Abstract
Purpose
To explore the personal and system factors that motivate and enhance outcomes for patients accessing a prosthetic service and using a lower-limb prosthesis within a low resource setting.
Materials and methods
This study employed a qualitative approach to explore the motivations and satisfaction of individuals with lower limb loss engaging with a prosthetic service in Mombasa, Kenya. In-depth interviews were conducted over Microsoft Teams with 10 lower limb prosthesis users and thematic analysis was applied.
Results
Five key themes emerged: acceptance, self-determination, hope, clinician relationship and perception. These findings demonstrate the importance of hopeful thinking and a supportive community in overcoming physical and stigmatising challenges. The findings further highlight the value of the service provider relationship beyond just prescribing an assistive device.
Conclusion
These results have relevance in developing patient-centred services, assistive devices and personnel training that are responsive, motivating, and cognisant of the service user. This is of particular interest as assistive technology services are newly developed in low resource settings.
This research provides an understanding of lower-limb prosthesis users’ satisfaction of a device and motivation for engaging with a prosthetic service within a low resource setting.
The relationship the rehabilitation professional has with the service user plays a significant role in facilitating motivation during rehabilitation.
Rehabilitation professionals should consider how they can foster a network of support amongst service users when planning services in remote, rural locations.
Rehabilitation professionals should be aware of how hopeful thinking can be facilitated during rehabilitation to support motivation.
When reviewing the success of services, or designing new service models, the service users should be consulted on what they would deem as a successful outcome.
IMPLICATIONS FOR REHABILITATION
Introduction
An estimated 1.5 million people undergo limb amputation each year [Citation1]. Low- and middle-income countries (LMICs) are projected to have a rapid increase in people living with an amputation in the coming years due to prevalence of non-communicable disease, trauma and conflict [Citation1–3].
Limb amputation can have a significant impact on the health, wellbeing and self-identity of a person [Citation4–7]. There are multiple, complex biopsychosocial factors involved in the process of loss and adjustment to a changed appearance as well as difference in functional ability [Citation7]. Studies have described how amputation can lead to a stark loss of independence and new feeling of burden (and dependence) on family and caregivers [Citation2,Citation7,Citation8].
Assistive technology
A prosthesis is an external device used in place of the absent limb [Citation9]. Prosthetics are an example of Assistive Technology (AT) that offer the potential to improve the mobility, quality of life and opportunity of a person with limb loss [Citation6,Citation7,Citation10]. They are identified as one of the five priority assistive products urgently needed globally [Citation11].
The World Health Organisation (WHO) estimate only 5–15% of people living with limb loss in LMICs have access to a needed prosthesis with demand projected to double by 2050 [Citation12]. This has led to an increasing global effort to understand the inherent complexities causing the gap in AT provision and how best to achieve appropriate and affordable AT access in LMICs [Citation13,Citation14,Citation15]. If the device does not suit the needs of a person or environment, then there is a risk of device rejection and service dissatisfaction [Citation16].
Prosthesis prescription
Prosthesis prescription can consist of multiple appointments and follow-ups in specially equipped clinics where an ongoing relationship with the prosthetist is needed [Citation9,Citation17]. New technological advancements may provide time-efficient and cost saving options which could enable more global provision. Studies have been trialling new technical interventions to help drive provision, e.g., through digital scanning and fabrication [Citation18,Citation19], and novel direct to limb fitting [Citation20] as well as the ability to provide mobile prosthesis services [Citation21]. These approaches are potentially advantageous in low resource settings where prosthetic service points are particularly scarce, and users often have to travel far to reach them [Citation1].
A person’s motivation to engage in services and rehabilitation has been anecdotally reported by health professionals as a key determinant of outcome. The multiple clinic visits required, often necessitating days away from work and family, can be particularly challenging in low resource settings where services are few and far between [Citation22]. There is also effort involved in learning to use, maintain and find comfort with the device [Citation23]. It is unsurprising therefore that motivated patients would be more likely to succeed in their rehabilitation, but research into the factors influencing individual prosthesis user motivation is lacking [Citation6,Citation24–26]. How we understand and design services to improve and support patients to be motivated in their rehabilitation will be key in broadening access to these important devices [Citation27].
Review of the literature
Intrinsic factors
Factors related to the individual response to an amputation, such as adjustment, coping, expectations, as well as personality factors, have been reported in literature in high income settings to influence motivation during rehabilitation [Citation24,Citation28]. A meta-synthesis of papers, largely from Europe, UK, USA, and Australia, found participants commonly reported on the importance of a positive and proactive outlook in overcoming challenges [Citation8]. In a Taiwanese study, an optimistic outlook and psychological adjustment were found to improve experiences of pain and ability to adapt to a new way of life [Citation7].
In qualitative research in the UK, having a strong determination to walk has been considered pivotal in having a successful outcome – as essential as the physicality required [Citation28]. An observational study in Japan of 64 unilateral lower limb amputees found a statistically significant correlation between motivation to walk and successful prosthesis use [Citation6].
The belief in a prosthesis to bring renewed independence and reduced dependence on others has been found to be highly motivating [Citation7,Citation28,Citation29]. Prosthesis users in Ireland discussed feelings of increased independence through the completion of functional and social activities that had a positive emotional and psychosocial impact, such as an increase in feelings of self-efficacy and reduced dependency on others [Citation29].
The physical challenge of rehabilitation has been found to be equally motivating by Danish military patients who reap rewards and satisfaction from performing well and pushing levels of physical progress [Citation30]. In contrast, overly ambitious activity goals have been demotivating for some civilian patients [Citation24]. Tailoring rehabilitation to the intrinsic motivations of the individual is therefore pertinent.
Social relationships
Social relationships can be fundamental for patient recovery post amputation [Citation8]. A study in the UK identified positive family influence as having an impact on motivation and patient advocacy [Citation26]. However, potential negative influence was seen when relatives put undue pressure on patients.
Aside from family, peer support from other individuals with limb loss can be significantly motivating. Peer support can help educate, reduce emotional distress, and provide participants with a more optimistic perspective [Citation7,Citation28,Citation31].
Relationships with the prosthetist, a clinician who makes and fits prosthetic limbs, can equally influence motivation [Citation32]. Studies have found how positive, supportive experiences with clinicians can increase engagement and motivation during lower limb rehabilitation [Citation33], although professionals can equally be a source of frustration and reduce interest in the rehabilitation process [Citation30,Citation32].
Understanding research in low resource settings
Most studies exploring individual’s motivation in depth, are from high resource settings with participants who have, arguably, greater access to a prosthesis service. When looking to LMICs, studies have outlined the importance of understanding the context when implementing new prosthesis services as cultural beliefs, income and identity could influence prosthesis uptake [Citation2,Citation27].
Prosthetists working in LMICs remarked on how avoiding societal stigma and associations of inferiority for those living with a disability can be motivating. Prosthesis users may want to appear “non-disabled” and acquire a prosthesis to conceal impairment and maximise reintegration into society [Citation27]. Even hospital staff have been found to contribute to stigma: a participant from a study in South Africa reported being discouraged from accessing services due to ridiculing from hospital staff after a local healer had placed traditional bands around his residual limb [Citation33].
Financial factors may be particularly motivating for users in studies from low resource settings, where inadequate public funding does not cover basic needs and physical ability to return to work through prosthesis use is a matter of necessity [Citation33]. Conversely, one individual in receipt of a free prosthesis from the Haitian Amputee Coalition post-earthquake in Haiti explained he would rather have the equivalent cost of the prosthesis to kick-start his business over receiving the device [Citation34]. In South Africa family support was a financial facilitator, reducing travel costs for participants when family members accompanied them to rehabilitation [Citation33]. Understanding the contextual, environmental, and financial factors within which the prosthesis service fits is therefore important for service development.
Summary
In summary, evidence has outlined how motivation is highly individual and a multifaceted phenomenon which can determine or hinder successful rehabilitation, influenced by intrinsic and extrinsic factors reported above.
The depth of research on prothesis user motivation has been focused on high income settings with only some studies identified from LMICs. There is a need to better understand the factors which influence prosthesis user motivation, within the LMIC context, to maximise prosthesis success, service delivery and reduce risk of product abandonment.
This information can help inform prosthetic service and technology design, particularly where services are newly established. This is of particular interest with the demand for AT service development in low resource settings [Citation1]. To help address this gap, we explore the motivations of prosthesis users living in Kenya.
Kenya is economically regarded as a lower-middle income economy that has scarcity of prosthesis service provision [Citation1,Citation35]. The research site selected was the Association for the Physically Disabled of Kenya (APDK) clinic in Mombasa which is a non-profit organisation that aims to improve the lives of disabled people through rehabilitation and empowerment [Citation36]. Therefore, the aim of this study was to explore the factors influencing motivation of lower limb amputees engaging with prosthesis services in Mombasa, Kenya. This was achieved through three objectives:
To understand motivating factors for individuals accessing a prosthesis through the APDK clinic in Mombasa.
To explore factors that influence prosthesis satisfaction in a low resource setting.
To identify barriers and opportunities that may inform future research and service delivery in low resource settings.
Materials and methods
The study utilised a qualitative methodology. Qualitative research provides a flexible and sensitive method of understanding the lived experiences of individuals within the specific context [Citation37]. Semi-structured interviews were conducted over Microsoft Teams due to the COVID-19 pandemic restricting travel and researchers and participants living across the UK and Kenya. Thematic analysis was used to identify reappearing patterns in the transcribed interview data, while allowing flexibility in encapsulating answers to the research question and aim [Citation37–40].
Ethics statement
Ethical approval was granted by AIC Cure Hospital Internal Review Board (Committee protocol No. 4465) and Association for the Physically Disabled of Kenya (APDK) and the University College London Ethics Committee (Committee protocol No APDKNAT/AmparoGmbH/001/05/2019).
Participant selection and recruitment
Participants were recruited by author JG who worked at the APDK rehabilitation clinic during July to August 2020 and could approach participants who met the inclusion criteria directly. This selection pool from APDK meant all participants would have at one point been offered or trialled a prosthesis. Participants were invited to take part in the study if they were over 18, had a lower limb amputation and had access to a mobile phone. There were no other limitations on the inclusion criteria as all experiences related to level of amputation, cause of amputation, and length of prosthesis use were considered of interest in answering the research question. The authors acknowledge the requirement for mobile phone access may have been a barrier to some participants, however some element of phone communication was required due to the COVID-19 pandemic limiting face-to-face conversations for safety reasons.
The aim for recruitment was 10 participants which was considered an adequate and achievable sample for a small-scale research project with time limitations. 10 participants was thought to be sufficient in providing rich data that would support the identification of patterns (codes) and where no new information would have been discovered from interviewing more participants [Citation37,Citation41].
The first 10 participants JG approached agreed to take part in the study. JG then provided participants with a participant information sheet and consent form and provided support for translation for participants who did not speak English.
Participant demographics
Equal numbers of male and female participants were sought to avoid influencing results based on gender, however due to more males than females accessing the clinic, eight male participants and two female participants were identified, these were the first 10 participants JG approached.
All participants had a below knee (i.e., transtibial) amputation, five were due to accidents involving transport or at work during adult life, two were due to injuries whilst playing as a child and three were due to wound complications secondary to diabetes. The ages ranged from 24 to 60 with a mean age of 39.
Demographics are fully outlined in .
Table 1. Participant Characteristics, *where information has a "-" it is because it was not known.
Data collection
Researcher JG was based in the region of the centre and facilitated participant recruitment, the researchers KM, BO, and CH were UK based and unable to travel to the region due to the COVID-19 pandemic. Researcher GM, who is based in Nairobi and a Swahili speaker assisted during all interviews and on transcription to improve consistency to the questioning and transcripts [Citation37]. Once JG had identified 10 participants who had read the participant information sheet and consented to being in the study, their names and telephone numbers were sent to GM and the UK based researchers securely. GM arranged times and dates for the interviews and confirmed over telephone that participants had read the information sheet, understood the purpose of the study and gained their verbally informed consent.
On the agreed time and date researcher KM and GM called the participant via conference call on Microsoft Teams. Before starting the interview, participants were asked if they had any outstanding questions about the study. The semi-structured interview was conducted following an interview guide (Supplementary Appendix 1) containing open questions and prompts. The interview guide was developed in collaboration with JG and GM who are both from Kenya and could advise on the context and cultural sensitivity of questions. Questions covered how the participants had heard about the clinic, how they travelled and their motivations. The guide helped explore the topic area systematically whilst allowing scope for participants to discuss issues not specifically anticipated [Citation37,Citation42].
Eight interviews were conducted in Swahili and, at the participants request, two interviews were conducted in a mixture of English and Swahili. All participants consented to being audio-recorded. The recordings were transcribed, anonymised and pseudonyms were given. Participants were reimbursed by the research team for telephone credit and provided with renumeration for their time which was agreed at the point of recruitment.
Data analysis
All interviews were recorded and transcribed immediately by the translator GM and interviewer KM. Transcripts were uploaded to Nvivo-12 and each given a pseudonym based on common name choices in Mombasa.
Thematic analysis was chosen due to its flexibility in methods of data collection and use in identifying patterns and drawing meaning across data [Citation37]. Although the researcher recognises there were pre-identified themes in the literature review these did not serve as theoretical ideas from which to perform a top-down analysis of the results. As such inductive thematic analysis was the primary method of data analysis.
Following a staged approach outlined by Braun and Clarke [Citation37] the researcher began the analysis by reading through transcripts for familiarisation of the content.
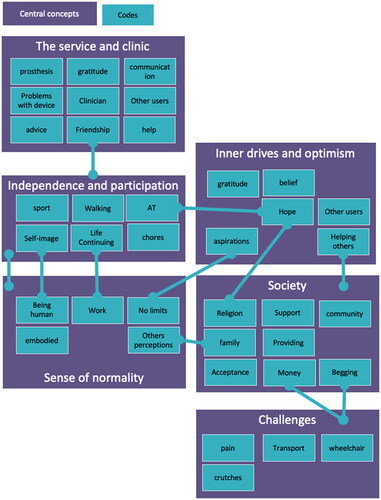
The transcripts were then searched for codes that were relevant and of interested to the research question. The codes served as concise phrases that represented the raw data. Once coding was completed, the researcher reviewed if the collated text represented the code it was assigned to, searched for overlaps within the codes and looked to see if the text reference could be assigned to another code. This immersive process helped the researcher look for broader patterns from the codes and identify central concepts (themes). These initial candidate themes served to tell the participants story, capturing something important that answered the research question ().
Figure 1. Figure showing central concepts and codes of the theme development.
After this initial theme generation, the researcher returned to the raw and coded data to ensure each theme was relatable to these and to check no important messages had been missed and that each theme was distinctive of the other. Themes were then defined and named with quotes from the participants, that captured the overarching concept but remained true to the participant’s language.
Researchers BO, CH and MDH enhanced the confirmability and credibility of the findings through reviewing sections of the raw data to confirm the themes were appropriate and accurately represented the data.
Reflexivity
The two researchers who were largely involved in participant recruitment and initial data analysis were JG, an APDK clinician and KM, a UK based clinician. As two rehabilitation professionals they identify how their own subjectivity and assumptions from working with patients may influence the research findings [Citation39].
Researchers’ perspective – JG, a APDK clinician
Author JG is a Kenyan orthopaedic technologist with 7 years of clinical experience working with clients in Kenya. At the time of the study JG worked at APDK rehabilitation clinic and could recruit the participants to the study. JG knew the participants well from a clinical perspective and while following the inclusion criteria there could be potential introduction of bias through participant selection. Those who were already engaged with the service and had a good relationship with JG would perhaps be more likely to be approached, and willing, to take part in research. To reduce the bias of JG’s influence on data collection, he was not part of the interviews and an independent translator, unknown to participants, was asked to support in the translation from English – Swahili.
Researchers’ perspective – KM, a UK clinician
KM, the first author who largely led on interviews and data analysis, is a UK trained physiotherapist, having worked in the UK and internationally.
KM recognises how her experiences working with patients during rehabilitation could have been consequential for her desire to study motivation and on the analysis of results. KM has first-hand experience of seeing how a person’s perceived motivation could either facilitate or be a barrier to “success” and future access to services. KM was particularly interested in studying motivation as she had prior experience of seeing how patients who were highly motivated to engage in rehabilitation often had a more hopeful outlook about their injury or illness and would approach challenges with positivity. These motivated patients seemed more likely to be referred on to further rehabilitative services, and KM was interested in thinking about her own role in facilitating motivation in the patients she worked with.
During the interview design, to minimise bias and enhance the dependability of the method, KM worked alongside other non-clinical researchers, BO and CH to shape the research aims and design non-leading interview questions that were based on the literature review over her clinical experience. This was of benefit to reduce the prior assumptions about motivation KM had noted in herself. Conducting the research in a different language provided opportunity for KM to reduce the risk of introducing bias during the conversation between the translator and participant. During analysis, KM strived to see outside of a physiotherapy lens’ when coding data and completed an audit trail to allow others to critique the process. Despite the efforts to reduce bias, KM recognises that she is conditioned to a health provider perspective which will impact interpretation of results – perhaps searching for themes and practical application to rehabilitation services. To reduce researcher bias and enhance the trustworthiness of the results investigator triangulation and confirmability was sought from non-clinical researchers BO, CH and MDH to ensure the identified themes were appropriate based on the coded and translated text. Aside from the potential researcher bias acknowledged by KM above, the researchers also identify other limitations of this study in the potential participant bias. Participants may have provided information they believe is desirable and perhaps the context of data capture does not capture the “real world.” There is also missed information from those patients who were no longer engaged in the service offered at APDK.
Results
Themes
Analysis produced five overarching themes. Titles for each theme were created using pertinent quotes from the participants:
Theme 1: Acceptance: “You have to now accept”
Theme 2: Self-determination: “I have the will”
Theme 3: A source of hope: “They had given me faith and hope”
Sub-theme 3.1: “We can encourage each other”
Sub-theme 3.2: “I believe in prostheses 100%”
Theme 4: Clinician Relationship: “When I tell him my problems, he listens”
Theme 5: Perception: “I will be like a normal human being”
Theme 1: acceptance – “you have to now accept”
The participants identified acceptance as an important part of their journey following an amputation. Acceptance was important in coming to terms with their disability and having a successful outcome with the prosthesis, as described by Neema and Abdi:
The challenge that is there is that you have to now accept that you are the way you are now unlike the way you were before. (Neema)
Because after all, my life has changed yes, my life has changed but at least the prosthesis has helped me I can move I can walk. (Abdi)
The gratitude in Abdi’s quote was echoed by others and appeared to form part of this acceptance process. Deep gratitude was felt towards the prosthesis in helping participants move forward with their life as well as to a higher being, God.
I will give thanks to God and there is no one else I would give praise and thanks to except him (Aisha)
Faith appeared to have a profound influence on how our participants accepted and dealt with challenges, as well as providing a source of hope.
The gratitude participants felt appeared to perhaps be enhanced by the scarcity of available services: some participants had been without a prosthesis for 7 years and were aware that not everyone will access to what they have. Ali and Hamisi described this experience:
Some they can’t get the crutches, they are just crawling, that is so hard. Some they are using tricycle or wheelchair (Ali)
if I hadn’t that leg I don’t know where I would be and maybe I would be on the road begging but I am not begging and that’s why I am thankful that I am continuing with my life well (Hamisi)
Theme 2: self-determination – “I have the will”
When discussing what participants felt influenced a successful outcome following an amputation, several participants identified how the determination of the individual is key:
If in my heart I have the will and hope that once I have the prosthetic leg I can achieve the goals I had wanted to achieve (Neema)
It is your own determination; I have never discouraged myself by saying that I have no leg or by saying I can’t do this (Issa)
A person should voluntarily do this and don’t be lazy with the exercises and even if they fall down they should give themselves hope and get themselves to stand up without any assistance from someone (Baraka)
Self-determination was seen as important when overcoming challenges. Challenges identified at the initial stage of prosthesis use were described as pain, socket discomfort and wound healing, which participants identified as often easing with perseverance of limb use:
[the prosthesis] was burning me…the rubber was very tight and walking was a problem…with time the skin became used after the swell and healing and it became comfortable. (Juma)
This determination to persevere appeared to derive from several different sources. Notable was the desire to avoid situations they believed to be undesirable or that created increased reliance on others. This included the avoidance of other pieces of Assistive Technology (crutches, wheelchairs) that were seen less favourably than the prosthesis:
You know when I lost my legs I was using a wheelchair… I started relying on other people (Chaka)
I used to see as if my life was over since moving in crutches people look at you and say that you are hurt or lame (Hamisi)
Theme 3: faith and hope – “they had given me faith and hope”
This overarching theme was derived from participants speaking about circumstances which had provided hope. It is divided into two subthemes: “We can encourage each other” and “I believe in prostheses 100%,” the subthemes respectively represent the support network of people and the prosthesis device as a source of hope.
Sub-theme: “We can encourage each other”
Participants spoke about family, friends and neighbours who motivated them on their journey. This was through several different support mechanisms, such as emotional, physical, and financial support:
There is my brother who saw about prosthesis in the internet and he called me… he told me he will help me… he told me he would love to see me stand again and work for myself… he got their numbers and called them, got the information, then he sent me fare to travel (Chaka)
This empathy and understanding from people around them appeared to provide encouragement for participants to persist and seek help. In particular, speaking with other prosthesis users was also found to be a source of inspiration:
I have a friend who has the prosthesis so sometimes we can talk, we can encourage each other because you know sometimes it can be hard so we can share the challenges we are facing. (Abdi)
I thought I was the only person being amputated, but I can see my friends also here, they have the same problem, some is worse than me (Ali)
The sharing of challenges and experiences appeared to be particularly motivating to participants in the early stages of their prosthetic rehabilitation, especially for those who had never met someone else with an amputation and could see them use a prosthesis well.
When you see someone else is walking with the prosthesis… that made me have hope (Neema)
Participants who were further along in their prosthesis journey then recognised how they had become inspired to support others who were newly adjusting to limb loss and prosthesis use:
You can help them in their thoughts and tell them that this is how I was and explain to them how you became how you are right now. (Neema)
Sub-theme: “I believe in prostheses 100%”
The hope of receiving a prosthesis that would enable participants to walk and continue with previous activities had initially inspired participants to attend APDK. Participants spoke about some of their expectations for the device:
I just wanted to get prosthesis and be able to walk again, those were my expectation, I had been told that there are false legs that one can get and they help one to be able to walk. (Juma)
Once accustomed to the device, the participants felt it offered endless opportunities and spoke highly of what they could now achieve:
Nothing is impossible (Issa)
Yes, now I am grateful I can do everything… I can do anything now I walk with my two legs (Mohamed)
Myself I believe in prostheses 100%, it can help one in many ways, one can be a barber, you can become a tuk-tuk driver, and you can drive an automatic car (Chaka)
Some participants did recognise that there were still tasks they could not achieve, for example:
I cannot climb a high place, the nature of my work requires me to climb high but I cannot do it on my own (Juma)
But this was often overshadowed by what they felt they could now achieve, relative to before when they were without a prosthesis.
Some participants spoke about the care they took in looking after their device, perhaps demonstrating the value they felt for it:
You know something that is of value and assistance needs to be nurtured, but if you have a don’t care attitude, you will hurt yourself and damage that which is helping you (Baraka)
Theme 4: clinical relationship – “when I tell him my problems he listens”
Participants provided insight into their experiences of the service delivery and the support offered by the service provider. They spoke about their provider as both a clinical expert and friend. The participants were initially motivated to attend the clinic as they viewed it with great hope as a place to get the support needed, even if they weren’t sure what to expect:
I can say it is the hope I had that once I went there I would be able to get the prosthesis (Aisha)
Once at the clinic, the service provider offered motivation. Guiding participants through the journey with reassurance and encouragement to persevere and expect some challenges:
I did not know how to walk with it, but [the Doctor] really helped me and told me I can move with it and I can walk, because I was [like] a child, he used to teach me on how to walk (Abdi)
Participants had faith in their service provider to solve problems they encountered. They felt able to call for help when needed, returning to the clinic, and displaying deep gratitude for the clinician’s support – who they unanimously referred to as “doctor”:
When I go the doctor asks me my problem and I explain, if my leg has broken he repairs it for me, when I tell him my problems he listens (Mohamed)
As well as holding their service provider in high regard, the participants spoke about their clinician fondly, feeling cared for, loved, and having formed friendships:
It is home since it made me walk again. In short APDK is my home (Baraka)
they treated me in a nice way and they loved me so that’s why sometimes they keep in touch, they like to know how they progress. (Ali)
Theme 5: perception – “I will be like a normal human being”
The participants hoped the prosthesis could help them return to a perceived normality. This perception of returning to “normality” was described through a physical appearance that matched their identity, ability, and societal perception prior to the injury. This included the ability to carry out day-to-day tasks such as cooking and cleaning, having a job and providing for a family.
Baraka first explains what he expected to be able to do prior to receiving the prosthesis, and then what he felt he had achieved when using it:
My expectations were I will be like a normal human being and be able to wear my shoes and wear my trousers and be able to go where I used to go in search of my basic needs (Baraka)
This ability to carry out tasks with a prosthesis appeared motivating in reducing the dependency one had on others. For example, Chaka who is a bilateral amputee and had been a wheelchair user for 3 years prior to receiving the prostheses. Since receiving the prosthetics, he had opened his own barber shop and how he could now “depend on myself.” He was not alone; others spoke significantly about reduced dependency:
I can take myself to the shop without any help, unlike there before when I used to depend on people to help me, I can go by myself to the toilet without asking for help (Mohamed)
Independence also meant the opportunity to work, something all participants were highly motivated by, which appeared to be irrespective of age or gender. Working appeared aligned with their sense of identity and roles in terms of being able to provide for themselves as well as others.
For now, I can work and get my own 500ksh without asking to be given by anybody, I am able to do my own work without depending on anybody… [I can] buy my children sugar for tea to be like other children (Juma)
Becoming self-reliant seemed motivating for participants’ own positive self-perception but also intrinsically linked to how participants felt others perceived them with their prosthesis on:
where I am people call me “boss” and I am very thankful and when you see me you will not know and you will just know I am a boss of a certain area (Hamisi)
Some participants described the experience of embodiment through using their prosthesis which added to their sense of a returned “normality”:
My experience ever since I put on the leg I feel as though I have my original leg (Issa)
Although the prosthesis was sometimes described as feeling like their previous limb, there was divided opinion over whether the prosthesis needed to aesthetically mirror this. Many felt it was not of importance so long it was helping in function, as exampled below:
I cannot feel ashamed to the prostheses that enables me to work and provide for my family, I can walk with shorts and careless (Chaka)
But this was not true for everyone, Abdi for example, explained:
I would like it to be more advanced in function and how it looks like…I would like it to be like my skin colour (Abdi)
A return to normality was motivating for participants and facilitated through the gain of functional tasks, the ability to work and earn money, and how others perceived them.
Discussion
This study explored motivations and satisfaction of individuals with lower limb loss engaging in prosthetic services in Mombasa, Kenya. The use of an in-depth qualitative approach has provided insight and themes illustrating how participants found motivation and hope to overcome challenges following an amputation and throughout the prosthetic rehabilitation experience.
Hope
Participants described hope through self-determination and optimism that eventually their situation would become easier, and they would be able to do what they used to – returning to their perceived normality. Their hope came from their faith, social support, and relationships and appeared persistent despite any unknowns related to service or device. It appeared that hope carried participants through initial challenges and provided motivation to persevere with exercises.
The theory of hope as a motivator has been explored within rehabilitation literature. Patients who are hopeful and optimistic often have greater success in reaching their goals, are more adept at accepting and overcoming challenges, have pride and look forward rather than focusing on past failings [Citation12]. These were qualities which the participants in this research seemingly possessed with their positive outlook on their situation and appeared generally satisfied with their device. Others have outlined how hope is particularly relevant for those who have been through a traumatic, disabling condition [Citation43].
Although in this study, hope appeared to be a significant reaction for all our participants, it is important to recognise that this positive outlook may have been linked to their willingness to participate in the study and there will no doubt be many, who are not captured here, that have perhaps lost hope or disengaged with services for a wide range of reasons. Individuals may need support in sustaining a positive outlook, it would therefore be of interest for future research to explore how professionals can facilitate hope during rehabilitation [Citation44].
Clinic support
Several of the participants described how APDK was like a home to them. All the participants who had used the service had done so through the Mombasa central clinic rather than a mobile service. The need to be an inpatient due to travel challenges provided opportunity to meet other amputees who provided support and encouragement. This interaction created a support network for the user, a sense of belonging and appeared to reduce participants feelings of isolation. Previous research has also found people are motivated by the social and practical support offered by a community [Citation34]. Meeting others can offer the realisation to an individual that their situation is not unique and can be helped by the development of peer support through seeing other people’s rehabilitation achievements and the process of social comparison [Citation8].
Prosthesis technology is advancing which offers opportunity for a more seamless end-to-end process of prosthesis fitting and fabrication through digital tools like laptops and 3D printers [Citation1]. In theory, these services would be mobile with fewer fabrication steps; saving time, reducing appointments, and providing opportunity to travel to rural locations. This may offer potential advantage over the current traditional methods which require a specific immobile infrastructure. When considering the transport and money barriers encountered by patients in low resource settings, these systems may have significant advantages [Citation27].
However, if services are decentralised and appointments reduced, the significance of human interaction and sense of community gained from a clinic setting should not be overlooked. Although they are a cost-saving initiative, fragmented service delivery has found to be a potential challenge of mobile clinics [Citation21]. Perhaps service designers need to consider how to facilitate the experience of belonging and community within a mobile infrastructure.
Service provider
Participants spoke about the significance of the service providers reassurance who encouraged them to accept their situation and move forward. The participants responded well to this support, finding confidence, motivation, and high levels of satisfaction with their provider.
The service provider was key to the participants positive experience and success. All participants trusted and respected their clinician greatly, not questioning his professional opinion. He was seen as a friend as well as clinical expert. The significance of this clinician-patient relationship is documented elsewhere and the gratitude expressed for the device and service correlates to findings from a service review in Haiti, where participants had been thankful to the staff for the free service [Citation34].
These positive experiences contrast to a study which analysed online-discussion groups of prosthesis users from higher resourced settings. Here people wrote about “firing” prosthetists because they believed they didn’t listen, restricted their device options, and used their clinical experience to set limits. This angered users who felt doctors should not be seen as knowing better [Citation32]. Perhaps the anonymity achieved online enables service users to post honestly. The differences between participant expectations could, in part, be due to contextual influences. In high resourced settings, there is more opportunity for some people to become empowered about their health. People research options independently and, through exposure to increased choice, their expectations and specifications of device and service provider may heighten. This contrasts with the expectations, gratitude, and our participant perception of their clinician within Kenya where there is less opportunity of service access, choice, education, and greater financial constraints.
The participants responses’, and previous research, all example the influence a clinician can have on a patient’s journey and engagement with services. Perhaps, alongside technical knowledge, there is benefit in developing and training soft skills within providers. Soft skills can be described as traits outside of technical knowledge, e.g., effective communication, compassion and patience – which have been argued as being more important for a patient experience than clinical expertise [Citation45].
Family and friend support
The motivating influence of family and friends was evident. Some researched and informed participants about the clinic, provided financial and transport means to attend as well as ongoing emotional encouragement. This facilitating effect to service access has been demonstrated in other low resource settings and highlights the importance of involving the persons social support in rehabilitation [Citation33]. Perhaps such motivating factors are especially pronounced in Kenya’s historically collectivist culture, where there is focus on family and community [Citation46].
These findings highlight how motivation and service engagement may be impacted if an individual does not have this network and perhaps emphasise the need for clinicians to identify this early and implement strategies to counterbalance it. Our participants’ experience provide detail to be considered for future research into service planning in cultures and communities that are highly dependent on these social support structures.
Disability and stigma
Being exposed to challenges provided motivation for participants to want for something different. Participants wanted to avoid crutches because of the physicality and awkwardness of them but also because they didn’t want to be viewed as a disabled person. Crutches were regarded as being used by someone who is “sick” or “lame.” These words could be the result of translated language from Swahili or perhaps demonstrate less of a differentiation between sickness and disability within the participants context. The interviews demonstrated how participants had certain beliefs about disability which could have influenced their motivation to engage in rehabilitation so to not be seen as disabled. Other researchers have speculated how the desire to not be viewed as disabled is more important in collectivist societies due to conformity tendencies [Citation47]. These findings highlight the importance of the ongoing work of APDK in educating communities about disability. Further studies focusing on disability and stigma in these communities will be important to determine the contribution stigma has in a person’s motivation.
The differing identity raised by participants between Assistive Technology (AT), namely crutches and a prosthesis are also echoed elsewhere. Previous research found the way in which AT is perceived, by others as well as self, influences the user’s sense of identity [Citation29]. Many participants felt embodied with their prosthesis and felt great gratitude and satisfaction because of it, something which others have identified as signifying success [Citation48].
In this study, the participants’ experiences and perceptions of disability and AT identity highlight the great need for ongoing research in this field. To ensure successful device uptake and delivery further work is needed to scope which device and device appearance would bring most benefit to a user – alongside the work to destigmatise perceptions of disability and AT.
Independence
The cosmesis of the device was seemingly not as important to all as perhaps assumed. The desired normal was not about appearance, but the returning to activities that create a sense of normality e.g., caring for oneself, household chores and working. This essence of normality can be about independence, acceptance and participation in society [Citation7,Citation49].
Not being reliant on other people was an important motivator for participants who spoke about toileting and carrying water without assistance. This highlighted the worth of outwardly modest functional gains to a person. These findings correlate with other studies from different countries in stressing what is important to individuals and demonstrating that success is not merely related to how far a person can walk unaided or how often they wear the prosthesis [Citation29].
There is reported nuance between functional and emotional independence [Citation29]. A previous study results exhibited Irish participants expressing independence as a psychological outcome related to self-worth and self-esteem. The Kenyan participants in this study also addressed independence as a positive emotional shift in identity as they transitioned from being dependent to independent.
Independence helped in re-establishing the participants sense of role and purpose within family life and society, providing agency and choice over what they could do. For those with family to provide for, finding work and knowing that others were reliant on them served as an important motivator. The psychological effect of independence is important to consider when looking at what motivates people to engage in rehabilitation and in evaluating how services measure success.
This research examples the subjective nature of success and how outcome measures in current use, like “walking 100 m unaided” fail to capture true meaning of success. It would be beneficial for rehabilitation goals and outcomes to focus on the emotional and subjective experience for a person alongside a physical achievement and to work with service users in the development of services to identify for them what would be a “good” outcome. There was a noted highly positive experience with the prosthesis reported by the participants interviewed – which could be attributed to how the participants were selected as all were actively engaged with the APDK clinic. To further explore the topic of motivation within rehabilitation and the impact it has on prosthesis success, it would be important to capture perspectives from those clients who are lost to follow-up in future research.
Conclusion
In summary, the participants in our study described the adjustment to living with an amputation and the engagement with prosthesis services as an emotional journey of acceptance and gratitude. Motivation was facilitated through strong clinician-patient relationships, social support networks, community, hope and self-determination to overcome adversity.
Participants appeared highly satisfied with the device and regarded the opportunity of receiving a prosthesis as a hopeful symbolism of a better future. The prosthesis enabled them to return to activities they used to, reintegrate into society, work, and become less dependent on others. These experiences highlight the need for service evaluations to incorporate holistic markers of success and not rely purely on objective scoring systems which may miss out on the nuances of a good outcome.
Our findings support programmes like AT2030 in evidencing the need for AT globally and how a prosthesis can have a significant impact on a person’s life – with the right supportive infrastructure in place. The study conclusions also inform how services can facilitate or hinder motivation in patients. This will help guide both new service development, as well as improving and addressing issues with current service delivery.
Further research with prosthesis users in different contexts, with different levels of limb amputation would be of interest to establish patterns between service user needs globally.
Supplementary Appendices.docx
Download MS Word (15.2 KB)Acknowledgements
The researchers wish to thank all of the interviewed participants for taking the time to share their insights into life as a prosthesis user living in Mombasa.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Liao C, Seghers F, Savage M, et al. Product narrative: prostheses [Internet]. 2020. Available from: https://at2030.org/pn-prostheses/
- Harkins CS, McGarry A, Buis A. Provision of prosthetic and orthotic services in low-income countries: a review of the literature. Prosthet Orthot Int. 2013;37(5):353–361.
- International Diabetes Federation. IDF diabetes atlas. Ninth edition [Internet]. 2019. [cited 2020 Jun 22]. Available from: https://www.diabetesatlas.org/upload/resources/material/20200302_133351_IDFATLAS9e-final-web.pdf
- Murray CD, Fox J. Body image and prosthesis satisfaction in the lower limb amputee. Disabil Rehabil. 2002;24(17):925–931.
- Davidson JH, Jones Le Cornet J, Cittarelli T, et al. Disability and Rehabilitation Management of the multiple limb amputee Management of the multiple limb amputee. 2009. [cited 2020 Jun 16]; Available from: https://www.tandfonline.com/action/journalInformation?journalCode=idre20
- Hamamura S, Chin T, Kuroda R, et al. Factors affecting prosthetic rehabilitation outcomes in amputees of age 60 years and over. J Int Med Res. 2009;37(6):1921–1927.
- Liu F, Williams RM, Liu HE, et al. The lived experience of persons with lower extremity amputation. J Clin Nurs. 2010;19(15–16):2152–2161.
- Murray CD, Forshaw MJ. The experience of amputation and prosthesis use for adults: a metasynthesis. Disabil Rehabil. 2013;35(14):1133–1142.
- WHO. Standards for prosthetics and orthotics. Part 2: implementation manual [Internet]. 2017. [cited 2020 Aug 13]. Available from: http://apps.who.int/bookorders
- Jefferies P, Gallagher P, Philbin M. Being “just normal”: a grounded theory of prosthesis use. Disabil Rehabil. 2018;40(15):1754–1763.
- ATscale. Strategy overview [Internet]. 2019. [cited 2019 Oct 31]. Available from:
- Coduti W, Schoen B. Hope model: a method of goal attainment with rehabilitation services clients. J Rehabil. 2014;80(2):30–40. https://www.researchgate.net/publication/267391857
- WHO. WHO | Assistive devices/technologies: what WHO is doing [Internet]. World Health Organization; 2016. [cited 2020 Aug 2]. Available from: http://www.who.int/disabilities/technology/activities/en/
- Holloway C, Austin V, Barbareschi G, et al. Scoping research report on assistive technology on the road for universal assistive technology [Internet]. 2018. Available from: https://www.disabilityinnovation.com/uploads/images/AT-Scoping-Report_2019-compressed-19.pdf
- Hub GDI. AT2030 Testing “what works” to enable access to life-changing assistive technology for all [Internet]. 2019. [cited 2020 Jun 11]. Available from: https://www.at2030.org/at3030-leaflet/
- Arabian A, Varotsis D, McDonnell C, et al. Global social acceptance of prosthetic devices. Seattle (WA): GHTC 2016 - IEEE Global Humanitarian Technology Conference: Technology for the Benefit of Humanity, Conference Proceedings. 2016. p. 563–568.
- O’Keeffe B, Rout S. Prosthetic rehabilitation in the lower limb. Indian J Plast Surg. 2019;52(1):134–143.
- Dickinson A, Donovan-Hall M, Kheng S, et al. Technologies to enhance quality and access to prosthetics & orthotics: the importance of a multidisciplinary, user-centred approach. WHO Global Report on Assistive Technology (GReAT) Consultation. Geneva: WHO; 2019. 10.5258/soton/p0014
- Karakoç M, Batmaz I, Sariyildiz M, et al. Sockets manufactured by CAD/CAM method have positive effects on the quality of life of patients with transtibial amputation. Am J Phys Med Rehabil. [Internet]. 2017;96(8):578–581. https://pubmed.ncbi.nlm.nih.gov/28085736/
- Williams R, Oldfrey B, Holloway C. AT2030 innovation insights: an AT innovator case study: Amparo [Internet] 2020. [cited 2021 Jul 25]. Available from: www.AT2030.org
- Junsaard T, Poomulna J, Chiablam C, et al. A study of mobile prosthetic services model with a proactive and integrated approach in Thailand aimed at achieving 100% accessibility for people with movement disabilities. J Dep Med Serv. 2018;43(4):65–71. https://he02.tci-thaijo.org/index.php/JDMS/article/view/247885/168378
- Marino M, Pattni S, Greenberg M, et al. Access to prosthetic devices in developing countries: pathways and challenges. Proceedings of the 5th IEEE Global Humanitarian Technology Conference, GHTC 2015. Seattle (WA): Institute of Electrical and Electronics Engineers Inc.; 2015. p. 45–51. [cited 2021 Oct 24]. Available from: https://pennstate.pure.elsevier.com/en/publications/access-to-prosthetic-devices-in-developing-countries-pathways-and
- Williams RJ, Takashima A, Ogata T, et al. A pilot study towards long-term thermal comfort research for lower-limb prosthesis wearers. Prosthet Orthot Int. 2019;43(1):47–54.
- Maclean N, Pound P. A critical review of the concept of patient motivation in the literature on physical rehabilitation. Soc Sci Med. 2000;50(4):495–506.
- Schaffalitzky E, Gallagher P, Maclachlan M, et al. Developing consensus on important factors associated with lower limb prosthetic prescription and use. Disabil Rehabil. 2012;34(24):2085–2094.
- Sansam K, O'Connor RJ, Neumann V, et al. Clinicians’ perspectives on decision making in lower limb amputee rehabilitation. J Rehabil Med. 2014;46(5):447–453.
- Kam S, Kent M, Khodaverdian A, et al. The influence of environmental and personal factors on participation of lower-limb prosthetic users in low-income countries: prosthetists’ perspectives. Disabil Rehabil Assist Technol. 2015;10(3):245–251.
- Ostler C, Ellis-Hill C, Donovan-Hall M. Expectations of rehabilitation following lower limb amputation: a qualitative study. Disabil Rehabil. 2014;36(14):1169–1175.
- Schaffalitzky E, Gallagher P, Maclachlan M, et al. Understanding the benefits of prosthetic prescription: exploring the experiences of practitioners and lower limb prosthetic users. Disabil Rehabil. 2011;33(15–16):1314–1323. https://www.tandfonline.com/action/journalInformation?journalCode=idre20
- Christensen J, Langberg H, Doherty P, et al. Ambivalence in rehabilitation: thematic analysis of the experiences of lower limb amputated veterans. Disabil Rehabil. 2018;40(21):2553–2560.
- Gallagher P, Maclachlan M. Adjustment to an artificial limb: a qualitative perspective. J Health Psychol. 2001;6(1):85–100.
- Murray CD. “Don’t you talk to your prosthetist?” communicational problems in the prescription of artificial limbs. Disabil Rehabil. 2013;35(6):513–521.
- Naidoo U, Ennion L. Barriers and facilitators to utilisation of rehabilitation services amongst persons with lower-limb amputations in a rural community in South Africa. Prosthet Orthot Int. 2019;43(1):95–103.
- Campbell DJT, Coll N, Thurston WE. Considerations for the provision of prosthetic services in post-disaster contexts: the Haiti Amputee Coalition. Disabil Soc. 2012;27(5):647–661.
- The World Bank. Kenya | Data [Internet]. 2020. [cited 2020 Aug 13]. Available from: https://data.worldbank.org/country/KE
- APDK. Who we are – Association for the Physically Disabled of Kenya – APDK [Internet]. 2020. [cited 2020 Aug 13]. Available from: https://www.apdk.org/who-we-are/
- Braun V, Clarke V. Successful qualitative research: a practical guide for beginners. London: SAGE Publications; 2013.
- Braun V, Clarke V. To saturate or not to saturate? Questioning data saturation as a useful concept for thematic analysis and sample-size rationales. Qual Res Sport Exerc Heal. 2021;13(2):201–216. 10.1080/2159676X.2019.1704846
- Braun V, Clarke V. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qual Res Psychol. 2021;18(3):328–352. https://www.tandfonline.com/action/journalInformation?journalCode=uqrp20
- Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3(2):77–101.
- Dejonckheere M, Vaughn LM. Semistructured interviewing in primary care research: a balance of relationship and rigour. Fam Med Com Heal. 2019;7:57. http://fmch.bmj.com/
- Jamshed S. Qualitative research method-interviewing and observation. J Basic Clin Pharm. 2014;5(4):87–88. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4194943/
- Ditchman N, Lee E-J, Huebner RA. Group procedures. In: Chan F, Berven N, Thomas K, editors. Counseling theories and techniques for rehabilitation and mental health professionals. 2nd ed. New York: Springer Publishing Company; 2015.
- Miller JF. Coping with chornic illness: overcoming powerlessness. 3rd ed. Philadelphia: F. A. Davis Company; 2020.
- Murphy H. The importance of “soft” skills in healthcare professions - Elsevier education [Internet]. 2020. [cited 2020 Sep 5]. Available from: https://evolve.elsevier.com/education/expertise/faculty-development/the-importance-of-soft-skills-in-healthcare-professions/.
- Njue JR, Rombo D, Ngige L. Family strengths and challenges in Kenya. Marriage Fam Rev. 2007;41(1–2):47–70. https://www.tandfonline.com/action/journalInformation?journalCode=wmfr20
- Vlachaki A, Paterson AMJ, Porter SC, et al. Design for health exploring users’ attitudes towards prosthesis aesthetics in the UK and Greece. Des Heal. 2020. [cited 2020 Jul 12], 4(1):4–23. Available from: https://www.tandfonline.com/action/journalInformation?journalCode=rfdh20
- Murray CD. Embodiment and prosthetics. In: Gallagher P, Desmond D, MacLachlan M, editors. Psychoprosthetics. London: Springer London; 2008. p. 119–129.
- Hjelle KM, Vik K. The ups and downs of social participation: experiences of wheelchair users in Norway. Disabil Rehabil. 2011;33(25–26):2479–2489.
- Global Disability Innovation Hub. AT2030 [Internet]. 2020. [cited 2022 Aug 26]. Available from: https://at2030.org/

