Abstract
Phenomenon: Supervisors and trainees can learn skills related to evidence-based medicine from each other in the workplace by collaborating and interacting, in this way benefiting from each other’s strengths. This study explores supervisors’ perceptions of how they currently learn evidence-based medicine by engaging in learning conversations with their trainee. Approach: Semi-structured, video-stimulated elicitation interviews were held with twenty-two Dutch and Belgian supervisors in general practice. Supervisors were shown fragments of their video-recorded learning conversations, allowing them to reflect. Recorded interviews were analyzed using a grounded theory-based approach.Findings: Supervisors did not immediately perceive workplace learning conversations as an opportunity to learn evidence-based medicine from their trainee. They mostly saw these conversations as a learning opportunity for trainees and a chance to maintain the quality of care within their practice. Nevertheless, during the interviews, supervisors did acknowledge that learning conversations help them to gain up-to-date knowledge and search skills or more awareness of their own knowledge or gaps in their knowledge. Not identified as a learning outcome was how to apply evidence-based medicine within a clinical practice by combining evidence with clinical expertise and the patient’s preferences. Insights: Supervisors acknowledge that they learn elements of the three aspects of evidence-based medicine by having learning conversations with their trainee, but they currently see this as secondary to the trainee’s learning process. Emphasizing opportunities for bidirectional learning could improve learning of evidence-based medicine during workplace learning conversations.
Introduction
Combining the three aspects of evidence-based medicine (EBM) – i.e., the best available evidence, the patient’s wishes and preferences, and the physician’s clinical expertise – is important in making medical decisions for individual patient care. Nevertheless, incorporating these three aspects into practice is not without its difficulties.Citation 1 , Citation 2 Teaching EBM involves five steps: ask a clinical question, acquire relevant evidence, appraise this evidence for its relevance, apply the relevant evidence in practice, and evaluate the result.Citation 3 To integrate EBM into local clinical practice and combine all three aspects of EBM, the focus must be on the latter two steps, which should be learned in the clinical workplace.Citation 2 , Citation 4 Researchers have studied how best to incorporate EBM learning and teaching into daily clinical practice, but attempts so far have been without great success.Citation 5–12 It is crucial to obtain a better view of current workplace-based practices so that support for EBM learning can be better tailored to the workplace.
Most postgraduate, general practice specialty training occurs in the workplace. Trainees work closely with their clinical supervisor, who serves as a role model, for example for how to apply and evaluate EBM.Citation 13 Supervisors themselves experience barriers to practicing EBM, however, generally because they lack literature search skills.Citation 14 , Citation 15 They might benefit from the knowledge of their trainees, who may have more up-to-date skills when it comes to searching for and appraising evidence. Supervisors, on the other hand, may have more insight into the patient’s perspective and can help trainees gain clinical expertise. It is useful to look for ways in which supervisors and trainees can optimize bidirectional learning and can benefit from each other’s strengths.
A suitable moment for bidirectional learning could be the “learning conversations” that are a standard part of general practice specialty training in the Netherlands and Flanders, Belgium. Learning conversations are regularly scheduled meetings during daily clinical practice in which supervisor and trainee discuss medical questions, selected topics or professional performance, in this way integrating feedback and debriefing at dedicated times.Citation 16 , Citation 17 The format provides opportunities for non-formal, deliberative workplace-based learning.Citation 18
Learning conversations are currently viewed primarily as a learning opportunity for trainees in which they are meant to show self-directed learning and to set learning goals. A previous study (part of the larger research project to which this study belongs) showed that trainees indeed see these conversations as an opportunity for EBM learning in which they might discuss the supervisor’s experience and the specific local context in light of what the evidence recommends.Citation 19 However, it is unclear whether supervisors see these conversations as an opportunity to learn EBM from their trainee as well. This study explores how supervisors currently perceive their own EBM learning in learning conversations with their trainee.
Method
Design
We performed a qualitative, grounded theory-based interview study because our research aimed to explain a process involving social interactions or experiences.Citation 20 To evoke reflection during the interviews and elicit the tacit knowledge that informs professional practice, we made use of the video-stimulated interviewing (VSI) technique.Citation 21–23
Setting
This study was conducted in general practices in the Netherlands and Flanders, Belgium, which have comparable general practitioner (GP) specialty training. Supervisor and trainee worked independently in the GP practice, but the supervisor was always available for questions and back-up. Both trainees and supervisors underwent formal training in EBM, but regular workplace-based learning conversations were also customary in both countries and part of daily clinical routine. These conversations were aimed at the trainee’s learning process but had an informal character in which all topics could be discussed.
Participants and sampling
Within the broader research project to which this study belongs,Citation 19 , Citation 24 we selected 22 supervisors and their trainees for maximum variation between September 2016 and April 2017 by giving promotional talks and distributing information leaflets during formal educational sessions at the GP training institutes in Antwerp and Ghent (Belgium) and Utrecht (the Netherlands).Citation 25 Since recruitment was more difficult in the Netherlands, convenience sampling was used there. Participants completed a short questionnaire about their baseline characteristics (), with maximum variation being maintained in both the Dutch and Flemish group.
Table 1. Characteristics of participants.
Data collection
Data collection took place between November 2016 and August 2017. All pairs of supervisors and trainees were asked to video three random learning conversations over a period of at least four months to take the developing relationship between supervisor and trainee into account. We only asked participants to record conversations addressing a medical topic or question and gave them no further instructions.
After recording the conversations, LW selected two video fragments per supervisor, from different recordings. A fragment was considered suitable when it showed the trainee asking the supervisor a medical question that was then followed by a discussion; this made the fragment appropriate as a starting point for reflection on all three aspects of EBM. The semi-structured video-stimulated elicitation interviews, conducted in the workplace, were held within two weeks of the final recording. Supervisors were asked to elaborate on their goals during the learning conversations and the role that all three aspects of EBM played during these conversations. Subsequently, participants were shown the selected video fragments, allowing them to elaborate on their own EBM learning during the conversation. During the data collection process, the interviewers read transcripts of previous interviews to allow earlier analytic insights and concepts to shape the elicitation interview when necessary, for example to make questions more to-the-point and understandable for the interviewees.
Data analysis and credibility
All interviews were audio-recorded, transcribed verbatim, and analyzed using NVivo 12 software. Analyzing and coding were performed by six researchers with different backgrounds (LW, KVR, MLB, EdG, HS and DB) to enhance trustworthiness and reflexivity during coding discussions. The first interviews were coded separately and discussed afterwards, leading to a provisional code tree that identified the main categories. Thereafter, four of the six researchers (LW, KVR, HS and DB) analyzed and coded the interviews in rotating pairs, discussing the codes until they reached consensus. The final interviews were coded individually but were always discussed extensively during research team meetings. After conducting and analyzing all 22 interviews, we felt that no new themes could be constructed and that our research questions could be answered. Using axial coding involving extensive discussions and reflections with the whole team to ensure triangulation, we constructed an overview of aspects of learning conversations as described by the supervisors and their own learning activities and outcomes regarding EBM.Citation 26
Results
Twenty-two supervisors participated in the study, selected to form a heterogeneous group in terms of experience, age, and practice type ().
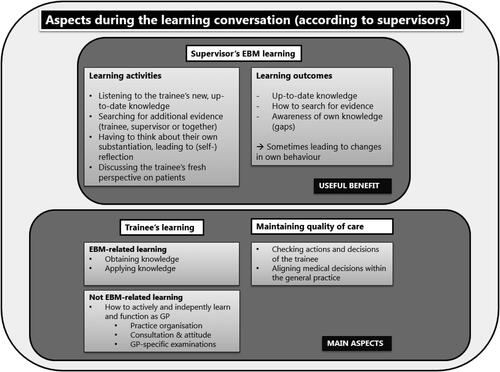
Analysis of these 22 supervisors’ interviews revealed that they perceived three different aspects playing a role during learning conversations: encouraging the trainee’s learning (both EBM and non-EBM), maintaining the quality of care within their general practice, and stimulating their own learning ().
Encouraging trainee’s EBM and non-EBM learning and maintaining the quality of care
Not surprisingly, most supervisors did prioritize their trainee’s learning process and goals during their learning conversations. Supervisors elaborated on what they saw as essential goals of this process. Some goals were EBM-related, but many were not. One important goal was that trainees should be able to learn actively and independently, take control of their learning processes and grow in their role as independently functioning GPs. Coaching trainees in how to take on such a role, for instance by discussing practical skills such as conducting GP-specific examinations and organizing and managing a practice, was seen as an important non-EBM aspects of these dedicated conversations.
And I consider that important, because it might be the most useful [information] to him when he sets up his own practice later. I do think so, because you learn the medical side of things as you go, and largely through independent study, but how to organise a practice and, for example, how to make sure that your instruments are disinfected, those are structural interventions that also have to be learned.
Supervisor 15
When addressing their trainee’s EBM learning, supervisors pointed out that knowledge-gathering is an individual task for the trainee and should not be part of the learning conversation. These supervisors tended to focus on how their expertise helped trainees to apply knowledge when assisting individual patients, for example by discussing how to share decision-making.
Because in theory they already know it all […] so that feeling, the feeling of dealing with the patient, what is the patient asking, what can you do? Do you go along with that, or not? To what extent do you want to lead the patient to something like, more like interaction. […] Not all patients would go along with what you suggest and then you’d have to look for something else. That’s how you interact with a patient to find the best solution.
Supervisor 14.
Supervisors also saw the learning conversation as an opportunity to maintain the quality of care within their practice. GP trainees worked independently, and if they did not ask for feedback or help, supervisors did not see the relevant patients. The supervisors therefore used the learning conversations to check up on their trainees’ actions and the decisions that they had made during consultations. They also used these conversations to align medical decisions.
Whether the trainee, so to speak, has overlooked anything. Just go over everything again, even an ordinary cold or so is discussed briefly. […] But then all patients get examined and that’s actually like doing a check for us, so to speak.
Supervisor 20.
Supervisor’s EBM learning
First and foremost, the supervisors saw learning conversations as an opportunity for their trainee to learn. However, when reflecting on the video-recorded conversations that they were shown during the interview, they did see their own learning as a benefit, with several learning activities leading to EBM learning for themselves.
Yes, I do pick up things, of course. Like when a trainee says ‘I’ve looked that up and this is how it is’. Sometimes a trainee tells me ‘You told me it’s this way, but I believe it’s something else’, and then I quickly adapt my policy.
Supervisor 12.
Supervisors associated most learning activities and outcomes with their gaining up-to-date knowledge on evidence, and not with the whole spectrum of EBM; they did not mention balancing the clinician’s expertise, the patient’s perspective, and the best available evidence as an aspect that they had learned from their trainee.
Up-to-date knowledge and search skills
The learning conversation allowed these supervisors to obtain new, up-to-date knowledge or to search for evidence in different ways. They sometimes described trainees as bringing new, up-to-date evidence or knowledge to the table of which they themselves were not yet aware. This might include evidence-based knowledge, but also forgotten facts about pathophysiology, or more general items from lectures at the training institute. Furthermore, some supervisor-trainee pairs first read a guideline or article individually and then discussed it in-depth during the learning conversations. The conversation could also be a starting point for seeking additional evidence in response to questions that came up during their discussion. Some pairs agreed to look for substantiating evidence individually and discuss it again during the next meeting.
So, when I think, well I don’t know but we’ll get back to it. So, then I think oh, let’s see what I can find out about it or see how a colleague does it. So, putting something I don’t know and she doesn’t know on the agenda is like challenging [me] to look up [the answer].
Supervisor 4.
During the conversation, some supervisors asked their trainee to search for additional evidence or to report the answer during the next conversation if a question or topic remained unclear. Supervisors often saw their trainees as more skilled at searching for evidence online and trainees would show their supervisor how to access all information quickly and easily during the learning conversation. The supervisors in our study not only gained up-to-date knowledge in this way but also learned how to obtain evidence.
For the knee, for example, if I wrote down that I’d do a Thessaly test and not a McMurray then he’d get on to the computer straight away and do a search to see what the specificity and sensitivity of it is. So that’s really useful for me because I don’t look at it like that, so in that sense it’s very nice working with XXX (trainee) because he looks at what it’s worth [the value] far more [than I do].
Supervisor 3.
Awareness of own knowledge
Supervisors found that the trainee’s questions during the learning conversations stimulated them to think about substantiating their behavior while reflecting on how they handle issues themselves during daily practice. Having to explain something to the trainee revealed their knowledge gaps and stimulated them to look for new evidence or to check their assertions against the literature.
As a learning outcome, this process of reflection sometimes led to the supervisors becoming aware of their own, often implicit and tacit, knowledge. In our interviews, the supervisors acknowledged that much of their behavior was based on internalized, less explicit routines drawn from their experience. Answering the trainees questions forced these supervisors to go back to their own reasoning and substantiations, presumably leading to more explicit EBM behavior themselves. Furthermore, having to reflect on their behavior so explicitly sometimes made them reconsider and change their behavior.
One of the nice things about working with people in training is always that [I] can take a critical look at what I’m doing, at the factual basis of what I do. That can also be an incentive to say, I’m going to look at a standard again, for example, or check what’s in the guideline nowadays.
Supervisor 16.
Gaining a fresh perspective on patients
The interviewees did not mention balancing the clinician’s expertise, the patient’s perspective and the best available evidence as an aspect that they had learned from their trainee. However, when discussing cases from daily practice, some supervisors noticed that trainees have a “fresh perspective” on patients whom they may have been treating for many years. Having a long history with patients is one of the strengths of general practice, but it can also obscure how the patient’s situation may have changed over time. By discussing such cases with their trainees, supervisors sometimes acquired a different perspective on the patient.
Yes, in terms of content, certainly but also, in a manner of speaking, like an outsider seeing a client for the first time with their [fresh] eyes while my [old] eyes have been wearing out for 20–25 years. […] And I’ve seen in learning conversations about a patient where I’ve said, my goodness, I’ve never seen that in her before. I’m seeing a completely different woman. I thought that was very nice. Supervisor 9.
Discussion
Most supervisors in our study did not immediately perceive learning conversations as an opportunity to learn EBM from their trainee. First and foremost, they saw these conversations as an opportunity for the trainee to learn and to monitor their trainee’s behavior to maintain the quality of care within their practice. Their own learning was seen as a valuable benefit, with several learning activities potentially leading to EBM learning. Learning outcomes included gaining up-to-date knowledge, search skills, and more awareness of their own knowledge or gaps in their knowledge.
There has been surprisingly little research on how medical supervisors themselves benefit from teaching and supervising in the workplace. Medical education research on supervisor learning focuses mainly on how they can acquire and update teaching skills, for instance through formal faculty development or informal experiential learning in the workplace,Citation 27 , Citation 28 but not on how they might gain new medical knowledge and skills. One recent report by Sun et al.Citation 29 did show that clinician-teachers can benefit their own learning by teaching medical topics, especially those that they are less likely to encounter in daily practice, such as crisis resource management. Parallels can be drawn with our results. Even though practicing EBM is an everyday activity, experienced GPs may not always practice it consciously. Experienced GPs rely more on tacit knowledge derived from mindlines – internalized, collectively reinforced tacit guidelines – making them less aware of their own reasoning and substantiations on a day-to-day basis.Citation 30 Having to discuss EBM during learning conversations deliberatively may help them to combine such implicit and more explicit reasoning.Citation 31
Our results show that supervisors make their trainees’ responsible for obtaining new EBM knowledge, stating that this is the trainee’s individual learning process or that trainees are more skilled in searching for evidence. However, this is also precisely what they say that they can learn from their trainees. This somewhat contradictory way of thinking may be an outcome of the culture and context of workplace-based teaching within general practice. Recent research by Elmberger et al.Citation 32 suggests that culture and context influence the way supervisors teach. They argue that “attention needs to shift from individual teachers to developing the systems in which they work” (p. 125). Current discourse within formal “teach-the-teacher” training focuses on making the trainee responsible for their learning so that they self-regulate their learning.Citation 33 , Citation 34 Given this, it is understandable that many supervisors regard obtaining EBM knowledge as something the trainee should do individually. However, our results suggest that supervisors may miss out on valuable learning opportunities for themselves if they persist in thinking that trainees should gain up-to-date knowledge on their own. Training institutes should use formal education to encourage supervisors to change the culture and context; EBM learning is not exclusively a self-regulating learning activity for trainees. We recommend designing EBM learning as an activity in which bidirectional learning can benefit both trainee and supervisor. By stimulating explicit discussions in the workplace, supervisor and trainee can better align their expectations regarding learning outcomes.Citation 35 , Citation 36
Limitations
Our interview questions asked supervisors about their own learning outcomes. The interviewees’ answers focused predominantly on gaining and updating evidence, and less on applying this new knowledge judiciously in practice while considering the clinician’s expertise and the patient’s perspective. It is interesting that application in practice was not mentioned at all, since using evidence in clinical decision-making, especially in general practice, cannot be separated from the situation, context, and individual patient.Citation 4 , Citation 37 It may be that, even though we tried to focus on applying all three aspects of EBM during the interview, the wording of this question still led supervisors to associate it with searching for and appraising evidence. Future research might explore other methods of elucidating how and what supervisors can also learn from their trainees about applying their newly obtained, up-to-date knowledge in practice, especially when that knowledge deviates from what supervisors are accustomed to doing based on their clinical experience, for example.
A further limitation of our study was that it was unfeasible for us to collect data in an iterative manner, although that is recommended for studies taking a grounded theory-based approach. We have argued that iterative, and thus more theoretical, sampling is frequently challenging to implement.Citation 38 Nevertheless, follow-up studies, starting with our model, would be recommended.
This study took a different and unique approach on EBM learning in the workplace by looking at what GP supervisors think they can learn from their trainees about EBM in the learning conversations format. There has been very little research addressing this question. Using the method of video-stimulated elicitation interviews produced richer results. Supervisors struggled to elaborate on their own learning opportunities, since they generally did not focus on this aspect of “being a supervisor.” Our method made it easier for them to reflect on specific and concrete video-recorded events, leading to richer and more informative data. The results of this study can help tailor EBM learning and teaching to the GP workplace by using learning conversations efficiently and by linking them explicitly to existing routines in daily practice.
Conclusion
GP supervisors do not immediately perceive workplace-based learning conversations as an opportunity for them to learn EBM from their trainee. They see these regular meetings as learning opportunity for the trainee and as a procedure for maintaining the quality of care within their GP practice. However, supervisors do acknowledge that learning conversations allow them to gain new, up-to-date knowledge and search skills themselves, as well as more awareness of their own knowledge and any gaps in that knowledge. Not identified as a learning outcome was how to apply EBM in a clinical practice by combining evidence with clinical expertise and the patient’s preferences. Emphasizing opportunities for bidirectional learning during learning conversations could improve workplace-based EBM learning.
Declaration of interest statement
The authors report no conflict of interest. The authors alone are responsible for the content and writing of this article.
Funding details
This study was supported by the Netherlands Organization for Health Research and Development (ZonMw) under Grant number 839130005. This funding body was not involved in the design of the study, in data collection, analysis and interpretation, or in writing the manuscript.
Ethical approval
This study was part of a larger research project on EBM learning in the GP workplace. Approval for the research project as a whole, in which pairs of supervisors and trainees took part, was granted by the ethical board of the NVMO (Dutch Society of Medical Education) under case number 706. Belgian ethical approval was issued by the Ethics Committee of the University Hospital of Ghent.
Acknowledgments
The authors would like to thank David Blom (DB) and Hilde Suijker (HS), both final-year medical students at the time of this study, for their help during data analysis. We also wish to thank all the GPs and trainees who participated in the study.
Data availability statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
- Sackett DL , Rosenberg WMC , Gray JM , Haynes RB , Richardson WS . Evidence based medicine: what it is and what it isn't. BMJ . 1996;312(7023):71–72. doi:https://doi.org/10.1136/bmj.312.7023.71.
- Greenhalgh T , Howick J , Maskrey N , Evidence Based Medicine Renaissance Group . Evidence based medicine: a movement in crisis? BMJ . 2014;348:g3725. doi:https://doi.org/10.1136/bmj.g3725.
- Dawes M , Summerskill W , Glasziou P , et al. Sicily statement on evidence-based practice. BMC Med Educ . 2005;5(1):1 doi:https://doi.org/10.1186/1472-6920-5-1.
- Galbraith K , Ward A , Heneghan C. A real-world approach to evidence-based medicine in general practice: a competency framework derived from a systematic review and Delphi process. BMC Med Educ . 2017;17(1):78. doi:https://doi.org/10.1186/s12909-017-0916-1.
- Albarqouni L , Hoffmann T , Glasziou P. Evidence-based practice educational intervention studies: a systematic review of what is taught and how it is measured. BMC Med Educ . 2018;18(1):177–178. doi:https://doi.org/10.1186/s12909-018-1284-1.
- Ilic D , Maloney S. Methods of teaching medical trainees evidence-based medicine: a systematic review. Med Educ . 2014;48(2):124–135. doi:https://doi.org/10.1111/medu.12288.
- Larsen CM , Terkelsen AS , Carlsen A-MF , Kristensen HK . Methods for teaching evidence-based practice: a scoping review. BMC Med Educ . 2019;19(1):259. doi:10.1136/bmjebm-2018-111024.73
- Flores-Mateo G , Argimon JM. Evidence based practice in postgraduate healthcare education: a systematic review. BMC Health Serv Res . 2007;7(1):119. doi:https://doi.org/10.1186/1472-6963-7-119.
- Hecht L , Buhse S , Meyer G. Effectiveness of training in evidence-based medicine skills for healthcare professionals: a systematic review. BMC Med Educ . 2016;16:103. doi:https://doi.org/10.1186/s12909-016-0616-2.
- Kortekaas MF , Bartelink MEL , Zuithoff N. a , et al. Does integrated training in evidencebased medicine (EBM) in the general practice (GP) specialty training improve EBM behaviour in daily clinical practice? A cluster randomised controlled trial. BMJ Open . 2016;6(9):e010537. doi:https://doi.org/10.1136/bmjopen2015010537.
- Young T , Rohwer A , Volmink J , Clarke M. What are the effects of teaching evidence-based health care (EBHC)? Overview of systematic reviews. PLoS One . 2014;9(1):e86706. doi:https://doi.org/10.1371/journal.pone.0086706.
- Ahmadi SF , Baradaran HR , Ahmadi E. Effectiveness of teaching evidence-based medicine to undergraduate medical students: a BEME systematic review. Med Teach . 2015;37(1):21–30. doi:https://doi.org/10.3109/0142159X.2014.971724.
- Passi V , Johnson S , Peile E , Wright S , Hafferty F , Johnson N. Doctor role modelling in medical education: BEME Guide No. 27. Med Teach . 2013;35:9. doi:https://doi.org/10.3109/0142159X.2013.806982.
- Te Pas E , van Dijk N , Bartelink MEL , Wieringa-De Waard M. Factors influencing the EBM behaviour of GP trainers: a mixed method study. Med Teach . 2013;35(3):e990–e997. doi:https://doi.org/10.3109/0142159X.2012.733044.
- Oude Rengerink K , Thangaratinam S , Barnfield G , et al. How can we teach EBM in clinical practice? An analysis of barriers to implementation of on-the-job EBM teaching and learning. Med Teach . 2011;33(3):e125–e130. doi:https://doi.org/10.3109/0142159X.2011.542520.
- Tavares W , Eppich W , Cheng A , et al. Learning conversations: an analysis of their theoretical roots and their manifestations of feedback and debriefing in medical education. Acad Med . 2020;95(7):1020–1025. doi:https://doi.org/10.1097/ACM.0000000000002932.
- Stolper CF , Van de Wiel MWJ , Hendriks RHM , et al. How do gut feelings feature in tutorial dialogues on diagnostic reasoning in GP traineeship? Adv Health Sci Educ Theory Pract . 2015;20(2):499–513. doi:https://doi.org/10.1007/s10459-014-9543-3.
- Eraut M. Non-formal learning and tacit knowledge in professional work. Br J Educ Psychol . 2000;70(1):113–136. doi:https://doi.org/10.1348/000709900158001.
- Welink LS , De Groot E , Pype P , et al . GP trainees’ perceptions on learning EBM using conversations in the workplace: a video-stimulated interview study. BMC Med Educ . 2020;20(1):139. doi:https://doi.org/10.1186/s12909-020-02051-2.
- Kennedy TJT , Lingard LA. Making sense of grounded theory in medical education. Med Educ . 2006;40(2):101–108. doi:https://doi.org/10.1111/j.1365-2929.2005.02378.x.
- van Braak M , de Groot E , Veen M , Welink L , Giroldi E . Eliciting tacit knowledge: the potential of a reflective approach to video-stimulated interviewing. Perspect Med Educ . 2018;7(6):386–393. doi:https://doi.org/10.1007/s40037-018-0487-9.
- Paskins Z , McHugh G , Hassell AB. Getting under the skin of the primary care consultation using video stimulated recall: a systematic review. BMC Med Res Methodol . 2014;14(1):101. doi:https://doi.org/10.1186/1471-2288-14-101.
- Henry SG , Fetters MD. Video elicitation interviews: a qualitative research method for investigating physician-patient interactions. Ann Fam Med . 2012;10(2):118–126. doi:10.1370/afm.1339.Department
- Welink LS , Van Roy K , Damoiseaux RAMJ , et al. Applying evidence-based medicine in general practice: a video-stimulated interview study on workplace-based observation. BMC Fam Pract . 2020;21(1):1–10. doi:https://doi.org/10.1186/s12875-019-1073-x.
- Patton M. Purposeful sampling. In: Qualitative Evaluation and Research Methods . Beverly Hills, CA: Sage. 1990:169–186.
- Watling CJ , Lingard L. Grounded theory in medical education research: AMEE Guide No. 70. Med Teach . 2012;34(10):850–861. doi:https://doi.org/10.3109/0142159X.2012.704439.
- Hartford W , Nimmon L , Stenfors T. Frontline learning of medical teaching: “you pick up as you go through work and practice”. BMC Med Educ . 2017;17(1):1–10. doi:https://doi.org/10.1186/s12909-017-1011-3.
- Steinert Y , Mann K , Centeno A , et al. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Med Teach . 2006;28(6):497–526. doi:https://doi.org/10.1080/01421590600902976.
- Sun NZ , Maniatis T , Steinert Y. Learning by teaching: benefits for frontline clinician-teachers. Med Educ . 2019;53(11):1154–1155. doi:https://doi.org/10.1111/medu.13977.
- Gabbay J , Le May A . Evidence based guidelines or collectively constructed “mindlines?” Ethnographic study of knowledge management in primary care. BMJ . 2004;329(7473):1013. doi:https://doi.org/10.1136/bmj.329.7473.1013.
- Norman G , Young M , Brooks L. Non-analytical models of clinical reasoning: the role of experience. Med Educ . 2007;41(12):1140–1145. doi:https://doi.org/10.1111/j.1365-2923.2007.02914.x.
- Elmberger A , Björck E , Liljedahl M , Nieminen J , Bolander Laksov K . Contradictions in clinical teachers’ engagement in educational development: an activity theory analysis. Adv Health Sci Educ Theory Pract . 2019;24(1):125–140. doi:https://doi.org/10.1007/s10459-018-9853-y.
- Sandars J , Cleary TJ. Self-regulation theory: applications to medical education: AMEE Guide No. 58. Med Teach . 2011;33(11):875–886. doi:https://doi.org/10.3109/0142159X.2011.595434.
- Sagasser MH , Kramer AWM , van Weel C , van der Vleuten CPM . GP supervisors' experience in supporting self-regulated learning: a balancing act. Adv Health Sci Educ Theory Pract . 2015;20(3):727–744. doi:https://doi.org/10.1007/s10459-014-9561-1.
- Jackson D , Davison I , Adams R , Edordu A , Picton A. A systematic review of supervisory relationships in general practitioner training. Med Educ . 2019;53(9):874–885. doi:https://doi.org/10.1111/medu.13897.
- Peters S , Clarebout G , Aertgeerts B , et al. Provoking a conversation around students ’ and supervisors ’ expectations regarding workplace learning. Teach Learn Med . 2019;32(3):1–12. doi:https://doi.org/10.1080/10401334.2019.1704764.
- Wieringa S , Engebretsen E , Heggen K , Greenhalgh T. Has evidence-based medicine ever been modern? A Latour-inspired understanding of a changing EBM. J Eval Clin Pract . 2017;23(5):964–970. Published online doi:https://doi.org/10.1111/jep.12752.
- Timonen V , Foley G , Conlon C. Challenges when using grounded theory: a pragmatic introduction to doing GT research. Int J Qual Methods . 2018;17(1):1–10. doi:https://doi.org/10.1177/1609406918758086.