Abstract
Purpose
Children with cerebral palsy (CP) have an increased risk of cognitive difficulties and should be offered cognitive assessments. In Sweden, the CPCog protocol recommends children with CP undergo cognitive assessments at the start of primary and secondary school. To assess children with CP can be challenging, in particular when children are non-vocal or do not speak the local language. In such instances, augmentative and alternative communication (AAC) and qualified medical interpreters should be considered. The purpose of this study was to monitor the implementation and equitable delivery of the CPCog protocol in Sweden between the years 2017–2020.
Materials and Methods
In this cross-sectional study, registry data were extracted from the combined follow-up program and national registry for individuals with CP (CPUP), and a convenience sample of psychologists responded to an online survey.
Results and Conclusions
Each year, less than 5% of eligible children had registered cognitive assessments in CPUP. There was underuse of AAC during assessments and a discrepancy between the registered versus reported use of interpreters. Psychologists perceived AAC as more reliable for cognitive assessments than interpreters. Greater availability of and capacity to offer cognitive assessments in other formats and languages could help increase test accessibility for all children with CP.
The cognitive assessment of children with cerebral palsy (CP) is a complex but important issue within disability and re/habilitation.
Individualized cognitive assessments should be offered and carried out by psychologists.
Rehabilitation centers should strive to be inclusive through reliable test adaptations for functional abilities, means of communication, and language.
Greater availability of- and capacity to offer cognitive assessments in more formats and languages could help increase test accessibility for children with disabilities.
Implications for Rehabilitation
Introduction
Individuals with cerebral palsy (CP) have an increased risk of cognitive difficulties, such as in language, attention, memory, control of behavior, and visual-spatial processing [Citation1]. In Sweden, cognitive abilities are assessed through validated and standardized tests, which are carried out by psychologists at habilitation centers. These tests can help pinpoint an individual’s unique learning strengths and difficulties and assist in diagnosing learning disorders, language disorders, and intellectual disability (ID) [Citation2,Citation3]. Awareness of learning difficulties or ID permit families and children with disabilities to receive services, assistance, and financial support, as well as help adjust expectations for the child accordingly [Citation4,Citation5]. Among children with CP, intelligence quotient (IQ) scores range considerably, from profound ID to giftedness [Citation6–9]. The scope of cognitive difficulties experienced by individuals with CP has also been shown to vary between- and within the different CP subtypes and gross motor function levels [Citation1].
Carrying out cognitive assessments for children with CP hinges on being able to communicate with the child and their family, which can be difficult if the child has speech or language disorders, physical problems that constrain vocalization, or if the child or their family do not speak the local language. Therefore, a holistic, inclusive approach to assessing cognition is needed to help all people with CP navigate life during childhood and beyond. Cognitive assessments can be helpful in this pursuit, as they can assist in developing individually tailored interventions and strategies [Citation10], identify appropriate assistive technology [Citation1,Citation11] as needed, help set reasonable expectations, and observe how children fare over time.
Systematic Follow-Up of cognition in children with CP
To stay attuned to the additional health needs of children with CP, systematic follow-up, including the follow-up of cognition, is recommended [Citation11]. In 2012, the development of the CPCognition (CPCog) protocol became the first systematic, large-scale, follow-up program of cognition in children with CP in the Scandinavian countries (Sweden, Norway, and Denmark). CPCog described the rationale for cognitive areas to assess, recommended instruments and ages for testing, and proposed guidelines for reporting data and assessing subgroups of persons with CP (e.g., subtype, gross motor function, immigrated to Sweden). CPCog aimed to detect cognitive strengths and difficulties in children, as well as assist in social and academic interventions. The reporting of findings to national quality registries was implemented to better understand cognitive functioning in children with CP and to prevent inequality of services (e.g., in education, in healthcare, economic support, assistance at home) provided to children with CP and their families. To fulfill these objectives, CPCog recommended assessments for overall cognitive functioning (and if ID is suspected, social functioning and adaptive behavior), visual-motor abilities, and executive functioning prior to the start of primary school and during or before the transition into secondary school in Scandinavia [Citation11].
CPCog
In Sweden, clinical data on persons with CP, including cognition, are collected and followed by Sweden’s national quality registry and follow-up program for individuals with CP (CPUP) [Citation12]. Prior to the year 2017, data on cognition were also collected in the former Swedish quality registry for habilitation, HabQ. Beginning in 2015 and in collaboration with HabQ, the CPCog protocol was implemented in Sweden, recommending that children with CP undergo cognitive monitoring prior to the start of primary school (aged 6–7 years) and during the transition into secondary school (aged 12–13 years). This set of guidelines is considered phase I and for phase II, a more fine-tuned, person-centered assessment schedule is planned. The following psychometric assessments were recommended for both age groups, due to their validity, availability, and feasibility: Wechsler Scales [Citation13,Citation14] for cognitive functioning; Beery-Buktenica Developmental Test of Visual-Motor Integration (VMI) [Citation15]; and Behavior Rating Inventory of Executive Function (BRIEF) [Citation16] parent/teacher questionnaire for executive functioning.
These assessment tools are psychometrically validated, available in all three Scandinavian languages, and are widely known and used in all three countries. For all tests, using the most recent version available was recommended. When the protocol was initiated, the VMI and BRIEF were recommended to both age groups. For the Wechsler scales, the most appropriate scale for the developmental or chronological age was recommended, i.e., either Wechsler Preschool and Primary Scale of Intelligence (WPPSI) [Citation13] or Wechsler Intelligence Scale for Children (WISC) [Citation14]. Although these recommendations were consistent for children with greater motor functions (i.e., Gross Motor Function Classification System (GMFCS) levels I-III), it was recommended that children in GMFCS levels IV-V undergo adapted assessments with subtests from the aforementioned (or other standardized) tests and, when needed, be carried out by professionals with specialized expertise [Citation11].
Using augmentative and alternative communication (AAC) for cognitive assessments
Augmentative and alternative communication (AAC) is an essential and reliable way to adapt and make cognitive assessments accessible to more children with CP [Citation17,Citation18], as it enables individuals who cannot speak to communicate, participate, and have control. AAC is a broad term which encompasses communication devices, systems, strategies, and tools that are used to replace or support speech. There are two types of AAC: unaided systems (e.g., manual signs, gestures) and aided systems (e.g., communication with symbols or letters, using for example partner-assisted scanning or gaze pointing to access speech generating devices and other communication aids) [Citation19].
From psychologists’ and test developers’ perspectives, the matter of using AAC and altered response modality for assessments is complex. To ensure validity and reliability, cognitive assessments are normed and standardized in a systematic manner [Citation20,Citation21]. This renders the assessor scripted in what they can say or do [Citation22], which may limit psychologist’s options for making assessments more accessible. Children with CP who experience the most severe motor impairments (i.e., GMFCS levels IV and V), and typically also experience problems with speech [Citation23], could be at a particularly increased risk of missing out on cognitive assessments due to assumptions being made about their abilities rather than assessed. Still, recent research [Citation1,Citation24] maintains that these groups can be meaningfully assessed through certain cognitive assessments, or through adaptations using the same access methods that children use when expressing themselves with AAC. This can include, for example, pointing, eye-tracking, or partner-assisted scanning, which involve altering the child’s response modality, such as pressing a yes/no button, or answering through gaze fixation [Citation17,Citation25].
Children with CP who have immigrated to Sweden
Another communicative challenge can be introduced by language barriers. For children with CP who immigrate to Sweden or for children with CP born in Sweden to parents who have immigrated, opportunities to undergo cognitive assessments may be missed or less accessible during childhood [Citation26]. Swedish and Danish studies have shown that children who have immigrated face more challenges related to CP (e.g., reduced functioning, and bilateral spastic CP) compared with their Scandinavian counterparts [Citation27,Citation28]. To what extent children with CP who immigrate to Sweden receive required care needs still remains understudied, as only two studies have touched on the topic [Citation26,Citation29]. Westbom and Hägglund [Citation26] found no differences by birth place for each GMFCS level treated with orthoses, standing frames, spinal braces, and botulinum toxin. Conversely, Josenby et al. [Citation29] found a significant interaction between birthplace and spinal bracing; fewer spinal braces were prescribed to children born outside the Nordic countries, and individuals born outside of the Nordic countries were less likely to have received intrathecal baclofen.
Medical interpreters for cognitive assessments
Language barriers are common in healthcare, and medical interpreters are used to liaise communication between patients, practitioners, and families. In 2017, Statistics Sweden reported that 23% of Sweden’s two million children under the age of 18 years have a foreign background (defined by one or both parents born abroad) [Citation30], and annual statistics from Sweden’s Legal, Financial and Administrative Services Agency showed that between the years 2014 and 2015, an estimated 128,447 interpreting assignments were requested [Citation31]. Despite a high demand for interpreters, studies show insufficient use of interpreters in clinical settings [Citation32–34] and insufficient understanding for interpreter use guidelines [Citation35], both of which pose barriers to healthcare access.
The reported underuse of interpreters in Swedish clinical settings [Citation32–34] poses equity, human rights [Citation36], and legal questions as per Section 821 of the Patient Act 2014 [Citation37]. However, the matter is not quite one-dimensional when considering cognitive assessments, which imply that verbal instructions cannot be altered [Citation22]. When a third party such as an interpreter is used to liaise a language barrier, interpreting strategies, such as paraphrasing, omission, adapting syntax, providing contextual information, and clarification—which can be appropriate and applicable in other medical interpreting settings [Citation38–40]—are not necessarily compatible with the strict requirements for carrying out an unbiased cognitive assessment.
Because limited guidelines exist for using an interpreter during cognitive assessments, and the challenging nature of interpreting during these assessments, psychologists may resort to a number of different paths when assessing a child with limited Swedish proficiency. This may result in children with limited Swedish proficiency missing out on assessments, immigrant families receiving less information, and having less reliable—and therefore less helpful—test results.
Communicative barriers and the equitable delivery of cognitive assessments
Given that both language and speech barriers present communicative obstacles for psychologists when cognitively assessing children with CP, it is necessary to investigate whether these barriers contribute to differences in children’s reception of cognitive assessments. To date, no studies have investigated the role of communicative challenges posed by AAC and interpreters in the delivery of cognitive assessments to children with CP. Ensuring equitable care requires more detailed information about the associations between the receipt of cognitive assessments and functional abilities, birthplace, and communicative needs, such as AAC and medical interpreters, respectively. It is also important to understand how practitioners currently use and perceive using AAC and medical interpreters for carrying out cognitive assessments. Together, this knowledge could be used to develop more detailed, inclusive guidelines for addressing communicative barriers in the delivery of cognitive assessments.
Aims
The overall purpose of this study was to follow-up on CPUP’s implementation of the CPCog protocol. Based on the CPCog recommendations for assessing cognition in children with CP, and the gap in research and guidelines for addressing communicative barriers, the aims were the following:
to examine the frequency of cognitive assessments during years 2017–2020 for children with CP aged 5–8 and 11–14 years living in Sweden,
to investigate the associations between the delivery of general cognitive assessments and functional abilities, birthplace, sex, and CP subtype, respectively,
to explore the use of AAC and medical interpreters for cognitively assessing children with CP in Sweden, and
to report psychologists’ perceptions of using AAC and medical interpreters for cognitively assessing children with CP.
Materials and methods
Study design, setting and participants
This cross-sectional registry study was based on CPUP registry data collected January 2017–December 2020 and CPCog survey data collected December 2020–February 2021 throughout Sweden. The CPCog survey utilized a 45-item anonymous questionnaire that was derived from a Norwegian questionnaire, which was developed to assess facilitators and barriers for implementing the CPCog protocol in clinics [Citation10]. The Swedish questionnaire added new questions about the use of AAC and medical interpreters and perceptions of using these communicative aids, which were used for the present study. Before the study was conducted, the aims and research questions were discussed with and supported by a CPUP user group, which included three adult family members of children with CP, three researchers specialized in CP, and one adult with CP. The registry data used in the present study were de-identified and covered under ethical approval (Dnr 2020-04511) by the Swedish Ethical Review Authority. Prior to administration of the survey, the Swedish Ethical Review Authority deemed that the survey did not require ethical approval (Dnr 2020-04930), as no personal or sensitive data were collected, and the survey was designed for quality improvement purposes.
CPUP registry data
CPUP registry data were collected from 15/21 healthcare regions in Sweden. These data included variables for age, sex, CP subtype, functional classifications, birthplace, cognitive assessment types, use of AAC during cognitive assessments, and the need for AAC/interpreters during cognitive assessments. Data on cognitive assessments and which communicative aids are used during these assessments is registered by psychologists. Regions Norrbotten, Västernorrland, Örebro, Västra Götaland, and Gotland, and Blekinge did not have any registered cognitive assessments in CPUP.
Sweden has approximately 10.38 million inhabitants, of which approximately 20% are foreign-born (n = 2.05 million) [Citation41]. CPUP follows 95% of people with CP born year 2000 or later in Sweden [Citation42], with 5207 registered children/adolescents aged 0–18 years in March 2021. Upon registration in CPUP, parents/guardians are informed that their child’s data can be used for research and may opt out at any time. Based on the CPCog-recommended age groups for cognitive assessments (before ages 6–7 and 12–13 years), children/adolescents were only included in this study if they were ages 5–8 or 11–14 years between the years 2017–2020 and had a confirmed CP diagnosis. For each age group, one year was added to both the lower and upper age limits (i.e., those ages 5, 8, 11, and 14 years) to capture a more reliable sample, as some children are tested earlier or later, and only birth year was used to estimate age at the time of follow-up.
CPCog survey data
CPCog survey data were collected across Sweden. The number of psychologists who cognitively assess children with CP in child rehabilitation centers (referred to as habilitation centers in Sweden) is unknown; however, at the time of data collection, an estimated maximum of 145 child habilitation centers [Citation43] had the capacity to cognitively assess children with CP. However, not all of these 145 centers had a psychologist currently employed, and no exhaustive list of psychologists working at these centers was available. Although some centers have the capacity to assess children with CP, many psychologists tend to assess children with other neuropsychiatric diagnoses. In sum, we were able to identify a total number of 143 licensed psychologists practicing within child habilitation centers. Of these 143 psychologists who were invited to participate, 52 psychologists (response rate = 36%) in 18/21 healthcare regions in Sweden participated. No psychologists from Gotland, Gävleborg, or Norrbotten participated.
The questionnaire was designed in REDCap [Citation44] with skipping patterns, and the questionnaire was piloted by clinical practitioners who were familiar with the cognitive follow-up of children with CP.
Participants were recruited through publicly available email addresses on child habilitation center websites and snowball sampling. For 18/21 regions, CPUP has a designated psychologist as a contact person for reaching other psychologists. These contact persons were consulted to identify as many of the psychologists as possible who work in the child habilitation setting. Invitations with an information letter were sent out by email with a link to the online questionnaire. Before filling out the questionnaire, participants were informed about the anonymous nature of the study and gave consent. Reminder emails were automatically sent up to two times to emails with no registered response.
Functional ability classification systems
The present study examines associations between the reception of cognitive assessments, and functional abilities. These abilities are measured by three validated, standardized, and frequently used functional ability systems: the Gross Motor Function Classification System (GMFCS) (a measure of gross motor skills, i.e., self-initiated movement and use of assistive devices for mobility) [Citation45], the Manual Ability Classification System (MACS) (a measure of how children with CP use their hands to handle objects in daily activities) [Citation46], and the Communication Function Classification System (CFCS) (a measure of communicative effectiveness) [Citation47]. All three of these classification systems were developed by clinicians and researchers and use a standardized, complementary five-level ordinal classification system of functional abilities for persons with CP. In all three of these systems, level I indicates the least experienced difficulty, and level V indicates the most severe experienced difficulty.
Subtypes of cerebral palsy
The classification of CP subtype is based on clinical characteristics and the predominant neurological finding, which, in Sweden, are typically assessed by a neuropediatrician during early childhood. The Surveillance of Cerebral Palsy in Europe classifies the overarching subtypes of CP to be spastic (uni- or bilateral), dyskinetic, ataxic, or non-classifiable [Citation48], and these are the subtypes used in CPUP.
Independent variables
Age, sex, CP subtype, born in Sweden
Age was categorized by ages “5–8 years” (reference category) and “11–14 years”. Sex was categorized as “male” (reference category) or “female”. As there were few children with dyskinetic, ataxic, and unclassifiable/mixed form CP, subtype was dichotomized for the logistic regression models. Dyskinetic, ataxic, and unclassifiable/mixed forms were combined to form “other” (reference category) and compared to “spastic”. This decision was based on the small sample size and literature generally examining only spastic CP, as it is the most common CP subtype [Citation48]. Born in Sweden was dichotomized as “yes” (reference category) or “no”.
GMFCS, MACS, and CFCS-levels
For the logistic regression models, each functional classification system, GMFCS, MACS, and CFCS was dichotomized as “levels I–III” or “levels IV–V”. This was done due to low numbers in cognitive assessments in our sample, particularly for the 11–14-year age group. Clinically, this divide captures a reliable distinction in functional abilities, i.e., the ability versus inability to walk for GMFCS, to handle objects for MACS, and to effectively send and receive messages for CFCS.
Dependent variable: cognitively assessed
Cognitively assessed was dichotomized as “yes” (reference category) or “no”. A child was considered cognitively assessed if they had received at least one registered cognitive assessment in CPUP, irrespective of which type, between the assessment years 2017–2020 and were aged 5–8 or 11–14 years during these years.
Statistical analysis
A total of 5207 children with CP ages 0 to 18 years were registered in CPUP as of March 2021. The 2627 children aged 5–8 years (n = 1402) and 11-14 years (n = 1225), i.e., “eligible” for cognitive assessments, between the years 2017 and 2020 were included. The 215 children who were born in 2009 (i.e., were 8 years old in 2017 and 11 years old in 2020) were only counted in the younger age group to avoid double counting. Of these 215 children, only eight had registered cognitive assessments.
All variables were categorical and are presented as absolute numbers and percentages. Chi-squared tests were used to probe the distribution of independent categorical variables by the outcome variable, cognitively assessed. To check for multicollinearity between functional classification levels, Kendall’s rank correlations were used. Using the glm() function, univariate and multiple logistic regressions were run, respectively, to generate the odds ratios (ORs) and adjusted odds ratios (AORs) for the associations between independent variables and the reception of cognitive assessments. Participants with missing values were removed.
Kendall’s rank correlations showed strong correlations between GMFCS and MACS levels (τ = 0.79), GMFCS and CFCS levels (τ = 0.65), and MACS and CFCS levels (τ = 0.73). Given that these higher correlations would introduce multicollinearity in the model, only CFCS and MACS were included in the adjusted logistic regression model. This decision was based on clinical relevance, as inability to use one’s hands and inability to effectively communicate can affect the performance on cognitive assessments in distinguishable ways.
Statistical significance was based on a 95% confidence interval (CI). Statistical analyses were carried out with R [Citation49] in RStudio [Citation50]. Although there were no statistically significant differences (χ2 p = < 0.05) found in the distributions for born in Sweden, CP subtype, and sex, these variables were added to the multiple logistic regression model to control for their possible influence on the outcomes and to allow for future post-estimation analysis ().
Table 1. Relevant background factors of the study sample and their chi-square (χ2) test p-values, presented by outcomes, cognitively assessed and not cognitively assessed*.
Results
Delivery of cognitive assessments
Fifteen out of Sweden’s 21 regions had at least one registered cognitive assessment in CPUP. Of the 2627 children with CP in our sample, 157 (approximately 6.0%) were cognitively assessed over the combined years 2017–2020 (). For each of these years individually, children in the 5–8-year age group had a higher proportion of registered assessments compared with children aged 11–14 years (). Statistically significant associations were found for being in CFCS levels IV–V, GMFCS levels IV–V, MACS levels IV–V, and being in the 11–14-year age group (). No significant associations were found for sex, CP subtype, and born in Sweden (). In the adjusted model, which accounted for the effects of MACS level, CFCS level, age groups, sex, CP subtype, and born in Sweden, adjusted odds ratios were only significant for being in CFCS levels IV–V and being in the 11–14-year age group ().
Figure 1. The percentage of eligible children across all age groups (5–8 years, 11–14 years, 5–8 and 11–14 years) who were cognitively assessed over the years 2017–2020.
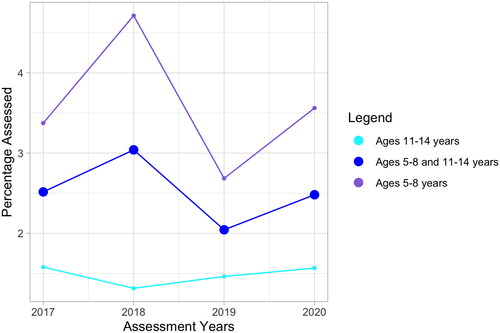
Table 2. Crude odds ratios (ORs), adjusted odds ratios (AORs), 95% confidence intervals (CI), and p-values for univariate and multiple logistic regression models for each predictor variable and the outcome variable, not cognitively assesseda.
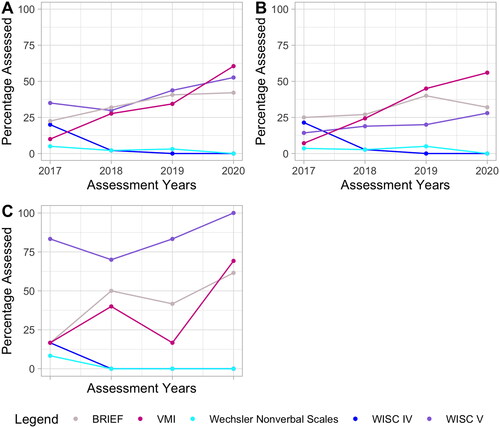
Types of cognitive assessments used
No children were assessed with the WPPSI-III or WPPSI-IV. For the combined age groups, there was an upward trend in the percentage of BRIEFs and VMIs that were carried out (). As expected, given the publication date, the percentage of WISC-IVs has a decreasing trend, and the percentage of WISC-Vs has, overall, an increasing trend (). In 2020, all 13 of the 11–14-year-olds who received at least one cognitive assessment were assessed with the WISC-V ().
Figure 2. Percentage of children who were assessed with the CPCog-recommended assessments (Wechsler Scales, VMI, BRIEF) out of the children who were cognitively assessed over the years 2017–2020. Plot A. Children with CP aged 5–8 years and 11–14 years out of the total number of assessed children in both of these age groups; Plot B. Children with CP aged 5–8 years out of children in this age group only; Plot C children with CP aged 11–14 years out of children in this age group only. CP: Cerebral palsy; VMI: Test of Visual Motor Integration; BRIEF: Behavior Rating Inventory of Executive Function; WISC IV: Fourth Edition of the Wechsler Intelligence Scale for Children; WISC V: Fifth Edition of the Wechsler Intelligence Scale for Children.
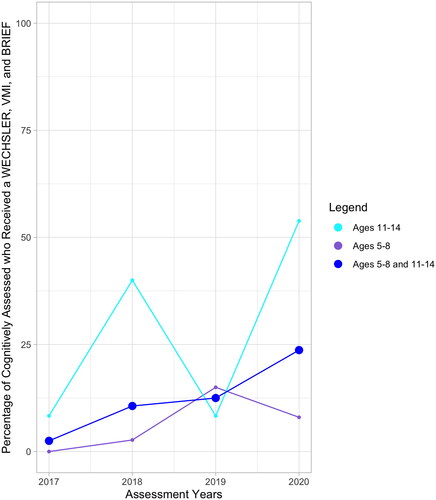
Percentage of children who received all three CPCog recommended assessments
The percentage of eligible children who received at least one assessment was higher in the younger age group for all four years (). Notably, for three out of the four years, there was a higher percentage of children in the older age group subpopulation who received all three recommended assessments ().
Figure 3. Plot shows the percentage of children (aged 5–8 years, 11–14 years, and both) who received all three CPCog recommended assessments, a Wechsler*, Visual Motor Integration (VMI), Behavior Rating Inventory of Executive Function (BRIEF), out of the total number of children who received a cognitive assessment over the years 2017–2020. *Included at least one of the following: Wechsler Nonverbal Scales of Ability, Fourth Edition of the Wechsler Intelligence Scale for Children (WISC IV), Fifth Edition of the Wechsler Intelligence Scale for Children (WISC V).
Use and perceptions of augmentative and alternative communication
As a child’s need for and the subsequent use of AAC for carrying out cognitive assessments are registered in CPCog, we were able to explore psychologists’ use and perceptions of AAC. Among the children who were cognitively assessed and needed AAC to communicate, AAC was only used for just over half during cognitive assessments. None of the respondents who used AAC for cognitive assessments reported that it “works very poorly” or was “not relevant” (). In terms of the type of AAC used, most psychologists reported using communication books/tables/loose symbols, whereas fewer used more advanced systems such as speech-generating devices, and one-fourth of respondents reported using other systems, including eye-tracking and manual signs. This survey data complemented the registered CPCog data, as the types of AAC used during assessments are not well-documented.
Table 3. Psychologists’ use and perceptions of alternative and augmentative communication, as reported in CPCog survey data and CPUP registry data.
Use and perceptions of interpreters
Of the children who were cognitively followed in CPUP, 10 children did not know Swedish, 29 were bilingual in Swedish and another language, and 117 only knew Swedish. When psychologists were asked, “Do children with CP who do not speak Swedish receive cognitive assessments?”, none responded “No”. In CPUP data on cognitive assessments, interpreters were used each time they were indicated as needed (). These data showed that oral interpreters (i.e., not sign language interpreters) were needed seven times for the parent/caretakers and the child, once for only the child, and twice for only the parents/guardians. Unfortunately, no data were available on the type of interpreter used (e.g., in-person, telephone, video-call).
Table 4. Psychologists’ use and perceptions of interpreters, as reported in CPCog survey data and CPUP registry data.
Discussion
The overarching aim of this study was to monitor the implementation of the CPCog protocol in Sweden in recent years. To achieve this, we examined associations between the delivery of cognitive assessments and functional abilities and explored how psychologists use and perceive AAC and interpreters for conducting cognitive assessments for children with CP.
Children with lower communicative ability were less likely to be assessed
Children with CP with lower communicative ability (CFCS levels IV–V) were less likely to be cognitively assessed compared with those with greater communicative ability (CFCS levels I-III), when controlling for other factors. This finding supports previous research [Citation9,Citation17,Citation51], which suggested that those with complex communication needs may miss out on assessments. Although significant differences were observed in the univariate logistic regression models for GMFCS and MACS levels IV–V, there were no significant differences after controlling for other variables. As CFCS and MACS levels were highly correlated, we expect that CFCS absorbs the effect of MACS when both MACS and CFCS are included in the model. Together, this study adds to the literature [Citation1,Citation17,Citation18,Citation52] underscoring the value of using adaptive response modality, nonverbal assessments, and AAC for cognitive assessments so that more children with CP can be cognitively assessed.
Children in older age group were less likely to be assessed
Children with CP in the older age group (11–14 years) were less likely to be cognitively assessed than the younger age group (ages 5–8 years). From the healthcare system perspective, this may be partially explained by the prioritization of early intervention in children with CP when resources (in this case psychologists) are scarce, and prioritization is necessary. However, it should be considered that the social and academic demands increase substantially during the onset of secondary school. Some examples are the increased reading and writing loads, mathematical concepts, and graph reading in secondary school, which can be difficult or exhausting for children with CP, as a result of difficulties in perception, visual-motor integration [Citation6] and difficulty or inability to use their hands [Citation46]. Although it may be feasible for some children with CP to keep up during primary school, the increased workload in secondary school can be burdensome. Following up with cognitive assessments during the transition into secondary school can help detect lesser impairments which might not be easily observable in younger ages, help families understand how the child will fare, and connect children with AAC or a helper at school as needed.
Registration of cognition in CPUP is low
We gather that the registration of cognition in CPUP has been consistently low over the years 2017–2020. However, data on cognition were registered during the year 2017 in HabQ for four Swedish regions, and these data were not included in our study. Therefore, monitoring the implementation of CPCog in Sweden with only CPUP data is challenging. Out of all those who were eligible for cognitive assessment over these years, less than 5% had a registered cognitive assessment each year, and out of those who did have a registered assessment, less than 25% had a registered Wechsler, VMI, and BRIEF per year from 2017 to 2020. To illustrate how this compares to the Norwegian branch of CPCog, 62% of eligible children had cognitive assessments registered in Norway’s national quality registry for CP (CPRN) at the end of 2020 [Citation53]. Unfortunately, psychologists rarely log when a cognitive assessment is offered but turned down or the reasons for which cognitive assessments are not carried out. In general, registries need this information to understand the true scope of when care is offered but turned down, or the reasons why care is not given.
Nevertheless, the low registration of cognition in CPUP suggests a need for improved resource allocation for cognitively assessing children with CP. As CP is the most common motor disability in childhood [Citation54,Citation55], there is consistent follow-up for physical therapy and occupational therapy; hence, even though CP is caused by damage to the brain [Citation56], the follow-up of cognition is less prioritized, possibly due to it being considered and treated as a mobility disability in most healthcare regions. There may also be shortages of psychologists in habilitation settings, or a shortage of psychologists who specialize in CP, although this is subject to more research. Still, the insufficient assessment of children with CP should be addressed. The increase of remote work and learning as a result of the Covid-19 pandemic has facilitated CPUP to hold more seminars on the cognitive follow-up of children with CP. These seminars have prompted a unique opportunity for not only relaying information concerning the CPCog protocol to psychologists, but also to receive feedback from psychologists on how to make registering data more convenient for them.
Underuse of AAC, uncertainty towards using interpreters
CPUP registry data suggested that AAC was only used for cognitive assessments about half the time when it was needed. To consider this together with CPCog survey data, responses showed that AAC was not always used when needed, and some psychologists reported not recalling if AAC was used during assessments. Taken together, both the registry and survey results suggest that AAC could be used more often during cognitive assessments and that psychologists need more knowledge about different forms of AAC. This finding builds upon previous findings [Citation17,Citation18,Citation24], which demonstrated that AAC can be used more often to cognitively assess children with CP who have greater functional limitations. Increasing knowledge of AAC and adapted response modality through training may help psychologists deliver more cognitive assessments to children with CP.
With respect to interpreters, however, CPUP registry data and CPCog survey data gave contrasting insight. In a limited sample of CPUP data on cognition, interpreters were indicated as needed and used 10/10 times. However, when psychologists were asked whether children with CP who do not speak Swedish undergo cognitive assessments, almost one-third of respondents reported “sometimes”, and of those who reported “yes” or “sometimes” to assessing non-Swedish-speaking children, nearly half reported that they did not know how many times they used interpreters for assessing non-Swedish speaking children over the last year. This may indicate uncertainty towards when to use interpreters for cognitive assessments, which would support previous findings underscoring uncertainty of guidelines for using interpreters in Swedish healthcare settings [Citation35]. We gather that psychologists’ uncertainty towards using interpreters for cognitive assessments is rooted in the goal of obtaining reliable results by striving for consistency with assessment guidelines. Nevertheless, optimizing solutions for cognitively assessing children with CP who do not speak the local language merits further investigation to help ensure that the child’s abilities are neither under- nor overestimated due to a language barrier.
In addition, 20 psychologists reported assessing fewer than five children over the last year with the help of an interpreter, which could total to a minimum of 20 children/families and a maximum of 80children/families who needed an interpreter for a cognitive assessment in the year 2020. The minimum total (n = 20) for the year 2020 is double the number that is reflected in the registry data for the combined years 2017–2020. This points to a higher number of non-Swedish-speaking families who require interpreters for cognitive assessments than what is reflected in the registry data. Thus, more research could help to better understand the role language and interpreters play in the context of cognitive assessments. Put simply, with Sweden’s linguistic landscape being so diverse [Citation31], habilitation centers and registries alike could benefit from considering and monitoring the role language has on the delivery of cognitive assessments—and other care—by gathering more detailed sociodemographic data.
Proportionally, trust is greater for AAC than interpreters
Our final key finding suggests that the proportion of psychologists who use AAC for cognitive assessments and trust the results is greater than the proportion who use interpreters and trust the results. Again, the strict standardized procedures (22) for carrying out cognitive assessments limit psychologists in terms of what they can alter. It is possible that AAC may allow psychologists to feel or be more in control, as it does not necessarily involve a third person but rather tools or technology, and it is typically at the psychologists’ discretion to interpret what the child is trying to communicate.
Conversely, using interpreters, who must alter natural features and underlying rules of language in order to deliver equal messages [Citation38–40], and who, as people, vary in terms of training and approach, may, with reason, introduce concerns for compromising the validity of cognitive assessments [Citation57]. When possible, in-person interpreters should be used during cognitive assessments for the comfort of the child and family, as well as to minimize miscommunication. One way to strengthen the use of interpreters during assessments could be for psychologists and interpreters to have a consultation before the assessment, such that the procedures can be understood, discussed, and practiced together. Another way to address this issue may be increased training [Citation58–60] for both psychologists who work in child habilitation and more specialized interpreters in some of Sweden’s most commonly requested languages for interpreting services. With increased training for how to carefully–and accurately–carry out cognitive assessments together, psychologists and interpreters may not only be able to work better together, but also help immigrant families and children with CP attain more accurate, and therefore more helpful results. It could also be beneficial for habilitation centers to strive for staff diversity and to consider the benefits of hiring psychologists who know other languages which are commonly spoken in Sweden.
Methodological considerations & limitations
When interpreting the results of this study, some methodological considerations and limitations should be considered, including systematic error, insufficient data, and limited variables to address confounding. For the CPCog survey, the snowballing strategy may have introduced selection bias. Our results may only reflect views of those who already have knowledge of or perceive the CPCog protocol to be important or a burden.
It should also be noted that we could neither account for the five regions who did not have cognitive assessments registered in CPUP, nor the three regions which were not represented by psychologists’ survey responses. Furthermore, children with missing values (N = 241) were excluded from our adjusted model. However, our finding that children with CP with lesser communicative ability are less likely to be assessed than children with greater communicative ability was consistent with other findings [Citation9,Citation17,Citation51]. In addition, our finding that children aged 11–14 years are less likely to be assessed than children aged 5–8 years was consistent with our expectations, given the prioritization of early intervention for children with CP [Citation61] and discussion with the CPUP psychologist network. Both of these findings are useful for addressing discrepancies in care.
Another limitation is our narrow sample and limited registry data on cognition. At the same time, this reflects a finding. Our results concerning the outcome, cognitively assessed, only reflect registered data, and thus imply limited generalizability. We suspect that a number of cognitive assessments take place but are not registered. The uptake of registering cognitive data in CPUP is a gradual process and varies considerably from region to region. Nevertheless, the small proportion of children who have cognition data registered in CPUP is an important finding, as it can be used during annual national meetings to motivate habilitation managers across all regions to register more data, as well as to help more families understand the utility of participating in CPCog follow-up.
Finally, given the limited breadth of registry data, this study could not account for unknown confounders, such as important demographic factors (e.g., race, ethnicity, language) and social determinants of health (e.g., neighborhood/distance from habilitation centers, parental/caretaker education, socioeconomic status, trust in institutions). Still, the work presented in this paper delivers valuable insight in support of why a broader range of sociodemographic data and research are necessary to consistently strive for equitable care.
Conclusions & directions for future work
The cognitive assessment of children with CP is a nascent and layered issue within disability and rehabilitation. In Sweden, between the years 2017-2020, less than 5% of children with CP who were eligible for a cognitive assessment had one registered each year. In Norway, where the CPCog protocol is also used and data on cognition are registered in an equivalent national registry, 62% of eligible children had a cognitive assessmnent registered by the end of 2020. This signals that the registration of cognitive assessment data in Sweden can be vastly improved. Notably, we found that children with lesser communicative and manual abilities, as well as children ages 11–14 years, were less likely to receive cognitive assessments.
As we predicted that complex communication needs could impact children’s reception of cognitive assessments, we explored psychologists’ perceptions and use of communicative aids (AAC and interpreters) for conducting cognitive assessments. Our findings suggested that psychologists perceived more reliability in AAC than interpreters, there was underuse of AAC during cognitive assessments, and there was a discrepancy between the registered versus reported use of interpreters. In light of these findings, we discussed the complexities of using AAC and interpreters for cognitive assessments. Not using AAC or interpreters when they are needed might lead to the under- or overestimation of a child’s cognitive abilities. However, if these aids are to be used during cognitive assessments, their reliability should be ascertained through more research and testing. Altogether, our study’s findings could aid in informing testing companies, who copyright cognitive assessments, to develop more inclusive guidelines or assessments for persons with disabilities which impact communication and fine motor skills. Greater availability of, and capacity to offer, cognitive assessments in more formats and languages could help increase test accessibility for all children with CP.
Acknowledgements
The authors thank the CPUP user group for their insightful feedback on this research and Dr. Mikkel Kranker Jørgensen for his thoughtful feedback on the manuscript.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Stadskleiv K. Cognitive functioning in children with cerebral palsy. Dev Med Child Neurol. 2020;62(3):283–289.
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders (DSM-5®). Washington D.C.: American Psychiatric Pub; 2013.
- World Health Organization. International classification of diseases for mortality and morbidity statistics (11th Revision) 2018.
- The National Board of Health and Welfare. Swedish disability policy: service and care for people with functional impairments 2009. p. 126–88.
- Cummins D, Kerr C, McConnell K, et al. Risk factors for intellectual disability in children with spastic cerebral palsy. Arch Dis Child. 2021;106(10):975–980.
- Stadskleiv K, Jahnsen R, Andersen GL, et al. Neuropsychological profiles of children with cerebral palsy. Dev Neurorehabil. 2018;21(2):108–120.
- Andersen GL, Irgens LM, Haagaas I, et al. Cerebral palsy in Norway: prevalence, subtypes and severity. Eur J Paediatr Neurol. 2008;12(1):4–13.
- Himmelmann K, Beckung E, Hagberg G, et al. Gross and fine motor function and accompanying impairments in cerebral palsy. Dev Med Child Neurol. 2006;48(6):417–423.
- Sigurdardottir S, Eiriksdottir A, Gunnarsdottir E, et al. Cognitive profile in young icelandic children with cerebral palsy. Dev Med Child Neurol. 2008;50(5):357–362.
- Knudsen M, Stadskleiv K, O’Regan E, et al. The implementation of systematic monitoring of cognition in children with cerebral palsy in Sweden and Norway. Disab Rehab. 2022;1–10. doi: 10.1080/09638288.2022.2094477.
- Bøttcher L, Stadskleiv K, Berntsen T, et al. Systematic cognitive monitoring of children with cerebral palsy–the development of an assessment and follow-up protocol. Scand J Disab Res. 2016;18(4):304–315.
- CPUP. CPUP -Uppföljningsprogram för personer med cerebral pares (CP) CPUP. 2021. https://cpup.se/vad-ar-cpup/
- Wechsler D. Wechsler preschool and primary scale of intelligence. 4th ed. Swedish version. Bromma: Pearson Clinical; 2014.
- Wechsler D. Wechsler intelligence scale for children. 5th ed. Swedish version. Bromma, Sweden: Pearson Clinical; 2016.
- Beery KE, Buktenica NA, Beery NA. Beery-Buktenica developmental test of Visual-Motor integration. 6th ed. (Beery VMI). Indianapolis: The Psychological Corporation, Harcourt Brace; 2010.
- Gioia GA, Isquith PK, Roth RM. Behavior rating inventory for executive function. In: Kreutzer JS, DeLuca J, Caplan B, editors. Encyclopedia of clinical neuropsychology. Cham: Springer International Publishing; 2018. p. 532–538.
- Kurmanaviciute R, Stadskleiv K. Assessment of verbal comprehension and non-verbal reasoning when standard response mode is challenging: a comparison of different response modes and an exploration of their clinical usefulness. Cogent Psychol. 2017;4(1):1275416.
- Geytenbeek JJ, Mokkink LB, Knol DL, et al. Reliability and validity of the C-BiLLT: a new instrument to assess comprehension of spoken language in young children with cerebral palsy and complex communication needs. Augment Altern Commun. 2014;30(3):252–266.
- Von Tetzchner S, Martinsen H. Introduction to augmentative and alternative communication: Sign teaching and the use of communication aids for children, adolescents and adults with developmental disorders: Whurr London. 2000.
- Carone DA, Strauss E, Sherman EMS, et al. A compendium of neuropsychological tests: administration, norms, and commentary: a review of: “oxford university press, New York, 2006”. Lezak, New York: Taylor & Francis; 2007.
- Lezak MD, Howieson DB, Loring DW, et al. Neuropsychological assessment. USA: Oxford University Press; 2004.
- International Test Commission. The ITC guidelines for translating and adapting tests 2017. www.InTestCom.org
- Andersen G, Mjøen TR, Vik T. Prevalence of speech problems and the use of augmentative and alternative communication in children with cerebral palsy: a registry-based study in Norway. Perspect Augment Altern Commun. 2010;19(1):12–20.
- Batorowicz B, Stadskleiv K, Renner G, et al. Assessment of aided language comprehension and use in children and adolescents with severe speech and motor impairments. Augment Altern Commun. 2018;34(1):54–67.
- Spillane MM, Ross KK, Vasa SF. A comparison of eye‐gaze and standard response mode on the PPVT‐R. Psychol Schs. 1996;33(4):265–271.
- Westbom L, Hägglund G. Refugee/immigrant children with cerebral palsy in the Swedish health care organization. Lakartidningen. 2019;116:FL9L.
- Westbom L, Hagglund G, Nordmark E. Cerebral palsy in a total population of 4–11 year olds in Southern Sweden. Prevalence and distribution according to different CP classification systems. BMC Pediatr. 2007;7(1):1–8.
- Petersen TG, Forthun I, Lange T, et al. Cerebral palsy among children of immigrants in Denmark and the role of socioeconomic status. Eur J Paediatr Neurol. 2019;23(3):507–516.
- Josenby AL, Czuba T, Alriksson-Schmidt AI. Gender differences in treatments and interventions received by children and adolescents with cerebral palsy. BMC Pediatr. 2020;20(1):45.
- Statistics Sweden. Different living conditions for children with Swedish and with foreign background: Statistics Sweden; 2017. https://www.scb.se/en/finding-statistics/statistics-by-subject-area/living-conditions/living-conditions/children-and-their-families/pong/statistical-news/children-and-their-families-2016/
- Kammarkollegiet. Fler auktoriserade tolker - vägen dit: Kammarkollegiet; 2017. https://www.kammarkollegiet.se/download/18.1abda2991677d325932f52a/1551777025426/Fler%20auktoriserade%20tolkar%20-%20v%C3%A4gen%20dit_Kammarkollegiet%20
- Granhagen Jungner J, Tiselius E, Blomgren K, et al. Language barriers and the use of professional interpreters: a national multisite cross-sectional survey in pediatric oncology care. Acta Oncol. 2019;58(7):1015–1020.
- Pergert P, Ekblad S, Enskär K, et al. Obstacles to transcultural caring relationships: experiences of health care staff in pediatric oncology. J Pediatr Oncol Nurs. 2007;24(6):314–328.
- Suurmond J, Lieveld A, Van de Wetering M, et al. Towards culturally competent paediatric oncology care. A qualitative study from the perspective of care providers. Eur J Cancer Care. 2017;26(6):e12680.
- Patriksson K, Wigert H, Berg M, et al. Health care professional’s communication through an interpreter where language barriers exist in neonatal care: a national study. BMC Health Serv Res. 2019;19(1):1–8.
- Norström E, Gustafsson K, Fioretos I. Interpreters in Sweden–a tool for equal rights? Gramma J Theory Critic. 2011;19:59–75.
- Sveriges Riksdag. Patientlag (2014:821): Sveriges Riksdag; 2014. https://www.riksdagen.se/sv/dokument-lagar/dokument/svensk-forfattningssamling/patientlag-2014821_sfs-2014-821
- Angelelli CV. Healthcare interpreting explained. New York, NY: Routledge; 2019.
- Pöchhacker F. Research and methodology in healthcare interpreting: center for translation studies. Vienna: University of Vienna; 2006.
- Major G, Napier J. Interpreting and knowledge mediation in the healthcare setting: what do we really mean by “accuracy”?2012.
- Statistics Sweden. Summary of population statistics 1960–2020: Statistics Sweden 2021. https://www.scb.se/en/finding-statistics/statistics-by-subject-area/population/population-composition/population-statistics/pong/tables-and-graphs/yearly-statistics–the-whole-country/summary-of-population-statistics/.
- CPUP. Årsrapport 2019 Lund, Sweden 2019. https://cpup.se/wp-content/uploads/2019/10/%c3%85rsrapport-CPUP-2019-PDF.pdf
- 1177 Vårdguiden. Hitta vård: 1177. Vårdguiden; 2021. https://www.1177.se/hitta-vard/?st=67842811-d7d9-4b53-bebb-0c7b20f256ed&nearby=false&s=name&g=&lat=&lng=&location=&caretype=Barnhabilitering&q=
- Harris PA, Taylor R, Minor BL, REDCap Consortium, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
- Palisano R, Rosenbaum P, Walter S, et al. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol. 1997;39(4):214–223.
- Eliasson AC, Krumlinde‐Sundholm L, Rösblad B, et al. The manual ability classification system (MACS) for children with cerebral palsy: scale development and evidence of validity and reliability. Dev Med Child Neurol. 2006;48(7):549–554.
- Hidecker MJC, Paneth N, Rosenbaum PL, et al. Developing and validating the communication function classification system for individuals with cerebral palsy. Dev Med Child Neurol. 2011;53(8):704–710.
- Cans C. Surveillance of cerebral palsy in Europe: a collaboration of cerebral palsy surveys and registers. Develop Med Child Neurol. 2007;42(12):816–824.
- Core Team R. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2019.
- RStudio Team. RStudio: Integrated development for R. Boston (MA): R Studio, PBC; 2020.
- Sherwell S, Reid SM, Reddihough DS, et al. Measuring intellectual ability in children with cerebral palsy: can we do better? Res Dev Disabil. 2014;35(10):2558–2567.
- Geytenbeek J, Harlaar L, Stam M, et al. Utility of language comprehension tests for unintelligible or non‐speaking children with cerebral palsy: a systematic review. Dev Med Child Neurol. 2010;52(12):e267–e77.
- NorCP. Årsrapport for 2020 med plan for forbedringstiltak: NorCP; 2020. https://www.siv.no/seksjon/CP-registeret_/Documents/Arsrapporter/NorCP%202020%20Årsrapport.pdf
- Accardo PJ, Capute AJ. Capute & accardo’s neurodevelopmental disabilities in infancy and childhood. The spectrum of neurodevelopmental disabilities. Baltimore, MD: Paul H. Brookes Pub.; 2008.
- Reddihough D. Cerebral palsy in childhood. Aust Fam Physician. 2011;40(4):192–196.
- Rosenbaum P, Paneth N, Leviton A, et al. A report: the definition and classification of cerebral palsy April 2006. Dev Med Child Neurol Suppl. 2007;109(suppl 109):8–14.
- ITC. The ITC guidelines for translating and adapting tests. 2nd ed. 2017. www.InTestCom.org
- Bansal A. Training healthcare professionals to work with interpreters. Br J Gen Pract. 2013;63(609):183–184.
- Ertl A, Pöllabauer S. Training (medical) interpreters—the key to good practice. MedInt: a Joint European Training Perspective. J Special Transl. 2010;14:166–193.
- Woll A, Quick KK, Mazzei C, et al. Working with interpreters as a team in health care (with care) curriculum tool kit for oral health professions. MedEdPORTAL. 2020;16:10894.
- Hadders-Algra M. Early diagnosis and early intervention in cerebral palsy. Front Neurol. 2014;5:185.

