improve the performance on motor and cognitive activities for people with ABI [Citation11]. Effects of goal setting in recovery were explored in four quantitative studies in the SR by Sugavanam et al. [Citation10]. The COPM was used in two of them of which the quality was weak to moderate. Occupational performance scores improved significantly at discharge indicating goal achievement and recovery. Also, in two case studies (but of low level evidence) where GMT and goal planning approach were applied, positive results were seen for goal achievement indicating recovery [Citation10]. In the same SR, in a prospective follow-up cohort study, goal attainment showed a moderate to strong correlation with perceived level of participation and motor ability at six months post discharge (no significant correlation prior discharge) [Citation10].
Four studies within a further SR including a mix of quantitative and qualitative studies of client-centered goal setting, suggested that once client-centered goals were set and training was adjusted to those goals, it led to short-term improvement in ADL, better global and motor outcomes and better self-perceived occupational performance [Citation12].
Summary of results
Regarding the role goal setting may have in enhancing engagement in rehabilitation, there was moderate evidence showing that when the process of goal setting and the meaning of it was unclear to the clients it weakened their perception of the participation in the goal setting process [Citation10]. Limited evidence showed that goal setting improved adherence to treatment regimens with clients with goals demonstrating greater adherence to the prescribed frequency of exercise and undertaking more or longer exercise sessions, than those without [Citation11]. Additionally, there was some low level evidence that client’s active participation in goal setting had positive impacts on clients and their engagement in the process of rehabilitation [Citation12]. Use of an explicit method in goal setting improved clients’ perception of active participation in goal setting [Citation12].
Regarding whether goal setting may improve outcomes of participation in ADL and occupational performance, there was strong evidence suggesting that the use of goal-directed interventions in outpatient settings may improve participant self-ratings of occupational performance [Citation13] and that prescribed, specific, challenging goals may improve immediate performance on simple tasks/body functions for people with ABI [Citation11]. Moderate evidence suggests that the use of goal-directed outpatient rehabilitation following TBI improves occupational performance, and psychosocial integration [Citation13]. Barriers to goal setting identified restricted communication, cognitive impairments, and/or lack of clarity over the purpose of goal-setting or the client’s perspective of their own role in this process.
Discussion
This review examined the evidence for goal setting to enhance engagement in rehabilitation and improve outcomes of participation in ADL and occupational performance for individuals with ABI. This was done through a systematic search considering previous SRs published between 1998 and June 2020. Four SRs met criteria for inclusion [Citation10–13]. The quality of the SRs was moderate, with one stronger study [Citation13], contributing to OCEBM of levels 1 and 2. Within the SRs the quality of studies was very mixed due to differing methodologies (RCTs, quantitative, qualitative, and case studies).
Although it was not possible to make robust conclusions of the role goal setting has in enhancing engagement due to limitations in reporting of effect sizes, there were results showing that goal setting impacts on therapist–client relationship [Citation10,Citation12] and can therefore impact on engagement in rehabilitation. Similarly, it was not possible to make firm conclusions of the effectiveness of goal setting on participation in ADL and occupational performance in this review; however, in all four SRs, there were results supporting goal setting interventions for improving outcomes of rehabilitation [Citation10–13].
Across the SRs in this study, goal setting was generally acknowledged as a central intervention aiming to increase adherence to therapy protocols and outcomes in rehabilitation [Citation10–13]. In many of the studies included in the SRs, the occupational performance outcomes were measured by clients’ self-ratings and how they perceived the situation. Patient-reported outcome measures are consistent with client-centered approaches for intervention [Citation6]; however, the manner in which goal setting was done, was not clearly articulated across the studies. Despite the recommendations for collaborative problem solving [Citation31] goal setting may not always have been done in agreement with the client [Citation10].
A model illustrating the factors influencing goal setting, engagement and consequent outcomes of rehabilitation is presented in . Previous literature [Citation9] has highlighted that positive attitudes of health professionals and use of specific goal setting approaches are supportive of the use of goal setting in rehabilitation. The findings from the current SR have highlighted the importance of the active involvement of the client and meaningfulness of goals to improve the life situation. Results also indicated that prescribed, specific, challenging goals can improve immediate performance on simple tasks/body functions for people with ABI [Citation11]. This is in congruence with the motivation theory by Locke whereby striving toward difficult goals may bring better results [Citation32]. Yet in the studies within the SR of Levack et al. [Citation11], the goals were mostly given to the clients by the treatment personnel and they were related to simple arithmetic or motor tasks. However, if the goals are suggested to a client by rehabilitation professional it raises a question of meaningfulness. Can they still have an impact on the participation, occupational performance, and well-being of an individual in the long term? In this respect, Plant et al. [Citation9] had previously questioned whether client-led goal setting is desirable during early stages of recovery (acute phase) when some individuals expected to be led by the staff; whereas in later stages, they were able to identify personally significant goals and work on them reflecting more a client-centered goal setting process. This reflects the findings from the SR of Rosewilliam et al. [Citation12] which demonstrated the need for flexibility and individuality when developing an active co-constructed process of engagement that is scaled to individual requirements through graded decision making. This also supports the need for different approaches in goal setting to be used appropriately depending on the stage of rehabilitation process and the situation and individual characteristics of the client and their families.
Figure 2. Model for considering factors influencing goal setting, engagement, and outcomes of rehabilitation.
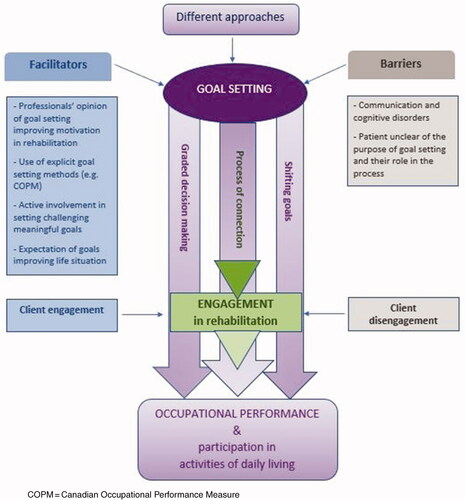
On the other side of the model (see ), barriers to goal setting reflect the findings from moderate evidence showing that when the process of goal setting and the meaning of “the goal” was unclear to the clients, their perception of their role and subsequent participation in goal setting was weakened [Citation10]. Communication and cognitive disorders often co-occur in individuals with ABI restricting involvement of these individuals in goal setting. This presents a challenge as people with communication and cognitive disorders are often excluded in studies related to goal setting [Citation10]. It is crucial to recognize that individuals with ABI may not be able to adopt the goal setting process due to their impairments which may also include a lack of self-awareness [Citation7]. Additionally, according to Bright et al. [Citation30] it is important to be aware that practitioner’s own engagement in service delivery which can equally impact on how the individual experiences rehabilitation and engages in it. Through a process of connection between the client and the professional, the client may move toward or away from a state of engagement [Citation2]. Thus, disengagement is not exclusively a problem of the client – the health care provider may play a vital role [Citation2]. The transactional framework further explains how the interaction with others impacts on engagement [Citation33].
Different approaches can be used for goal setting which can impact on access and uptake as well as engagement and outcomes (see ). Although low quality evidence was found for goal setting to contribute to higher quality of life and self-efficacy in goal pursuit, Levack et al. in their Cochrane review of individuals with a range of disabilities, did not find evidence of an impact on functional abilities or engagement in intervention [Citation5]. When focusing specifically on individuals with BI, our SR identified barriers, such as communication or cognitive impairments may diminish client participation or impair realistic, “best-interest” decision making respectively and thus impact on outcomes. Whereas explicit methods for goal setting, such as the COPM, can be used to facilitate client participation and graded decision making in the goal setting process. Individuals with ABI need information of their condition and the rehabilitation process to enable them to make decisions related to their goals, which may also shift as the process proceeds. The communication between the therapist and the client is central in goal setting and has a role in improving engagement [Citation10,Citation30] (see ).
It is prominent that participation outcomes following goal setting were minimally evident in this review. They were mentioned in only two studies within two SRs in the form of psychosocial reintegration [Citation13] and perceived level of participation [Citation10]. Notably, in one of the SRs [Citation12], it was reported that clients more often chose goals aiming to improve their level of participation whereas, in contrast most of the professionals were focusing on impairments and activity levels. As participation in everyday occupations is seen as vital for all humans [Citation34] and it is described as having a positive influence on health and well-being [Citation35], it is crucial in ABI rehabilitation to pay more attention to these discrepancies between clients and professionals.
In the SR by Rosewilliam et al., it was noted that a high number of the studies related to client-centered practice originated from the profession of occupational therapy where client centeredness is a significant part of the educational training [Citation12]. However, as this review revealed, there are still gaps in including clients in the goal setting process. There is a need for further research to explore the impact of different methods of goal setting on engagement, participation, and occupational performance. Additionally, further education of the rehabilitation professionals about the goal setting process as a whole (barriers/facilitators, the meaning of engagement of professionals, different goal setting approaches and their appropriate use) is required. In rehabilitation practice, it is important to develop ways to increase clients’ understanding of goal setting and the rehabilitation process. Rehabilitation professionals should also consider developing tools to support participation of individuals, particularly those with greater communication or cognitive deficits, in the identification and setting of meaningful, challenging but realistic goals.
Limitations
This SR was conducted in the English language which might have resulted in failure to reach some essential information on the topic, particularly for different cultural contexts. There are arguments that goals will differ between people with stroke and TBI [Citation10] in part due to differences in the age groups of individuals [Citation36]. This has not been taken into consideration in the current review.
A major limitation in the methods of each of the included SRs, was the lack of comparability of included studies; arguably the same can be said of this SR [Citation15]. However, the breadth of papers and methodologies allowed for greater consideration of not only impacts of goal setting, but factors contributing to more effective outcomes. In many of the original articles within the included SRs, the actual extent of clients’ involvement in goal setting was not made clear [Citation10,Citation12] and goal setting was not clearly defined [Citation13]. These facts decrease the accuracy of both the validity and reliability of the findings. In one of the SRs [Citation12], some studies were included in which authors were not clear about the exact number of stroke survivors. Additionally, Levack et al. [Citation11] referred to four studies where one of the authors was common to all of them and the studies were published in brief time intervals between 2001 and 2002 with similar recruitment and sampling strategies across one, two, or three research sites. Therefore, it may be speculated if there was some degree of overlap of the populations in these studies. These questions related to overlap of populations in these studies diminish the strength of the evidence [Citation37].
The overall results of the SRs were not precise, for example, the strength of the evidence was not always explained. Further, the recruitment and sampling of the populations in the SRs were not presented clearly enough to be able to consider the application of the results to the local population (see ). The tools for quality assessment had some limitations which increases the degree of subjectivity in two of the SRs [Citation10,Citation12]. Furthermore, risks of detection and performance bias were present because blinding the participants and personnel was not possible to maintain in many studies [Citation10,Citation13].
Several SRs had to be excluded in this study because findings related to goal setting were not analyzed separately from other interventions or individuals with ABI were not considered independently. It is not known whether including these additional studies would have changed the conclusions of this review. The CASP was used for appraising the included studies in this SR. There are other available tools, such as the Grading of Recommendations Assessment, Development and Evaluation (GRADE) [Citation38], that could also have been used. The CASP was justified because it enabled transparency and comparison between SRs which incorporated different methodologies, along with better consistency and reliability for independently co-rating the studies with colleagues who were using the same tool.
Most of the search, extraction of the data, and documentation were done by one author. Although feedback was actively used, the work accomplished individually may have risk of bias. Despite the limitations described, the current SR provides further evidence of the benefits of goal-setting for individuals with ABI, albeit with some caveats as illustrated in .
Conclusions
This paper highlights the complexity of goal setting in ABI rehabilitation and provides supportive evidence regarding the benefits of goal setting in enhancing the engagement in rehabilitation and outcomes of occupational performance. This review identified limited empirical evidence, both in quantity and quality, that active participation in goal setting may contribute to better engagement in rehabilitation and better outcomes of participation and occupational performance; with the important proviso of the need to consider the individual context within rehabilitation. Highlighted also is the need to understand the role that active involvement plays in goal setting, particularly within various stages of rehabilitation and across different cultures. The extent, to which goal setting on its own makes a difference, is more difficult to unravel due to the multidimensional nature of engagement. Research is warranted to develop new resources that enable those with cognitive and communication disorders to participate actively in goal setting process.
Disclosure statement
This work was undertaken in part fulfillment for a MSc in Occupational Therapy for the first author (maiden name Paloniemi). The authors report no conflicts of interest.
Note
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Notes
1 It is notable that one author was common to all these studies and it is questionable if the population in these studies was partly the same. These four studies were only one hour long experiments and thus of limited relevance to clinical rehabilitation.
References
- Järvikoski A, Härkäpää K. Kuntoutuksen perusteet [principles of rehabilitation]. 5th ed. Helsinki: WSOYpro; 2011.
- Bright FAS, Kayes NM, Worrall L, et al. A conceptual review of engagement in healthcare and rehabilitation. Disabil Rehabil. 2015;37(8):643–654.
- Medley AR, Powell T. Motivational interviewing to promote self-awareness and engagement in rehabilitation following acquired brain injury: a conceptual review. Neuropsychol Rehabil. 2010;20(4):481–508.
- Van den Broek MD. Why does neurorehabilitation fail? J Head Trauma Rehabil. 2005;20(5):464–473.
- Levack WM, Weatherall M, Hay‐Smith EJC, et al. Goal setting and strategies to enhance goal pursuit for adults with acquired disability participating in rehabilitation. Cochrane Database Syst Rev. 2015;7:CD009727.
- Sumsion T. A revised occupational therapy definition of client-centred practice. Br J Occup Ther. 2000;63(7):304–309.
- Ylvisaker M, Mcpherson K, Kayes N, et al. Metaphoric identity mapping: facilitating goal setting and engagement in rehabilitation after traumatic brain injury. Neuropsychol Rehabil. 2008;18(5–6):713–741.
- Parsons J, Plant S, Slark J, et al. How active are patients in setting goals during rehabilitation after stroke? A qualitative study of clinician perceptions. Disabil Rehabil. 2018;40(3):309–316.
- Plant SE, Tyson SF, Kirk S, et al. What are the barriers and facilitators to goal-setting during rehabilitation for stroke and other acquired brain injuries? A systematic review and meta-synthesis. Clin Rehabil. 2016;30(9):921–930.
- Sugavanam T, Mead G, Bulley C, et al. The effects and experiences of goal setting in stroke rehabilitation – a systematic review. Disabil Rehabil. 2013;35(3):177–190.
- Levack WMM, Taylor K, Siegert RJ, et al. Is goal planning in rehabilitation effective? A systematic review. Clin Rehabil. 2006;20(9):739–755.
- Rosewilliam S, Roskell C, Pandyan A. A systematic review and synthesis of the quantitative and qualitative evidence behind patient-centred goal setting in stroke rehabilitation. Clin Rehabil. 2011;25(6):501–514.
- Wheeler S, Acord-Vira A, Davis D. Effectiveness of interventions to improve occupational performance for people with psychosocial, behavioral, and emotional impairments after brain injury: a systematic review. Am J Occup Ther. 2016;70(3):7003180060p1–7003180060p9.
- Fink A. Conducting research literature reviews: from the internet to paper. 3rd ed. Thousand Oaks (CA): SAGE Publications; 2010.
- Smith V, Devane D, Begley CM, et al. Methodology in conducting a systematic review of systematic reviews of healthcare interventions. BMC Med Res Methodol. 2011;11(1):1–6.
- Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339:b2535.
- Davies KS. Formulating the evidence based practice question: a review of the frameworks. Evid Based Library Inform Pract. 2011;6(2):75–80.
- Kersten P, McCambridge A, Kayes NM, et al. Bridging the gap between goal intentions and actions: a systematic review in patient populations. Disabil Rehabil. 2015;37(7):563–570.
- Baker C, Worrall L, Rose M, et al. A systematic review of rehabilitation interventions to prevent and treat depression in post-stroke aphasia. Disabil Rehabil. 2017;19:1–23.
- Hurn J, Kneebone I, Cropley M. Goal setting as an outcome measure: a systematic review. Clin Rehabil. 2006;20(9):756–772.
- Kennedy MR, Coelho C, Turkstra L, et al. Intervention for executive functions after traumatic brain injury: a systematic review, meta-analysis and clinical recommendations. Neuropsychol Rehabil. 2008;18(3):257–299.
- Krasny-Pacini A, Chevignard M, Evans J. Goal management training for rehabilitation of executive functions: a systematic review of effectiveness in patients with acquired brain injury. Disabil Rehabil. 2014;36(2):105–116.
- Parke HL, Epiphaniou E, Pearce G, et al. Self-management support interventions for stroke survivors: a systematic meta-review. PLoS One. 2015;10(7):e0131448.
- Powell JM, Rich TJ, Wise EK. Effectiveness of occupation- and activity-based interventions to improve everyday activities and social participation for people with traumatic brain injury: a systematic review. Am J Occup Ther. 2016;70(3):7003180040p1.
- Warner G, Packer T, Villeneuve M, et al. A systematic review of the effectiveness of stroke self-management programs for improving function and participation outcomes: self-management programs for stroke survivors. Disabil Rehabil. 2015;37(23):2141–2163.
- Yang SY, Lin CY, Lee YC, et al. The Canadian Occupational Performance Measure for patients with stroke: a systematic review. J Phys Ther Sci. 2017;29(3):548–555.
- Cullen N, Chundamala J, Bayley M, et al. The efficacy of acquired brain injury rehabilitation. Brain Inj. 2007;21(2):113–132.
- CASP UK. CASP Critical Appraisal Skills Programme [Internet]. CASP UK; 2018; [cited 2018 Jan 29]. Available from: http://www.casp-uk.net/
- Oxford Centre for Evidence-Based Medicine – Levels of Evidence; 2009; [Internet]; [cited 2018 Feb 10]. Nuffield Department of Primary Care Health Sciences. Available from: http://www.cebm.net/blog/2009/06/11/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/
- Bright F, Kayes N, Cummins C, et al. Co-constructing engagement in stroke rehabilitation: a qualitative study exploring how practitioner engagement can influence patient engagement. Clin Rehabil. 2017;31(10):1396–1405.
- World Health Organization. Framework on integrated, people-centred health services. Sixty-ninth world health assembly A69/39: WHO; 2016; [cited 2018 Apr 26]. Available from: http://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_39-en.pdf?ua=1&ua=1
- Locke EA, Latham GP. Building a practically useful theory of goal setting and task motivation: A 35-year odyssey. Am Psychol. 2002;57(9):705–717.
- Green D, Payne S. Understanding organisational ability and self-regulation in children with developmental coordination disorder. Curr Dev Disord Rep. 2018;5(1):34–42.
- Law M. Participation in the occupations of everyday life. Am J Occup Ther. 2002;56(6):640–649.
- World Health Organisation (WHO). International classification of functioning, disability, and health. Geneva: ICF; 2001.
- Phipps S, Richardson P. Occupational therapy outcomes for clients with traumatic brain injury and stroke using the Canadian Occupational Performance Measure. Am J Occup Ther. 2007;61(3):328–334.
- Green D. Limitations of meta-analyses. J Autism Dev Disord. 2012;42(8):1774–1775.
- The GRADE Working Group. What is GRADE? [Internet]. The GRADE Working Group; 2018; [cited 2018 Jan 29]. Available from: http://www.gradeworkinggroup.org/
- Spinal Cord.com. Acquired brain injuries. Spinal Cord, Inc.; [cited 2018 Apr 17]. Available from: https://www.spinalcord.com/acquired-brain-injury
- Law M, King G, Russell D, et al. The person-environment-occupation model: a transactive approach to occupational performance. Can J Occup Ther. 1996;63:9–23.