ABSTRACT
It is challenging to organize interprofessional activities in terms of coordinating students’ various schedules. These challenges can be overcome by providing flexible online opportunities based on virtual patients (VPs). This study set out to study feasibility of using a blended approach based on virtual patients and a flexible interprofessional student encounter. The encounter was arranged in pairs or triads between nursing and medical students from two separate courses. Data were gathered through a questionnaire and followed up with group interviews. Reflective texts from the interprofessional encounters were analyzed in relation to descriptions of interprofessional competence. The great majority (86%) chose to meet online due to its flexibility. The participants gained an understanding of the other profession’s roles and competences and a holistic patient awareness. Given its flexible and scalable opportunities, the blended online virtual patient approach provides a valuable contribution to an interprofessional programme.
Introduction
The need for interprofessional competence of future health professionals is undisputed. Many health profession schools increase their interprofessional activities to respond to the demands of interprofessional competence in healthcare. Interprofessional competence is relating to values and ethics, roles and responsibilities, interprofessional communication, along with teams and teamwork (IPEC Citation2016). An important aspect of interprofessional education (IPE) is student encounters in which students from various professions discuss clinical cases bringing complementary professional perspectives to the fore.
However, the implementation of such encounters faces challenges of integrating different curricular content and timing (Wong et al., Citation2019). A practical challenge is when students study on different campuses with varying schedules (Lawlis et al., Citation2014). Consequently, it is valuable to evaluate learning activities with less logistical demands that yet contribute to interprofessional learning. By using digital technology, flexible online learning activities can be organized to support such a strategy (Pulman et al., Citation2009; Weinstein et al., Citation2010). Earlier work has used technology to provide discussion forums in which students elaborate on various professional and interprofessional approaches to patient management in online settings (Cannistraci et al., Citation2018; Miers et al., Citation2007). The content for such discussions is often connected to clinical scenarios to which post-factum reasoning can be applied.
Another approach is to use interactive patient scenarios, virtual patients (VPs), to increase the process of active clinical reasoning (Cook & Triola, Citation2009). Shoemaker et al. (Citation2015) implemented an interprofessional VP activity with three health profession student groups and found it to increase interprofessional competencies and create awareness of how different professions contribute to patient care. Online IPE has been proposed as a scalable and sustainable alternative for developing teamwork in health profession students (Djukic et al., Citation2015). However, there are relatively few contemporary reports on online IPE, which could be explained by challenges in combining technological competence and educational expertise in the intersection of various professional perspectives. Miers et al. (Citation2007) highlight the need for efforts in preparing both students and staff for an online IPE context.
Online courses have been successfully implemented in which students learn about interprofessional competence, albeit without interacting with other students (Potthoff et al., Citation2020). Approaches to enquiry-based interprofessional learning for large amounts of students has been implemented using asynchronous online discussions. In addition to logistical benefits, pedagogical gains have also been identified with online opportunities (Harrison et al., Citation2012; Hughes et al., Citation2004). Students generally find such discussions engaging, appreciate the flexible opportunities, yet miss the “social information” available in face-to-face encounters (Harrison et al., Citation2012; Hughes et al., Citation2004).
Students’ motivation is crucial in professional education, which can be enhanced by establishing authenticity and relevance in active learning situations (Kember et al., Citation2008). Simulated activities have been shown to establish authenticity and relevance for students (Edelbring et al., Citation2019). Moreover, simulated clinical scenarios can be presented online using VPs for which IPE objectives can be designed (Posel et al., Citation2015). The use of VPs has been identified as an active approach to clinical reasoning training (Kononowicz et al., Citation2019). However, few reports exist on using VPs in conjunction with a collaborative interprofessional discussion. There is broad consensus on what interprofessional competence is, yet this competence is complex to assess and requires a variety of approaches in the design of learning activities. Thus, there is a need for an overarching IPE strategy in which several learning activities are implemented (Thistlethwaite et al., Citation2019). An important part of IPE curricula is student encounters in which they meet and discuss clinical scenarios with students from other professions. This study aims to explore the feasibility of using VPs in combination with online student encounters for interprofessional learning.
Research questions
How do flexible online encounters contribute to interprofessional learning?
How do medical and nursing students express interprofessional aspects in joint discussions based on virtual patient cases?
Methods
Context
This study was performed with second year nursing and third year medical students at a large medical university in Sweden in two consecutive cohorts during autumn 2017. In total, 280 students (119 nursing, 161 medical) were invited to participate. Nursing students were recruited from a course in primary healthcare and medical students from a course in dermato-venereology. For most activities, the medical and nursing programmes run on different campuses.
Interprofessional learning activity
Four VPs were designed using the VIC VP platform (Tait, Citation2019). The VPs suffered from venous leg ulcer, arterial leg ulcer, eczema, or pruritus (itching). The VIC platform allows for choices of actions in relation to the specific case and thereby gather patient information as a basis for clinical reasoning. The students then suggest a likely diagnosis and suggest further action and management followed by pre-programmed feedback on the selected actions.
Both medical and nursing students first worked individually with the four VPs in their respective courses in a self-directed manner. They were then randomly assigned to an interprofessional group for a collaborative case discussion (). The groups were stratified for profession and consent to participate in the study. Because of the greater number of medical students, the groups were either pairs or triads, with two medical students in each triad. A free choice was given for the form of the meeting; for example, a physical face-to-face or an online setting. Each group selected one of the four VPs as a basis for the collaborative assignment guided by four questions:
1) How would you jointly manage this patient in practice?
2) Please describe the collaborative clinical reasoning and actions in relation to the patient.
3) What does the collaboration between the nurse and the physician look like in this patient case?
4) What opportunities, challenges, and risks do you see with collaboration in health care?
Answers to these questions were sent to a teaching assistant and formed a basis for teacher feedback to students.
Data collection and analyses
Data collection
Data consisted of questionnaire data, collaborative assignment texts, and group interviews (). A group of three researchers with nursing, medical, and education competence performed the analyses, with critical contributions from all authors.
Questionnaire
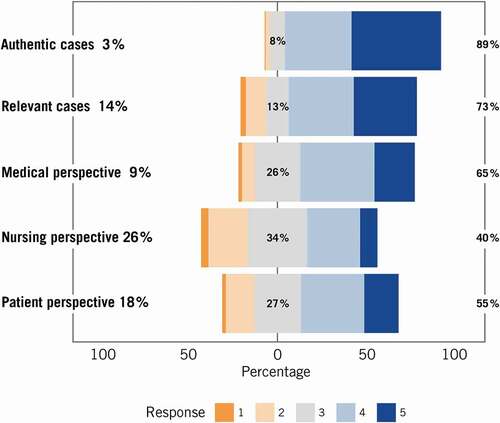
A questionnaire was devised with Likert-graded items (1–5; strongly disagree-strongly agree with a neutral midpoint) on relevance, authenticity, and characteristic perspectives of the VPs adapted from a simulation-based interprofessional learning study (Edelbring et al., Citation2019). Free text questions concerned forms for and evaluations of the VPs and the collaborative assignment. The questionnaire was distributed to medical students in conjunction with the course exams and to the nursing students during a seminar in the first cohort and, for practical reasons, online for the second cohort. The questionnaire was analyzed using descriptive statistics and visualized using stacked bar plots. Differences between groups and between perceived medical and nursing perspectives were analyzed using the Mann–Whitney test.
Collaborative assignment
Data from the group assignment in the second cohort was gathered from groups in which all students in the group consented to participate in the study (23 groups). The assignment texts were first assessed in terms of quality of the reflections by using a four-level rating based on Moon’s framework for assessing student reflections (Moon, Citation2007). The criteria range from Level 1 displaying a purely descriptive text with no reflective considerations and Level 4 represents deep reflection displaying metacognitive awareness.
This assessment was first performed individually by three analysts, then calibrated regarding differences and resolving these with consensus. The interprofessional content of the texts were then collaboratively and deductively coded into six aspects of interprofessional competence (below) based on principles of thematic analysis (Braun and Clarke, Citation2006). The interprofessional aspects were synthesized from two broadly used interprofessional competence frameworks: the Interprofessional Education Collaborative (IPEC, The interprofessional educational collaborative, Citation2016) and the Interprofessional Collaborator Assessment Rubric (Curran et al., Citation2011):
(1) Collaborative patient-centred care relates to the ability to apply patient-centred principles through interprofessional collaboration.
(2) Conflict management and resolution concerns the ability to effectively manage and resolve conflict between and with other healthcare providers, patients, and families.
(3) Interprofessional communication is the ability to communicate with patients, families, communities, and professionals in health and other fields effectively in a respectful and responsive manner.
(4) Roles and responsibilities relates to the ability to explain one’s own roles and responsibilities, as well as understanding the roles and responsibilities of other healthcare professionals.
(5) Teams, teamwork, and collaboration involves the ability to contribute to effect team functioning to improve collaboration and quality of care.
(6) Values/ethics for interprofessional practice describes working with individuals of other professions to maintain a climate of mutual respect and shared values.
Group interviews
Group interviews were conducted to enrich questionnaire data and to identify possible new aspects. Students from the second cohort were randomly selected and invited to two groups from nursing (4 students) and two from medicine (10 students). Researchers not directly involved with these students conducted the interviews (authors SE, JN, and SS). The interviewers used a preliminary analysis of the questionnaires as a guide, but also allowed free discussion between participants. The transcripts were deductively analyzed using already identified themes from the questionnaire, while allowing for new themes to emerge (Braun and Clarke, Citation2006). Free text data, collaborative reflections, and group interview data were analyzed separately, however reported collectively in the result section.
Ethical considerations
The ethical aspects were discussed and the research was approved in the regional ethical board in Stockholm (dnr: 217/1166-31). Participation in the study was voluntary and only consenting students were involved.
Results
A total of 201 students responded to the questionnaire: 141 medical and 60 nursing students (). The response rate was high overall (71%) but very low (19%) for nursing students in the second cohort in which the questionnaire was distributed online. Median age was 25 years, 61% were women, 37% men, and 2% did not state their sex.
Table 1. Questionnaire respondents in two cohorts
Student choices of meeting form
The great majority (86%) chose to meet online for the collaborative assignment. The online meeting varied between using Skype, Facebook Messenger, Google Docs, or a combination thereof. The predominant reason for selecting an online encounter was flexibility in time and space. The students expressed challenges in finding common times and places for a physical meeting because of the distance to another campus, perceived lack of time, and competing schedules. However, some students (14%) arranged a physical face-to-face meeting. A salient reason was that the physical form was efficient to enrich the discussion and get a meaningful value in the encounter with the other profession. Examples of meeting places were the university library, study rooms, and cafés.
Perceptions of the interprofessional encounter
In the free text questionnaire responses and in the interviews, students generally reported a great value in joint case discussions. The medical students expressed an increased awareness of roles and different professional perspectives, while not many expressed topic-related knowledge gains. For example: “It was good! Interesting to learn how nursing students think”. They mentioned an increased understanding of nurses’ roles and perspectives and noted that these perspectives differed from their own. The greater picture on patient work became clearer.
Nursing students reported increased knowledge on physicians’ roles and their perspective on the patient cases, a deeper understanding on their own roles, and the importance of collaboration. For example, “I realized that the physician and nursing professions belong together and that they depend on each other”. Several nursing students commented on the lack of engagement of their medical student peers and that they seemed unaware of nursing processes. For example, “I realized that medical students don’t really understand what nursing students learn, and also that they are people like us, unsure about our future professional roles”.
A core value of the encounter was the direct interaction in the encounter. However, the form of the interaction was less crucial. It could occur both face-to-face and also synchronously online. The encounter was not highly appreciated by all. Despite overall positive reports on increased knowledge on roles and awareness of nurses’ perspective, several of the medical students stated that the collaborative activity was unnecessary and that they did not learn anything useful from it. Short available time, bad timing in relation to another clinical exam, and lack of a physical meeting assisted by a teacher was mentioned as reasons. Fewer, positive comments expressed that it was fun and rewarding to meet nursing students and that discussions on patient cases that would otherwise seldom occur during education. One example: “It was good! Interesting to learn how nursing student thinks”. Nursing students also mentioned negative aspects, mostly regarding the lack of engagement and lack of understanding for nursing processes on the part of the medical students.
Collaborative assignment content
Forty-five medical students (out of 86) and 33 nursing students (out of 60) consented to analysis of their collaborative reflective texts. Ten of the consenting nursing students were grouped with non-consenting medical students and not analyzed. Therefore, in total, 23 interprofessional groups were analyzed. The great majority (18) selected a virtual patient suffering from leg ulcer as a basis for their collaborative assignment. The reflection level in the assignments were overall shallow in their expressions. No groups presented the highest (4) level of reflection, three groups displayed Level 3, 11 groups Level 2 and nine groups Level 1. Most expressions regarding interprofessional competencies were categorized into Roles and Responsibilities, followed by Teams and, teamwork, and Collaboration and interprofessional communication. Fewer expressions were categorized into Values/ethics and conflict management and resolution.
Roles and responsibilities
Most of responses to assignment questions regarded the roles and responsibilities of nurses and physicians in relation to the selected patient case. For example, a typical description of roles was:
The nurse is responsible for the caring and wound care in joint consultation with the physician. The physician prescribes the relevant tests for Torsten [the VP] and the nurse performs the tests (collaborative reflection, Group 18).
Students from both professions learned more about each other. Several nursing students expressed that they wished medical students had more knowledge about their education and expertise. The interprofessional encounter opened the nursing field to some extent with concrete examples in relation to a patient case.
You got to see a bit of the nursing practice that nurses learn a lot about and are very competent in. In this case you really learnt that it’s a much bigger thing than you first thought (collaborative reflection, Group 18).
The importance of clear roles and responsibilities were salient in the data. For the students, the borders between professional roles were sometimes perceived as blurred, and they articulated a risk for everyone’s responsibility being no one’s responsibility. However, they stated the value of using competencies from several professions for the benefit for the patient.
Students expressed the nurse’s role as being responsible for caring relations and assessment of patient care needs. The physician’s role was characterized as responsible for medical investigation, assessment, and treatment. Other professions than nurses and physicians engaged in patient care were also mentioned, such as dieticians and assistant nurses.
Teams, teamwork, and collaboration
Collaboration was considered of utmost importance for patient-centered quality of care. A holistic patient view and a well-functioning working environment were provided as reasons for interprofessional collaboration. However, the students saw challenges, such as malfunctioning interpersonal relations and organization structures not always supporting team collaboration.
A more holistic patient view can be reached based on the different perspectives from nurses and physicians, both medically and caring-wise (collaborative reflection, Group 19).
Interprofessional communication
Good and clear communication was mentioned as being crucial for collaboration in healthcare. When interprofessional communication fails, the patients risk “falling through the cracks”. The benefits of good communication were mentioned, such as higher quality of care, better compliance for the patients, and also helpful in continuing learning for professionals. Nonfunctional communication was seen as a risk, both in verbal communication and in written documentation, such as in patient-records. Hierarchy and lack of knowledge about roles were identified as hampering communication, as well as fostering a climate that does not allow for questioning decisions.
Collaborative patient-centered care
Students expressed that efficient interprofessional collaboration and communication and taking each other’s competencies and experiences into consideration are essential for patient safety and increased patient satisfaction of delivered healthcare. Through collaboration, healthcare professionals can focus on the patient’s unique care needs, leading to the best possible medical treatment and high-quality care.
Values/ethics for interprofessional practice
For a well-functioning interprofessional practice, the students discussed the importance of good understanding and respect for the other health profession’s knowledge. This contributes to better care for the patient, but also to a better working climate with possibilities to question others’ decisions. Mutual professional insights could elucidate new aspects, and provide a holistic view of the patient’s problems and his/her care needs. Challenges for interprofessional practice were identified, such as hierarchies in healthcare and limiting the sharing of knowledge and values.
Conflict management and resolution
The students mentioned several examples of challenging situations. However, few suggestions of how these could be resolved were provided. High workload and time pressure were concrete obstacles to managing misunderstandings and resolving conflicts between healthcare professionals. A tight working schedule made it difficult to find the time for an interprofessional dialogue in relation to patient care. One suggestion was that healthcare teams reflect at the end of each week on what had worked well or not.
Characteristics of virtual patient cases
The students perceived the characteristics of the VP cases as being clinically authentic (89%) and relevant (73%) for their learning in the preparatory individual work (). The authenticity was strengthened by the ability to interact with the patient from the first encounter in the waiting-room throughout the whole clinical reasoning process. The VP interaction was perceived as being an active approach to learning. Furthermore, the cases were perceived as being representative for primary healthcare.
-You felt as you were there, as if it was a real situation(group interview, Nursing 1).
-And this thing about Carbamide cream. That it stings on baby skin. It’s easier to remember [when it’s in a VP case]. If you’d read it in a text, you would perhaps never have remembered it. -No, but now it became real (group interview, Nursing 2).
The characteristics of the VP cases were perceived differently by the two student groups, except for the medical perspective that was perceived as salient for both nursing and medical students (65% agreeing, ). The nursing perspective were rated remarkably less, 40% agreeing and large numbers of disagreeing or neutral to this statement (). The patient perspective was relatively low endorsed, with 55% agreeing that this perspective was prominent in the cases. However, the group interviews revealed that the students had difficulty interpreting the meaning of perspectives in characterizing VP cases from these perspectives.
Table 2. Descriptive statistics of Likert item responses to the questionnaire
Course integration
The general impression among the students was that the VP activity was not a priority in their studies since it was not graded, and they had several other assignments during the same period. They also sought more clear descriptions regarding the assignments. Many students wanted a mandatory scheduled physical meeting.
The meeting has to be tighter regulated; students don’t do it by themselves(medical student, questionnaire free text).
Discussion
This study sought to increase knowledge about flexible interprofessional encounters based on joint virtual patient experiences. Our study showed that a flexible interprofessional student encounter is possible for students in two separate courses, and that interprofessional learning took place. Most students chose an online format. The most prominent aspect of interprofessional competence in student reflections was the roles and responsibilities of different professions. Furthermore, it provided a holistic patient perspective through the complementary professional view.
Discrepancy between preferred and selected meeting form
The dominant selected online setting for the encounters did not, however, resonate with how students express their preferences for a collaborative interprofessional encounter. There were mixed individual expectations on the interprofessional encounter, ranging from just getting the mandatory assignment done to getting to know and exchange experiences with students from another profession. Most of these expectations seem to have been met in both online and physical encounters. The unmet goals and disappointments of the encounters, such as disinterested peers, were not related to the form of the meeting. The synchronous interaction and preferable visible face-to-face interactions seem to have played an important role in the encounters. A synchronous setting has previously been reported as being important (Cummins et al., Citation2016), while sometimes difficult to conduct online due to technical reasons (Evans et al., Citation2014). No student in this study reported any technology-related issues; thus, it is reasonable to believe that online technologies have matured and students are more accustomed to using them. Therefore, a cognitive presence, identified as being necessary in effective online learning, was also possible to achieve in the online settings (Garrison et al., Citation2001).
Perceptions and content of the interprofessional encounter
The interprofessional educational value for students from the encounters can be said to consist of increased holistic patient views and encounters with a different professional perspective. Consequently, it contributed to their forthcoming professional development, even if low levels of reflection were observed.
The generally shallow characteristics of student reflections show that not many had previously reflected on how interprofessional collaborations come into play in relation to concrete patient cases. In line with suggestions from Djukic et al. (Citation2015), the online contribution may thus not be enough to establish the whole extent of IPE competencies. Not all six interprofessional aspects used as analytical framework were sufficiently covered by the activity. Instead, the encounter presents a valuable contribution, complementary within an overarching IPE programme (Anderson et al., Citation2016). Key contributions were personal student encounters across professional borders and a high degree of learner agency in the situation.
Improved course integration
Successful IPE should be based on relevant patient situations in line with real practice (Wong et al., Citation2019). Our findings established that this could be reached by using VPs. However, in this specific activity, future implementations can improve on assignment instructions and examination interprofessional learning outcomes. For example, the current examination was not fully aligned with the interprofessional activity. Reflective assignments were found to promote a reflective interprofessional practice and can be assessed by analyzing levels of reflection (Naeger et al., Citation2015) as well as the interprofessional content. Such assessment could be used either formatively to support students’ reflective awareness, or summative within an overarching IPE programme (Anderson et al., Citation2016).
Student autonomy
The interprofessional encounters were not initiated by students themselves but designed as a learning activity, intersecting two courses in separate professional study programmes. The literature on collaborative learning identify a conflict between learner autonomy and teacher-organized collaboration (i.e., scripted collaboration) (Kollar et al., Citation2006). Given that the collaborative encounter occurred on students’ own terms, without teacher access, the outcomes are supposedly related to a high self-regulated ability and productive teacher instructions or assignment questions. The interprofessional encounter was thus loosely scripted, supported by assignment questions based on a common VP case.
The students freely negotiated aspects such as form, time, and place. Consequently, students’ preparedness and support for self-regulation should be considered in the further design of such flexible interprofessional encounters (Edelbring, Citation2012; Edelbring & Wahlstrom, Citation2016; Vermunt & Donche, Citation2017). Students’ inner motivation is important for taking ownership of their learning process. However, this motivation should resonate with teacher support and a constructive alignment of the course design. Teachers play a role in signaling the importance of interprofessional collaboration and the model for teacher support should be adapted to students’ needs in the activity (Evans et al., Citation2020).
In this study, teacher support was provided after the actual encounter, in response to issues that students wished to discuss. As it turned out, many students wished for a deeper discussion in a mandatory teacher-led seminar as a part of the student encounters. Whether such an activity had promoted deeper interprofessional awareness and connection to the other profession is, however, an unanswered question. In this activity, motivation for interprofessional collaboration were provided through seeing the larger picture – a more holistic patient view – because of encountering another professional perspective. This insight was made during or at the end of the activity. It is reasonable to believe that having this motivation prior to the activity would have engaged the students even more in the process.
The interprofessional value can increase in further constructive alignment of the educational framework, foremost regarding clearly communicated intended learning outcomes. Assuming that students’ autonomy is fueled by their short and long-term goals, these students saw a benefit for their long-term goal as future health professionals in getting to know more about the other profession. However, the short-term goals were largely focusing on other demands in the primary learning objectives in the courses, which was not made explicit as professional development or interprofessional competence. Besides the clinical case-related knowledge, The VP case work that preceded the encounter served the purpose of creating a common frame of reference for the interprofessional encounter. The interprofessional value can improve even more if already at this point ask students to note aspects that they want to ask or discuss with the other profession.
The nursing perspective that is not obvious
The medical perspective was easily recognized by both medical and nursing students. However, the nursing perspective in the VPs was not easily observed by the medical students. In another design comparison between mixed student groups and mono-professional case-based interprofessional education showed that medical students in mono-professional groups were not able to identify nursing roles in the clinical case to the same extent as those in mixed groups (Mitchell et al., Citation2010). Thus, efforts should be made to make nursing perspectives concrete in VP presentations as well as in the educational framework surrounding the activity. This can be done in identifying concrete actions related to the specific VP scenarios in addition to theoretical models describing nursing practice. The high amount of “neither or”-responses to all perspective-related questionnaire statements indicate that students need more precise and concrete explanations of perspectives. Consequently, besides differences between the medical and nursing perspectives, no far-reaching conclusions can be drawn on students’ abilities to grasp different professional perspectives in VPs from these results.
Conclusions
Logistical challenges in interprofessional education can be overcome with online encounters. Although many students prefer teacher-led discussions, insights into interprofessional competence can be reached through online encounters. Students can gain a holistic patient view and increase their awareness of the roles and competencies of the other profession in such encounters. Given its flexible and scalable opportunities, the blended online virtual patient approach provides a valuable contribution to an overarching IPE strategy.
Additional information
Funding
Notes on contributors
Samuel Edelbring
Samuel Edelbring, PhD, is Associate professor in medical education and vice dean for education at the Faculty of medicine and health at the Örebro University. He leads the research group “Learning and professional development” which explores research questions relating to interprofessional learning, clinical reasoning and students’ self-efficacy in professional practice.
Eva Broberger
Eva Broberger, RNT, PhD, is a senior lecturer in nursing at the Department of Neurobiology, Care Sciences and Society, Karolinska Institutet. Her research interests are in interprofessional learning, students’ learning and professional development.
Susanna Sandelius
Susanna Sandelius Rn, Med.lic. is a lecturer at the Department of Neurobiology, Care sciences and Society, Karolinska Institutet, Sweden.
Jessica Norberg
Jessica Norberg is a MD and clinical teacher in Dermatology. She is interested in developing teaching practices supporting students’ clinical reasoning.
Desiree Wiegleb Edström
Desiree Wiegleb Edström, MD, PhD, is Senior lecturer at the School of Medical Sciences, Örebro University and Associate professor in Dermatology. She is involved in designing web-based virtual patients for interprofessional contexts and is interested in exploring clinical reasoning in everyday clinical practice.
References
- Anderson, E., Smith, R., & Hammick, M. (2016). Evaluating an interprofessional education curriculum: A theory-informed approach. Medical Teacher, 38(4), 385–394. https://doi.org/https://doi.org/10.3109/0142159X.2015.1047756
- Braun, V., & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in Psychology, 3(2), 77–101. https://doi.org/https://doi.org/10.1191/1478088706qp063oa
- Cannistraci, P., Kehm, B., Pieper, B. B., Speerschneider, K., Farber, S. L., & Storandt, B. C. (2018). Difficult to doable: Interprofessional collaborative practice in distance education. Journal of Nursing Education, 57(4), 225–228. https://doi.org/https://doi.org/10.3928/01484834-20180322-06
- Cook, D. A., & Triola, M. M. (2009). Virtual patients: A critical literature review and proposed next steps. Medical Education, 43(4), 303–311. https://doi.org/https://doi.org/10.1111/j.1365-2923.2008.03286.x
- Cummins, M., Rajan, N. S., Hodge, C., & Gouripeddi, R. (2016). Patterns and perceptions of asynchronous video discussion in a graduate health sciences course. Journal of Nursing Education, 55(12), 706–710. https://doi.org/https://doi.org/10.3928/01484834-20161114-08
- Curran, V., Hollett, A., Casimiro, L. M., McCarthy, P., Banfield, V., Hall, P., Lackie, K., Oandasan, I., Simmons, B., & Wagner, S. (2011). Development and validation of the interprofessional collaborator assessment rubric (ICAR). Journal of Interprofessional Care, 25(5), 339–344. https://doi.org/https://doi.org/10.3109/13561820.2011.589542
- Djukic, M., Adams, J., Fulmer, T., Szyld, D., Lee, S., Oh, S.-Y., & Triola, M. (2015). E-Learning with virtual teammates: A novel approach to interprofessional education. Journal of Interprofessional Care, 29(5), 476–482. https://doi.org/https://doi.org/10.3109/13561820.2015.1030068
- Edelbring, S. (2012). Measuring strategies for learning regulation in medical education: Scale reliability and dimensionality in a Swedish sample. BMC Medical Education, 12(1), 76. https://doi.org/https://doi.org/10.1186/1472-6920-12-76
- Edelbring, S., Allvin, R., Karlsson, K., Hjelmqvist, H., Hjelm, C., Brandt, J., & Tamás, É. (2019). Interprofessionell simulering är engagerande och relevant (Interprofessional simulation: An engaging and relevant technique for teamwork practice). Läkartidningen, 116(19–20), 116. PMID: 31192437. https://pubmed.ncbi.nlm.nih.gov/31192437/
- Edelbring, S., & Wahlstrom, R. (2016). Dynamics of study strategies and teacher regulation in virtual patient learning activities: A cross sectional survey. BMC Medical Education, 16(1), 122. https://doi.org/https://doi.org/10.1186/s12909-016-0644-y
- Evans, S., Knight, T., Sønderlund, A., & Tooley, G. (2014). Facilitators’ experience of delivering asynchronous and synchronous online interprofessional education. Medical Teacher, 36(12), 1051–1056. https://doi.org/https://doi.org/10.3109/0142159X.2014.918254
- Evans, S., Ward, C., Shaw, N., Walker, A., Knight, T., & Sutherland-Smith, W. (2020). Interprofessional education and practice guide No. 10: Developing, supporting and sustaining a team of facilitators in online interprofessional education. J Interprof Care, 34(1), 4-10. https://doi.org/https://doi.org/10.1080/13561820.2019.1632817
- Garrison, D. R., Anderson, T., & Archer, W. 2001. Critical thinking and computer conferencing: A model and tool to assess cognitive presence. American Journal of Distance Education, 15(1), 7-23.
- Harrison, G., Mulloy, B., Harris, A., & Flinton, D. (2012). On-line case discussion assessment in ultrasound: The effect on student centred and inter-professional learning. Radiography, 18(3), 160–165. https://doi.org/https://doi.org/10.1016/j.radi.2012.03.003
- Hughes, M., Ventura, S., & Dando, M. (2004). On-line interprofessional learning: Introducing constructivism through enquiry-based learning and peer review. Journal of Interprofessional Care, 18(3), 263–268. https://doi.org/https://doi.org/10.1080/13561820410001731304
- IPEC, The interprofessional educational collaborative. (2016) . Core competencies for interprofessional collaborative practice: 2016 update. Interprofessional Education Collaborative Expert Panel.
- Kember, D., Ho, A., & Hong, C. (2008). The importance of establishing relevance in motivating student learning. Active Learning in Higher Education, 9(3), 249–263. https://doi.org/https://doi.org/10.1177/1469787408095849
- Kollar, I., Fischer, F., & Hesse, F. W. (2006). Collaboration Scripts – A Conceptual Analysis. Educational Psychology Review, 18(2), 159–185. https://doi.org/https://doi.org/10.1007/s10648-006-9007-2
- Kononowicz, A. A., Woodham, L. A., Edelbring, S., Stathakarou, N., Davies, D., Saxena, N., Car, L. T., Carlstedt-Duke, J., Car, J., & Zary, N. (2019). Virtual patient simulations in health professions education: systematic review and meta-analysis by the digital health education collaboration. Journal of Medical Internet Research, 21(7), e14676. https://doi.org/https://doi.org/10.2196/14676
- Lawlis, T. R., Anson, J., & Greenfield, D. (2014). Barriers and enablers that influence sustainable interprofessional education: A literature review. Journal of Interprofessional Care, 28(4), 305–310. https://doi.org/https://doi.org/10.3109/13561820.2014.895977
- Miers, M. E., Clarke, B. A., Pollard, K. C., Rickaby, C. E., Thomas, J., & Turtle, A. (2007). Online interprofessional learning: The student experience. Journal of Interprofessional Care, 21(5), 529–542. https://doi.org/https://doi.org/10.1080/13561820701585296
- Mitchell, M., Groves, M., Mitchell, C., & Batkin, J. (2010). Innovation in learning - An inter-professional approach to improving communication. Nurse Education in Practice, 10(6), 379–384. https://doi.org/https://doi.org/10.1016/j.nepr.2010.05.008
- Moon, J. (2007). Getting the measure of reflection: Considering matters of definition and depth. Journal of Radiotherapy in Practice, 6(4), 191–200. https://doi.org/https://doi.org/10.1017/S1460396907006188
- Naeger, D. M., Hua, E. W., Ahearn, B., & Webb, E. M. (2015). Reflective writing: A potential tool to improve interprofessional teamwork with radiologists. Academic Radiology, 22(10), 1221–1225. https://doi.org/https://doi.org/10.1016/j.acra.2015.07.006
- Posel, N., Mcgee, J. B., & Fleiszer, D. M. (2015). Twelve tips to support the development of clinical reasoning skills using virtual patient cases. Medical Teacher, 37(9), 813–818. https://doi.org/https://doi.org/10.3109/0142159X.2014.993951
- Potthoff, M., Doll, J., Maio, A., & Packard, K. (2020). Measuring the impact of an online IPE course on team perceptions. Journal of Interprofessional Care, 34(4), 557–560. https://doi.org/https://doi.org/10.1080/13561820.2019.1645647
- Pulman, A., Scammell, J., & Martin, M. (2009). Enabling interprofessional education: The role of technology to enhance learning. Nurse Education Today, 29(2), 232–239. https://doi.org/https://doi.org/10.1016/j.nedt.2008.08.012
- Shoemaker, M. J., De Voest, M., Booth, A., Meny, L., & Victor, J. (2015). A virtual patient educational activity to improve interprofessional competencies: A randomized trial. Journal of Interprofessional Care, 29(4), 395–397. https://doi.org/https://doi.org/10.3109/13561820.2014.984286
- Tait, G. 2019. Virtual interactive case system, VIC [Online]. Toronto General Hospital. https://pie.med.utoronto.ca/VIC/index.htm
- Thistlethwaite, J. E., Dunston, R., & Yassine, T. (2019). The times are changing: Workforce planning, new health-care models and the need for interprofessional education in Australia. J Interprof Care, 33(4), 361–368. https://doi.org/https://doi.org/10.1080/13561820.2019.1612333
- Vermunt, J. D., & Donche, V. (2017). A learning patterns perspective on student learning in higher education: State of the art and moving forward. Educational Psychology Review, 29(2), 269–299. https://doi.org/https://doi.org/10.1007/s10648-017-9414-6
- Weinstein, R. S., McNeely, R. A., Holcomb, M. J., Doppalapudi, L., Sotelo, M. J., Lopez, A. M., Erps, K. A., Martin, C. J., Krupinski, E. A., Graham, A. R., & Barker, G. P. (2010, Fall). Technologies for interprofessional education: The interprofessional education-distributed. Journal of Allied Health, 39(Suppl 1), 238–245. https://pubmed.ncbi.nlm.nih.gov/21174046/
- Wong, P. S., Chen, Y. S., & Saw, P. S. (2019, October 11). Influencing factors and processes of interprofessional professional education (IPE) implementation. Medical Teacher, 1–7. Online ahead of print. https://doi.org/https://doi.org/10.1080/0142159X.2019.1672864