Abstract
Airway management competency extends beyond technical skills to encompass a comprehensive approach to optimize patient outcomes. Initial and continuing education for airway management must therefore extend beyond a narrow focus on psychomotor skills and task completion to include appreciation of underlying pathophysiology, clinical judgment, and higher-order decision making.
NAEMSP recommends:
Active engagement in deliberate practice should be the guiding approach for developing and maintaining competence in airway management.
EMS learners and clinicians must be educated in an escalating approach to airway management, where basic airway maneuvers form the central focus.
Educational activities should extend beyond fundamental knowledge to focus on the development of clinical judgment.
Optimization of patient outcomes should be valued over performance of individual airway management skills.
Credentialing and continuing education activities in airway management are essential to advance clinicians beyond entry-level competency.
Initial and continuing education programs should be responsive to advances in the evidence base and maintain adaptability to re-assess content and expected outcomes on a continual basis.
Introduction: Defining Competency in Airway Management
In medical education, competence has various definitions but consistently focuses on an individual’s ability to perform a specific task. The attainment of competence is often likened to learning a clinical skill, but this is only a small part of the process. Clinical practice poses clinicians with multi-layered, ill-defined problems. Achieving the best possible patient outcomes therefore requires advanced clinical judgment - the ability to perceive a scenario, reason through management options, and decide a course of action (Citation1,Citation2).
Time and resources in education and training are invested with the goal of preparing EMS clinicians to take optimal care of patients. Prehospital research has demonstrated that adherence to evidence-based priorities of care is more important than the specific tool that is used to manage the patient’s airway (Citation3). As a result, the development of clinical airway skills is only one piece in the attainment of overall competence in airway management. Though airway training often focuses on the acquisition of the component clinical skills (e.g. bag mask ventilation, supraglottic airway [SGA] placement, endotracheal intubation), comprehensive airway management is greater than the sum of its parts, and includes knowledge of the strengths and weaknesses of different techniques and clinical decision making skills to choose the right technique for the right patient at the right time (Citation4,Citation5). Development of clinical competence in airway management therefore engages the three key domains of learning, psychomotor, cognitive and affective, to ensure internalization of the knowledge, skills, and attitudes necessary to implement a comprehensive approach (Citation6,Citation7). This resource document reviews the rationale supporting NAEMSP’s recommendations for airway management education and training.
Principles of Airway Management Education
Active Engagement in Deliberate Practice Should Be the Guiding Approach for Developing and Maintaining Competence in Airway Management.
The application of clinical judgment in situations necessitating airway management is a key component that differentiates entry-level (minimal competence) from skill mastery (advanced competence). Given the effects of out-of-hospital airway management on patient outcomes (Citation8), our educational goal is EMS clinician expertise: the ability to implement comprehensive airway management with reproducible quality under the diversity of conditions encountered in prehospital care (Citation9,Citation10).
Unfortunately, there is no clear time trajectory for attainment of advanced competence and this trajectory likely varies among learners (Citation11). However, the development of expertise has been studied in a wide variety of disciplines (Citation9,Citation10, Citation12). Contrary to common perception, expertise is not developed through experience alone. In many fields, including medicine, there is little correlation between experience alone and objective performance (Citation13). During initial education in airway management, novice EMS clinicians focus on learning to perform tasks with acceptable proficiency. This takes the form of basic knowledge of airway anatomy, oxygenation, and ventilation, and the details of procedure performance. Once EMS clinicians are familiar with fundamental concepts, they develop proficiency and automate some task components in order to perform skills with greater complexity. As a specialty, we tend to rely on a combination of clinical experience and intermittent training to maintain skills and foster further growth toward expertise. However, not only are clinical experiences unreliable in frequency, in the absence of focus on continued improvement, clinicians remain in a state of arrested development where they “go through the motions” and not only fail to improve over time but eventually have skill deterioration (). Growth from minimum to advanced competence in comprehensive airway management requires conscious effort at improving not only skills, but the development of increasingly sophisticated mental models that incorporate the complexities of pathophysiology, team dynamics, and evidence to enable higher-order decision making. Ideally, initial education accomplishes more than the development of minimum competence; it should leverage the three domains of learning to prepare learners to begin the consistent and lifelong work of improving their performance (Citation7) to advanced levels of competence (Citation6, Citation14).
Figure 1. An illustration of the course of improvement with and without deliberate practice. Initial education focuses on the development of minimum competency. Once minimum competency has been achieved, the focus of clinical practice and continuing medical education should be the development of mastery or advanced competency. While everyday activities can maintain minimum competency, the development of expertise requires deliberate practice. Figure modified from Ericsson (1998) (Citation9) © European Council for High Ability, reprinted by permission of Taylor & Francis Ltd, http://www.tandfonline.com on behalf of European Council for High Ability.
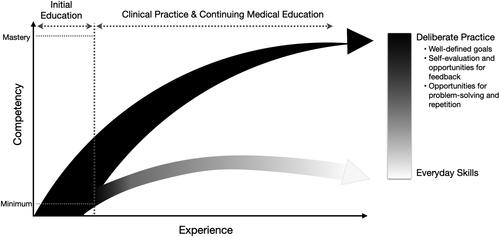
Activities will improve performance over time if a number of conditions are met, together classified as “deliberate practice”, a term coined by Ericsson et al. (Citation15) (). First, the focus of instruction must be to improve some aspect of performance for a well-defined task. Goal-oriented practice is by definition tailored to the level of the learner. Ideally, training goals should push EMS clinicians to exceed their current levels of performance by targeting their zones of proximal development (Citation13, Citation15,Citation16). This is not to say that different learner levels cannot participate in the same educational scenario, but that the goal or objective of the exercise should be tailored to the current learner level (). For learning to occur, it is critical that the goal is sensitive to the cognitive load of the EMS clinician (Citation17,Citation18). If an educational activity incorporates excessive content that far exceeds a learner’s current level, the learner will have a difficult time absorbing new information. Second, learners must receive detailed, immediate feedback on their performance. Feedback is a key step in corrective action to foster improvement, and it should be given as proximally to the task as possible and specific regarding what needs to be improved. Ideally, educational activities are of short duration with opportunities for feedback, reflection, and correction (Citation13). Over time, the goal is for EMS clinicians to develop self-assessment skills that allow them to monitor their own performance to identify areas for improvement. Importantly, patient follow-up is a form of educational feedback gained in the course of clinical experience that allows EMS clinicians to reflect on and refine their mental schema of illness and patient management; lack of access to patient follow-up remains a significant barrier to improve EMS clinician performance. Finally, learners must have ample opportunities to improve their performance gradually by performing the same or similar tasks repeatedly. Opportunities for repetition should occur both in rapid cycles and over time. Spaced repetition or distributed practice allow for the revisiting of topics or skill repetition over time and are useful for low-frequency events, including airway management (Citation19).
Table 1. Examples of integration of deliberate practice principles into airway management training and education.
A clinician’s ability to implement airway management develops through fundamental knowledge, practice, experience, and continuous analysis of practice (Citation20,Citation21). The salient goal of education and training is to help EMS clinicians develop mental representations that can be drawn upon during the process of clinical care. The complexity and diversity of these refined mental representations form the foundation of advanced competence that we are striving for as leaders, educators, and learners.
The Psychomotor Domain: Airway Skills
EMS Learners and Clinicians Must Be Educated in an Escalating Approach to Airway Management, Where Basic Airway Maneuvers Form the Central Focus.
The relative benefits and harms of different airway management approaches relate not only to underlying patient pathophysiology, but also to the skill of the clinician performing the procedure. The goal of prehospital airway management is to ensure adequate oxygenation and ventilation. The optimal prehospital airway management skill to meet this goal depends on clinician experience, clinician scope, resources available to meet other care priorities, and the environment (Citation22,Citation23). From a psychomotor perspective, the focus of education and training paradigms must also account for these complexities, ensuring focus on the skills most likely to make a difference in patient outcome given system resources. Effective basic airway skills remain the cornerstone of safe airway management at all levels (Citation4, Citation24,Citation25). While the goal remains the attainment of advanced competence in all skills, in most education and training paradigms, the ability to achieve advanced competency in basic airway skills (patient positioning, airway adjuncts, bag mask ventilation, and SGA use) exceeds the ability to achieve competency in advanced airway skills such as endotracheal intubation (Citation26–31).
In most EMS systems, the availability of tools and resources to educate EMS clinicians in basic airway management far exceeds those available to ensure advanced competency in the high-risk skill of endotracheal intubation. The following tools are considered the cornerstone of prehospital comprehensive airway instruction: lectures, videos, task trainers, low- and high-fidelity simulation, cadavers, the operating room, and clinical experience (). Historically, prehospital clinicians are taught how to perform an “airway skill” on a task trainer and deemed competent by an educator after a successful number of attempts in the classroom environment. With adequate instruction, these training devices are of benefit to practice and develop minimum competence with basic airway maneuvers such as placing oropharyngeal and nasopharyngeal airways (OPA/NPA), hand-ventilation using a bag-valve-mask, and even placement of SGAs (Citation44,Citation45). With regard to advanced skills such as endotracheal intubation, task trainers and low-fidelity mannequins are adequate for entry-level training in skill components, but achieving minimum competence let alone expert longitudinal performance with these devices is difficult if not impossible. A study of critical care paramedics using daily manikin intubation practice failed to show an improvement in live patient successful airway placement (Citation32).
Table 2. Strengths and weaknesses of airway management education tools.
While fundamental procedural understanding may be demonstrated through the use of simulation, it is challenging if not impossible to achieve competence without supervised clinical exposure to real patients. The operating room is an ideal education and training location for all levels of prehospital clinicians for both initial and retention of comprehensive airway skills. The operating room allows for a variety of airway skills to be practiced, including suctioning, OPA/NPA insertion, manual ventilation techniques, SGA insertion, and intubation (Citation35,Citation36). With regard to endotracheal intubation, significant clinical experience (> 20 endotracheal intubations) is necessary to develop > 90% success and is the greatest predictor of procedural success (Citation26, Citation43). In a study of endotracheal intubation experience of paramedic students from 60 programs, the median number of ETI encounters per student was 7 (IQR 4-12), and only 10-15% of the students achieved the standard of cumulative experience associated with proficiency in the skill (Citation26). This suggests that training programs may not have the resources to ensure minimum competency of their graduates in this high-risk skill. As such, at all levels of scope of practice and training, basic airway maneuvers are the foundation of life-saving airway management and should continue to form the central focus.
The Cognitive Domain: Development of Clinical Judgment and Higher Order Decision Making
Educational Activities Should Extend beyond Fundamental Knowledge to Focus on the Development of Clinical Judgment.
Airway management is a decision-dense process. In a Delphi study examining clinical decisions made during high acuity emergency calls, of 42 consensus important clinical decisions, 13 pertained specifically to airway management, while many others, including decisions around medication choice, treatment initiation, or changes in care plan, were directly related (Citation46). The cognitive domain refers to what a learner needs to know and includes the development of intellectual abilities and skills (Citation47). Within the cognitive domain, learners ascend through five levels of mastery: recall, comprehension, applying information, analyzing information, and synthesizing or creating (Citation48). Given the decision-density of prehospital airway management, while thorough understanding of airway assessment, physiology, and pharmacology form fundamental components of competence, development of clinical judgment encompassing the clinical reasoning process and its end point, decision making, occurs through higher order thinking that needs to be fostered (Citation1). (Citation46, Citation49).
Constructing educational activities that support the development of clinical judgment requires some familiarity with the process of clinical decision-making itself (Citation46, Citation49–51). Metacognition, the process of “thinking about thinking”, enables awareness of the decision process. While further research is needed to better elucidate the process of paramedic decision-making (Citation46), research from the field of cognitive psychology has demonstrated how decision-making occurs through use of intuitive or analytical processes (Citation52). Understanding the strengths and weaknesses of both these cognitive approaches, combined with self-awareness of which system is being used to make a decision, can help clinicians avoid diagnostic error and treat the patient appropriately (Citation52). It also allows deliberate practice to occur, as it enables focused analysis of the decision-making process, targeted goals for improvement, and a mechanism for refinement of mental schema.
There are multiple educational techniques that can be used that emphasize the development of clinical judgment and metacognition. These include simulation cases with reflection, development of cognitive-forcing strategies, the Think Aloud approach, and the Cognitive Autopsy (Citation49,Citation50, Citation53,Citation54). Each of these educational formats involves the opportunity to reflect on decisions in the context of clinical scenarios, either real or created. Regardless of the approach, educators should specifically discuss which clinical decisions are important, where the diagnostic and treatment pitfalls exist, and strategies to maintain situational awareness and make safe decisions in high-acuity clinical scenarios that require out-of-hospital airway management (Citation46, Citation55,Citation56).
Cognitive competence is dynamic and needs to be assessed both initially and over time. One proposed method for assessing higher order thinking is collaborative assignments that require learners to engage in problem-based tasks (Citation57). Another proposed method is using both a cognitive exam and simulation, as one study found a good association between the two (Citation58). Situational awareness specifically can be assessed using the Situation Awareness Global Assessment Technique (SAGAT) (Citation59). Educational activities should be continued beyond the initial training, with ample opportunities for retraining and continued practice. Once competency is achieved, skill decay occurs if the skills are not used frequently. It is likely that this applies to the cognitive domain as well. Systems should be in place to prevent this, as retraining provides measurable increases in self-efficacy and performance (Citation60).
There are many barriers to developing the cognitive domain in EMS learners. There remain many approaches and settings in which EMS education is taught and some may not be ideal (Citation61). Paramedic program accreditation does require program and outcome data (CAAHEP), but there is no single repository for EMT program data and each state has varying requirements, including none at all (Citation62). A lack of data sharing among training centers, EMS systems, and health care facilities makes determining meaningful outcomes from airway educational programs difficult. On a clinician level, lack of follow-up limits feedback to clinicians for self-assessment of their clinical judgment. These barriers have created challenges in researching and identifying best practices, learner requirements, and effective educational methods related to developing clinical competency in airway management (Citation63).
The Role of the Affective Domain in Airway Management
Optimization of Patient Outcomes Should Be Valued over Performance of Individual Airway Management Skills.
When it comes to airway management, treatment decisions should be centered on patient outcomes and not a desire to perform a procedure for the sake of the intervention. The clinician should ask oneself “which airway intervention will provide the greatest opportunity of survival?” with each encounter and consider the “right airway for the right patient.” For decades, endotracheal intubation has been viewed as the defining procedure of paramedic practice. This narrow view has led many to focus exclusively on attaining successful intubation, losing sight of the manner of intubation and how it may potentially harm the patient. Furthermore, the intubation-centric education has blinded clinicians to the possibility that endotracheal intubation may be harmful or adversely impact other important aspects of care (Citation64).
The affective domain of learning encompasses a clinician’s values and motivations and thus has a critical role to play in the development of competence in airway management. (Citation65). Our goal in airway management education is for our learners to internalize the value of patient outcome over procedural success in such a way that it influences their behavior in the course of patient care. In many EMS programs, the assessment of affective domain focuses on the student’s attitude toward class (did you dress professionally and try your best?) and bedside manner during simulated and real-life patient interactions. While professionalism and empathy toward the patient are important facets of EMS clinical care, closer analysis of values and attitudes toward procedural skills is often an overlooked feature of the affective learning domain. An EMS clinician skillful in the affective domain is an advocate for quality patient care and patient care systems while making patient care decisions with the patient at the center (Citation66). Affective domain in airway management applies most to the values and patient empathy considered when managing the airway. While the cognitive aspect is knowing the appropriate way to manage an airway, the affective domain highlights the decision to perform this intervention based on the balance between airway knowledge and what an individual values regarding the procedure. Clinicians should be taught that endotracheal intubation is just one of many tools for achieving airway management and should only be used when likely to improve patient outcome.
Traditionally we think of the affective domain as being taught through role modeling. This and implicit learning may be successful, but this is highly dependent on the learner having access to mentors who display the proper values (Citation66,Citation67). In order to improve affective performance, educational activities should focus on the goals of the student, be based on real clinical scenarios, be repeated over time, and involve intentional reflection (Citation68). Reflection allows for learning experiences to be deliberately drawn from actual experiences and allows for the transformation of experience into more meaningful concepts that can be applied to future patients (Citation69). A well-structured and deliberate reflective practice will allow for learners to connect the right affective learning objectives to the experience and begin to value patient-centered airway performance.
Like the psychomotor and cognitive domain, the affective domain is described in a taxonomy that spans from entry level performance (“Receiving” - willingness to learn about a value) to mastery (“Characterization” - acting consistently in accordance to a value). While many theorists argue that values, attitudes, and beliefs cannot be graded, one can assess the judgment and comprehensiveness of the rationale for the treatment decision (Citation68). There have been multiple attempts to validate scoring rubrics that can be used to assess an individual’s affective domain. While these have a role, many are geared toward evaluating professionalism and are less helpful for specific skills such as airway performance (Citation70). Epstein’s framework is a qualitative scale that may be a reliable option. as it simplifies affective taxonomy into three stages and can be used immediately after a transformative learning session or as a spot check on individual or system performance (Citation68). Epstein’s or other educational frameworks allow for a structured way to evaluate the decision-making that occurred in the case and assess whether it aligns with the values the organization wishes to demonstrate around airway management. Through formal evaluation of the affective domain, one is able to evaluate whether a need for improvement exists.
Credentialing and Continued Education
Credentialing and Continuing Education Activities in Airway Management Are Essential to Advance Clinicians beyond Entry-Level Competency.
Credentialing is a clinical determination of an EMS professional’s ability to practice and is based upon the verification by the EMS medical director and organizational clinical leadership of an EMS clinician’s cognitive, affective, and psychomotor abilities with patient care (Citation71). Credentialing and continuing education are essential aspects of airway management training.
While many people consider credentialing analogous to “system entry,” the term also refers to the maintenance of the ability to practice in an EMS organization and usually includes maintenance of continuing education and ongoing performance assessments. Credentialing is a continuous process and not a one-time event. Credentialing and continued education are essential to the development and maintenance of high-quality care as an EMS clinician. External markers of skill performance such as national certification help establish entry-level competence but do not guide the EMS clinician through the development from new graduate to mastery in the field of airway management. A robust credentialing and continuing education program that aims to not only confirm entry-level competence but also develop clinician skills over time is necessary to the provision of quality airway management over the course of a career. Credentialing assessments must be uniform, equally accessible, fair, consistent, objective, and based on clearly communicated evidence-based clinical performance standards, and consist of these four principles: 1) demonstration of sufficient cognitive knowledge; 2) demonstration of mature, responsible affective ability; 3) display of accurate, appropriate psychomotor skills; 4) integrating knowledge, psychomotor skills, and affect in applying critical thinking in medical decision-making for patient care (Citation72).
An airway management credentialing program is vital to continued competency given the risk of skill fade in rarely performed, complex skills such as endotracheal intubation (Citation73). Studies have shown success rates of endotracheal intubations are tied to the number of patients intubated by the individual clinician (Citation74) and one study identified that one intubation per quarter was enough to demonstrate continued competence in difficult airway intubations (Citation75).
A continued credentialing program should be designed to instruct, continually monitor, and evaluate performance in all three cognitive domains of airway management with a particular focus on clinical judgment in airway management. This can be accomplished through multiple facets. An initial training and skills assessment may serve as the first step to system entry, but continual monitoring of airway performance data in the EMS system should be performed and used to shape continued credentialing procedures. Self-assessment is a validated tool used throughout medicine to enhance learning, ensure retention, and highlight the salient details of high-risk, low-frequency procedures (Citation76,Citation77). The broad acceptance of self-assessment across medicine should indicate the value to EMS physician medical directors and adoption should be strongly considered in the initial and continuous credentialing process.
Constructive feedback and evaluations should be provided to individual EMS clinicians throughout the continuous credentialing process. When personnel are not performing well, which may be identified through review of airway cases, monitoring system benchmarks at the EMS clinician level, or during witnessed airway management in the field or simulation lab, feedback should be clear and transparent about any errors or inappropriate acts. When necessary, a remediation plan should be created for the individual to address any shortcomings regarding cognitive, affective, or psychomotor domains. The intent for the remediation should be to provide additional educational opportunities and attempts for reevaluation when deemed appropriate.
Airway Training and Evolving Evidence
Initial and Continuing Education Programs Should Be Responsive to Advances in the Evidence Base and Maintain Adaptability to Re-Assess Content and Expected Outcomes on a Continual Basis.
Our initial education systems are the beginning, not the end, of the learning process. In the field of EMS, there has been much focus on the assurance of minimum competence. While clearly this is important, it is not the only goal of airway management training and education. High quality care happens when EMS clinicians make decisions that are safe, effective, and focused on patient outcome. Our understanding the impact of specific prehospital airway management decisions on patient outcomes has and will continue to evolve as research transforms best practices. Advanced competence itself therefore remains a moving target, demanding focused effort from educators, clinical leaders, and clinicians themselves to re-assess and update content on a continual basis.
References
- Dickison P, Haerling KA, Lasater K. Integrating the national council of state boards of nursing clinical judgment model into nursing educational frameworks. J Nurs Educ. 2019;58(2):72–8. doi:https://doi.org/10.3928/01484834-20190122-03.
- Dickison P, Luo X, Kim D, Woo A, Muntean W, Bergstrom B. Assessing higher-order cognitive constructs by using an information-processing framework. Journal of Appl Testing Technol. 2016;17(1):1–19.
- Carney N, Totten AM, Cheney T, Jungbauer R, Neth MR, Weeks C, Davis-O'Reilly C, Fu R, Yu Y, Chou R, Daya M. Prehospital airway management: A systematic review. Prehosp Emerg Care. 2021;1–28. doi:https://doi.org/10.1080/10903127.2021.1940400.
- Panchal AR, Finnegan G, Way DP, Terndrup T. Assessment of paramedic performance on difficult airway simulation. Prehosp Emerg Care. 2020;24(3):411–20. doi:https://doi.org/10.3109/10903127.2015.1102993.
- Prekker ME, Kwok H, Shin J, Carlbom D, Grabinsky A, Rea TD. The process of prehospital airway management: Challenges and solutions during paramedic endotracheal intubation*. Crit Care Med. 2014;42(6):1372–8. doi:https://doi.org/10.1097/CCM.0000000000000213.
- Krathwohl DR. A revision of Bloom's taxonomy: An overview. Theory into Practice. 2002;41(4):212–8. doi:https://doi.org/10.1207/s15430421tip4104_2.
- Michels ME, Evans DE, Blok GA. What is a clinical skill? Searching for order in chaos through a modified Delphi process. Med Teach. 2012;34(8):e573–81–e581. doi:https://doi.org/10.3109/0142159X.2012.669218.
- Baker PA, Weller JM, Greenland KB, Riley RH, Merry AF. Education in airway management: Education in airway management. Anaesthesia. 2011;66(Suppl 2):101–11. doi:https://doi.org/10.1111/j.1365-2044.2011.06939.x.
- Ericsson KA. The Scientific Study of Expert Levels of Performance: general implications for optimal learning and creativity. High Ability Studies. 1998;9(1):75–100. doi:https://doi.org/10.1080/1359813980090106.
- Ericsson KA. Deliberate practice and the acquisition and maintenance of expert performance in medicine and related domains. Acad Med [Internet]. 2004;79(10):S70–S81.
- McGaghie WC, Issenberg SB, Cohen ER, Barsuk JH, Wayne DB. Does simulation-based medical education with deliberate practice yield better results than traditional clinical education? A meta-analytic comparative review of the evidence. Acad Med. 2011;86(6):706–11.
- Ericsson KA. Acquisition and maintenance of medical expertise: A perspective from the expert-performance approach with deliberate practice. Acad Med. 2015;90(11):1471–86. doi:https://doi.org/10.1097/ACM.0000000000000939.
- Anders Ericsson K. Deliberate practice and acquisition of expert performance: A general overview. Acad Emerg Med. 2008;15(11):988–94. doi:https://doi.org/10.1111/j.1553-2712.2008.00227.x.
- Peyton JR, editor. Teaching & learning in medical practice. Rickmansworth: Manticore Europe Limited; 1998.
- Ericsson KA, Krampe RT, Tesch-Römer C. The role of deliberate practice in the acquisition of expert performance. Psychol Rev. 1993;100(3):363–406. doi:https://doi.org/10.1037/0033-295X.100.3.363.
- Vygotsky LS. Mind in society: The development of higher psychological processes. Cambridge, MA: Harvard University Press; 1980.
- Young JQ, Van Merrienboer J, Durning S, Ten Cate O. Cognitive Load Theory: Implications for medical education: AMEE Guide No. 86. Med Teach. 2014;36(5):371–84. doi:https://doi.org/10.3109/0142159X.2014.889290.
- Leppink J, van den Heuvel A. The evolution of cognitive load theory and its application to medical education. Perspect Med Educ. 2015;4(3):119–27. doi:https://doi.org/10.1007/s40037-015-0192-x.
- Cheng A, Nadkarni VM, Mancini MB, Hunt EA, Sinz EH, Merchant RM, Donoghue A, Duff JP, Eppich W, Auerbach M, American Heart Association Education Science Investigators; and on behalf of the American Heart Association Education Science and Programs Committee, Council on Cardiopulmonary, Critical Care, Perioperative and Resuscitation; Council on Cardiovascular and Stroke Nursing; and Council on Quality of Care and Outcomes Research, et al. Resuscitation education science: Educational strategies to improve outcomes from cardiac arrest: A scientific statement from the American Heart Association. Circulation. 2018;138(6):e82–e122. doi:https://doi.org/10.1161/CIR.0000000000000583.
- Kienle GS, Kiene H. Clinical judgement and the medical profession. J Eval Clin Pract. 2011;17(4):621–7. doi:https://doi.org/10.1111/j.1365-2753.2010.01560.x.
- Muntean W. Nursing clinical decision-making: A literature review. Paper Commissioned by the National Council of State Boards of Nursing. 2012. https://www.ncsbn.org/Nursing_Clinical_Decision_Making_A_Literature_Review.htm
- Guyette FX, Wang HE. EMS airway management: system considerations. In: Emergency medical services: clinical practice and systems oversight; 2021;vol. 1. p. 19–29.
- Bossers SM, Schwarte LA, Loer SA, Twisk JW, Boer C, Schober P. Experience in prehospital endotracheal intubation significantly influences mortality of patients with severe traumatic brain injury: a systematic review and meta-analysis. PloS One. 2015; 10(10):e0141034. doi:https://doi.org/10.1371/journal.pone.0141034.
- Jarvis JL, Gonzales J, Johns D, Sager L. Implementation of a clinical bundle to reduce out-of-hospital peri-intubation hypoxia. Ann Emerg Med. 2018;72(3):272–9. doi:https://doi.org/10.1016/j.annemergmed.2018.01.044.
- Leeuwenburg T. Access to Difficult Airway equipment and training for rural GP-anaesthetists in Australia: results of a 2012 survey. Rural Remote Health. 2012;12:2127. doi:https://doi.org/10.22605/RRH2127.
- Wang HE, Seitz SR, Hostler D, Yealy DM. Defining the learning curve for paramedic student endotracheal intubation. Prehosp Emerg Care. 2005;9(2):156–62. doi:https://doi.org/10.1080/10903120590924645.
- Wang HE, Mann NC, Mears G, Jacobson K, Yealy DM. Out-of-hospital airway management in the United States. Resuscitation. 2011;82(4):378–85. doi:https://doi.org/10.1016/j.resuscitation.2010.12.014.
- Wang HE, Yealy DM. How many attempts are required to accomplish out-of-hospital endotracheal intubation? Acad Emerg Med. 2006;13(4):372–7. doi:https://doi.org/10.1197/j.aem.2005.11.001.
- Bledsoe BE, Slattery DE, Lauver R, Forred W, Johnson L, Rigo G. Can emergency medical services personnel effectively place and use the Supraglottic Airway Laryngopharyngeal Tube (SALT) airway? Prehosp Emerg Care. 2011;15(3):359–65. doi:https://doi.org/10.3109/10903127.2011.561410.
- Gahan K, Studnek JR, Vandeventer S. King LT-D use by urban basic life support first responders as the primary airway device for out-of-hospital cardiac arrest. Resuscitation. 2011;82(12):1525–8. doi:https://doi.org/10.1016/j.resuscitation.2011.06.036.
- Middleton PM, Simpson PM, Thomas RE, Bendall JC. Higher insertion success with the i-gel supraglottic airway in out-of-hospital cardiac arrest: a randomised controlled trial. Resuscitation. 2014;85(7):893–7. doi:https://doi.org/10.1016/j.resuscitation.2014.02.021.
- Lubin J, Carter R. The feasibility of daily mannequin practice to improve intubation success. Air Med J. 2009;28(4):195–7. doi:https://doi.org/10.1016/j.amj.2009.03.006.
- DuCanto J, Serrano KD, Thompson RJ. Novel airway training tool that simulates vomiting: suction-assisted laryngoscopy assisted decontamination (SALAD) system. West J Emerg Med. 2017;18(1):117–20. doi:https://doi.org/10.5811/westjem.2016.9.30891.
- Forney ED, Stokes NA, Ashley DW, Montgomery A, Benjamin Christie D. Can education and enhanced medical director oversight improve definitive airway control in the prehospital environment? Am Surg. 2021;87(1):159–61. doi:https://doi.org/10.1177/0003134820945228.
- Verma R, Sethi N, Honwad M, Singh S. Evaluation of four supraglottic devices used by paramedical staff for securing airway in simulated emergency airway management. Med J Armed Forces India. 2021;77(1):86–91. doi:https://doi.org/10.1016/j.mjafi.2020.02.002.
- Hansen ML, Wagner A, Schnapp A, Lin A, Le N, Deverman S, Pedigo E, Johnson A, Cusick J, Gries H, et al. Cluster cross-over randomised trial of paediatric airway management devices in the simulation lab and operating room among paramedic students. Emerg Med J. 2021;38(1):27–32. doi:https://doi.org/10.1136/emermed-2020-209929.
- Sun Y, Pan C, Li T, Gan TJ. Airway management education: simulation based training versus non-simulation based training-A systematic review and meta-analyses. BMC Anesthesiol. 2017;17(1):17. doi:https://doi.org/10.1186/s12871-017-0313-7.
- Le Guen M, Martin F. High-fidelity simulation in airway management: Aim or tool towards skills and safety? Anaesth Crit Care Pain Med. 2019; 38(4):327–8. doi:https://doi.org/10.1016/j.accpm.2019.06.007.
- Bischof JJ, Panchal AR, Finnegan GI, Terndrup TE. Creation and validation of a novel mobile simulation laboratory for high fidelity, prehospital, difficult airway simulation. Prehosp Disaster Med. 2016;31(5):465–70. doi:https://doi.org/10.1017/S1049023X16000534.
- Hall RE, Plant JR, Bands CJ, Wall AR, Kang J, Hall CA. Human patient simulation is effective for teaching paramedic students endotracheal intubation. Acad Emerg Med. 2005;12(9):850–5. doi:https://doi.org/10.1197/j.aem.2005.04.007.
- Luckey-Smith KN, High KR, Cole EM. Effectiveness of surgical airway training lab and assessment of skill and knowledge fade in surgical airway establishment among prehospital providers. Air Medical Journal. 2020;39(4):244. doi:https://doi.org/10.1016/j.amj.2020.05.003.
- Hodnick R, Zitek T, Galster K, Johnson S, Bledsoe B, Ebbs D. A comparison of paramedic first pass endotracheal intubation success rate of the VividTrac VT-A 100, GlideScope Ranger, and direct laryngoscopy under simulated prehospital cervical spinal immobilization conditions in a cadaveric model. Prehosp Disaster Med. 2017;32(6):621–4. doi:https://doi.org/10.1017/S1049023X17006872.
- Warner KJ, Carlbom D, Cooke CR, Bulger EM, Copass MK, Sharar SR. Paramedic training for proficient prehospital endotracheal intubation. Prehosp Emerg Care. 2010;14(1):103–8. doi:https://doi.org/10.3109/10903120903144858.
- Fiala A, Lederer W, Neumayr A, Egger T, Neururer S, Toferer E, Baubin M, Paal P. EMT-led laryngeal tube vs. face-mask ventilation during cardiopulmonary resuscitation - a multicenter prospective randomized trial. Scand J Trauma Resusc Emerg Med. 2017;25(1):104–7. doi:https://doi.org/10.1186/s13049-017-0446-1.
- Roth D, Hafner C, Aufmesser W, Hudabiunigg K, Wutti C, Herkner H, Schreiber W. Safety and feasibility of the laryngeal tube when used by EMTs during out-of-hospital cardiac arrest. Am J Emerg Med. 2015;33(8):1050–5. doi:https://doi.org/10.1016/j.ajem.2015.04.048.
- Jensen J. Paramedic clinical decision-making: results of two Canadian studies. Int Paramed Pract. 2011;1(2):63–71. doi:https://doi.org/10.12968/ippr.2011.1.2.63.
- Bloom BS, Engelhart MD, Furst EJ, Hill WH, Krathwohl DR. Taxonomy of educational objectives: the classification of educational goals: handbook I: cognitive domain. New York: D. Mckay; 1956.
- Gray K. Assessing data on student learning in cognitive & affective domains. [Internet]. 2021. https://study.com/academy/lesson/assessing-data-on-student-learning-in-cognitive-affective-domains.html.
- Croskerry P. Diagnostic failure: a cognitive and affective approach. In: Advances in patient safety: Vol 2. Agency for healthcare research and quality. Rockville, MD; 2005. p. 241–53.
- Croskerry P. The importance of cognitive errors in diagnosis and strategies to minimize them. Acad Med. 2003;78(8):775–80. doi:https://doi.org/10.1097/00001888-200308000-00003.
- Sandhu H, Carpenter C, Freeman K, Nabors SG, Olson A. Clinical decisionmaking: opening the black box of cognitive reasoning. Ann Emerg Med. 2006;48(6):713–9. doi:https://doi.org/10.1016/j.annemergmed.2006.03.011.
- Croskerry P. Clinical cognition and diagnostic error: applications of a dual process model of reasoning. Adv Health Sci Educ Theory Pract. 2009;14(1):27–35. doi:https://doi.org/10.1007/s10459-009-9182-2.
- Banning M. The think aloud approach as an educational tool to develop and assess clinical reasoning in undergraduate students. Nurse Educ Today. 2008;28(1):8–14. doi:https://doi.org/10.1016/j.nedt.2007.02.001.
- Bond W, Kuhn G, Binstadt E, Quirk M, Wu T, Tews M, Dev P, Ericsson KA. The use of simulation in the development of individual cognitive expertise in emergency medicine. Acad Emerg Med. 2008;15(11):1037–45. doi:https://doi.org/10.1111/j.1553-2712.2008.00229.x.
- Myatra SN, Kalkundre RS, Divatia JV. Optimizing education in difficult airway management: meeting the challenge. Curr Opin Anaesthesiol. 2017;30(6):748–54. doi:https://doi.org/10.1097/ACO.0000000000000515.
- Lee Chang A, Dym AA, Venegas-Borsellino C, Bangar M, Kazzi M, Lisenenkov D, Qadir N, Keene A, Eisen LA. Comparison between simulation-based training and lecture-based education in teaching situation awareness. a randomized controlled study. Ann Am Thorac Soc. 2017;14(4):529–35. doi:https://doi.org/10.1513/AnnalsATS.201612-950OC.
- Kasilingam G, Ramalingam M, Chinnavan E. Assessment of learning domains to improve student’s learning in higher education. J Young Pharm. 2014;6(1):27–33. doi:https://doi.org/10.5530/jyp.2014.1.5.
- Studnek JR, Fernandez AR, Shimberg B, Garifo M, Correll M. The association between Emergency Medical Services field performance assessed by high-fidelity simulation and the cognitive knowledge of practicing paramedics. Acad Emerg Med. 2011;18(11):1177–85. doi:https://doi.org/10.1111/j.1553-2712.2011.01208.x.
- Hunter J, Porter M, Phillips A, Evans-Brave M, Williams B. Do paramedic students have situational awareness during high-fidelity simulation? A mixed-methods pilot study. Int Emerg Nurs. 2021;56:100983. doi:https://doi.org/10.1016/j.ienj.2021.100983.
- Youngquist ST, Henderson DP, Gausche-Hill M, Goodrich SM, Poore PD, Lewis RJ. Paramedic self-efficacy and skill retention in pediatric airway management. Acad Emerg Med. 2008;15(12):1295–303. doi:https://doi.org/10.1111/j.1553-2712.2008.00262.x.
- Leggio WJ, Grawey T, Stilley J, Dorsett M, on behalf the Education Committee of the National Association of EMS Physicians. Education Committee of the National Association of EMS Physicians. EMS curriculum should educate beyond a technical scope of practice: Position statement and resource document. Prehosp Emerg Care. 2021;25(5):724–6. doi:https://doi.org/10.1080/10903127.2021.1925793.
- National Association of State EMS Officials. EMS Workforce planning and development: Guidelines for state adoption; 2014.
- Page D, Brazelton T, Kokx G, Jennings PA, Williams B. Paramedic student encounters with patients during clinical placements: A multi-institutional cohort study. J Am Coll Emerg Physicians Open. 2021;2(2):e12391. doi:https://doi.org/10.1002/emp2.12391.
- Carlson JN, Colella MR, Daya MR, De Maio VJ, Nawrocki P, Nikolla DA, Bosson N. Prehospital cardiac arrest airway management: An NAEMSP Position Statement and Resource Document. Prehosp Emerg Care. 2022;26(0):54–63. doi:https://doi.org/10.1080/10903127.2021.1971349.
- Krathwohl D, Bloom B, Masia B. II: Handbook II: Affective Domain. New York: David McKay, 1964.
- Yanofsky SD, Nyquist JG. Using the affective domain to enhance teaching of the ACGME competencies in anesthesiology training. J Educ Perioper Med: JEPM. 2010;12(1):E055.
- Pagatpatan CP, Valdezco JAT, Lauron JDC. Teaching the affective domain in community-based medical education: A scoping review. Med Teach. 2020; 42(5):507–14. doi:https://doi.org/10.1080/0142159X.2019.1707175.
- Stephens M, Ormandy P. An evidence-based approach to measuring affective domain development. J Prof Nurs. 2019;35(3):216–23. doi:https://doi.org/10.1016/j.profnurs.2018.12.004.
- Kolb DA. Experiential learning: experience as the source of learning and development. 2nd ed. Upper Saddle River, NJ: Pearson Education, Inc; 2015.
- Santee JA, Marszalek JM, Hardinger KL. A critique of validity analysis from instruments assessing the affective domain. Curr Pharm Teach Learn. 2019;11(2):218–29. doi:https://doi.org/10.1016/j.cptl.2018.11.010.
- National Association of State EMS Officials. National EMS Scope of Practice Model 2019. (Report No. DOT HS 812-666). Washington, DC: National Highway Traffic Safety Administration; 2019.
- Clinical credentialing of EMS providers. Prehosp Emerg Care. 2017; 21(3):397–8.
- Bentley MA, Shoben A, Levine R. The demographics and education of Emergency Medical Services (EMS) professionals: A national longitudinal investigation. Prehosp Disaster Med. 2016;31(0):S18–S29. doi:https://doi.org/10.1017/S1049023X16001060.
- Deakin C, King P, Thompson F. Prehospital advanced airway management by ambulance technicians and paramedics: is clinical practice sufficient to maintain skills? Emerg Med J. 2009;26(12):888–91. doi:https://doi.org/10.1136/emj.2008.064642.
- Thomas F, Rhoades C, Carpenter J, Holleran R, Handrahan D. Difficult airway simulator intubation success rates using commission on accreditation of medical transport systems training standards. Air Med J. 2011;30(4):208–15. doi:https://doi.org/10.1016/j.amj.2010.12.001.
- Nayar SK, Musto L, Baruah G, Fernandes R, Bharathan R. Self-assessment of surgical skills: A systematic review. J Surg Educ. 2020;77(2):348–61. doi:https://doi.org/10.1016/j.jsurg.2019.09.016.
- Erumeda NJ, Couper ID, Thomas LS. A self-assessment study of procedural skills of doctors in peri-urban district hospitals of Gauteng, South Africa. Afr J Prim Health Care Fam Med. 2019;11(1):e1–8. doi:https://doi.org/10.4102/phcfm.v11i1.1975.

