Abstract
Purpose
For persons on disability benefits who are facing multiple problems, active labour market policies seem less successful. Besides health problems, these people perceive personal, social, and environmental problems. Since very little is known about these “non-medical” problems our aim was to explore the prevalence of clients experiencing multiple problems, the types and number of perceived problems, combinations of perceived problems, and associated characteristics in a group of work disability benefit recipients.
Methods
We performed a cross-sectional study, using self-reported data on perceived problems and socio-demographics, and register data from the Dutch Social Security Institute on diagnosed diseases and employment status. A convenient group of labour experts recruited eligible clients on work disability benefit.
Results
Of the 207 persons on work disability benefit, 87% perceived having multiple problems. Most reported problems were related to physical (76%) or mental (76%) health. Health problems most frequently occurred together with a mismatch in education, financial problems, or care for family members. Clients with lower education experienced significantly more problems than clients with an intermediate or high educational level.
Conclusions
Clients with multiple problems face severe and intertwined problems in different domains of life, and need tailored multi-actor work disability management.
Clients with multiple problems face severe and intertwined problems in different domains of life; therefore, interventions tailored to deal with needs related to specific problems might be more effective than traditional programs.
Interventions should match experienced barriers, and involve multi-actor work disability management with all the challenges of mutual cooperation.
For persons with multiple problems a focus on pure medical barriers is too narrow, because personal, social, and environmental factors might also obstruct participation in work.
Implications for rehabilitation
Background
To improve the labour market prospects of persons with disabilities, over the past decades several countries within the Organisation for Economic Cooperation and Development have reformed their disability programs. These programs are designed to foster labour market integration of people who, due to illness or disability, face challenges in staying or (re-)entering in the workforce [Citation1]. So-called active labour market policies have proved to be effective for unemployment benefit recipients. However, for persons on disability benefit, or unemployed people facing multiple problems, these policies appear to be less successful while these specifically focus on return to work instead of using a more holistic way of supporting people, and addressing an integrated approach at individual, sociostructural, and environmental level [Citation2,Citation3]. Besides health issues, they are often faced with personal difficulties such as relational, financial, domestic, addiction, and/or educational problems [Citation4]. Often, the difference between long-term beneficiaries (unemployed for longer than 12 months in the Netherlands [Citation5]) and short-term beneficiaries is the presence not just of a single problem but of a cluster of problems. Moreover, most of these barriers for return to work seem to interact with each other [Citation6]. Studies in the UK and in the Netherlands show that for individuals facing multiple problems, including poor health, the probability of successfully returning to work is lower than for persons facing unemployment only [Citation7,Citation8]. These studies also reported a clear negative association between the number of problems and having paid employment.
In general, experiencing interacting multiple barriers to employment is in itself the greatest barrier, rather than the type of problems [Citation9], as people often do not know where to begin, and there is no single solution for return to work. People with multiple problems seem to get into a vicious circle of solving one problem only to be confronted with the next [Citation6]. However, literature adequately addressing multiple problems among disability claimants is scarce. Furthermore, the concept “multiple problems” is defined and described differently in various studies, referred to as multiple barriers, multiple disadvantages, numerous problems, or just problems [Citation7,Citation8,Citation10–14]. To comply with national studies, the current definition of multiple problems was used: there are multiple problems in persons when they have to deal with two or more related and possibly reinforcing problems for a longer period of time, and the person concerned is unable to develop and conduct adequate management with regard to control or solve the problems, resulting in problematic participation in society and labour market [Citation8].
It is important to gain more knowledge about the impact of multiple problems on work disability recipients, especially since identifying barriers can actually provide an incentive for action, and helping disadvantaged clients to address barriers more effectively can lead to improved outcomes for them [Citation15,Citation16].
The aim of this study is to explore the prevalence of clients experiencing multiple problems, the types and number of perceived problems, combinations of perceived problems, and associated characteristics in a group of work disability benefit recipients.
Methods
Design
The current study is a cross-sectional study using baseline data from the longitudinal Comprehensive Approach to Reintegration for clients with multiple problems study (CARm study) [Citation14]. The CARm study is a randomised trial to evaluate the effectiveness of a training for labour experts to improve work participation by clients with multiple problems. All participants provided written informed consent. The Medical Ethics Committee of the University Medical Center Groningen (UMCG), the Netherlands, approved recruitment, consent and field procedures (ref. M16.194601). The trial, “The effectiveness of the CARm training for labour experts to improve work participation of clients with multiple problems”, was registered at the Dutch Trial Register (NTR5733).
Participants
For the trial, disability benefit recipients who met the following criteria were included: clients who have been granted for a work disability benefit and have been assessed with residual work capacity, but are unemployed or not working the complete number of hours according to their residual work capacity, having an age of 18–65, and being able to understand and write Dutch.
Recruitment
Recruitment took place in two stages. First, we had to recruit labour experts willing to participate in the trial. In the Dutch social security system, labour experts play a key role in supporting the re-integration process of persons with a work disability and remaining work capacity. In general, disability benefit recipients are assigned to a labour expert when they are in need of support for their participation and reintegration in work, resulting in the labour expert being responsible for the more disadvantaged and complex clients with multiple problems.
Second, these labour experts had in turn to recruit clients eligible to participate in the trial.
To recruit labour experts, we informed managers of The Dutch Social Security Institute for Employee Benefit Schemes (UWV) about the study. The managers selected and informed a contact person per district. These contact persons then were asked to forward an invitation, written by the researcher to all labour experts in their district, to participate in the study. In total n = 353 labour experts (within 11 districts in the Netherlands) were addressed for participation. The inclusion period was between February and March 2016, and ended after 40 labour experts had signed up for the study. During a meeting, all included labour experts were then further informed about their role in this study.
Participating labour experts were asked to recruit participants from among their clients, and then to inform those who met the inclusion criteria about the study.
From clients interested in participating in the trial, labour experts then collected name, address, and e-mail address and sent these to a research assistant. The research assistant then sent to each participant a letter providing more detailed information about the study, along with a consent form and the first questionnaire. After returning the informed consent form, participants were included in the study. Clients were recruited by labour experts between April and December 2016.
Measures
For this study, we used data from a self-reporting questionnaire, including items on perceived problems and socio-demographics. We derived diagnosed diseases and employment status from register data of the Dutch Social Security Institute: the Institute for Employee Benefit Schemes (UWV).
Perceived problems, severity, and multiplicity
We assessed perceived problems using a self-constructed questionnaire, asking the participants if they experienced problems in the following areas: (1) physical health, (2) mental health, (3) financial problems, (4) care for family or children, (5) educational mismatch (too low or not appropriate), (6) problems with the Dutch language, (7) problems with police or justice, (8) housing, (9) addiction, and (10) domestic violence. These areas were derived from the categories of multiple problems, selecting the problems most suitable for the target population out of the four domains (psychological problems, cultural problems, economic problems, and normative problems) as reported by Statistic Netherlands (CBS) [Citation8]. For each reported problem, participants were asked to score the severity of their problems on a four-point Likert scale: (1) no barriers, (2) mild barriers, (3) moderate barriers, and (4) severe barriers. Perceiving problems (yes/no) were defined as experiencing mild to severe barriers on an item with a score of 2 or higher. Multiple problems (yes/no) were defined as experiencing two or more problems.
Covariates
Socio-demographic characteristics included gender, age, living status, educational level, and paid employment. All data, except employment status, were collected with a self-reporting questionnaire. Living status was operationalised with the question: are you living alone or living together with others. Educational levels were categorised as low (elementary, preparatory middle-level), intermediate (middle-level applied; higher general continued), and high (university applied sciences; research university). Paid employment was measured using data on gross wages and social benefit pensions from the Dutch tax register, which were available through data linkage with Polis register data from UWV. Data on these income characteristics were available on monthly basis with a follow-up period of one year from the time of enrolment in the CARm trial. Paid employment was dichotomised into (yes/no) regarding receiving income from employment according to the register data of UWV during the month of the study inclusion.
Data on diagnoses were retrieved from the register data provided by UWV. When clients apply for disability benefits, insurance physicians use the Dutch Classification of Occupational Health and Social Insurance (CAS) to categorise diagnoses, derived from the International Statistical Classification of Disease and Related Health Problems [Citation17] (ICD-10). The CAS is based on the International Statistical Classification of Disease and Related Health Problems (ICD-10), a medical classification list from the World Health Organization [Citation18]. During the medical disability assessment, insurance physicians can list up to three disorders. In this study, we used only the primary diagnose, the one causing the most important limitations to being able to work according to the insurance physician. For generalisability reasons, diagnoses were clustered into four groups: somatic diseases (e.g., cardiovascular disorders and lumbar disc disorders), intellectual disabilities (e.g., mild mental retardation (IQ range 50–69)), psychiatric disorders (e.g., depressive episodes), and developmental diseases (e.g., autism spectrum disorders).
Analyses
To analyse the number, type, and severity of perceived problems we used descriptive statistics (frequencies, percentages, means, and standard deviations). To analyse combinations of perceived problems, we visualised the combinations in a matrix, and in flow chart structures. We presented the most informative structure, based on frequency; this means starting off from perceived mental and/or physical problems and the three most reported additional perceived problems, up to three levels. Furthermore, we dichotomised the diseases diagnosed by the insurance physician as primarily physical or mental. We conducted subgroup analyses, using frequencies to explore whether the perceived additional problems were similarly distributed in both diagnosis groups.
We analysed associations of age, gender, educational level, living circumstances, paid employment, and type of diagnosed disease with the number of perceived problems, using univariable and multivariable linear regression analyses. We selected all variables with a p < 0.20 in the univariable analyses for multivariable linear regression analysis, as stricter p values can fail in identifying variables known to be important [Citation19]. In the multivariable model, we used p < 0.05 to interpret as statistically significant. For all analyses, we used the statistical package SPSS version 25.0 (SPSS Inc., Chicago, IL).
Results
In total, 40 labour experts approached 418 eligible clients. After sending the study documents, 207 clients of 38 labour experts (range 1–9 clients per labour expert) provided informed consent, returned the questionnaires, and were included in the study. The study sample consisted of 95 male clients (46%), with a mean age of 36 years (SD 13.0). One-third (33%) were low educated, 35% lived alone, and 14% were in paid employment. Most clients were diagnosed with a somatic disease (35%) or a psychiatric disorder (31%), followed by developmental disorders (15%) and intellectual disabilities (14%) ().
Table 1. Participant characteristics.
Type and severity of perceived problems
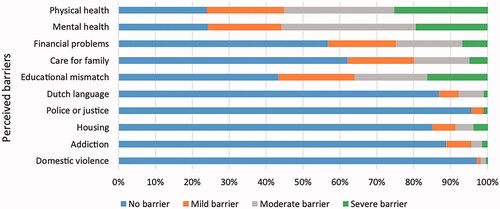
Of the 207 included clients, 156 (76%, two missing value, n = 205) perceived physical problems, 49 (24%) perceived no physical problems. Furthermore, 156 (76%, one missing value, n = 206) perceived mental problems and 50 (24%) perceived no mental problems. In addition, 57% perceived an educational mismatch, 43% perceived financial problems, 38% experienced barriers due to care for family, 15% perceived housing problems, 13% perceived problems with the Dutch language, 11% problems with addiction, 4% problems with police or justice, and 3% because of domestic violence ().
Table 2. Type and number of perceived problems.
About a quarter of the participants (25%) with physical health problems rated these problems as severe, 19% perceived their mental health problems as severe, and 16% perceived problems regarding an educational mismatch as severe ().
Number and combinations of perceived problems
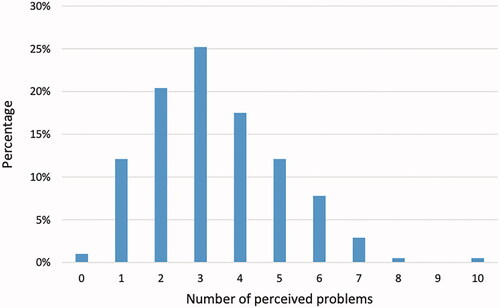
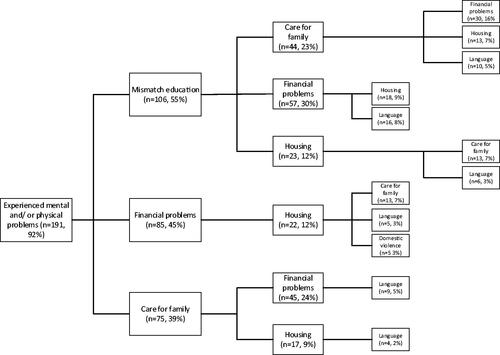
A total of 179 (87%) participants reported multiple (two or more) problems. On average, three (1.7 SD) problems were perceived, and 12% reported having six or more problems (). We found several combinations of perceived problems. Of the 191 clients with mental and/or physical problems, 106 (55%) also perceived a mismatch in education, 85 (45%) perceived financial problems, and 75 (39%) perceived problems due to care for family (). When looking separately at the subgroup of participants with only mental or physical problems, we found similar patterns. Although not many participants perceived problems caused by domestic violence (n = 6), all of those who did perceived a 100% combination of additional problems with mental health, finances, and educational level (see for more details). Although 204 participants were diagnosed with a mental or physical disorder, despite their diagnosis 12 participants (6%) within this group reported no barriers due to these disorders. Of the 12, 75% experienced problems due to mismatch in education and 33% because of financial problems (Supplementary Figures).
Table 3. Heat map with additional problems (n = 207)Table Footnotea
Associations with number of perceived problems
In the univariable analyses, we found male gender, an intermediate or high educational level, and developmental disorders to be associated with a lower number of perceived problems. In the multivariable analysis, we found significant association of intermediate educational level (B = −0.717; 95% CI –1.234 to −0.200), and high educational level (B= −1.347; 95% CI −2.030 to −0.664) with a lower number of perceived problems (see ).
Table 4. Univariate and multivariate linear regression associations between sociodemographic characteristics and number of perceived barriers.
Discussion
Main findings
The aim of this study was to explore the prevalence, type, number, and combinations of problems experienced by disability benefit recipients, and to study the associations of socio-demographic characteristics and type of diagnosis with the number of perceived problems. The prevalence of multiple problems was high; 87% of the participants reported at least two problems, and the average number of problems was three. Most reported problems were related to physical health, mental health, and/or an educational mismatch. Up to 25% of participants experienced these problems as a severe barrier. The most frequent combinations of health problems occurred with a mismatch in education, financial problems, or care for family members. In the multivariable model, the number of problems perceived by participants was negatively associated with educational level; i.e., higher educated participants perceived fewer problems.
Comparison with other studies
To our knowledge, this study is the first to report the percentage of disability claimants who face multiple problems, as well as the number and combinations of problems they perceive. These findings are in line with a qualitative study which showed that sick-listed unemployed workers perceived several barriers to returning to work [Citation6]. This study also reported that not only health problems, but also low education, financial problems, and lack of childcare facilities were perceived as barriers [Citation6].
Only a small percentage of our study population perceived problems with domestic violence. However, in this specific group, almost all perceived additional problems with physical and mental health, finances, educational mismatches, and housing, and about half of them perceived problems with care for family, Dutch language, and addiction. Although the group who perceive problems with domestic violence is small, it seems to be a very problematic group, with people who experience many problems in different facets of their lives, including work [Citation20,Citation21].
When exploring associations with the number of perceived problems, we found that higher educated recipients of benefits perceive fewer barriers. This is in line with earlier research, showing that those with lower educational levels encounter more barriers to employment [Citation13,Citation22,Citation23]. A possible explanation for this may be that higher educated people act sooner when a problem occurs. It is known from the literature that higher education is associated with social problem-solving [Citation24]. Another plausible explanation might be that higher educated people usually have healthier lifestyles, better working conditions, they act sooner when a problem occurs and are better able to adjust their working conditions [Citation25,Citation26]. Another possible explanation may be that some of the problems in our questionnaire are known to be associated with lower educational levels. People with higher education usually have a higher household income [Citation13], and therefore fewer financial problems. On the other hand, housing is a typical problem for people receiving a low income [Citation27]. Educational mismatches are also more often perceived as problems by lower educated unemployed workers [Citation22,Citation23].
Strengths and limitations
This study provided insight into personal and social environmental barriers towards working or participating in society beyond the medical diagnose of an insurance physician. We were able to include a geographically representative sample of clients from all regions in the Netherlands, both rural and urban, and from economically strong and less strong regions. Furthermore, for employment status and diagnosed disease we used register data, which are more objective than self-reported data. To measure multiple problems we unfortunately lacked a validated instrument, and therefore had to use a self-constructed questionnaire, but the constructed questionnaire, based on areas reported by Statistics Netherlands [Citation8], seemed to work well in quantifying the amount and severity of problematic areas. Due to selection bias, we probably underestimated problems with the Dutch language, as participants had to be able to understand, read and write Dutch. Additionally, recruitment of participants was performed by labour experts, therefore, only disability benefit recipients assigned to labour experts were included in our study. These clients are in need for extra support with regards to participation and reintegration to the labour market, due to their disadvantaged situation. Therefore, the results of our study are only generalisable to a subgroup of clients receiving work disability benefits, i.e., those who are referred to labour experts for support on their participation and reintegration.
Implications for practice and research
To encourage (re)employment of people receiving work disability benefits, recognition of the existence of multiple problems and how they affect employment chances is necessary [Citation1,Citation8].
Although in social security settings, new instruments have been developed to assess individuals’ work capacity [Citation28–30], the focus is still mainly on barriers associated with health issues and not on issues like domestic violence, financial problems, and problems due to care for family. Involving multiple institutions and disciplines in work capacity assessments could lead to a broader overview of the perceived problems of the claimants, although it would place high demands on cooperation and data-sharing by all those involved [Citation14].
A number of employment support and rehabilitation programs are available to help people on disability benefits return to the labour market. Some studies of these programs showed promising results [Citation31]; however, particularly studies involving disadvantaged populations (lower educated, poor health) have reported poorer outcomes and lower levels of adherence [Citation32,Citation33]. There are strong suggestions that individually focused “downstream” interventions, such as self-management support, have limited effectiveness in these groups [Citation34] because they fail to take into account potential barriers within the person’s wider social context (e.g., literacy, resources, and social supports) [Citation35–39]. As clients with multiple problems face severe and intertwined problems in different domains of their lives, interventions tailored to their specific needs and wishes might be more effective than traditional programs [Citation14]. Such interventions, developed to match the person’s experienced barriers, would involve multi-actor work disability management, with all the challenges of mutual cooperation [Citation40].
The limited availability of scientific evidence seems to warrant further research on the impact of multiple problems and how these interact. Currently, no validated questionnaire to measure multiple problems is available. Although our constructed questionnaire, based on areas as reported by Statistics Netherlands [Citation8], seemed to work well, in future research it is recommended to develop a validated questionnaire to measure multiple problems, which can also be used in other studies. Fundamental work is needed to further build a theoretical framework and validate measures to assess multiple and combined problems. Practice-based scientific research should focus on what works for whom, and develop interventions that tackle the complexity of multiple problems.
Conclusions
This study showed, among clients on work disability benefits, a high prevalence of perceived multiple problems. Along with physical and mental health problems, subjects frequently reported problems with mismatch in education, finances, and care for family. In addition to the medical diagnosis of the insurance physician, clients perceive a range of personal and social environmental barriers that may hinder reintegration. Since these problems are diverse, clients with multiple problems on work disability benefit might be better off with a more tailored reintegration approach, aimed specifically at their needs and wishes. A focus only on physical or mental disorders is too narrow. Since clients experience a variety of personal, social, and environmental factors which obstruct participation in work, a more integrated, individual approach involving multi-actor work disability management might be more successful.
Supplementary Figures
Download (1.9 MB)Disclosure statement
The authors have no declarations of interest to report.
References
- OECD. Sickness, disability and work: breaking the barriers: a synthesis of findings across OECD countries. Paris: OECD Publishing; 2010.
- Dean H. Re-conceptualising welfare-to-work for people with multiple problems and needs. J Soc Pol. 2003;32(3):441–459.
- Martin JP. Activation and active labour market policies in OECD countries: stylized facts and evidence on their effectiveness. IZA J Labor Policy 4. 2015. DOI:10.1186/s40173-015-0032-y
- Singley SG. Barriers to employment among long-term beneficiaries: a review of recent international evidence. Wellington: Ministry of Social Development; 2003.
- CBS. Werklozen; 2020 [cited 2020 Aug 27]. Available from: https://www.cbs.nl/nl-nl/visualisaties/dashboard-arbeidsmarkt/werklozen
- Audhoe SS, Nieuwenhuijsen K, Hoving JL, et al. Perspectives of unemployed workers with mental health problems: barriers to and solutions for return to work. Disabil Rehabil. 2018;40(1):28–34.
- Berthoud R. Multiple disadvantage in employment: a quantitative analysis. York: Joseph Rowntree Foundation; 2003.
- Bosselaar H, Maurits E, Molenaar-Cox P, et al. Clients with multiple problems. An orientation and report in relation to (labour)participation (Multiproblematiek bij cliënten. Verslag van een verkenning in relatie tot (arbeids)participatie (in Dutch). Meccano kennis voor beleid en AStri Beleidsonderzoek en-advies; Utrecht/Leiden: Ministry of Social Affairs and Employment; 2010.
- European Foundation for the Improvement of Living and Working Conditions. Access to employment for vulnerable groups. Foundation paper no. 2; Dublin; 2002.
- Dean H, MacNeill V, Melrose M. Ready to work? Understanding the experiences of people with multiple problems and needs. Benefits. 2003;11(1):19–25.
- Blumenberg E. On the way to work: welfare participants and barriers to employment. Econ Dev Quart. 2002;16(4):314–325.
- Perkins D, Nelms L. Assisting the most disadvantaged job seekers. In: Carlson E, editor. A future that works: Economic, Employment and the evironment. Newcastle: Center of Full Employment and Equity, University of Newcastle; 2004.
- Lindsay SJD. Discrimination and other barriers to employment for teens and young adults with disabilities. Disabil Rehabil. 2011;33(15–16):1340–1350.
- Brongers KA, Cornelius B, van der Klink JJL, et al. Development and evaluation of a strength-based method to promote employment of work-disability benefit recipients with multiple problems: a feasibility study. BMC Public Health. 2020;20(1):71.
- Butterworth P, editor. The challenge of greater economic and social participation: describing the disadvantage of lone mothers receiving income support. Steps Forward for Families: Research, Practice and Policy: 8th Australian Institute of Family Studies Conference. Citeseer; 2003.
- Butterworth P. The prevalence of mental disorders among income support recipients: an important issue for welfare reform. Aust N Z J Public Health. 2003;27(4):441–448.
- World Health Organization. The global burden of disease: 2004 update. Geneva: World Health Organization; 2004.
- World Health Organization: International Classification of Diseases; 2016 [cited 2017 Feb 6]. Available from: http://www.who.int/classifications/icd/en/
- Mickey RM, Greenland S. The impact of confounder selection criteria on effect estimation. Am J Epidemiol. 1989;129(1):125–137.
- Knight L, Hester M. Domestic violence and mental health in older adults. Int Rev Psychiatry. 2016;28(5):464–474.
- Lloyd S. The effects of domestic violence on women’s employment. Law Policy. 1997;19(2):139–167.
- Scharn M, Oude Hengel K, Boot CRL, et al. Influence of chronic diseases on societal participation in paid work, volunteering and informal caregiving in Europe: a 12-year follow-up study. J Epidemiol Community Health. 2019;73(2):136–141.
- Laaksonen M, Gould R. Return to work after temporary disability pension in Finland. J Occup Rehabil. 2015;25(3):471–480.
- Heidrich SM, Denney N. Does social problem solving differ from other types of problem solving during the adult years? Exp Aging Res. 1994;20(2):105–126.
- Robroek SJ, Rongen A, Arts CH, et al. Educational inequalities in exit from paid employment among Dutch workers: the influence of health, lifestyle and work. PLoS One. 2015;10(8):e0134867.
- de Breij S, Qvist JY, Holman D, et al. Educational inequalities in health after work exit: the role of work characteristics. BMC Public Health. 2019;19(1):1–15.
- Anderson KA, Richardson VE, Fields NL, et al. Inclusion or exclusion? Exploring barriers to employment for low-income older adults. J Gerontol Soc Work. 2013;56(4):318–334.
- Bickenbach J, Posarac A, Cieza A, et al. Assessing disability in working age population. In: A Paradigm Shift: from impairment and Functional Limitation to the Disability Approach. Washington (DC): World Bank; 2015.
- Sengers JH, Abma FI, Ståhl C, et al. Work capacity assessments and efforts to achieve a job match for claimants in a social security setting: an international inventory. Disabil Rehabil. 2020;1–10.
- OECD. New ways of addressing partial work capacity. Thematic review on sickness, disability and work issues paper and progress. OECD report; 2007.
- OECD. Transforming disability into ability: policies to promote work and income security for disabled people. Paris: OECD; 2003.
- Van Hecke A, Heinen M, Fernández-Ortega P, et al. Systematic literature review on effectiveness of self-management support interventions in patients with chronic conditions and low socio-economic status. J Adv Nurs. 2017;73(4):775–793.
- Glazier RH, Bajcar J, Kennie NR, et al. A systematic review of interventions to improve diabetes care in socially disadvantaged populations. Diabetes Care. 2006;29(7):1675–1688.
- Hardman R, Begg S, Spelten E. What impact do chronic disease self-management support interventions have on health inequity gaps related to socioeconomic status: a systematic review. BMC Health Serv Res. 2020;20(1):150.
- Adams RJ. Improving health outcomes with better patient understanding and education. Risk Manag Healthc Policy. 2010;3:61.
- Greenhalgh TJB. Patient and public involvement in chronic illness: beyond the expert patient. BMJ. 2009;338:b49.
- Kendall E, Rogers A. Extinguishing the social? State sponsored self-care policy and the chronic disease self-management programme. Disabil Soc. 2007;22(2):129–143.
- Furler J, Harris M, Rogers A. Equity and long-term condition self-management. London (UK): SAGE Publications; 2011.
- Harvey PW, Docherty B. Sisyphus and self-management: the chronic condition self-management paradox. Aust Health Rev. 2007;31(2):184–192.
- Liukko J, Kuuva N. Cooperation of return-to-work professionals: the challenges of multi-actor work disability management. Disabil Rehabil. 2017;39(15):1466–1473.