ABSTRACT
In the past forty years, clinician-educators have become indispensable to academic medicine. Numerous clinician-educator-training programs exist within graduate medical education (GME) as clinician-educator tracks (CETs). However, there is a call for the clinician-educator pipeline to begin earlier. This work aims to identify and characterize clinician-educator track-like programs (CETLs) available in undergraduate medical education (UME). We developed an algorithm of 20 individual keyword queries to search the website of each U.S. allopathic medical school for CETLs. We performed the web search between March to April 2021 and repeated the search between July and September 2021. The search identified CETLs for 79 (51%) of the 155 U.S. allopathic medical schools. The identified CETLs commonly address the clinician-educator competency of educational theory (86%, 68/79), are formally organized as concentrations or analogous structures (52%, 41/79), and span all four years of medical school (37%, 29/79). The prevalence of CETLs varies with geography and medical school ranking. We provide an overview of the current state of CETLs as assessed from institutional websites. To create a future with a sustainable output of skilled clinician-educators, UME must continue to increase the number and quality of CETLs.
Introduction
In the past forty years, clinician-educators have become indispensable to the medical education enterprise [Citation1,Citation2]. Clinician-educators comprise the majority of academic physicians [Citation3], fulfill both educational and clinical missions of academic medical centers [Citation4], and receive recognition through distinct promotional tracks [Citation1,Citation5]. A recent consensus definition for the 21st-century clinician-educator [Citation6] highlights the multifaceted nature of the role: an individual who participates in clinical practice, applies theory to education practice, engages in scholarship, and consults on education issues. Indeed, with major national organizations such as the Carnegie Foundation calling for significant reforms to medical training [Citation7], a sustainable pipeline of clinician-educators who are education scholars – in addition to being exceptional teachers – is necessary to advance medical education [Citation8,Citation9].
However, the current paradigm of undergraduate medical education (UME) rarely teaches students the educator skills essential for the practice of future clinician-educators [Citation6,Citation10,Citation11]. Clinician-educators often must pursue master’s or doctoral programs in health professions education [Citation12,Citation13], faculty development programs [Citation14], and/or post-residency medical education fellowships [Citation15]. Over the past two decades, clinician-educator-training programs have begun appearing in residency programs as clinician-educator tracks (CETs) [Citation16,Citation17]. This emergence may be due to the recognition that residents skilled in clinician-educator competencies are needed to soon join the clinician-educator workforce. Moreover, enhanced recruitment of future clinician-educators in residency may counteract low faculty clinician-educator retention rates [Citation18], thereby bolstering the number of clinician-educators at academic medical centers [Citation16]. This is in addition to the ongoing need to develop resident teaching skills – up to one third of medical student teaching is performed by residents [Citation19] – coupled with accreditation organization requirements for resident teaching [Citation20,Citation21].
Recent literature has called for the clinician-educator pipeline to begin earlier than residency: in undergraduate medical education [Citation22,Citation23]. Cultivating educator identities in medical students may be a solution for generating sustained interest in the clinician-educator pathway during training. Exposure to and identification with educator role models fosters educator identity and produces future clinician-educators, according to the community of practice framework [Citation24,Citation25]. Furthermore, clear career pathways and early research exposure are known to positively influence the choice to become an academic physician [Citation26,Citation27].
The 2020 supplement to Academic Medicine [Citation28] highlights the recent expansion of student enrichment tracks in UME. Other works document the rise in scholarly concentration programs, including those in medical education [Citation29,Citation30]. These emerging formal structures show promise for extending the clinician-educator pipeline into earlier stages of medical training, encouraging educator identity formation in medical students as CETs do for residents. Our study will refer to these structures for medical students as clinician-educator track-like programs (CETLs).
Existing literature mainly centers on programs that train students to be better teachers [Citation10,Citation31,Citation32]. However, with increasing attention in UME to programs developing the educator skills (e.g., scholarship) and knowledge (e.g., pedagogical theory) vital to the 21st-century clinician-educator [Citation6,Citation33–35], a comprehensive study of the current state of CETLs nationwide is needed. This work aims to identify and characterize CETLs in UME at U.S. allopathic medical schools in order to understand how medical schools prepare students for careers as clinician-educators and to inform future directions for CETL development.
Materials and methods
Algorithmic search overview
Four trained medical student researchers (A.A.A., R.C.B., E.S.L., M.A.S.) performed an algorithmic web search of all 155 U.S. allopathic medical schools to identify those with existing CETLs in March-April 2021. Three researchers (R.C.B., E.S.L., M.A.S.) repeated the search in July-September 2021. Prior to the search, we obtained the list of U.S. allopathic medical schools from the Liaison Committee on Medical Education (LCME) website [Citation36]. We independently executed the search algorithm for distinct school lists and exchanged schools for the second iteration of the search. In developing the search algorithm, we adhered to established recommendations for conducting systematic web searches [Citation37]. Prior works studying UME scholarly concentration programs [Citation29,Citation38] and reviewing medical school websites [Citation39] informed our search methodology.
CETL definition and exclusion criteria
Using the clinician-educator definition of Sherbino and colleagues [Citation6] and criteria for CETs established by Friedman and colleagues [Citation16], we defined CETLs as programs that target UME learners and address three core clinician-educator competencies: direct teaching, educational scholarship, and educational theory. We categorized CETLs as full or partial depending on the number of criteria met. Full CETLs meet all 4 criteria (longitudinal, direct teaching, educational scholarship, educational theory) whereas partial meet 3 or fewer (). We established criteria to exclude specialty- and knowledge-specific programs, non-dual degree programs in education, and programs meeting specific CETL criteria that are not substantive enough to constitute a CETL ().
Table 1. Definition of a clinician-educator track-like (CETL) program in undergraduate medical education (UME).
Table 2. Exclusion criteria for clinician-educator track-like (CETL) programs.
Web search algorithm
The web search used an algorithmic approach (). We first located the website for each medical school through the Medical School Admission Requirements (MSAR) online database [Citation40] and confirmed it with a Google search. Entering the website name into the Google search bar (‘site:[website name]’) limited the search to the institutional website. We conducted a series of queries using 20 keywords, in order, until we identified a full CETL for each school. We chose keywords in consultation with an experienced research librarian (J.M.S.). For each keyword query, we clicked on all links on the first page of Google results and scanned the directly linked web pages for content that fit our CETL criteria.
Figure 1. (a) Web search algorithm. (b) Cumulative percentage of clinician-educator track-like (CETL) programs identified after each search term.
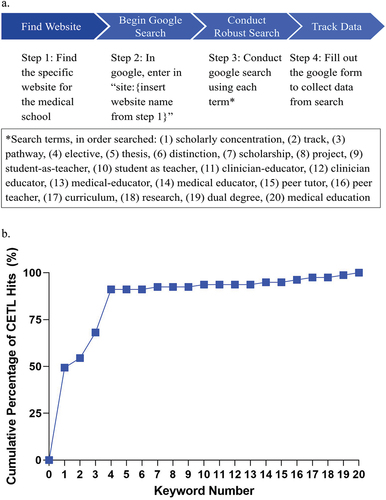
If an individual keyword query was negative (i.e., did not uncover content consistent with a CETL), we continued through the keyword list until a query was positive or until all keywords were exhausted. When a keyword query was positive, we extracted the following information in a Google form: (1) keyword resulting in CETL hit; (2) website link for CETL; (3) number of CETL criteria filled; (4) type of CETL (full/partial); (5) brief program description; (6) length and timing of program; and (7) explanation of how the program fulfills ‘direct teaching,’ ‘educational scholarship,’ and/or ‘educational theory’ criteria. We also recorded when all keyword queries were exhausted for a school without hitting a CETL program ().
Data analysis
We reviewed extracted data as a group and calculated Cohen’s kappa statistics to measure inter-rater reliability. Group discussion resolved disagreements and ensured consensus. An independent reviewer (A.W.O.) verified and compiled CETL information for each institution post-extraction. We performed descriptive data analysis in Google Sheets and identified medical school subgroups by institution characteristics (geographic region, private/public, ranking). Two-sample z-tests for independent proportions assessed for subgroup differences in CETL availability.
Results
Web search
We analyzed inter-rater reliability during the two iterations of the search to evaluate reproducibility. We observed a median percent agreement of 87% for 2 raters performing the web search algorithm for the same institutions (range across 5 rater pairs: 80–100%) and a Cohen’s kappa of 0.75 (range: 0.59–1.00). This reflects substantial agreement between raters in finding CETLs through the web search [Citation41]. More detailed reporting of inter-rater reliability can be found in Table A1 in the Appendix.
We also examined when CETLs were identified during the execution of the search algorithm. Forty-nine percent (39/79) of CETLs were identified after 1 keyword search: ‘scholarly concentration.’ Ninety-one percent (72/79) of CETLs were identified within 4 keyword searches ().
CETL identification
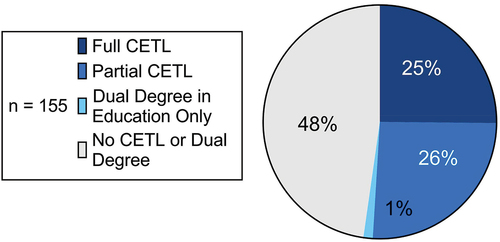
The web search identified CETLs at 79 (51%) of the 155 U.S. allopathic medical schools. Thirty-nine (25%) have full CETLs; 40 (26%) have partial CETLs, including 3 that also offer a dual degree in education; and 2 (1%) do not have CETLs but offer a dual degree in education (). Individual program summaries and links for all 79 CETLs identified in this study are in .
Table 3. Identified clinician-educator track-like (CETL) programs by institution.
CETL program components
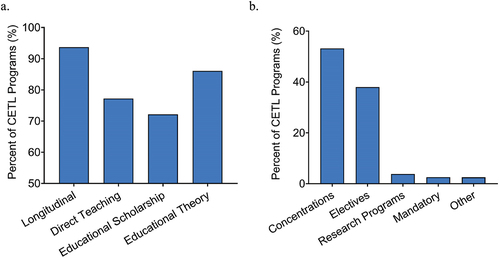
We aimed to understand how CETLs differ according to their program components (longitudinal, direct teaching, educational scholarship, educational theory). Of the 79 CETLs, the 39 full CETLs contain all 4 components. The 40 partial CETLs include 26 that have 3 CETL components. Seventeen longitudinal programs incorporate direct teaching and educational theory, 7 longitudinal programs incorporate educational scholarship and educational theory, and 2 longitudinal programs incorporate direct teaching and educational scholarship. Twelve CETLs have 2 components. Eight longitudinal programs incorporate educational scholarship, 3 non-longitudinal programs incorporate direct teaching and educational theory, and 1 longitudinal program incorporates educational theory. Two partial CETLs contain only 1 component (1 educational scholarship program and 1 educational theory program). Overall, 94% (74/79) of CETLs are longitudinal, and educational theory (86%, 68/79) is more prevalent than direct teaching (77%, 61/79) and educational scholarship (72%, 57/79) ().
CETL classification, length, and timing
We classified CETLs according to shared characteristics and naming conventions (). Most often (52%, 41/79), CETLs are designated as formal concentrations or similar structures: concentrations (20%, 16/79), pathways (10%, 8/79), tracks (10%, 8/79), distinctions (6%, 5/79), projects (5%, 4/79), or certificates (1%, 1/79). Collectively, these CETLs are academic experiences promoting in-depth learning in a topical area of focus and are usually but not always distinct from core medical school curricula.
Thirty of the 79 (38%) CETLs are designated as electives, the majority of which occur exclusively during the fourth year of medical school (70%, 21/30). Three of the 79 (4%) CETLs are research programs. Two of these occur during the summer between the first and second year of medical school. One occurs during the third year. Two of the 79 (3%) CETLs are school requirements (a 4-year Student-As-Teacher program and a month-long Teaching Practicum). The remaining 2 (3%) CETLs represent uniquely branded experiences: a Scholars program and a 4-year course not designated as an elective.
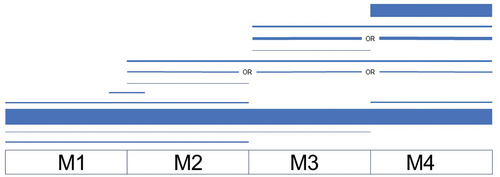
CETLs vary tremendously in length. A plurality of programs (37%, 29/79) span all 4 years of medical school. Eighteen of the 79 CETLs (23%) last 4 weeks and 15 (19%) are between 4 weeks and 1 year. A smaller number of programs are longer than 1 year but shorter than 4 years (10%, 8/79) and even fewer are shorter than 4 weeks (6%, 5/79). Timing of CETLs during medical school is also quite heterogeneous. Although a majority of CETLs start in the first year and continue through the fourth year (37%, 29/79) or occur exclusively during the fourth year (30%, 24/79), programs occur at all points during medical school ().
Figure 4. Clinician-educator track-like (CETL) program timing chart (n = 75). Line thickness represents the number of schools. Four schools are excluded from the visualization as their programs may occur at an unspecified or variable time during M1 – M4 (3) or unspecified time during ‘upper years’ (1).
CETLs by institution characteristics
We additionally analyzed whether CETL program availability is associated with institutional geographic location, public or private status, and ranking among medical schools according to U.S. News & World Report [Citation42].
Medical schools were geographically divided into Midwest (23%, 35/155), Northeast (23%, 36/155), South (37%, 57/155), West (15%, 23/155), or Territorial (3%, 4/155), according to U.S. Census Bureau definitions [Citation43]. A higher proportion of Northeast institutions have CETLs (69%, 25/36) compared to institutions in the South (37%, 21/57, p < 0.05). Other geographic regions do not significantly differ from each other in CETL availability. Public (45/93, 48%) and private (34/62, 55%) institutions offer CETLs at similar rates. With respect to third-party ranking, the top 50 medical schools for research according to U.S. News & World Report more commonly have CETL programs (65%, 33/51) than unranked schools and schools ranked 51 or above (44%, 46/104, p < 0.05).
Dual degree programs
Among the 116 schools without a full CETL, 4% (n = 5) offer a dual degree program for medical students. The dual degree programs encompass 2 general education programs and 3 health professions education programs.
Discussion
Our web search provides an exploratory look at the current state of CETLs in UME. The search algorithm was reproducible, with a median percent agreement between raters of 87% (range across rater pairs: 80%-100%), despite 3–6 months separating the 2 independent searches and program availability changing throughout the time period. Approximately half (51%, 79/155) of U.S. allopathic medical schools have identifiable structures to prepare their students for careers as clinician-educators. Prior works demonstrate that formal training in educational theory, curriculum design, scholarship, and teaching produces better educators [Citation44–46] as well as better learners [Citation47]. Medical students soon will be residents and faculty whose educator competencies will benefit trainees and patients alike [Citation47]. These constitute compelling reasons for all U.S. allopathic medical schools to implement – and continually improve – CETLs and dual degree programs in education for their medical students.
Most commonly, CETLs address the clinician-educator competency of educational theory, are formally organized as concentrations (or analogous structures), and span all four years of medical school. Nevertheless, programs exhibit significant heterogeneity in their naming, timing, and content. Friedman and colleagues [Citation16] report on heterogeneity in the timing of CETs in graduate medical education (GME), proposing that future research examine the type and amount of time required in CETs for sufficient clinician-educator skill-building and professional identity formation. We encourage similar research for CETLs in UME. Applying the community of practice framework [Citation24,Citation25], a greater number of hours devoted to a CETL or dual degree program in education may result in deeper interactions within the medical education community of practice, stronger professional identity formation, and a higher likelihood for medical students to become clinician-educators. Clinician-educators commonly describe their entry into the position as serendipitous and characterize the career pathway as ill-defined [Citation48]. This underscores the critical role that time-intensive CETLs could have in spurring early entry into the clinician-educator career pathway. Future research should explore this role by assessing the long-term impact of CETLs and dual degree programs in education on career trajectory.
With CETLs and CETs increasing in UME and GME, respectively, coordination is necessary to promote continuous development along the educator skill spectrum and reduce curricular redundancy across these two stages of training. Soriano and colleagues [Citation32] found that UME student-as-teacher programs have remarkably similar content and teaching formats to resident-as-teacher programs [Citation49]. A clear framework of educator competencies for both UME and GME may facilitate the alignment of CETLs with CETs to achieve optimal outcomes. The key roles, domains of competence, and core competencies for clinician-educators defined by Sherbino and colleagues [Citation6] may serve as a foundation for institutions seeking to design their own competency frameworks. Standardizing such frameworks would create a shared language for clinician-educator competency building and transform how future clinician-educators are developed. It may therefore behoove educational leadership at institutions with CETs and CETLs to collaborate on a consensus competency framework for use across UME and GME nationwide.
Models of successful CETLs are useful references for institutions aiming to implement their own programs. In recognition of this, our study aims to effectively summarize 79 distinct CETLs representing the diversity of offerings at U.S. allopathic medical schools. Numerous works discuss the challenges of such programs. Faculty doubts about student teaching competence may drive institutional resistance to implementation [Citation32], though students are known to be as good as faculty in certain teaching contexts [Citation50]. It is reasonable to suppose that this capability may extend to other clinician-educator domains. In their report on a scholarly concentrations program at the Vanderbilt University School of Medicine, Gotterer and colleagues [Citation51] describe additional challenges: deciding on program timing, tracking student progress, and funding program expenses, among others. Nevertheless, suggestions for actualizing such programs despite their challenges have also been published. Freret and colleagues [Citation52] describe 12 tips for implementing student-as-teacher programs, including defining program scope, promoting longitudinal trainee and faculty relationships, and collecting feedback from all stakeholders. These tips may be adapted to enhance nascent or existing CETLs. We recommend educational leaders draw from the pool of existing CETLs, anticipate challenges to implementing and maintaining their own program, and adhere to published guidance to maximize the chances of CETL success.
While CETLs are most immediately pertinent to medical students, their relevance may begin before medical school. Celebi and colleagues [Citation53] found that implementation of a CET in their residency program was associated with increased applicant interest, larger application numbers, and enhanced applicant quality. We speculate that CETLs may have a similar impact on medical school admissions, particularly for programs that are prominently featured on medical school institutional websites. The content of residency program websites is known to be important for residency applicants [Citation54], and as most medical school applicants use the Internet as an information source when applying [Citation39], the importance of website advertising likely applies to medical school recruitment as well. In our study, the prevalence of CETLs interestingly varied with institutional geography (more common in the Northern region of the U.S. than the Southeast) and ranking (greater presence at top 50 research institutions than lower-ranked/unranked institutions), but not with institutional status as public or private. Medical school applicants aspiring to become clinician-educators may benefit from awareness of these trends when curating their list of prospective schools.
Limitations
Several limitations exist for this study. First, our data do not account for CETLs and CETL components that may be in place but are not evident on institutional websites. Despite this, our CETL sample is large: 79 programs representing 51% of all U.S. allopathic medical schools. This exceeds the number of formal medical education training programs reported in similar works [Citation32]. Our data are also descriptive of various CETL characteristics and are as current as institutional websites, although some websites may be outdated. Second, our web search was not sensitive to program information (e.g., outcomes) typically reported by surveys and case reports. For this work, we desired to have a comprehensive and contemporary picture of institutional CETLs at allopathic medical schools across the U.S. Web surveys are known for low response rates [Citation55,Citation56], and CETLs are sparse in the current literature. Nevertheless, further surveying of educational leadership at medical schools and systematic literature review would add invaluable program information and, importantly, clarify the scope of individual CETLs to enable further analysis. Third, website analysis is inherently subjective, and the personalized algorithms of search engines risk the introduction of selection bias [Citation57]. We employed a comprehensive, algorithmic web search strategy to counteract this, with high inter-rater reliability scores indicating search reproducibility and low rater subjectivity. Finally, our definition for CETL was limited and did not include the many ways medical students may prepare for future clinician-educator careers, such as serving on their institution’s curriculum committee and developing courses [Citation11,Citation22]. Future research should explore these opportunities as well as programs that address clinician-educator competencies beyond the scope of our work (e.g., leadership).
Conclusion
In conclusion, we provide an overview of the current state of clinician-educator track-like programs (CETLs) in undergraduate medical education (UME) as assessed from institutional websites. Only half of U.S. allopathic medical schools appear to have formal structures to prepare their students for careers as clinician-educators. To create a future with a sustainable output of skilled clinician-educators, UME must continue to increase the number and quality of CETLs and dual degree programs in education. Future studies should explore CETL outcomes, including end-of-program learner satisfaction, demonstrated learner proficiency in clinician-educator competencies, and long-term impact on career trajectory.
Notes on contributors
Ryan C. Bahar, ScB, Medical Student, Yale School of Medicine
Aidan W. O’Shea, ScB, Medical Student, University of Rochester School of Medicine and Dentistry
Eric S. Li, BS, Medical Student, Yale School of Medicine
Madisen A. Swallow, MS, Medical Student, Yale School of Medicine
August A. Allocco, BS, Medical Student, Yale School of Medicine
Judy M. Spak, MLS, Head of Academic Research and Education, Cushing/Whitney Medical Library, Yale School of Medicine
Janet P. Hafler, EdD, Associate Dean for Educational Scholarship, Professor of Pediatrics, and Director of the Teaching and Learning Center, Yale School of Medicine.
Acknowledgments
The authors would like to acknowledge the Yale School of Medicine Teaching and Learning Center for their unwavering commitment to clinician-educator training and medical education scholarship as well as their tremendous support of this work.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Greenberg L. The evolution of the clinician-educator in the USA and Canada: personal reflections over the last 45 years. Acad Med. 2018;93(12):1764–21.
- Levinson W, Rubenstein A. Mission critical–integrating clinician-educators into academic medical centers. N Engl J Med. 1999;341(11):840–843.
- Levinson W, Branch WT Jr, Kroenke K. Clinician-educators in academic medical centers: a two-part challenge. Ann Intern Med. 1998;129(1):59–64.
- Levinson W, Rubenstein A. Integrating clinician-educators into academic medical centers: challenges and potential solutions. Acad Med. 2000;75(9):906–912.
- Fleming VM, Schindler N, Martin GJ, et al. Separate and equitable promotion tracks for clinician-educators. JAMA. 2005;294(9):1101–1104.
- Sherbino J, Frank JR, Snell L. Defining the key roles and competencies of the clinician-educator of the 21st century: a national mixed-methods study. Acad Med. 2014;89:783–789.
- Irby DM, Cooke M, O’Brien BC. Calls for reform of medical education by the Carnegie foundation for the advancement of teaching: 1910 and 2010. Acad Med. 2010 Feb;85(2):220–227.
- Collins J. Teacher or educational scholar? They aren’t the same. J Am Coll Radiol. 2004;1(2):135–139.
- Fincher RM, Simpson DE, Mennin SP, et al. Scholarship in teaching: an imperative for the 21st century. Acad Med. 2000;75(9):887–894.
- Pasquinelli LM, Greenberg LW. A review of medical school programs that train medical students as teachers (MED-SATS). Teach Learn Med. 2008;20(1):73–81.
- Peluso MJ, Hafler JP. Medical students as medical educators: opportunities for skill development in the absence of formal training programs. Yale J Biol Med. 2011;84(3):203–209.
- Tekian A. Doctoral programs in health professions education. Med Teach. 2014;36(1):73–81.
- Tekian A, Harris I. Preparing health professions education leaders worldwide: a description of masters-level programs. Med Teach. 2012;34(1):52–58.
- Leslie K, Baker L, Egan-Lee E, et al. Advancing faculty development in medical education: a systematic review. Acad Med. 2013;88:1038–1045.
- Cataldi ML, Kelly-Hedrick M, Nanavati J, et al. Post-residency medical education fellowships: a scoping review. Med Educ Online. 2021;26(1):1920084.
- Friedman K, Lester J, Young JQ. Clinician-Educator tracks for trainees in graduate medical education: a scoping review. Acad Med. 2019;94(10):1599–1609.
- Jibson MD, Hilty DM, Arlinghaus K, et al. Clinician-educator tracks for residents: three pilot programs. Acad Psychiatry. 2010;34(4):269–276.
- Corrice AM, Fox S, Bunton SA. Retention of full-time clinical MD faculty at US medical schools. AAMC Anal Brief. 2011;11(2):1–2.
- Bing-You RG, Sproul MS. Medical students’ perceptions of themselves and residents as teachers. Med Teach. 1992;14(2–3):133–138.
- Accreditation Council for Graduate Medical Education (ACGME). 2021. Common Program Requirements. [cited 2021 Dec 06]. Available from: https://www.acgme.org/What-We-Do/Accreditation/Common-Program-Requirements
- Liaison Committee on Medical Education (LCME). 2021b. Functions and structure of a medical school: standards for accreditation of medical education programs leading to the MD degree. [accessed 2021 December 06]. http://www.lcme.org/publications/#Standards.
- Blatt B, Plack M, Suzuki M, et al. Introducing medical students to careers in medical education: the student track at an annual medical education conference. Acad Med. 2013;88(8):1095–1098.
- Hassan S, Reddy P, Wolniak K. A path that needs more attention in medical school. Acad Med. 2020;95(6):821.
- Cantillon P, D’Eath M, De Grave W, et al. How do clinicians become teachers? A communities of practice perspective. Adv Health Sci Educ Theory Pract. 2016;21(5):991–1008.
- Wald HS, Anthony D, Hutchinson TA, et al. Professional identity formation in medical education for humanistic, resilient physicians: pedagogic strategies for bridging theory to practice. Acad Med. 2015;90:753–760.
- O’Sullivan PS, Niehaus B, Lockspeiser TM, et al. Becoming an academic doctor: perceptions of scholarly careers. Med Educ. 2009;43(4):335–341.
- Straus SE, Straus C, and Tzanetos K. International campaign to revitalise academic medicine. 2006. Career choice in academic medicine: systematic review. J Gen Intern Med. 2006;21(12):1222–1229.
- McOwen KS, Whelan AJ, Farmakidis AL. Medical education in the USA and Canada, 2020. Acad Med. 2020;95(9S A Snapshot of Medical Student Education in the USA and Canada: Reports From 145 Schools):S2–S4.
- Burk-Rafel J, Mullan PB, Wagenschutz H, et al. Scholarly concentration program development: a generalizable, data-driven approach. Acad Med. 2016;91(11 Association of American Medical Colleges Learn Serve Lead: Proceedings of the 55th Annual Research in Medical Education Sessions):S16–S23.
- Havnaer AG, Chen AJ, Greenberg PB. Scholarly concentration programs and medical student research productivity: a systematic review. Perspect Med Educ. 2017;6(4):216–226.
- Blanco MA, Maderer A, Oriel A, et al. How we launched a developmental student-as-teacher (SAT) program for all medical students. Med Teach. 2014;36(5):385–389.
- Soriano RP, Blatt B, Coplit L, et al. Teaching medical students how to teach: a national survey of students-as-teachers programs in U.S. medical schools. Acad Med. 2010;85(11):1725–1731.
- Chen HC, Wamsley MA, Azzam A, et al. The health professions education pathway: preparing students, residents, and fellows to become future educators. Teach Learn Med. 2017;29(2):216–227.
- Harvey MM, Berkley HH, O’Malley PG, et al. Preparing future medical educators: development and pilot evaluation of a student-led medical education elective. Mil Med. 2020;185(1–2):e131–e137.
- Song C, Davis BJ, Lambert DR. The medical education pathway: description and early outcomes of a student-as-teacher program. Acad Med. 2015;90(4):458–461.
- Liaison Committee on Medical Education (LCME). 2021a. Accredited MD Programs in the USA. [cited 2021 Dec 06]. Available from: http://lcme.org/directory/accredited-u-s-programs/
- Stansfield C, Dickson K, Bangpan M. Exploring issues in the conduct of website searching and other online sources for systematic reviews: how can we be systematic? Syst Rev. 2016;5(1):191.
- Wilson LA, Gilliam MA, Richmond NL, et al. Geriatrics scholarly concentration programs among U.S. medical schools. J Am Geriatr Soc. 2020;68(9):2117–2122.
- Pollock JR, Moore ML, Smith JF, et al. Content and functionality of USA medical school websites. Cureus2021;13(6):e15534.
- Medical School Admissions Requirements (MSAR). 2021. [cited 2021 Dec 06]. Available from: https://mec.aamc.org/msar-ui/#/landing
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174.
- U.S. News & World Report (USNWR). 2021. 2022 best medical schools: research. [cited 2021 Dec 06]. Available from: https://www.usnews.com/best-graduate-schools/top-medical-schools/research-rankings
- USA. 1994. Geographic areas reference manual. Washington (DC): dept. of Commerce, Economics and Statistics Administration, Bureau of the Census; [cited 2021 Dec 06]. Available from: Chapter 6, Statistical Groupings of States and Counties. https://www2.census.gov/geo/pdfs/reference/GARM/Ch6GARM.pdf
- Andreatta PB, Hillard ML, Murphy MA, et al. Short-term outcomes and long-term impact of a programme in medical education for medical students. Med Educ. 2009;43(3):260–267.
- Pessegueiro AM, Kipps K, Friedman J. Training residents for future careers in medical education. Med Educ. 2018;52(5):565–566.
- Zipkin DA, Ramani S, Stankiewicz CA, et al. Clinician-educator training and its impact on career success: a mixed methods study. J Gen Intern Med. 2020;35(12):3492–3500.
- Dandavino M, Snell L, Wiseman J. Why medical students should learn how to teach. Med Teach. 2007;29(6):558–565.
- Hu WC, Thistlethwaite JE, Weller J, et al. ‘It was serendipity’: a qualitative study of academic careers in medical education. Med Educ. 2015;49(11):1124–1136.
- Snell L. Planning and implementing a teaching skills improvement program for residents. In: Edward JC, Friedland JA, Bing-You R, editors. Residents’ teaching skills (pp. 81-99). New York (NY): Springer; 2001.
- Tolsgaard MG, Gustafsson A, Rasmussen MB, et al. Student teachers can be as good as associate professors in teaching clinical skills. Med Teach. 2007;29(6):553–557.
- Gotterer GS, O’Day D, Miller BM. The emphasis program: a scholarly concentrations program at Vanderbilt University school of medicine. Acad Med. 2010;85(11):1717–1724.
- Freret T, Rana J, Schwartzstein RM, et al. Twelve tips for implementation of “student-as-teacher” programs. Med Teach. 2017;39(12):1221–1226.
- Celebi JM, Nguyen CT, Sattler AL, et al. Impact of a scholarly track on quality of residency program applicants. Educ Prim Care. 2016;27(6):478–481.
- Svider PF, Gupta A, Johnson AP, et al. Evaluation of otolaryngology residency program websites. JAMA Otolaryngol Head Neck Surg. 2014 Oct;140(10):956–960.
- Fricker RD, Schonlau M. Advantages and disadvantages of internet research surveys: evidence from the literature. Field Methods. 2002;14(4):347–367.
- Manfreda KL, Bosnjak M, Berzelak J, et al. Web Surveys versus other survey modes: a meta-analysis comparing response rates. Int J Market Res. 2008;50(1):79–104.
- Curkovic M. The implications of using internet search engines in structured scientific reviews. Sci Eng Ethics. 2019;25:645–646.
Appendix
Table A1. Agreement assessment between reviewers performing the web search algorithm.