Abstract
Objective: Visceral adipose index (VAI) is a novel parameter for the evaluation of visceral obesity. As we know that obesity is a risk factor for erectile dysfunction (ED). So, in this study, we compared the VAI levels between the men with ED and without ED.
Materials and method: A total of 177 men were included in the study. Ninety-five men with ED and 82 men without ED (control). All men were evaluated for ED by Index of Erectile Function-5 items (IIEF-5). VAI levels were calculated using body mass index, high density lipoprotein and tryglyceride levels.
Results: Mean age was 53.5 (38–69) in men who have ED and 53.1 (34–69) in control. The men with ED had higher body mass index (BMI), triglyceride (TG) levels, higher waist circumference (WC) and lower high-density lipoprotein-cholesterol (HDL-C) levels. Mean VAI level was 5.18 ± 2.50 in study group and 3.47 ± 1.76 in control goup, respectively. VAI levels were statistically higher in men with ED (p < .001).
Discussion: The simplicity of WC and BMI measurement and TG and HDL assessment, make VAI an easily applicable index for the evaluation of visceral fat dysfunction. VAI can be useful index for the evaluation and calculation of erectile dysfunction risk.
Introduction
Sexual dysfunction in general and erectile dysfunction (ED) in particular significantly affect men’s quality of life. Erectile dysfunction (ED), the consistent inability over at least 3 months to achieve or maintain penile erection sufficient for satisfactory sexual performance, affects nearly one in three men older than 50 years [Citation1,Citation2]. It is a multifactorial condition that is estimated to affect more than 150 million men worldwide [Citation3]. Because of its high prevalence, profound effect on quality of life, and association with diabetes mellitus and cardiovascular disease, the medical and socioeconomic consequences of ED are substantial [Citation4,Citation5]. An erection is a complex event that requires an intact arterial and venous system, normal innervation, normal hormonal factors and functioning erectile tissue (endothelium). Abnormalities in one or more of these factors can lead to ED. Well-established risk factors for ED include hypertension, hyperlipidemia, diabetes, smoking, low testosterone, alcohol and drug abuse, anemia, trauma to/surgery of the pelvis or spine, coronary arteria disease (CAD), peripheral vascular disease, Peyronie’s disease and depression [Citation6,Citation7].
Obesity is significantly associated with erectile dysfunction (ED) and this has been neither in the focus of medical practitioners nor researchers. Studies show that obese males have a 30% higher chance of developing sexual dysfunction than the people of normal weight. The relation between obesity and sexual dysfunction is not understood completely till date. Though some studies suggest that obesity is associated with low androgen levels in men with ED, researches in this direction are few and far between [Citation8]. Obesity is measured by several methods, but for practical purposes and simplicity, it is represented in clinical urology by WC or BMI [Citation9]. Body weight and adiposity are significantly associated with ED [Citation6,Citation10,Citation11]. Convergent data from the Health Professionals Follow-up Study, the National Health and Nutrition Examination Survey (NHANES) and MMAS show that compared to men with a BMI of less than 25 kg/m2 the odds of ED are higher in men with a BMI of 25 to 30 kg/m2 and even higher in men with a BMI of greater than 30 kg/m2. The risk is increased 1.5- to 3-fold. Other measures of adiposity, including the waist-to-hip ratio and abdominal circumference, are also independently associated with ED risk. Also, metabolic syndrome (MS) prevalence in patients with ED has been also evaluated in other studies, and a high prevalence of abdominal obesity has been found in these patients [Citation12–14]. A prospective study carried out in Rancho Bernardo, California, after 25 years of follow-up, demonstrated that higher BMI was associated with a significant increase in ED risk [Citation15]. Obesity-related comorbidities and metabolic syndrome contribute to the impairment of nitric oxide (NO) synthesis in vascular beds, reduce testosterone (T) plasma levels, alter endothelial function and increase dyslipidemia, all of which contribute to the pathophysiology of ED [Citation16]. In a previous study, the authors showed that, the identification of a routinely applicable indicator for the evaluation of visceral adipose function, with higher sensitivity and specificity than classical parameters (such as waist circumference (WC), BMI, and lipids), could be useful for cardiometabolic risk assessment [Citation17]. They calculate a model of adipose distribution (MOAD). To correct MOAD for fat function, TG (mmol/l) and HDL (mmol/l) levels were introduced in the formula. They used the visceral adiposity index (VAI) as this formula for cardiometabolic risk assessment. In this context, we thought that we could use the VAI for the assessment of ED. So, in this study we compared the VAI levels between the men with ED and without ED. To our knowledge the relation between ED and VAI have not been reported previously. This is the first study in English literature about in this field.
Materials and method
We performed a prospective cross-sectional study of participants who visited our hospital from April 2013 to March 2016. All men were evaluated for ED. Ninety-five men with erectile dysfunction and 82 normal men for sexual function were included in the study. The men’s ages, comorbidities, body mass indexes (BMI) and previous surgeries were determined. The men who have smoking, alcohol and drug abuse, have some drug therapy, which effect the erectile function (like androgen therapy), trauma to/surgery of the pelvis or spine, Peyronie’s disease and depression were excluded from the study.
The men’s sexual functions were evaluated by International Index of Erectile Function-5 items (IIEF-5). The IIEF-5 included five questions that were filled based on the 5-point Likert scale. The points ranged 5–25 and points below 21 indicated erectile dysfunction. Subjects were categorized based on their points into the following groups: severe erectile dysfunction (5–10), moderate erectile dysfunction (11–15), mild erectile dysfunction (16–20) and normal (25–21).
Assays for serum total and high-density lipoprotein cholesterol (HDL-C), triglyceride (TG), levels were performed in the hospital’s chemistry laboratory with autoanalyzer.
VAI was calculates for males as this formula like previous study [Citation17].
WC: waist circumference, BMI: body mass index, TG: tryglyceride, HDL: high-density lipoprotein.
Statistical analysis
The baseline characteristics of the controls and the subjects were compared using a twosample t-test or Mann–Whitney U-test for the continuous variables. Also, logistic regression models were used. All statistical tests were two-tailed, and statistical significance was defined as p < .05. All analysis were conducted using SPSS version 15.0 (SPSS Inc., Chicago, IL).
Results
A total of 177 men between the ages of 34 and 69 years were analyzed. Overall, 95 men had ED and 82 men had no ED, respectively. Mean age was 53.5 (38–69) in men who have ED and 53.1 (34–69) in control. There were no statistical difference for age. Body mass indexes (BMI) were 29.11 ± 2.87 in study group and 27.27 ± 2.97 in control group. BMI were statistically higher in study group than control group (p < .001). Comparison of the men with ED or without ED, the men with ED had higher TG levels, higher WC and lower HDL-C levels. The difference was statistically significant for all values. Also, we compared the VAI levels between groups. Mean VAI level was 5.18 ± 2.50 in study group and 3.47 ± 1.76 in control group, respectively. VAI levels were statistically higher in men with ED (p < .001) (). Characteristics of all men are shown in . Univariate and multivariate logistic regression analyses were conducted to determine the potential confounders for erectle dysfunction. Although univariate analyses revealed that BMI, WC, TG, HDL-C level and VAI were correlated with erectile dysfunction, only VAI [1.194 OR (1.110–1.305), p 1/4 0.011] was statistically significant in multivariate analysis. Logistic regression models showed that VAI is an indicator of visceral fat dysfunction independently associated with ED. Among all variables examined, only VAI independently correlated with ED.
Figure 1. Mean VAI levels in men with and without ED. VAI levels were higher in men with ED than men without ED. (p < .001). VAI: visceral adipose index; ED: erectile dysfunction.
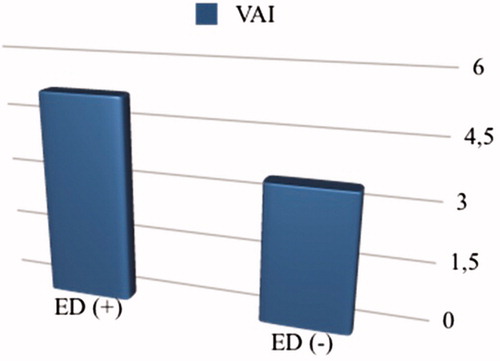
Table 1. Characteristics of men with or without ED.
Discussion
The purpose of this investigation was to examine the association between ED and adiposity in Turkish men. The main finding in this study was the significant association of VAI, a new predictor for visceral adipose distribution with ED.
Obesity induces alterations in cytokine and adipokine secretions. These proinflammatory factors contribute to endothelial dysfunction and insulin resistance, pathologies that increase the risk of ED [Citation18]. Obesity is a proinflammatory state resulting in increased release and secretion of proinflammatory cytokines and adipokines, free fatty acids and estrogens from adipose tissue. These increases are important risk factors that may contribute to the development of metabolic syndrome and type 2 diabetes as well as androgen deficiency [Citation19,Citation20]. Also, obese men may present hypogonadothrofic hypogonadism, mainly related to higher insulinemia and aromatase activity. Obese men may present relatively excess of estradiol and deficiency in testosterone, leading to an imbalance between these two hormones. The greater this imbalance, the more depressive symptoms had the patients [Citation21,Citation22]. Inversely, studies show that long-term testosterone treatment in elderly men with hypogonadism and erectile dysfunction reduces obesity parameters such as body weight, waist circumference and body mass index and improves metabolic syndrome and health-related quality of life [Citation23,Citation24]. On the other hand, as previously reported [Citation25], testosterone replacement therapy was associated with improvements in quality of life, ED and lower urinary tract symptoms.
Visceral fat is an active secretory tissue producing inflammatory cytokines, adipokines, biochemical modulators and other proinflammatory factors including interleukin (IL)-6, IL-1 b, plasminogen activator inhibitor-1, tumor necrosis factor (TNF)-a, angiotensinogen, vascular endothelial growth factor and serum amyloid A. These factors contribute to systemic and peripheral vascular inflammation and dysfunction [Citation18]. Also, aromatase, the enzyme that converts testosterone to estradiol, is mainly located in adipose tissue. Obesity is associated with elevated estrogen in men activating hypothalamic estrogen receptors triggering inhibition of the hypothalamic-pituitarygonadal axis. Treatment with aromatase inhibitors reverses the hypogonadotropic hypogonadism associated with obesity [Citation26]. Men with obesity and insulin resistance showed attenuated Leydig cell responsiveness to exogenous gonadotropin stimulation [Citation27]. Also, a previous study indicates relationships between TT and the occurrence of MetS and its individual components. Excess body weight in men is a factor associated with lower TT levels. It seems necessary to determine TT in men with MetS and overweight or obesity. Aging and obese men with tip 1 diabetes mellitus might have subnormal testosterone levels and that their glycemic control, lipid profiles and erectile function might benefit from testosterone replacement therapy [Citation28,Citation29]. The prevalence of LT increased markedly with increasing BMI and ED. So physicians should be alert to the possibility of symptoms of hypogonadism [Citation30]. On the other hand, adiponectin is an anti-inflammatory agent and is known to protect against atherosclerosis, and it has been observed that adiponectin levels are reduced in obese individuals [Citation31]. In contrast to adiponectin, leptin levels are elevated in obese individuals and it has been shown that high leptin levels contribute towards endothelial dysfunction as well as atherosclerosis [Citation32].
High BMI has been shown to associate with erectile dysfunction in previous cross-sectional and prospective studies [Citation33,Citation34], and WC has been shown to be a better predictor of erectile dysfunction than BMI [Citation35,Citation36]. These findings are particularly important because the prevalence of obesity indicated by high BMI, which is equally matched by that of large WC, continues to rise worldwide, consuming some 10% of health care resources [Citation37,Citation38]. WC is a major clinical parameter used for the indirect evaluation of increased visceral fat [Citation39]. In a previous study, a higher BMI and obesity prevalence in patients with ED in comparison with subjects with normal erectile function. WC was significantly higher in patients with ED in comparison with the control group [Citation40]. Also, in a previous study, Esposito et al. reported that weight loss in obese patients with ED improves sexual function and is associated with a lower concentration of endothelial dysfunction markers [Citation41]. Nevertheless, WC alone does not help in distinguishing between subcutaneous and visceral fat mass. Because of that, in the previous study authors identified an index that could be used as a surrogate marker of “adipose tissue dysfunction.” VAI was significantly correlated with all metabolic syndrome factors and cardio- and cerebrovascular events [Citation17]. The previous study showed that interestingly, VAI was independently associated with cardiovascular events. These findings might be explained by the fact that VAI includes both physical and metabolic parameters, perhaps indirectly reflecting other nonclassical risk factors, such as altered production of adipocytokines, increased lipolysis and plasma-free fatty acids, which are not signified by BMI, WC, TGs and HDL separately. Therefore, VAI might be a valuable index of both fat distribution and function. So, in our study, we evaluated the relationship between visceral obesity and ED, which previously described, using VAI levels of the men. This is the first study demonstrated the relation ED and VAI which shown the increased visceral fat. Mean VAI level was 5.18 ± 2.50 in study group and 3.47 ± 1.76 in control group, respectively. VAI levels were statistically higher in men with ED (p < .001).
A component of VAI, hypertriglyceridemia and the increase of small and dense low-density lipoprotein cholesterol particles contribute to vascular damage and trigger an inflammatory response, resulting in monocyte adhesion to the endothelial cells. The increased flow of free glucose and fatty acids to the vascular smooth muscle cells and to the surrounding inflammatory cells stimulates an excessive formation of reactive oxygen and nitrogen species. Subsequently, the increase in free radicals in the mitochondria impairs NO production. So, NO impairment effects erectile dysfunction. The components of VAI formula are affected the sexual function in men when they were evaluated separately. Because of that, VAI reveals the effects of WC, HDL and trylgiceride more clearly. Similarly, in a previous study, Lemieux et al. tested, in two independent study samples, the ability of simple and inexpensive tools to screen for high-risk patients [Citation42]. It is suggested that the simultaneous interpretation of waist girth and fasting TG levels may contribute to a better identification of individuals characterized by the simultaneous presence of hyperinsulinemia, hyperapo B and the small, dense LDL phenotype who are at increased risk of coronary heart disease. So, in this study, hypertriglyceridemic waist phenotype was described like VAI. But, only the waist circumference and triglycerides are present in this study. In addition to this value, there are HDL cholesterol and BMI in VAI formula. As we know, high BMI has been shown to associate with erectile dysfunction in previous cross-sectional and prospective studies. Also, elevated high-density lipoprotein cholesterol levels in the blood (HDL-C) represent one of the strongest epidemiological surrogates for protection against coronary heart disease, endothelial dysfunction and in addition ED. So, VAI reveals the effects of WC, BMI, HDL and trylgiceride more clearly. As a result, VAI appears to be superior to hypertriglyceridemic waist phenotype.
In conclusion, the simplicity of WC and BMI measurement and TG and HDL assessment, make VAI an easily applicable index for the evaluation of visceral fat dysfunction. ED is thought to be a warning sign for vascular disease, and a potential marker for atherosclerosis, endothelial dysfunction and cardiovascular disease. In this context, VAI can be an useful index for the evaluation and calculation of ED risk which was used for cardiometabolic risk.
Disclosure statement
We have no conflict of interest.
References
- Montorsi F, Adaikan G, Becher E, et al. Summary of the recommendations on sexual dysfunctions in men. J Sex Med. 2010;7:3572–3588.
- Fisher WA, Eardley I, McCabe M, et al. Erectile dysfunction (ED) is a shared sexual concern of couples I: couple conceptions of ED. J Sex Med. 2009;6:2746–2760.
- Ayta IA, McKinlay JB, Krane RJ. The likely worldwide increase in erectile dysfunction between 1995 and 2025 and some possible policy consequences. BJU Int. 1999;84:50–56.
- Seftel AD, Sun P, Swindle R. The prevalence of hypertension, hyperlipidemia, diabetes mellitus and depression in men with erectile dysfunction. J Urol. 2004;171:2341–2345.
- Dong JY, Zhang YH, Qin LQ. Erectile dysfunction and risk of cardiovascular disease: meta-analysis of prospective cohort studies. J Am Coll Cardiol. 2011;58:1378–1385.
- Johannes CB, Araujo AB, Feldman HA, et al. Incidence of erectile dysfunction in men 40 to 69 years old: longitudinal results from the Massachusetts male aging study. J Urol. 2000;163:460–463.
- Panach-Navarrete J, Martínez-Jabaloyas JM, DE-SDT Study Group. The influence of comorbidities on the aging males' symptoms scale in patients with erectile dysfunction. Aging Male. 2017;20:146–152.
- Corona G, Mannucci E, Fisher AD, et al. Low levels of androgens in men with erectile dysfunction and obesity. J Sex Med. 2008;5:2454–2463.
- Lee RK, Chung D, Chughtai B, et al. Central obesity as measured by waist circumference is predictive of severity of lower urinary tract symptoms. BJU Int. 2012;110:540–545.
- Saigal CS, Wessells H, Pace J, et al. Predictors and prevalence of erectile dysfunction in a racially diverse population. Arch Intern Med. 2006;166:207.
- Bacon CG, Hu FB, Giovannucci E, et al. Association of type and duration of diabetes with erectile dysfunction in a large cohort of men. Diabetes Care. 2002;25:1458.
- Corona G, Mannucci E, Petrone L, et al. A comparison of NCEPATPIII and IDF metabolic syndrome definitions with relation to metabolic syndrome-associated sexual dysfunction. J Sex Med. 2007;4:789–796.
- Traish AM, Guay A, Feeley R, et al. The dark side of testosterone deficiency, I: metabolic syndrome and erectile dysfunction. J Androl. 2009;30:10–22.
- Demir O, Akgul K, Akar Z, et al. Association between severity of lower urinary tract symptoms, erectile dysfunction and metabolic syndrome. Aging Male. 2009;12:29–34.
- Fung MM, Bettencourt R, Barrett-Connor E. Heart disease risk factors predict erectile dysfunction 25 years later: the Rancho Bernardo Study. J Am Coll Cardiol. 2004;43:1405–1411.
- Blaya R, Thomaz LD, Guilhermano F, et al. Total testosterone levels are correlated to metabolic syndrome components. Aging Male. 2016;19:85–89.
- Amato MC, Giordano C, Galia M, et al. Visceral Adiposity Index: a reliable indicator of visceral fat function associated with cardiometabolic risk. Diabetes Care. 2010;33:920–922.
- Guzik TJ, Mangalat D, Korbut R. Adipocytokines - novel link between inflammation and vascular function? J Physiol Pharmacol. 2006;57:505–528.
- Goh VH, Hart WG. Association of general and abdominal obesity with age, endocrine and metabolic factors in Asian men. Aging Male. 2016;19:27–33.
- Traish AM, Feeley RJ, Guay A. Mechanisms of obesity and related pathologies: androgen deficiency and endothelial dysfunction may be the link between obesity and erectile dysfunction. Febs J. 2009;276:5755–5767.
- Monteagudo PT, Falcão AA, Verreschi IT, et al. The imbalance of sex-hormones related to depressive symptoms in obese men. Aging Male. 2016;19:20–26.
- Cao J, Chen TM, Hao WJ, et al. Correlation between sex hormone levels and obesity in the elderly male. Aging Male. 2012;15:85–89.
- Yassin DJ, Doros G, Hammerer PG, et al. Long-term testosterone treatment in elderly men with hypogonadism and erectile dysfunction reduces obesity parameters and improves metabolic syndrome and health-related quality of life. J Sex Med. 2014;11:1567–1576.
- Salman M, Yassin DJ, Shoukfeh H, et al. Early weight loss predicts the reduction of obesity in men with erectile dysfunction and hypogonadism undergoing long-term testosterone replacement therapy. Aging Male. 2017;20:45–48.
- Yassin A, Nettleship JE, Talib RA, et al. Effects of testosterone replacement therapy withdrawal and re-treatment in hypogonadal elderly men upon obesity, voiding function and prostate safety parameters. Aging Male. 2016;19:64–69.
- Loves S, Ruinemans-Koerts J, de Boer H. Letrozole once a week normalizes serum testosterone in obesity-related male hypogonadism. Eur J Endocrinol. 2008;158:741–747.
- Pitteloud N, Hardin M, Dwyer AA, et al. Increasing insulin resistance is associated with a decrease in Leydig cell testosterone secretion in men. J Clin Endocrinol Metab. 2005;90:2636–2641.
- Rotter I, Kosik-Bogacka D, Dołęgowska B, et al. Analysis of relationships between the concentrations of total testosterone and dehydroepiandrosterone sulfate and the occurrence of selected metabolic disorders in aging men. Aging Male. 2015;18:249–255.
- Saad F, Yassin A, Almehmadi Y, et al. Effects of long-term testosterone replacement therapy, with a temporary intermission, on glycemic control of nine hypogonadal men with type 1 diabetes mellitus - a series of case reports. Aging Male. 2015;18:164–168.
- Kaplan SA, Lee JY, O'Neill EA, et al. Prevalence of low testosterone and its relationship to body mass index in older men with lower urinary tract symptoms associated with benign prostatic hyperplasia. Aging Male. 2013;16:169–172.
- Kadowaki T, Yamauchi T. Adiponectin and adiponectin receptors. Endocr Rev. 2005;26:439–451.
- Correla ML, Rahmouni K. Role of leptin in the cardiovascular and endocrine complications of metabolic syndrome. Diabetes Obes Metab. 2006;8:603–610.
- Larsen SH, Wagner G, Heitmann BL. Sexual function and obesity. Int J Obes (Lond). 2007;31: 1189–1198.
- Bacon CG, Mittleman MA, Kawachi I, et al. A prospective study of risk factors for erectile dysfunction. J Urol. 2006;176:217–221.
- Janiszewski PM, Janssen I, Ross R. Abdominal obesity and physical inactivity are associated with erectile dysfunction independent of body mass index. J Sex Med. 2009;6:1990–1998.
- Riedner CE, Rhoden EL, Ribeiro EP, et al. Central obesity is an independent predictor of erectile dysfunction in older men. J Urol. 2006;176:1519–1523.
- Okosun IS, Chandra KM, Boev A, et al. Abdominal adiposity in U.S. adults: prevalence and trends, 1960-2000. Prev Med. 2004;39:197–206.
- Li C, Ford ES, McGuire LC, et al. Increasing trends in waist circumference and abdominal obesity among US adults. Obesity (Silver Spring). 2007;15:216–224.
- Mathieu P, Pibarot P, Larose E, et al. Visceral obesity and the heart. Int J Biochem Cell Biol. 2008;40:821–836.
- Costanzo P, Knoblovits P, Valzacchi GR, et al. Erectile dysfunction is associated with a high prevalence of obesity and metabolic syndrome. Rev Argent Endocrinol Metab. 2008;45:142–148.
- Esposito K, Giugliano F, Palo CD, et al. Effect of lifestyle changes on erectile dysfunction in obese men: a randomized controlled trial. JAMA. 2004;291:2978–2984.
- Lemieux I, Pascot A, Cuouillard C, et al. Hypertriglyceridemic waist: a marker of the atherogenic metabolic triad (hyperinsulinemia; hyperapolipoprotein B; small, dense LDL) in men? Circulation. 2000;102:179–184.

