ABSTRACT
Although outcomes are a critical component of evidence-based practice, measuring augmentative and alternative communication (AAC) outcomes remains problematic. This is, in part, because there is no consensus on how to operationally define AAC communication outcomes. To gain greater insight into AAC communication outcomes, we used the communicative competence framework to determine which areas of AAC intervention have received the greatest attention and how these outcomes are being measured. The following data were charted from the 77 studies that met the inclusion criteria for the scoping review: study design, study participants, study communication target (e.g., language, word learning, etc.), and communication outcome measurements. Across the included studies, researchers used a variety of standardized and non-standardized measures to assess outcomes. Seventy-seven percent of the studies assessed social skills and 62% assessed linguistic skills. A limited number of studies measured operational (14%), strategic (4%), and psychosocial (18%) skills. Using the communicative competence framework enabled us to identify gaps in the research that has been conducted to date.
Augmentative and alternative communication (AAC) provides individuals who are unable to effectively use their natural speech an alternative way to engage with the people in their community and influence their environment (Beukelman & Mirenda, Citation2020). Given that communication is a dynamic interaction, successful communication relies on both the individual using an AAC system as well as their communication partner. Individuals who are prescribed AAC often receive treatment that focuses on helping them learn to effectively communicate using their AAC system. To determine whether individuals who use AAC benefit from intervention, researchers and clinicians must document AAC communication outcomes.Footnote1 Outcomes measurement is a critical component of evidence-based practice because it lets researchers and clinicians determine “what works, for whom, under what conditions” (Smith, Citation2000). Given the heterogeneity of AAC users and their communication needs, there are a wide range of communication goals that may be addressed within intervention. In order to determine what works for whom, under what conditions researchers and clinicians must use a common set of definitions. This is challenging given that the focus of AAC intervention, which is assessed on an individual basis, is influenced by the skills, goals, and needs of the individual. To date, there is no consensus on how to operationally define AAC communication outcomes. This may be due, in part, to a lack of validated data collection tools as well as the diversity of the population who uses assistive technology such as AAC (e.g., Smith, Citation2000). Therefore, within this study we used the communicative competence framework (Light, Citation1989; Light & McNaughton, Citation2014) to determine which areas of AAC intervention have received the greatest attention and how these outcomes are being measured.
Communication competencies as a framework for measuring AAC communication outcomes
In the field of augmentative and alternative communication (AAC), the outcomes that researchers choose to measure often differs across studies. This is because the different stakeholders in the field of AAC (e.g., AAC users, AAC device manufacturers, funding agencies, practicing speech-language pathologists) value different types of outcomes (Scherer, Citation2017). While a researcher may be interested in documenting a person’s ability to use their device during social settings to interact with others, a funding agency may be more interested in documenting the economic benefit of funding a device (Lenker et al., Citation2005; Smith, Citation2016). Within the field of communication, there are numerous ways in which communication outcomes may be measured including administering standardized language assessments, using surveys and questionnaires and training observers to document behaviors of interest such as turn-taking or conversational breakdowns. Identifying and/or developing a common set of definitions for describing AAC communication outcomes will enable researchers and clinicians to make comparisons across research studies and facilitate the development of measurement tools that support the evaluation of meaningful outcomes using approaches that provide useful information for all of the stakeholders, which should ultimately improve outcomes for people of all ages that need AAC to communicate.
Classification systems may offer a viable framework for enabling researchers to determine what areas of AAC intervention have received the greatest attention and how outcomes are being measured in these areas. The International Classification of Functioning, Disabilities and Health (ICF) is the leading outcome measurement for how individuals with disabilities, including people who require AAC, interact with the world (World Health Organization [WHO], Citation2001). The ICF framework addresses an individual’s functioning and disability within the context of their participation in the community and at home (WHO, Citation2001). Using communication competencies (Light, Citation1989; Light & McNaughton, Citation2014), which describes the functionality and adequacy that facilitate participation in the community and at home to characterize an individual’s outcome is in line with the ICF framework’s focus on participation in everyday life. For people who require AAC, communication competence is built upon an individual’s knowledge and skills across four domains: linguistic competence, operational competence, strategic competence, and social competence; and communication competence considers the psychosocial factors that impact effective communication (Light, Citation1989; Light & McNaughton, Citation2014).
Linguistic competence is an individual’s knowledge and understanding of the spoken and written language used in their community and home, as well as their knowledge of the linguistic code used on their AAC device (e.g., selecting the appropriate symbols to create the phrase “I like to sing”). Operational competence is the “technical operation of AAC strategies and techniques” (Light & McNaughton, Citation2014, p. 3). For people who use high-tech AAC systems, such as speech generating devices, this includes turning the system on and off, navigating between pages, and utilizing the appropriate selection technique (e.g., direct selection, scanning, eye gaze). Strategic competence is the ability to compensate for limitations of the device. For example, a person who requires AAC may need to explain their AAC system and how they use it to an unfamiliar communication partner. Social competence involves pragmatic (e.g., communicating for a variety of functions, turn taking, terminating topics, etc.) and sociorelational skills (i.e., “the interpersonal aspects of communication that form the foundation for developing effective relationships;” Light & McNaughton, Citation2014, p. 3).
The communicative competence framework acknowledges that while each of these competencies are separate, they are intertwined and impact one another. For example, an individual with high linguistic competency (e.g., creating sentences using an AAC system), but low strategic competence (e.g., the ability to clearly communicate a message when the relevant vocabulary is not found on the system) will struggle to communicate when they don’t have access to relevant vocabulary. In addition to the knowledge, judgment, and skills that communication functionality and adequacy are built upon, the communicative competence framework considers the psychosocial factors that may impact communicative competence, such as individual attitudes toward AAC, environmental support and barriers, and policy and practice support and barriers (Light & McNaughton, Citation2014). Consideration of the psychosocial impact is critical given that the attitudes and perceptions of the AAC user, as well as their family members, can act as a facilitator or barrier to an individual’s overall use of the AAC device (Baxter et al., Citation2012; Moorecroft et al., Citation2019). An appealing aspect of the communication competence framework is that it takes all of the skills necessary for effective communication on an AAC system into consideration.
Current study
In summary, although outcomes are a critical aspect of evidence-based practice, there is currently no consensus on how to operationally define AAC communication outcomes. Within this study, we used the communicative competence framework to determine a) which areas of AAC intervention have received the greatest attention and b) how outcomes are being measured in these areas. We determined that a scoping review was the ideal methodology as this process would let us evaluate the previous literature to assess outcome characteristics of other researchers' work. Scoping reviews, which are conducted in a systematic way using clearly defined methodological frameworks (Arksey & O’Malley, Citation2005; Tricco et al., Citation2018) and reporting guidelines (Tricco et al., Citation2018), are designed to provide overviews of broad topics that may involve a sizable and diverse set of literature (e.g., Arksey & O’Malley, Citation2005; Tricco et al., Citation2018). Scoping reviews are widely used in AAC research; researchers have published scoping reviews on topics ranging from the effectiveness of AAC interventions for individuals with autism (Schlosser & Koul, Citation2015) to the impact that AAC intervention has on receptive language abilities of children with developmental disabilities (Dada et al., Citation2021).
Methods
Inclusion/exclusion criteria
We included peer-reviewed research articles published between 1990 and 2021. To be included in the review the study participants needed to be using some type AAC system ranging from no-tech AAC systems like the Picture Exchange Communication System (Bondy & Frost, Citation1994) to speech-generating devices, there was a focus on face-to-face communication, and the study included a measure of communication outcomes. Studies were excluded if the participants were not using AAC or if they focused on manual sign, if the patients were in acute care or were in-patient, and if the study measured communication outcomes related to social media. We chose to exclude research studies focused on patients in acute care because our initial review revealed that the majority of these studies focused on patients in comas. We chose to exclude communication outcomes related to social media because of potential differences in how we communicate using social media as compared to how we communicate during face-to-face interactions.
Identifying and selecting studies
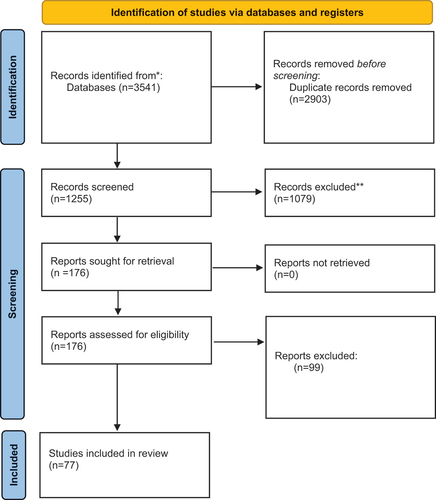
We followed the PRISMA guidelines for conducting a scoping review. A search across electronic databases was used to collect published studies. The search terms used were: Assistive Technology or AAC, and Communication, and Outcomes. Articles published between 1990 and 2021 were extracted from the following databases: Compendex, IEEE, PsycINFO, PubMed, Scopus, Web of Science. Covidence, a scoping review management software, was used to organize the studies for this review. The initial search yielded 4158 articles, which were imported into Covidence. Of the 4158 articles, 2,903 were duplicates yielding a total of 1255 unique articles to review. In the first round of screening, the title and abstract of each article was reviewed by three of the authors leaving a total of 176 articles for a full text review. During the full text review, 77 of the 176 articles were determined to meet the inclusion criteria (see ).
Data charting
We extracted the following data from the 77 studies that met the inclusion criteria: study design, study participants, communication target of the study (e.g., language, word learning, etc.), and communication outcome measurements. Measurements unrelated to communication were not extracted from articles.
Study design
The articles were differentiated based upon the study design employed by the researcher and the definitions found in Aggarwal and Rangathan’s (Citation2019a, Citation2019b) study design series were used to guide this coding. Articles were initially classified as qualitative or analytical (i.e., quantitative). Analytical studies were further classified as observational or interventional based on the presence of a treatment from the researcher.
Participant characteristics
The following demographic information was collected from each study: participant(s) age, sex, and diagnosis. For studies that used single-subject research designs if there were fewer than four participants, the research assistants listed each participant’s age. Researchers calculated the mean age when it was not specifically reported (and there were more than three participants). If specific participant age information was not provided, the information that the study provided was noted. When coding for participant diagnosis, all present diagnostic information was listed for the participants (including whether no official diagnosis was provided), participant information regarding delays/impairments were listed.
Study target
For the purpose of this review, study target was defined as the focus of the study (i.e., the facet of communication impacted by the AAC intervention that the researchers sought to evaluate). When multiple communication targets were included in the same study all targets were listed.
Communication outcomes measures
Researchers coded all of the measures that were used to assess communication outcomes. After the initial coding, outcome measures were further classified by measurement type: a) standardized assessments, b) surveys, questionnaires & structured observations, and c) non-standardized measures (i.e., trained observation or language sample analysis). Next, each measurement was classified to determine which aspect of communicative competence the outcome measure was used to assess: linguistic, social, operational, strategic, and psychosocial. When multiple outcome measurements were used within the same study, all measures were coded.
Communication competence
Interrater reliability
Sixty-five percent of the articles were screened by the first and fourth author during the initial screening (i.e., title and abstract review). There was an agreement of 87%. Disagreements were resolved with a third reviewer and during this phase the exclusionary criteria was refined to include patients in acute care or in-patient (e.g., patients with comas), which accounted for the majority of disagreements. Two undergraduate research assistants were trained on coding the articles for the full text screening and data charting. The reliability for the data charting of all variables was 96%, which was calculated based on a random 20% sample of articles. All disagreements were discussed until consensus was achieved.
Data analysis plan
First, we broadly summarize the studies included in this scoping review including the types of study designs used, ages and populations studied, and communication targets. Next, we described how AAC communication outcomes are being measured across research studies by calculating the number of studies that used a) standardized assessments, b) surveys, questionnaires, and structured observations, and c) non-standardized assessments. Finally, we classified the communication outcomes according to the communicative competence framework (Light, Citation1989; Light & McNaughton, Citation2014).
Results
Ninety-four percent of the studies (n = 72) used an analytical study design and 6% (n = 5) used a qualitative study design. Sixty-seven percent of the studies (n = 52) assessed communication outcomes in children (i.e., participants 18 years of age and under), 24% (n = 19) assessed communication outcomes in adults (i.e., participants over the age of 18 years), and 7% assessed outcomes in a sample that included adults and children (n = 6). Fifty-two percent of the studies (n = 40) had participants with a variety of diagnoses (or participants with multiple diagnoses), 35% of the studies (n = 19) focused solely on autistic participants, 4% (n = 3) focused on participants with cerebral palsy, 4% (n = 3) focused on participants with aphasia (n = 3), and 3% (n = 2) focused on participants with developmental delays. The remaining studies focused on participants with Down syndrome (n = 1), laryngectomies (n = 1), traumatic brain injury (n = 1), hypotonia (n = 1), Huntington’s disease (n = 1), amyotrophic lateral sclerosis (n = 1), and Rett’s syndrome (n = 1). Three studies did not report on the specific population studied.
Studies often had more than one communication target and the targets varied widely across research studies, with the largest number of studies targeting social communication, requesting, vocabulary and syntax. Fifty-five percent of the studies (n = 42) targeted social-communication skills, with 8% of these studies (n = 10) specifically targeted requesting, 17% of the studies (n = 13) targeted vocabulary and 14% (n = 11) targeted syntax. Other study targets included, among other things, literacy (n = 3), natural language production (n = 4), and communication modality (n = 4). See Appendix A for a detailed table of each study target.
Research Question 1: Which areas of AAC intervention have received the greatest attention (using the communicative competence framework as a structure for analysis)?
When we classified communication outcomes according to the communicative competence framework (Light, Citation1989; Light & McNaughton, Citation2014) we found that 75% (n = 60) assessed social skills, 62% of the studies (n = 48) assessed linguistic skills, 18% (n = 14) assessed psychosocial skills, 14% (n = 8) assessed operational skills, and 4% (n = 3) assessed strategic skills. Forty-nine percent (n = 38) of the studies measured one communicative competency domain, 32% (n = 25) measured two domains, 17% (n = 13) measured three domains, and 1% (n = 1) measured four domains.
Research Question 2: How are outcomes measured in those areas?
A wide variety of measures were used to assess communication outcomes across the studies. Forty-one percent of the studies (n = 32) used standardized assessments, 46% (n = 36) used surveys, questionnaires, and structured observations, and 94% used non-standardized assessments. Most standardized assessments were used in one or two studies with the exception of the Mullen Scales of Early Learning (Mullen, Citation1995) and Peabody Picture Vocabulary Test (Dunn et al., Citation1997) which were each used in 5% of the studies (ns = 5). The MacArthur Bates Communicative Developmental Inventory (Fenson, Citation2007; Fenson et al., Citation1993) and Vineland Adaptive Behavior Scales (Sparrow et al., Citation2005) were each used in 3% of the studies (ns = 3). A similar pattern was observed for surveys, questionnaires, and structured observations with only the Communication Matrix (n = 4; Rowland, Citation2011), Early Social Communication Scale (n = 3;Mundy et al., Citation2003), and Quebec User Evaluation of Satisfaction with Assistive Technology − 2nd edition (n = 3; Demers et al., Citation2002) being used in more than two studies. The two most widely used outcome measures were trained observation (i.e., training research assistants to reliably document communication outcomes of interest such as requesting, functional responses, number of communication acts, time of device use, initiations, efficiency, and communication repair) which was used in 63% of the research studies, and language sample analysis, which was used in 25% of the research studies. See for a detailed description of each of the assessments used.
Table 1. Communication outcome assessments used across research studies.
Owing to the large variability in the types of outcomes assessed across research studies, it was not possible to summarize how each type of outcome was assessed. Therefore, we focused on the most frequently assessed outcomes. In the social competency domain, researchers most frequently assessed requesting (n = 16), turn-taking (n = 13), initiations (n = 5), and joint attention (n = 4). All of the research studies assessing requesting used observation (Alzrayer, Citation2020; Alzrayer et al., Citation2021; Bock et al., Citation2005; Boesch et al., Citation2013; Flores et al., Citation2012; Ganz et al., Citation2009; Gevarter, Horan, et al., Citation2020; Gevarter et al., Citation2021; Ivy et al., Citation2020; Kasari et al., Citation2014; Lancioni et al., Citation2009; Lerna et al., Citation2014; Olive et al., Citation2008; Ricci et al., Citation2017; Snodgrass et al., Citation2013; Son et al., Citation2006). Language sampling and observation were used to assess turn-taking; five studies used observation (Bayldon et al., Citation2021; Chapin et al., Citation2022; Therrien & Light, Citation2016; Thunberg et al., Citation2007; Timpe et al., Citation2021), and eight studies used language sample analysis (Borgestig et al., Citation2021; Hux et al., Citation2010; Light et al., Citation2021; Lund & Light, Citation2006; Mathisen et al., Citation2009; Meinzen-Derr et al., Citation2017, Citation2019, Citation2021). With regard to initiations, four studies used observation (Bayldon et al., Citation2021; Conklin & Mayer, Citation2011; Lerna et al., Citation2014; McMillan & Renzaglia, Citation2014) and one study used language sample analysis (Hux et al., Citation2010). Two of the four studies assessed joint attention using the Early Social Communication Scale (Almirall et al., Citation2016; Hampton et al., Citation2020), one using the Clinical Assessment of Language Comprehension (Romski et al., Citation2008), and one using observation (Lerna et al., Citation2014).
In the linguistic domain, researchers tended to focus on general language skills (n = 14), semantics, and syntax. Eleven of the 14 studies that assessed general language skills used standardized assessments, such as the Mullen, Preschool Language Scale, and Clinical Evaluation of Language Fundamentals (Barker et al., Citation2013; Boesch et al., Citation2013; Hampton et al., Citation2020; King et al., Citation2020; Lerna et al., Citation2014; Lund & Light, Citation2006; Mathisen et al., Citation2009; Meinzen-Derr et al., Citation2021; Parsons et al., Citation2020; Romski et al., Citation2008; Rose et al., Citation2020). The other three studies used the Communication Matrix (Borgestig et al., Citation2021), a semi-structured interview (Hagan & Thompson, Citation2014), and the Focus on Communication Outcomes Under Six (Thomas-Stonell et al., Citation2016). The most widely assessed area of syntax was mean length of utterance. All six studies that assessed mean length of utterance used language sample analysis (Hayes & Traughber, Citation2021; Kasari et al., Citation2014; Light et al., Citation2021; Mathisen et al., Citation2009; Meinzen-Derr et al., Citation2017, Citation2019, Citation2021). Kasari et al. (Citation2014) used language sample analysis to assess the number of unique word combinations and Mathisen et al. (Citation2009) used language sample analysis to assess production of one-word utterances. Johnson et al. (Citation2008) used observation to assess sentence production and Mongeau and Lussier-Desrochers (Citation2017) used observation to assess production and comprehension of word combinations and sentences.
With regard to semantics, eight studies used observation to assess the number of target words identified (Caron et al., Citation2020; Trembath et al., Citation2009), number of functional vocabulary words (Gevarter, Horan, et al., Citation2020), number of social/action words (Gevarter, Groll, et al., Citation2020), correct/incorrect use of pronouns (Olive et al., Citation2008), words per minute (Babb et al., Citation2021; Wandin et al., Citation2021), intelligible words/word approximations (Ganz et al., Citation2008), symbol production (Johnson et al., Citation2008), and generalization of symbols to novel stimuli (Snodgrass et al., Citation2013). Ten studies used language sample analysis to assess expressive vocabulary (Ganz & Simpson, Citation2004), the number of different words (Almirall et al., Citation2016; Barker et al., Citation2013; Kasari et al., Citation2014; Meinzen-Derr et al., Citation2017, Citation2019, Citation2021), the total number of words (Meinzen-Derr et al., Citation2017, Citation2019; Sevcik et al., Citation2004), type-token ratio (Mathisen et al., Citation2009), and intelligible words (Ganz & Simpson, Citation2004; Mathisen et al., Citation2009). One study used the Diary of Communicative Development to assess vocabulary (Sevcik et al., Citation2004), and two studies used standardized assessments, such as the Peabody Picture Vocabulary Test to assess vocabulary (Lund & Light, Citation2006; Olive et al., Citation2008). Finally, three of the six studies assessing communication effectiveness used observation (Thunberg et al., Citation2007, Citation2009, Citation2011). Childes et al. (Citation2017) used the Communicative Effectiveness Survey, Ferm et al. (Citation2010) used the Effectiveness Framework of Functional Communication and Johnson et al. (Citation2008) used the Communicative Effectiveness Index.
Discussion
In this scoping review, we used the communicative competence framework to gain insight into which areas of AAC intervention have received the greatest attention and how outcomes are being measured in these areas. When outcomes were categorized according to the communicative competence framework over half of the research studies assessed participants’ linguistic skills and social skills. However, only a limited number of studies assessed participants operational (n = 8), strategic competence (n = 3) or psychosocial factors (n = 14). This gap in research would not have been apparent if we had not used the communicative competence framework for considering outcomes measurements. As noted within the communicative competence framework, in order to effectively communicate using an AAC system, individuals must not only understand the linguistic system of their culture and AAC device as well as the social aspects of communication, they must also be able to effectively operate the system and compensate for limitations of an AAC system. In addition, it is critical to understand the psychosocial impact that the device has on the AAC user and their quality of life.
Assessing operational and strategic competency, as well as the psychosocial impact that an AAC device has, is especially important since these factors often appear to be barriers for AAC use. For example, (Moorecroft et al. Citation2019 systematic review of barriers and facilitators to the provision and use of low-tech and unaided AAC systems for people with complex communication needs and their families found the most prominent barriers included the attitudes of professionals, family members and the AAC user. This is consistent with Baxter et al. (Citation2012) systematic review of the barriers and facilitators to the use of high-tech AAC devices, which revealed that family attitudes and perceptions served as a barrier or facilitator of AAC use. These findings highlight the need for researchers to consider all aspects of communication competence, since AAC outcomes need to consider not only the ability of an individual to effectively communicate using a system but also their ongoing use and satisfaction with the system in place. If an individual abandons their system, they will no longer have a system that will enable them to communicate and, ultimately, participate in their community.
The two most widely used outcome measures were trained observation (used in 63% of the research studies) and language sample analysis (used in 25% of the research studies). The widespread use of language sample analysis and trained observation to assess a variety of communication outcomes is consistent with recent discussions around the paucity of standardized measures available to assess communication outcomes in AAC users (e.g., Brady et al., Citation2013; Broomfield et al., Citation2019; Enderby, Citation2014; Light & Mcnaughton, Citation2015). The large number of studies that relied on trained observation protocols developed by researchers demonstrates the innovative approach that researchers have taken to enable them to document the communicative outcomes of interest in a systematic way. While useful, a drawback to this approach is that the operational definitions used across trained observations may differ making comparisons across research studies challenging. Another drawback to this approach is moving these measures into clinical practice. Once research determines that the process was beneficial to learn about communication outcomes, that needs to be translated into clinical practice. The wide use of language sample analysis aligns with recent publications highlighting the clinical utility of language sample analysis for assessing language outcomes in individuals who use AAC for years (e.g., Kovacs & Hill, Citation2015; Mooney et al., Citation2021; Van Tatenhove, Citation2014). However, researchers continue to differ in how language sampling is conducted due to variable configurations across speech-generating devices. As noted by Mooney et al. (Citation2021) “vocabulary configurations on a speech-generating device may or may not have the option to insert bound morphemes, making it challenging to determine how to consider one’s use of, or lack of, bound morphemes” (p. 49). A common set of assessment tools would facilitate consistency in terms of what aspects of communication are being measured as well as how they are measured, enabling comparison across research studies. However, the heterogeneity of individuals who use AAC, which ranges from nonspeaking autistic children who are in the process of developing language to adults with ALS who are losing the ability to communicate verbally, makes developing a common set of tools especially challenging.
Although none of the standardized measures used across research studies were specific to AAC users, 11% (n = 9) of the research studies used surveys and questionnaires specifically developed for AAC users. The Communication Matrix, which was used in four studies, is a “communication skills assessment” designed for individuals who use any type of communication behavior including alternative forms. The matrix focuses on two major aspects of communication – why an individual is communicating and how they are communicating (Rowland, Citation2011). Unlike the Communication Matrix, the Psychosocial Impact of Assistive Devices Scale, which was used in one study, and the QUEST-2, which was used in three studies, assesses the impact of the device on an individual’s life and the patient’s satisfaction with the device. Finally, the Augmentative Communication Employment Training and Supports Survey was used in one study to assess employment outcomes.
Taken together, these findings indicate that researchers are relying on non-standardized measures to assess a wide variety of language skills including pragmatics, semantics, and syntax communication outcomes in people who use AAC. Using the communicative competence framework revealed patterns that were not apparent when we approached communication outcomes from the viewpoint of research question 1 (i.e., how outcomes are being assessed).
Limitations
While the information obtained from this scoping review provides important insight into how AAC outcomes are being measured across research studies, there are limitations to this study. The first being in how we chose to categorize AAC outcome measures. It is possible that using a different categorization method for research question 1 may have enabled the study team to gain greater insight from the data obtained. Future research should work to tie together the classification systems such as communicative competence with the International Classification of Functioning, Disabilities and Health (ICF), which addresses an individual’s functioning and disability within the context of their participation in the community and at home (WHO, Citation2001). Using a combination of these systems to examine AAC communication outcomes would enable researchers to capture how communication targets such as employment outcomes related to participation in the community and at home. Another limitation is the broad view of this study. While this view was beneficial to lay the foundation for the need for better clarification and definition of AAC outcome measures, a focus within one diagnostic population may have yielded insight into the benefits and drawbacks of particular measures for that population. This study also did not review each of the measures used to determine if they consider various aspects of the communicative competence framework. Finally, though we extracted data from 77 studies, we may have missed some relevant papers as a result of our search criteria and inclusion/exclusion criteria. We may have identified additional insights if we had searched additional databases (e.g., Google Scholar), or included gray literature (e.g., peer reviewed abstracts, conference proceedings, magazine articles). Broadening the databases and the inclusion criteria may have increased the breadth of outcome measures addressing AAC communication in contemporary research studies.
Conclusion
In conclusion, the findings from this scoping review highlight the wide number of studies assessing linguistic and social outcomes in people who use AAC. However, the use of communicative competence framework revealed significant gaps in research. Given that operational and strategic competence as well psychosocial factors impact AAC use, we believe that it is critical for researchers to begin to assess all measures of communicative competence in order to provide stakeholders with a comprehensive understanding of the impact of AAC on individuals’ communication.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Notes
1 Given the complex nature of communication interactions, we chose to focus this scoping review on the measurement of communication outcomes and development of the AAC user’s communication competency rather than the communication partner.
References
- Aggarwal, R., & Ranganathan, P. (2019a). Study designs: Part 2–Descriptive studies. Perspectives in Clinical Research, 10(1), 34. https://doi.org/10.4103/picr.PICR_154_18
- Aggarwal, R., & Ranganathan, P. (2019b). Study designs: Part 4–Interventional studies. Perspectives in Clinical Research, 10(3), 137. https://doi.org/10.4103/picr.PICR_91_19
- *Almirall, D., DiStefano, C., Chang, Y. C., Shire, S., Kaiser, A., Lu, X., & Kasari, C. (2016). Longitudinal effects of adaptive interventions with a speech-generating device in minimally verbal children with ASD. Journal of Clinical Child & Adolescent Psychology, 45(4), 442–456. https://doi.org/10.1080/15374416.2016.1138407
- *Alzrayer, N. M. (2020). Transitioning from a low-to high-tech Augmentative and alternative communication (AAC) system: Effects on augmented and vocal requesting. Augmentative and Alternative Communication, 36(3), 155–165. https://doi.org/10.1080/07434618.2020.1813196
- *Alzrayer, N. M., Aldabas, R., Alhossein, A., & Alharthi, H. (2021). Naturalistic teaching approach to develop spontaneous vocalizations and augmented communication in children with autism spectrum disorder. Augmentative and Alternative Communication, 37(1), 14–24. https://doi.org/10.1080/07434618.2021.1881825
- Arksey, H., & O’Malley, L. (2005). Scoping studies: Towards a methodological framework. International Journal of Social Research Methodology, 8(1), 19–32. https://doi.org/10.1080/1364557032000119616
- *Babb, S., Gormley, J., McNaughton, D., & Light, J. (2019). Enhancing independent participation within vocational activities for an adolescent with ASD using AAC video visual scene displays. Journal of Special Education Technology, 34(2), 120–132. https://doi.org/10.1177/0162643418795842.
- *Babb, S., Jung, S., Ousley, C., McNaughton, D., & Light, J. (2021). Personalized AAC intervention to increase participation and communication for a young adult with Down syndrome. Topics in Language Disorders, 41(3), 232. https://doi.org/10.1097/TLD.0000000000000240
- *Babb, S., McNaughton, D., Light, J., Caron, J., Wydner, K., & Jung, S. (2020). Using AAC video visual scene displays to increase participation and communication within a volunteer activity for adolescents with complex communication needs. Augmentative and Alternative Communication, 36(1), 31–42. https://doi.org/10.1080/07434618.2020.1737966.
- Baker, A., Bean, A., Cargill, L. P., & Lyle, S. (2022). Within arm’s reach: The role of proximity in speech generating device use of ambulatory children with autism. International journal of speech-language pathology, 24(1), 88–96.
- *Barker, R. M., Akaba, S., Brady, N. C., & Thiemann-Bourque, K. (2013). Support for AAC use in preschool, and growth in language skills, for young children with developmental disabilities. Augmentative and Alternative Communication, 29(4), 334–346. https://doi.org/10.3109/07434618.2013.848933.
- Baxter, S., Enderby, P., Evans, P., & Judge, S. (2012). Barriers and facilitators to the use of high‐technology augmentative and alternative communication devices: A systematic review and qualitative synthesis. International Journal of Language & Communication Disorders, 47(2), 115–129. https://doi.org/10.1111/j.1460-6984.2011.00090.x
- *Bayldon, H., Clendon, S., & Doell, E. (2021). Shared storybook intervention for children with complex physical, cognitive and sensory needs who use partner-assisted scanning. International Journal of Disability, Development and Education, 70(5), 1–18. https://doi.org/10.1080/1034912X.2021.1913719
- Beukelman, D. R., & Mirenda, P. (2020). Augmentative and alternative communication: Supporting children and adults with complex communication needs. Paul H. Brookes Publishing.
- *Bock, S. J., Stoner, J. B., Beck, A. R., Hanley, L., & Prochnow, J. (2005). Increasing functional communication in non-speaking preschool children: Comparison of PECS and VOCA. Education and Training in Developmental Disabilities, 264–278.
- *Boesch, M. C., Wendt, O., Subramanian, A., & Hsu, N. (2013). Comparative efficacy of the Picture exchange communication system (PECS) versus a speech-generating device: Effects on social-communicative skills and speech development. Augmentative and Alternative Communication, 29(3), 197–209. https://doi.org/10.3109/07434618.2013.818059.
- *Borgestig, M., Al Khatib, I., Masayko, S., & Hemmingsson, H. (2021). The impact of eye-gaze controlled computer on communication and Functional independence in children and young people with complex needs–A multicenter intervention study. Developmental Neurorehabilitation, 24(8), 511–524. https://doi.org/10.1080/17518423.2021.1903603.
- Brady, N. C., Thiemann-Bourque, K., Fleming, K., & Matthews, K. (2013). Predicting language outcomes for children learning augmentative and alternative communication: Child and environmental factors. Journal of Speech Language and Hearing Research, 56(5), 1595–1612. https://doi.org/10.1044/1092-4388(2013/12-0102)
- *Brock, K., Koul, R., Corwin, M., & Schlosser, R. (2017). A comparison of visual scene and grid displays for people with chronic aphasia: A pilot study to improve communication using AAC. Aphasiology, 31(11), 1282–1306. https://doi.org/10.1080/02687038.2016.1274874.
- Broomfield, K., Harrop, D., Judge, S., Jones, G., & Sage, K. (2019). Appraising the quality of tools used to record patient-reported outcomes in users of augmentative and alternative communication (AAC): A systematic review. Quality of Life Research, 28(10), 2669–2683. https://doi.org/10.1007/s11136-019-02228-3
- *Bryen, D. N., Cohen, K. J., & Carey, A. (2004). Augmentative communication Employment Training and Supports (ACETS): Some Employment-related outcomes. Journal of Rehabilitation, 70(1). 10–18.
- *Caron, J., Light, J., & McNaughton, D. (2020). Effects of an AAC app with transition to literacy features on single-word reading of individuals with complex communication needs. Research and Practice for Persons with Severe Disabilities, 45(2), 115–131. https://doi.org/10.1177/1540796920911152.
- *Chan, J., Falk, T. H., Teachman, G., Morin McKee, J., & Chau, T. (2010). Evaluation of a non-invasive vocal cord vibration switch as an alternative access pathway for an individual with hypotonic cerebral palsy–a case study. Disability and Rehabilitation: Assistive Technology, 5(1), 69–78. https://doi.org/10.3109/17483100903278107.
- *Chapin, S. E., McNaughton, D., Light, J., McCoy, A., Caron, J., & Lee, D. L. (2022). The effects of AAC video visual scene display technology on the communicative turns of preschoolers with autism spectrum disorder. Assistive Technology, 34(5), 577–587. https://doi.org/10.1080/10400435.2021.1893235.
- *Childes, J. M., Palmer, A. D., Fried-Oken, M., & Graville, D. J. (2017). The use of technology for phone and face-to-face communication after total laryngectomy. American Journal of Speech-Language Pathology, 26(1), 99–112. https://doi.org/10.1044/2016_AJSLP-14-0106.
- *Clarke, M., Newton, C., Cherguit, J., Donlan, C., & Wright, J. A. (2011). Short‐term outcomes of communication aid provision. Journal of Assistive Technologies, 5(4), 169–180. https://doi.org/10.1108/17549451111190597
- *Conklin, C. G., & Mayer, G. R. (2011). Effects of implementing the Picture Exchange Communication System (PECS) with adults with developmental disabilities and severe communication deficits. Remedial and Special Education, 32(2), 155–166. https://doi.org/10.1177/0741932510361268.
- Dada, S., Flores, C., Bastable, K., & Schlosser, R. W. (2021). The effects of augmentative and alternative communication interventions on the receptive language skills of children with developmental disabilities: A scoping review. International Journal of Speech-Language Pathology, 23(3), 247–257. https://doi.org/10.1080/17549507.2020.1797165
- Demers, L., Monette, M., Lapierre, Y., Arnold, D. L., & Wolfson, C. (2002). Reliability, validity, and applicability of the Quebec user Evaluation of satisfaction with assistive Technology (QUEST 2.0) for adults with multiple sclerosis. Disability and Rehabilitation, 24(1–3), 21–30. https://doi.org/10.1080/09638280110066352
- *Desai, T., Chow, K., Mumford, L., Hotze, F., & Chau, T. (2014). Implementing an iPad-based alternative communication device for a student with cerebral palsy and autism in the classroom via an access technology delivery protocol. Computers & Education, 79, 148–158. https://doi.org/10.1016/j.compedu.2014.07.009
- Diehl, S. K., & Wallace, S. E. (2018). A modified multimodal communication treatment for individuals with traumatic brain injury. Augmentative and Alternative Communication, 34(4), 323–334.
- Dunn, L. M., Dunn, L. M., & Dunn, D. M. (1997). Peabody picture vocabulary test-IIIA. American Guidance Services.
- Enderby, P. (2014). Introducing the therapy outcome measure for AAC services in the context of a review of other measures. Disability and Rehabilitation: Assistive Technology, 9(1), 33–40. Scopus. https://doi.org/10.3109/17483107.2013.823576.
- *Falk, T. H., Chan, J., Duez, P., Teachman, G., & Chau, T. (2010). Augmentative communication based on realtime vocal cord vibration detection. IEEE Transactions on Neural Systems and Rehabilitation Engineering, 18(2), 159–163. https://doi.org/10.1109/TNSRE.2009.2039593.
- Fenson, L. (2007). MacArthur-Bates communicative development inventories. Paul H. Brookes Publishing Company.
- Fenson, L., Dale, P., Reznick, J. S., Thal, D., Bates, E., Hartung, J. P., Pethick S, & Reilly J. (1993). MacArthur communicative development inventories. Singular.
- *Ferm, U., Sahlin, A., Sundin, L., & Hartelius, L. (2010). Using talking mats to support communication in persons with Huntington’s disease. International Journal of Language & Communication Disorders, 45(5), 523–536. https://doi.org/10.3109/13682820903222809
- *Flores, M., Musgrove, K., Renner, S., Hinton, V., Strozier, S., Franklin, S., & Hil, D. (2012). A comparison of communication using the apple iPad and a picture-based system. Augmentative and Alternative Communication, 28(2), 74–84. https://doi.org/10.3109/07434618.2011.644579.
- Frost, L. A., & Bondy, A. S. (1994). PECS training manual. Newark: Pyramid Educational Consultants.
- *Ganz, J. B., Parker, R., & Benson, J. (2009). Impact of the picture exchange communication system: Effects on communication and collateral effects on maladaptive behaviors. Augmentative and Alternative Communication, 25(4), 250–261. https://doi.org/10.3109/07434610903381111.
- *Ganz, J. B., & Simpson, R. L. (2004). Effects on communicative requesting and speech development of the picture exchange communication system in children with characteristics of autism. Journal of Autism and Developmental Disorders, 34(4), 395–409. https://doi.org/10.1023/B:JADD.0000037416.59095.d7
- *Ganz, J. B., Simpson, R. L., & Corbin-Newsome, J. (2008). The impact of the Picture exchange communication system on requesting and speech development in preschoolers with autism spectrum disorders and similar characteristics. Research in Autism Spectrum Disorders, 2(1), 157–169. https://doi.org/10.1016/j.rasd.2007.04.005.
- *Gevarter, C., Groll, M., & Stone, E. (2020). Dynamic assessment of augmentative and alternative communication application grid formats and communicative targets for children with autism spectrum disorder. Augmentative and Alternative Communication, 36(4), 226–237. https://doi.org/10.1080/07434618.2020.1845236
- *Gevarter, C., Groll, M., Stone, E., & Medina Najar, A. (2021). A parent-implemented embedded AAC intervention for teaching navigational requests and other communicative functions to children with autism spectrum disorder. Augmentative and Alternative Communication, 37(3), 180–193. https://doi.org/10.1080/07434618.2021.1946846.
- *Gevarter, C., Horan, K., & Sigafoos, J. (2020). Teaching preschoolers with autism to use different speech-generating device display formats during play: Intervention and secondary factors. Language, Speech, and Hearing Services in Schools, 51(3), 821–838. https://doi.org/10.1044/2020_LSHSS-19-00092.
- *Griffith, J., Dietz, A., & Weissling, K. (2014). Supporting narrative retells for people with aphasia using augmentative and alternative communication: Photographs or line drawings? Text or no text? American Journal of Speech-Language Pathology, 23(2), S213–S224. https://doi.org/10.1044/2014_AJSLP-13-0089.
- *Hagan, L., & Thompson, H. (2014). It’s good to talk: Developing the communication skills of an adult with an intellectual disability through augmentative and alternative communication. British Journal of Learning Disabilities, 42(1), 66–73. https://doi.org/10.1111/bld.12041.
- *Hamm, B., & Mirenda, P. (2006). Post-school quality of life for individuals with developmental disabilities who use AAC. Augmentative and Alternative Communication, 22(2), 134–147. https://doi.org/10.1080/07434610500395493.
- *Hampton, L. H., Kaiser, A. P., & Fuller, E. A. (2020). Multi-component communication intervention for children with autism: A randomized controlled trial. Autism, 24(8), 2104–2116. https://doi.org/10.1177/1362361320934558
- Hayes, L. E., & Traughber, M. C. (2021). Improving facilitation of student communication through observational feedback within a partner instruction model. Language, Speech, and Hearing Services in Schools, 52(2), 542–553. https://doi.org/10.1044/2020_LSHSS-20-00049.
- *Hux, K., Buechter, M., Wallace, S., & Weissling, K. (2010). Using visual scene displays to create a shared communication space for a person with aphasia. Aphasiology, 24(5), 643–660. https://doi.org/10.1080/02687030902869299.
- *Icht, M., Levine-Sternberg, Y., & Mama, Y. (2020). Visual and auditory verbal long-term memory in individuals who rely on augmentative and alternative communication. Augmentative and Alternative Communication (Baltimore, Md: 1985), 36(4), 238–248. https://doi.org/10.1080/07434618.2020.1852443
- *Ivy, S., Robbins, A., & Kerr, M. G. (2020). Adapted picture exchange communication system using tangible symbols for young learners with significant multiple disabilities. Augmentative and Alternative Communication, 36(3), 166–178. https://doi.org/10.1080/07434618.2020.1826051.
- *Johnson, R. K., Hough, M. S., King, K. A., Vos, P., & Jeffs, T. (2008). Functional communication in individuals with chronic severe aphasia using augmentative communication. Augmentative and Alternative Communication, 24(4), 269–280. https://doi.org/10.1080/07434610802463957.
- *Kasari, C., Kaiser, A., Goods, K., Nietfeld, J., Mathy, P., Landa, R., Murphy, S., & Almirall, D. (2014). Communication interventions for minimally verbal children with autism: A sequential multiple assignment randomized trial. Journal of the American Academy of Child & Adolescent Psychiatry, 53(6), 635–646. https://doi.org/10.1016/j.jaac.2014.01.019
- *Keskinen, T., Heimonen, T., Turunen, M., Rajaniemi, J. P., & Kauppinen, S. (2012). SymbolChat: A flexible picture-based communication platform for users with intellectual disabilities. Interacting with Computers, 24(5), 374–386. https://doi.org/10.1016/j.intcom.2012.06.003.
- *King, M., Romski, M., & Sevcik, R. A. (2020). Growing up with AAC in the digital age: A longitudinal profile of communication across contexts from toddler to teen. Augmentative and Alternative Communication, 36(2), 128–141. https://doi.org/10.1080/07434618.2020.1782988.
- Kovacs, T., & Hill, K. (2015). A tutorial on reliability testing in AAC language sample transcription and analysis. Augmentative and Alternative Communication, 31(2), 148–158. https://doi.org/10.3109/07434618.2015.1036118
- *Lancioni, G. E., O’Reilly, M. F., Singh, N. N., Sigafoos, J., Didden, R., Oliva, D., Campodonico, F., de Pace, C., Chiapparino, C., & Groeneweg, J. (2009). Persons with multiple disabilities accessing stimulation and requesting social contact via microswitch and VOCA devices: New research evaluation and social validation. Research in Developmental Disabilities, 30(5), 1084–1094. https://doi.org/10.1016/j.ridd.2009.03.004
- Lenker, J. A., Scherer, M. J., Fuhrer, M. J., Jutai, J. W., & DeRuyter, F. (2005). Psychometric and administrative properties of measures used in assistive technology device outcomes research. Assistive Technology, 17(1), 7–22. https://doi.org/10.1080/10400435.2005.10132092
- *Lerna, A., Esposito, D., Conson, M., & Massagli, A. (2014). Long‐term effects of PECS on social–communicative skills of children with autism spectrum disorders: A follow‐up study. International Journal of Language & Communication Disorders, 49(4), 478–485. https://doi.org/10.1111/1460-6984.12079
- Light, J. (1989). Toward a definition of communicative competence for individuals using augmentative and alternative communication systems. Augmentative and Alternative Communication, 5(2), 137–144. https://doi.org/10.1080/07434618912331275126
- Light, J., Barwise, A., Gardner, A. M., & Flynn, M. (2021). Personalized early AAC intervention to build language and literacy skills: A case study of a 3-year-old with complex communication needs. Topics in Language Disorders, 41(3), 209. https://doi.org/10.1097/TLD.0000000000000254
- Light, J., & McNaughton, D. (2014). Communicative competence for individuals who require augmentative and alternative communication: A new definition for a new era of communication? Augmentative and Alternative Communication, 30(1), 1–18. https://doi.org/10.3109/07434618.2014.885080
- Light, J., & Mcnaughton, D. (2015). Designing aac research and intervention to improve outcomes for individuals with complex communication needs. Augmentative and Alternative Communication, 31(2), 85–96. https://doi.org/10.3109/07434618.2015.1036458
- *Lund, S. K., & Light, J. (2006). Long-term outcomes for individuals who use augmentative and alternative communication: Part I–What is a “good” outcome? Augmentative and Alternative Communication, 22(4), 284–299. https://doi.org/10.1080/07434610600718693.
- *Mathisen, B., Arthur-Kelly, M., Kidd, J., & Nissen, C. (2009). Using MINSPEAK: A case study of a preschool child with complex communication needs. Disability and Rehabilitation: Assistive Technology, 4(5), 376–383. https://doi.org/10.1080/17483100902807112.
- *McMillan, J. M., & Renzaglia, A. (2014). Supporting speech generating device use in the classroom. Part two: Student communication outcomes. Journal of Special Education Technology, 29(3), 49–61. https://doi.org/10.1177/016264341402900304.
- *Meinzen-Derr, J., Sheldon, R., Altaye, M., Lane, L., Mays, L., & Wiley, S. (2021). A Technology-assisted language intervention for children who are deaf or hard of hearing: A randomized clinical trial. Pediatrics, 147(2). https://doi.org/10.1542/peds.2020-025734.
- Meinzen-Derr, J., Sheldon, R. M., Henry, S., Grether, S. M., Smith, L. E., Mays, L., & Wiley, S. (2019). Enhancing language in children who are deaf/hard-of-hearing using augmentative and alternative communication technology strategies. International journal of pediatric otorhinolaryngology, 125, 23–31.
- *Meinzen-Derr, J., Wiley, S., McAuley, R., Smith, L., & Grether, S. (2017). Technology-assisted language intervention for children who are deaf or hard-of-hearing; a pilot study of augmentative and alternative communication for enhancing language development. Disability and Rehabilitation: Assistive Technology, 12(8), 808–815. https://doi.org/10.1080/17483107.2016.1269210.
- *Mohan, V., Kunnath, S. K., Philip, V. S., Mohan, L. S., & Thampi, N. (2019). Capitalizing on technology for developing communication skills in autism spectrum disorder: A single case study. Disability and Rehabilitation: Assistive Technology, 14(1), 75–81. https://doi.org/10.1080/17483107.2017.1413144.
- *Mongeau, C., & Lussier-Desrochers, D. (2017, July). Mobile technologies used as communication support system for people with intellectual disabilities: An exploratory study. In International Conference on Applied Human Factors and Ergonomics (pp. 254–263). Springer, Cham.
- Mooney, A., Bean, A., & Sonntag, A. M. (2021). Language sample collection and analysis in people who use augmentative and alternative communication: Overcoming obstacles. American Journal of Speech-Language Pathology, 30(1), 47–62. https://doi.org/10.1044/2020_AJSLP-19-00055
- *Mooney, A., Bedrick, S., Noethe, G., Spaulding, S., & Fried-Oken, M. (2018). Mobile technology to support lexical retrieval during activity retell in primary progressive aphasia. Aphasiology, 32(6), 666–692. https://doi.org/10.1080/02687038.2018.1447640.
- Moorcroft, A., Scarinci, N., & Meyer, C. (2019). A systematic review of the barriers and facilitators to the provision and use of low-tech and unaided AAC systems for people with complex communication needs and their families. Disability and rehabilitation. Assistive technology, 14(7), 710–731.
- Mullen, E. M. (1995). Mullen scales of early learning. AGS.
- Mundy, P., Delgado, C., Block, J., Venezia, M., Hogan, A., & Seibert, J. (2003). Early social communication scales (ESCS). FL: Coral Gables.
- *Olive, M. L., Lang, R. B., & Davis, T. N. (2008). An analysis of the effects of functional communication and a voice output communication aid for a child with autism spectrum disorder. Research in Autism Spectrum Disorders, 2(2), 223–236. https://doi.org/10.1016/j.rasd.2007.06.002.
- *Parsons, D., Vaz, S., Lee, H., Robinson, C., & Cordier, R. (2020). A twelve-month follow-up of an information communication technology delivered intervention for children with autism spectrum disorder living in regional Australia. Research in Developmental Disabilities, 106, 103743. https://doi.org/10.1016/j.ridd.2020.103743
- *Quinn, E. D., Kaiser, A. P., & Ledford, J. R. (2020). Teaching preschoolers with Down syndrome using augmentative and alternative communication modeling during small group dialogic reading. American Journal of Speech-Language Pathology, 29(1), 80–100. https://doi.org/10.1044/2019_AJSLP-19-0017.
- *Ricci, C., Miglino, O., Alberti, G., Perilli, V., & Lancioni, G. E. (2017). Speech generating technology to support request responses of persons with intellectual and multiple disabilities. International Journal of Developmental Disabilities, 63(4), 238–245. https://doi.org/10.1080/20473869.2017.1288888.
- *Romski, M. A., Haarbauer-Krupa, J., Cheslock, M., Sevcik, R. A., & Adamson, L. B. (2008). Language and communication changes in a child with holoprosencephaly: A case report. Journal of Medical Speech-Language Pathology, 16(2), 77–83.
- *Rose, V., Paynter, J., Vivanti, G., Keen, D., & Trembath, D. (2020). Predictors of expressive language change for children with autism spectrum disorder receiving AAC-infused comprehensive intervention. Journal of Autism and Developmental Disorders, 50(1), 278–291. https://doi.org/10.1007/s10803-019-04251-2
- Rowland, C. (2011). Using the communication matrix to assess expressive skills in early communicators. Communication Disorders Quarterly, 32(3), 190–201. https://doi.org/10.1177/1525740110394651
- Scherer, M. J. (2017). Technology adoption, acceptance, satisfaction and benefit: Integrating various assistive technology outcomes. Disability and Rehabilitation Assistive Technology, 12(1), 1–2. https://doi.org/10.1080/17483107.2016.1253939
- Schlosser, R. W., & Koul, R. K. (2015). Speech output technologies in interventions for individuals with autism spectrum disorders: A scoping review. Augmentative and Alternative Communication, 31(4), 285–309. https://doi.org/10.3109/07434618.2015.1063689
- *Seale, J. M., Bisantz, A. M., & Higginbotham, J. (2020). Interaction symmetry: Assessing augmented speaker and oral speaker performances across four tasks. Augmentative and Alternative Communication, 36(2), 82–94. https://doi.org/10.1080/07434618.2020.1782987.
- *Senner, J. E., Post, K. A., Baud, M. R., Patterson, B., Bolin, B., Lopez, J., & Williams, E. (2019). Effects of parent instruction in partner-augmented input on parent and child speech generating device use. Technology and Disability, 31(1–2), 27–38. https://doi.org/10.3233/TAD-190228
- *Sevcik, R. A., Romski, M. A., & Adamson, L. B. (2004). Research directions in augmentative and alternative communication for preschool children. Disability and Rehabilitation, 26(21–22), 1323–1329. https://doi.org/10.1080/09638280412331280352.
- Smith, R. O. (2000). Measuring assistive technology outcomes in education. Diagnostique, 25(4), 273–290. https://doi.org/10.1177/073724770002500403
- Smith, R. O. (2016). The emergence and emergency of assistive technology outcomes research methodology. Assistive Technology Outcomes & Benefits, 10(1), 19–37.
- *Snodgrass, M. R., Stoner, J. B., & Angell, M. E. (2013). Teaching conceptually referenced core vocabulary for initial augmentative and alternative communication. Augmentative and Alternative Communication, 29(4), 322–333. https://doi.org/10.3109/07434618.2013.848932.
- *Son, S. H., Sigafoos, J., O’Reilly, M., & Lancioni, G. E. (2006). Comparing two types of augmentative and alternative communication systems for children with autism. Pediatric Rehabilitation, 9(4), 389–395. https://doi.org/10.1080/13638490500519984.
- *Soto, G., Clarke, M. T., Nelson, K., Starowicz, R., & Savaldi-Harussi, G. (2020). Recast type, repair, and acquisition in AAC mediated interaction. Journal of Child Language, 47(1), 250–264. https://doi.org/10.1017/S0305000919000436.
- Sparrow, S. S., Cicchetti, D., & Balla, D. A. (2005). Vineland adaptive behavior scales (2nd edition manual ed.) NCS Pearson Inc.
- *Sreekumar, S., Sangeetha, G. S., & Mathew, B. S. (2019). Advancement to higher communicative functions with transition to iPad app–a case report. Disability and Rehabilitation: Assistive Technology, 15(4), 480–483. https://doi.org/10.1080/17483107.2019.1629116
- *Tan, P., & Alant, E. (2018). Using peer-mediated instruction to support communication involving a student with autism during mathematics activities: A case study. Assistive Technology, 30(1), 9–15. https://doi.org/10.1080/10400435.2016.1223209.
- *Therrien, M. C., & Light, J. (2016). Using the iPad to facilitate interaction between preschool children who use AAC and their peers. Augmentative and Alternative Communication, 32(3), 163–174. https://doi.org/10.1080/07434618.2016.1205133.
- *Thomas-Stonell, N., Robertson, B., Oddson, B., & Rosenbaum, P. (2016). Communicative participation changes in pre-school children receiving augmentative and alternative communication intervention. International Journal of Speech-Language Pathology, 18(1), 32–40. https://doi.org/10.3109/17549507.2015.1060530.
- *Thunberg, G., Ahlsén, E., & Dahlgren Sandberg, A. (2007). Children with autistic spectrum disorders and speech‐generating devices: Communication in different activities at home. Clinical Linguistics & Phonetics, 21(6), 457–479. https://doi.org/10.1080/02699200701314963.
- *Thunberg, G., Ahlsen, E., Sandberg, A. D., & Clarke, M. (2011). Autism, communication and use of a speech-generating device in different environments – A case study. Journal of Assistive Technologies, 5(4), 181–198. https://doi.org/10.1108/17549451111190605
- *Thunberg, G., Sandberg, A. D., & Ahlsén, E. (2009). Speech-generating devices used at home by children with autism spectrum disorders: A preliminary assessment. Focus on Autism and Other Developmental Disabilities, 24(2), 104–114. https://doi.org/10.1177/1088357608329228.
- Timpe, E. M., Kent-Walsh, J., Binger, C., Hahs-Vaughn, D., Harrington, N., & Schwartz, J. B. (2021). Using the ImPAACT Program with preschoolers with Down syndrome: A hybrid service-delivery model. Augmentative and Alternative Communication, 37(2), 113–128.
- *Trembath, D., Balandin, S., Togher, L., & Stancliffe, R. J. (2009). Peer-mediated teaching and augmentative and alternative communication for preschool-aged children with autism. Journal of Intellectual and Developmental Disability, 34(2), 173–186. https://doi.org/10.1080/13668250902845210.
- Tricco, A. C., Lillie, E., Zarin, W., O’Brien, K. K., Colquhoun, H., Levac, D., Moher, D., Peters, M. D. J., Horsley, T., Weeks, L., Hempel, S., Akl, E. A., Chang, C., McGowan, J., Stewart, L., Hartling, L., Aldcroft, A., Wilson, M. G., Garritty, C., … Straus, S. E. (2018). PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Annals of Internal Medicine, 169(7), 467–473. https://doi.org/10.7326/M18-0850
- Van Tatenhove, G. (2014). Issues in language sample collection and analysis with children using AAC. Perspectives on Augmentative and Alternative Communication, 23(2), 65–74. https://doi.org/10.1044/aac23.2.65
- Walters, C., Sevcik, R. A., & Romski, M. (2021). Spoken vocabulary outcomes of toddlers with developmental delay after parent-implemented augmented language intervention. American Journal of Speech-Language Pathology, 30(3), 1023–1037.
- *Wandin, H., Lindberg, P., & Sonnander, K. (2021). Aided language modelling, responsive communication and eye-gaze technology as communication intervention for adults with Rett syndrome: Three experimental single case studies. Disability and Rehabilitation: Assistive Technology, 1–15. https://doi.org/10.1080/17483107.2021.1967469
- World Health Organization. (2001). IFC: International Classification of functioning, disability and Health.
- Yoder, P. J., & Lieberman, R. G. (2010). Brief report: Randomized test of the efficacy of Picture Exchange Communication System on highly generalized picture exchanges in children with ASD. Journal of Autism & Developmental Disorders, 40, 629–632.