ABSTRACT
International policy documents emphasize the need to develop interprofessional education (IPE) to support collaborative dementia care in the community. The aim of this short report is to describe the development and pilot evaluation of an interprofessional dementia education workshop for primary care healthcare professionals. A three-hour workshop was iteratively developed through consultation with an expert reference group and people with dementia. The workshop was piloted with three separate primary care teams. A total of fifty-four primary care based healthcare staff who represented fourteen different health care roles in primary care participated in the pilot evaluation. The pilot workshops were evaluated using a mixed method approach which included post-workshop questionnaires for participants (n= 54)and a post-workshop focus group (n=8) with the program design team and workshop facilitators. The results of the pilot phase indicated that the workshop was useful and feasible. The workshop improved participants’ self-reported knowledge, understanding and confidence to support people with dementia and their families.Areas for improvement were identified and will be used to inform improvements to the workshop content and delivery in advance of a national roll-out. Future evaluations of the implementation of this interprofessional educational workshop will focus on its impact on healthcare professional behavior and outcomes for the person with dementia and their families.
Introduction
Primary care based health professionals are challenged by dementia care and dementia strategies across Europe emphasize the need for all staff working in primary care to be appropriately trained. There is growing recognition of the need to develop IPE to support collaborative dementia care in the community (Dreier-Wolfgramm et al., Citation2017; Jackson et al., Citation2016). Evidence suggests that models of IPE for healthcare professionals working in dementia primary care can be effective (Lee, Weston, & Hillier, Citation2013).
The aim of the study described here was to develop an interprofessional dementia workshop for primary care teams (PCTs) and evaluate the pilot phase of the implementation of the interprofessional workshop.
Background
Development of the education programme
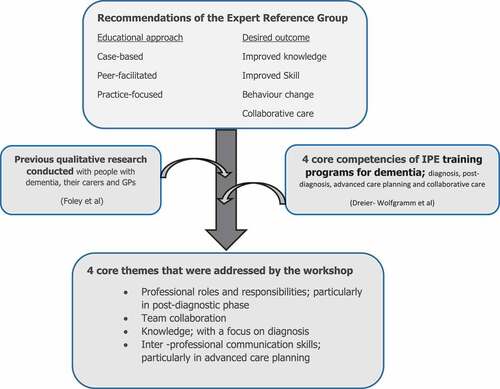
An educational needs analysis was conducted with an expert reference group comprising of an occupational therapist, physiotherapist, public health nurse, dementia clinical nurse specialist and two GPs. Each member of the expert reference group consulted with their peers and reviewed empirical literature regarding dementia education needs. In a subsequent two-hour consensus meeting the members of expert reference group mapped needs identified into key themes. These themes informed the design of the educational intervention (see ). Recommendations on the core competencies of IPE training programs for dementia were considered (Dreier-Wolfgramm et al., Citation2017). These recommendations advised the integration of clinical case studies and vignettes into programs. The expert reference group agreed that small group learning which focused on case-based discussion would most benefit the PCT.
The expert reference group consensus, together with data from interviews with GPs, people with dementia and their family caregivers reported elsewhere (Foley, Boyle S., Jennings A., & Smithson W. H., Citation2017) informed the development of an interactive, interprofessional dementia workshop for primary care teams (see ). The three-hour interactive workshop is designed around an interprofessional case study. The workshop and full facilitator’s guide is available on the following link http://dementiapathways.ie/education/pct-dementia-workshops. Two workshops were facilitated by the CNS and the third was co-facilitated by a GP and a physiotherapist.
Methods
To evaluate the workshops we adopted a sequential explanatory mixed methods design strategy. This two-step method involved first collecting quantitative data from workshop participants in the form of a post workshop questionnaire. We then conducted a qualitative focus group with the workshop facilitators and workshop observers.
Data collection
Primary care teams (PCTs) in the southern region of Ireland were identified through the professional network of the research team who work clinically in the region. Any PCT who met regularly as a functioning team was eligible for inclusion. From this population a sample of three PCTs were purposively selected to include PCTs of different practice location (urban/rural/mixed) and with different local dementia services and supports.
After the workshop participants were asked to complete an anonymous questionnaire evaluating the workshop. In a post-workshop focus group the workshop observers and facilitators were asked to identify strengths and weakness of the program. The facilitators were also asked about the pre-workshop training, workshop resources, content and delivery.
Analysis
The responses to the questionnaires were entered into Excel (2013) and analysed. Free text responses were collated into a word document and analysed by three members of the research team (AJ, TF, KMcL). The focus group was recorded using detailed field notes. Two members of the research team (AJ, TF) thematically analysed the focus group data.
Ethical considerations
Ethical approval was received from Cork Social Research Ethics Committee (Log 2017–100)
Results
Questionnaire data
In total, 54 participants representing 14 different community-based health care roles attended the three pilot workshops. The professional groups in highest attendance were; physiotherapists (n = 19), public health nurses (n = 11), occupational therapists (n = 9) and GPs (n = 4). Of these participants, 85% (n = 46) were female, and 76% (n = 41) had over five years’ experience working in primary care. The results of the questionnaire showed that more than 80% of participants agreed that the workshop improved their knowledge, confidence and understanding of dementia. (See supplementary file 1 for full table of questionnaire results)
Qualitative data from free-text responses to the questionnaires highlighted that participants valued “learning from different disciplines and their angle on caring for dementia”. The inclusion of a case study and the ability to engage in “group discussion” with PCT colleagues was particularly valued. While the majority of participants did not suggest areas for improvement some participants believed that there could be “greater opportunity” for inter-disciplinary discussions.
Post workshop focus group
Three main issues emerged from the focus group; the challenge of completing the workshop within the three hour timeframe, the benefits of co-facilitation and the depth of clinical content required.
The facilitators’ greatest concern was how to cover the material in three-hours, whilst allowing participants enough time to engage with the course content. Facilitators and observers agreed that co-facilitation of the workshop with at least two facilitators was the preferred option as this model provided “support” to the facilitator and further “promoted interprofessional discussion”. The results of the participants’ questionnaires were presented and further interpreted in the context of the workshop facilitators’ experiences and observers’ experiences of the workshop. Participant feedback highlighted the value of interprofessional learning, therefore, strategies to encourage interprofessional discussions were considered. Finally, the logistical challenge of bringing together teams to engage in the workshop was noted. Strategies to overcome this challenge were considered including; future workshop accreditation, incentives to attend and how to support staff release for the national rollout phase.
Discussion
This pilot phase of an interprofessional educational intervention for PCT professionals supporting people with dementia in the community was considered useful, feasible and was evaluated positively overall by the participants and by the facilitators.
The use of a case study was valued by the workshop participants. Similarly, previous research that evaluated a primary care based IPE program in dementia care found that case-based discussions were well received by the participating health care professionals (Lee et al., Citation2013). Although some participants felt that the workshop was too short, given the time-constraints of clinical practice it is unlikely that PCTs would be able to engage with a longer workshop. Our pilot IPE workshops improved the participants’ self-reported confidence in dementia care. The workshop participants reported an improved understanding of the skillset that other disciplines can bring to dementia care. Similarly, a recent systematic review that examined the role and impact of IPE in the care of people with dementia found that the use of IPE is likely to facilitate improvements in health care professionals’ attitudes towards other professionals’ role in dementia care (Jackson et al., Citation2016).
The vast majority of participants agreed that the workshop positively contributed to enhanced team work and collaboration. This may impact on teamwork factors, including the creation of shared value systems, clarification of roles and responsibilities and conflict management. A previous systematic review of the effects of IPE has highlighted its role in improving professionals attitudes to one another and in increasing collaborative knowledge (Reeves et al., Citation2016). Likewise, in the area of dementia care, IPE has been shown to have the potential to improve collaborative knowledge (Jackson et al., Citation2016). Further research as part of the national roll-out of these IPE workshops will help to determine whether this improved attitude towards teamwork promotes ongoing positive working relationships and whether it ultimately impacts upon interprofessional patient referrals.
In addition to the learners’ experiences of the IPE workshop we also sought to establish the experience of the workshop facilitators. The benefits of co-facilitation were highlighted. Research has found co-facilitation to be an important method of strengthening collaboration and supporting IPE facilitators (Crow & Smith, Citation2003). Exploring the experience of the facilitators also helped to identify the support needs of the facilitators. This will be used to inform the ‘train the trainer sessions’ we will develop for the national roll-out.
This pilot phase helped us to identify a number of practical implementation problems. Most notably the challenges of recruitment of PCTs given the small number of functioning PCTs who meet on a regularly basis in Ireland. The logistical challenges of bringing together interprofessional teams was a significant issue identified. This challenge has been identified in previous primary care based IPE programs (Paquette-Warren et al., Citation2014).
Study limitations
The evaluation of the learners’ experiences of the pilot IPE workshops focused on assessing the participants’ views of the workshop, identifying if the workshop impacted on the healthcare professionals’ attitudes to collaborative care and assessing if it improved participants’ self-reported knowledge and skill. In terms of interprofessional outcomes identified on a modified Kirkpatrick (Hammick, Freeth, Koppel, Reeves, & Barr, Citation2007) this pilot phase reached level 2b. Measuring behavioural change among participants and the impact on outcomes for people with dementia was beyond the scope of this phase of the study. However, it will be considered as the intervention is modified and prepared for roll-out across PCTs nationally.
The observers who participated in the workshops were members of the wider research team, however, they were not personally involved in the development of this specific work stream of the project. Nonetheless, the role of the research team in the focus group is a potential limitation of the study. Additionally, it is possible that the involvement of the research team in the focus groups impacted on the feedback provided by the workshop facilitators. However, the facilitators were encouraged to speak freely and share any concerns they had about the training they had received or workshop content and delivery.
Concluding comments
This report highlights the value of involving the relevant stakeholders in the design of the educational content and emphasizes the value of piloting of educational interventions prior to full roll-out. Feedback from the learners and from the facilitators will be used to further refine the workshop prior to national roll-out.
Supplemental Material
Download MS Word (12.3 KB)Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Crow, J., & Smith, L. (2003). Using co-teaching as a means of facilitating interprofessional collaboration in health and social care. Journal of Interprofessional Care, 17(1), 45–55. doi:10.1080/1356182021000044139
- Dreier-Wolfgramm, A., Michalowsky, B., Austrom, M. G., van der Marck, M. A., Iliffe, S., Alder, C., … Hoffmann, W. (2017). Dementia care management in primary care: Current collaborative care models and the case for interprofessional education. Zeitschrift fur Gerontologie und Geriatrie, 50(Suppl 2), 68–77. doi:10.1007/s00391-017-1220-8
- Foley, T., Boyle, S., Jennings, A., & Smithson, W. H. (2017). “We’re certainly not in our comfort zone”: A qualitative study of GPs’ dementia-care educational needs. BMC Family Practice, 18(1), 66. doi:10.1186/s12875-017-0639-8
- Hammick, M., Freeth, D., Koppel, I., Reeves, S., & Barr, H. (2007). A best evidence systematic review of interprofessional education: BEME Guide no. 9. Medical Teacher, 29(8), 735–751. doi:10.1080/01421590701682576
- Jackson, M., Pelone, F., Reeves, S., Hassenkamp, A. M., Emery, C., Titmarsh, K., & Greenwood, N. (2016). Interprofessional education in the care of people diagnosed with dementia and their carers: A systematic review. BMJ Open, 6(8), e010948. doi:10.1136/bmjopen-2015-010948
- Lee, L., Weston, W. W., & Hillier, L. M. (2013). Developing memory clinics in primary care: An evidence-based interprofessional program of continuing professional development. The Journal of Continuing Education in the Health Professions, 33(1), 24–32. doi:10.1002/chp.21163
- Paquette-Warren, J., Roberts, S. E., Fournie, M., Tyler, M., Brown, J., & Harris, S. (2014). Improving chronic care through continuing education of interprofessional primary healthcare teams: A process evaluation. Journal of Interprofessional Care, 28(3), 232–238. doi:10.3109/13561820.2013.874981
- Reeves, S., Fletcher, S., Barr, H., Birch, I., Boet, S., Davies, N., … Kitto, S. (2016). A BEME systematic review of the effects of interprofessional education: BEME guide no. 39. Medical Teacher, 38(7), 656–668. doi:10.3109/0142159X.2016.1173663