Abstract
Aim
To longitudinally investigate speech production (consonant proficiency, consonant errors and perceived velopharyngeal competence) in 17 internationally adopted (IA) children with unilateral cleft lip and palate (UCLP) at three time points.
Method
Consonant proficiency (percent consonants correct, consonant inventory) and number and type of consonant errors were calculated based on blind phonetic transcriptions of words from the Swedish Test of Articulation and Nasality (SVANTE). Velopharyngeal competence was perceptually rated by three blinded experienced speech-language pathologists at the ages of 3, 5 and 7–8 years.
Results
A significant positive development of speech production was found, although most children still scored very low for consonant proficiency at the age of 7–8 compared with normative values: the median for percent consonants correct was 79.7 and many children still had persisting cleft-related and developmental consonant errors. At the age of 7–8, almost half of the children were rated as having a competent velopharyngeal function and only three as having an incompetent velopharyngeal function.
Conclusion
Persisting speech difficulties at school age in IA children with UCLP were found in the present study, which is one of the very few longitudinal studies. Our results highlight the need for detailed follow-up of speech production in clinical settings. Speech disorders may have a severe impact on a child’s intelligibility and participation with peers, and there is a need for more studies investigating the actual everyday effect of the difficulties found.
Introduction
For purposes such as taking part in everyday communication, playing and socializing with peers, and expressing one’s thoughts properly, all children need to communicate effectively. Although communication by definition involves several persons, having a speech disorder may severely affect how someone communicates and interacts with peers. For school-aged children, the risk of failing to interact with peers, being misinterpreted and of suffering social exclusion may be higher for those whose speech intelligibility is reduced owing to a speech disorder [Citation1].
Existing research into internationally adopted (IA) children with cleft lip and palate (CLP) has found a high prevalence of speech disorders with articulation difficulties and velopharyngeal (VP) incompetence [Citation2–6]. VP incompetence, including hypernasality, nasal emissions and weak pressure consonants, is a common area of weakness in the speech of children with CLP [Citation7] and may have a considerable effect on articulation, speech intelligibility and quality of life [Citation8,Citation9] – not least as a result of potential negative reactions from peers [Citation10,Citation11]. For this reason, children with VP incompetence may need secondary palatal surgery to improve their speech; a higher frequency of secondary palatal surgery has indeed been described among IA children with CLP [Citation4,Citation5,Citation12,Citation13]. In the present study, the term VP incompetence is used to define an insufficient VP function. This is in line with the ICHOM standard for outcome measures in cleft care [Citation14] and with the method used in the present study to assess articulation and VP function [Citation15].
Poor articulation proficiency with low percent consonants correct (PCC) scores relative to non-adopted (NA) children with CLP has been found in 3- and 5-year-old IA children with unilateral CLP [Citation2,Citation3]. By contrast, Sahlsten Schölin et al. [Citation5] did not find any articulation differences between IA and NA children with CLP at 5 years of age. However, they found a higher frequency of VP incompetence at 5 years of age among their IA children with CLP than among their NA children with CLP, and 28% of their IA children had undergone secondary palatal surgery prior to speech assessment, while only 4% of their NA children had undergone any secondary palatal surgical procedures.
Apart from speech disorders, researchers have highlighted a higher risk of language delay in IA children with CLP than in NA children with CLP [Citation6,Citation16]. However, a recent study found no significant differences in language ability between IA children with CLP and IA children without CLP at 7–8 years of age [Citation17]. Interestingly, the only area where a significant difference was found in that study between the IA children with and without CLP was speech production measured using PCC, where the IA children with CLP presented with low PCC scores. This poor performance in speech ability found in Larsson et al. [Citation17] was in line with earlier findings by Morgan et al. [Citation4], who studied 21 IA children with CLP at age 7–8 years and assessed about 70% of them as having an articulation impairment, also finding that many children still had cleft-related articulation errors at that age. Additionally, Morgan et al. [Citation4] also found a high prevalence of developmental speech characteristics (DSCs) in IA children with CLP compared with NA children with CLP, highlighting the possible risk of phonological mislearning in IA children with CLP. Further, Morgan et al. [Citation4] found an association between the time of achieving a sufficient VP closure and articulation proficiency: the longer a child had had a sufficient VP closure, the better his or her articulation proficiency was.
Longitudinal studies of speech ability in IA children with CLP can make important contributions to our understanding of the course of their speech development and its impact on their lives, but there are few such studies. Previous research into IA children with CLP mostly involves cross-sectional studies of mainly pre-school children and there are generally few studies of this group of children. Although international adoptions of children to Europe are in fact decreasing [Citation18], which may seem to reduce the need for such research, detailed longitudinal descriptions of speech production in IA children with CLP may also contribute to the broader knowledge base on speech development in children with the late palatal repair.
The purpose of the present study was to longitudinally investigate speech-production development in IA children with unilateral CLP (UCLP). The children were assessed at three time points: at the ages of 3 (T1), 5 (T2) and 7–8 (T3) years. It was hypothesized that PCC, consonant inventory and perceived velopharyngeal competence would increase with age. Further, it was hypothesized that consonant errors would decrease with age.
Materials and methods
Participants
Seventeen children (four girls and thirteen boys) were included in the present study. At the start, all 32 IA children with UCLP born in China in 2006–2009 who were enrolled in the routine cleft-care programme at a Swedish CLP centre were invited to participate. Written informed consent to participate at all three-time points was obtained from the parents of seventeen children (four girls and thirteen boys). The study was approved by the Regional Ethical Review Board of Gothenburg, Sweden (case No. 865-13). Background information, including age at adoption, the highest level of education in the (adoptive) family and speech and language status before adoption, was collected from the parents at the time of the assessment at the age of 7–8 years. The children had been adopted to Sweden at a median age of 20 months (range: 16–33). At the time of the assessments, no child was bilingual, had a severe hearing impairment or had a known developmental disability. The children’s median number of visits to a speech-language pathologist (SLP) between the ages of 3 years (T1) and 5 years (T2) was 9 (minimum–maximum 2–19), that between T2 and the age of 7–8 years (T3) was 4 (minimum–maximum 0–21), and that between T1 and T3 was 15 (minimum–maximum 3–37). Information on the type of speech interventions could not be retrieved since all children were treated by several different local SLPs from a large geographical area.
This study was part of a larger project studying speech and language skills in IA children with UCLP. Data from nine of the children in the present study were included in a previous cross-sectional study performed at the age of 3 years [Citation3]. All 17 children in the present study were included in two other studies performed at the age of 5 years [Citation2] and at the age of 7–8 years [Citation17].
Of the seventeen participants, ten had undergone surgical interventions in China prior to their adoption: seven had undergone lip repair and three had undergone lip repair and palatoplasty. In Sweden, all children were treated in accordance with the Gothenburg protocol for surgical interventions [Citation19] and given the treatment they needed as soon as possible after the adoption. Their median age at soft-palate closure in Sweden was 25 months (range: 19–42). Hard-palate closure was performed at a median age of 35 months (range: 27–55).
Secondary velopharyngeal (SVP) surgery was performed with soft-palate re-repair using intravelar veloplasty or palatopharyngeal flap. Four children underwent secondary soft-palate re-repair prior to T2, of whom two underwent additional palatopharyngeal-flap surgery between T2 and T3. Another two children underwent soft-palate re-repair between T2 and T3, one of whom also underwent palatopharyngeal-flap surgery twice. Of the six children who underwent SVP surgery, three also underwent palatal-fistula repair prior to T2. Another child underwent secondary-fistula repair in the hard palate twice (once prior to T2 and once between T2 and T3). Another three children underwent palatal-fistula repair between T2 and T3, of whom one did so twice. Finally, three children underwent alveolar-cleft surgery with a bone transplant prior to T3.
Audiometry screenings performed at the ages of 3 (T1), 5 (T2) and 7–8 (T3) years using pure-tone averages (PTAs) calculated for the frequencies of 500, 1000, 2000 and 4000 Hz showed median PTAs of 21 dB/22 dB (left/right) at T1, 20 dB/20 dB at T2 and 20 dB/20 dB at T3. Data were missing for one child at T1 and for another child at T3. The audiometry screenings were generally performed within 1 month of T1, within 2 months of T2 and within 9 months of T3, although one child’s third audiometry screening took place 17 months before T3. includes full information about the individual participants, including background variables and test scores.
Table 1. Individual data on all 17 participants at different timepoints.
Procedure
The material analysed for the present study consists of data and speech recordings from standardized speech assessments performed by the cleft-team SLPs at the CLP centre at the ages of 3 years (T1 – median age: 38 months, range: 35–46) and at the age of 5 years (T2 – median age: 60 months, range: 58–64) as well as from a speech assessment performed by the first author in a quiet room at a place chosen by the parents (usually at home or at the hospital) at the age of 7–8 years (T3 – median age: 88 months, range: 84–103). At T1, data were missing for four children: the audio recordings were missing for two children while two others had too little speech (very few words) for an assessment using the articulation test. All audio recordings were performed using a portable digital stereo audio recorder (Tascam Hdp2, Teac Corporation) and a microphone (Ecm-ms 957, Sony Corporation). The microphone was placed at a distance of approximately 40 cm from the child.
Speech measures: analyses and reliability
To assess speech production at T1, T2 and T3, the Swedish Articulation and Nasality Test (SVANTE) [Citation15] were used. This is a norm-referenced picture-naming test encompassing 59 words enabling the assessment of a child’s consonant proficiency, consonant errors, consonant inventory and nasality. Each of the 59 words includes one target consonant vulnerable to structural deficits. The target consonants included in the SVANTE are /p b t d k g f s/, which are all represented three times in the word-initial position, twice in the medial position and twice in the word-final position. The SVANTE also includes /ɕ/ three times word-initially as well as additional words for assessing the nasals /m n ŋ/ and /v j ɧ h r l/. Hence the full Swedish consonant inventory of 18 consonant phonemes could be assessed. The SVANTE also includes 13 sentences where high- and low-pressure consonants and nasals occur together. In the present study, those sentences were used as speech material to assess perceived VP competence at T2 and T3.
All recordings of speech elicited by the SVANTE were edited in the free software PRAAT [Citation20] into one separate .wav file for each word, which was then gathered in one data folder per child. Hence there were a maximum of 59 .wav files – one for each word/target consonant – per child. After editing, semi-narrow phonetic transcriptions of the target consonants in each word were performed using the IPA alphabet [Citation21] and Ext IPA [Citation22]. Only the following diacritics were used: [ ͋ ] for nasal emission, [ ͌ ] for velopharyngeal friction and [ ͉ ] for weak articulation; in addition, the symbol [ n͋˳] for the non-oral active nasal fricative was used. At all timepoints, there was one master transcriber (an experienced SLP) who phonetically transcribed all speech material.
Based on the phonetic transcriptions, the variable of percent consonants correct (PCC) was calculated by dividing the number of correctly produced target consonants by the total number of target consonants and then multiplying the quotient by 100 [Citation23]. Further, the number of established consonant phonemes (consonant inventory) was determined for each time point using the phonetic transcriptions; a consonant was considered established in a child’s speech if it occurred in at least half of the possible instances [Citation15].
To study perceived velopharyngeal competence (VPC), speech material from the SVANTE recordings was used. At T1, samples of connected speech from the assessment were used. At this time point, spontaneous utterances (at least two-word utterances or spontaneous counting during play) were used. At T2 and T3, recordings of the 12 SVANTE sentences were used. The SVANTE sentences include target consonants typically vulnerable to structural deficits. These include high- and low-pressure consonants and nasal consonants in combination with plosive consonants [Citation15]. For each child, there was one .wav file for each timepoint intended for perceptual analysis of VPC. For agreement calculations, 30% of the .wav files were doubled. All .wav files were coded and presented in random order.
An overall perceptual judgement of VPC (VPC-Rate) was performed by three experienced SLPs. The judges could listen to each file as many times as they wished and used a three-point ordinal scale including competent (0), marginally incompetent (1) and incompetent (2) VP (velopharyngeal) function. VP function was considered to be marginally incompetent when there was evidence of minor problems suggesting borderline VP closure not requiring surgery, and incompetent when there was clear evidence of problems with VP closure that would require surgical intervention [Citation24]. The rating chosen by the majority of the three judges for each child yielded that child’s VPC-Rate value. VPC-Rate has been proven to be a valid measure for assessing perceived VP function in clinical research [Citation24].
Further, the phonetic transcriptions were used to determine the frequency of four categories of consonant errors – (1) non-oral articulation, (2) retracted oral articulation, (3) deletion of target consonant and (4) developmental speech characteristic – by calculating the proportion of target consonants replaced by each error type.
Glottal plosives or fricatives, glottal reinforcements and active nasal fricatives as well as cases where an unvoiced stop or fricative target consonant was replaced by a nasal consonant were all counted as non-oral articulation. Cases, where a target consonant with an anterior place of articulation was replaced with a consonant with a palatal/velar/uvular place of articulation, were categorized as retracted oral articulation. The third category, deletion of target consonant, was frequent in our speech material. Since deletions of target consonants can be considered either as related to the cleft (as seen in Willadsen et al. [Citation25], and in Larsson et al. [Citation2]) or as a consequence of a developmental speech disorder [Citation26], we have chosen to report them as a separate category [Citation27]. Finally, the types of developmental speech characteristics found in the present material were the following: velar fronting (replacement of a velar place of articulation with a dental/alveolodental one), stopping (change of manner of articulation into a plosive), approximation (change of manner of articulation into an approximant) and voicing issues (difficulties differentiating between voiced and voiceless consonants).
Inter- and intra-transcriber agreement for the phonetic transcriptions was calculated as the percentage of agreement, point by point. For all time points, 30% of the speech files were doubled and re-transcribed approximately four months after the first transcriptions. For inter-transcriber agreement, a second SLP transcribed the same speech files. The agreement had to be reached with respect to the manner of articulation and with respect to one of four categories of the place of articulation: (1) bilabial-labiodental, (2) interdental-dental-alveolar-postalveolar-retroflex, (3) palatal-velar-uvular and (4) glottal. Additionally, the agreement had to be reached with respect to the presence or absence of symptoms of incompetent VP function (audible nasal air leakage, weak pressure consonants and nasal realisations of oral voiced consonants). All outcomes were calculated as median inter- and intra-transcriber agreement.
At T1, the rates of inter-transcriber agreement for place and manner of articulation were 81% and 91%, respectively, while the corresponding values for the intra-transcriber agreement were 93% and 97%. The rates of inter-transcriber agreement for non-oral articulation and symptoms of incompetent VP function at T1 were 96.5% and 91%, respectively, while the rates of the intra-transcriber agreement were 99% and 97.5%. At T2, inter- and intra-transcriber agreement for place and manner of articulation was 82%/96% and 93%/98%, respectively. For non-oral articulation and symptoms of incompetent VP function, the rates of the inter-transcriber agreement were 89% and 77%, while the rates of the intra-transcriber agreement were 98% and 87%. At T3, the corresponding figures for inter- and intra-transcriber agreement for place and manner of articulation were 85%/97% and 91%/98%. For non-oral articulation, the corresponding figures were 92% and 97%, while the figures for symptoms of incompetent VP function were 66% and 83%.
Intra-rater agreement for the perceptual assessment of overall VP competence – calculated point by point and reported as the percentage of agreement – was 64.3%, 92.9% and 100%, respectively, for the three raters. Inter-rater agreement was measured as the frequency of (1) agreement between all three raters (64.3%), (2) agreement between two of the raters (35.7%) and (3) no agreement between any of the raters (0%).
Statistics
All statistical calculations were carried out using the Statistical Package for Social Sciences [Citation28]. Since the sample size was small and it was not expected that the data would be normally distributed, non-parametric statistical tests were performed as part of the analysis of the speech variables: the Wilcoxon signed-rank test was used to calculate differences in speech-production variables between T1 and T2 and between T2 and T3. The level of statistical significance was set to p < .05 (two-tailed).
Results
Speech production
Speech production, measured using PCC scores and consonant inventory, increased with age, as expected (). Significant differences in PCC scores were seen both between T1 and T2 (Z = −3.18, p = .001) and between T2 and T3 (Z = −3.62, p < .001). However, the group scored below the age-specific norms at all time points. The median PCC score was 15.8 at T1, 60 at T2 and 79.7 at T3. At T1, eleven of thirteen children (85%) (data were missing for four children) had PCC scores more than 2 SD below the age-specific norm [Citation15] while this was the case for sixteen out of seventeen children (94%) at T2 and T3.
Figure 1. Percent consonants correct (PCC) at the three-time points (T1–T3). The solid black line represents norm values for 3-, 5- and 7-year-old Swedish children without cleft lip and palate [Citation15].
![Figure 1. Percent consonants correct (PCC) at the three-time points (T1–T3). The solid black line represents norm values for 3-, 5- and 7-year-old Swedish children without cleft lip and palate [Citation15].](/cms/asset/d81fce65-7c82-4ad9-8eea-d8f1f0270928/ilog_a_2083673_f0001_b.jpg)
Figure 2. Development of the median PCC score for each participant between T1 and T3. The red dotted line represents the age-specific norms for 3-, 5- and 7-year-old children [Citation15].
![Figure 2. Development of the median PCC score for each participant between T1 and T3. The red dotted line represents the age-specific norms for 3-, 5- and 7-year-old children [Citation15].](/cms/asset/471d9225-cb15-4d18-bb3b-290159a131d9/ilog_a_2083673_f0002_c.jpg)
Figure 3. Mean consonant inventory at the three timepoints (T1–T3).
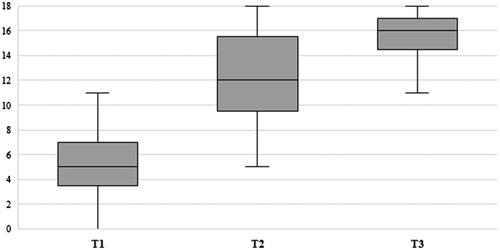
The children’s mean consonant inventory at T1 was 5.4 (SD = 2.73). At T2 and T3, it was 12.2 (SD = 3.5) and 15.7 (SD = 1.8), respectively. A significant difference in consonant inventory was found both between T1 and T2 (Z = −3.12, p < .01) and between T2 and T3 (Z = −3.19, p = .001).
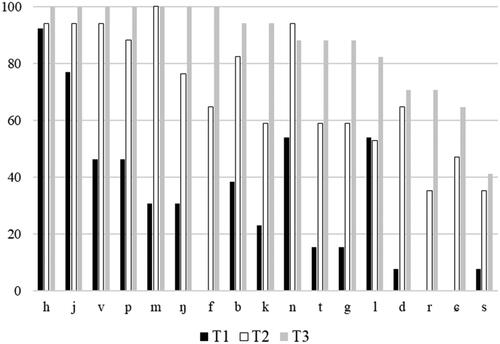
As is clear from these results, even at T3 there were consonants which were not yet established in the inventories of most children. shows the percentages of children having established each consonant at T1, T2 and T3.
Figure 4. Percentage of children having established each consonant phoneme at T1, T2 and T3 (since the/ɧ/phoneme was not elicited for six and five children at T1 and T2, respectively, it is not included).
Consonant errors
The frequency of non-oral articulation, deletion of target consonants and developmental speech characteristics decreased substantially with age (). Despite wide variation in frequency, thirteen of the seventeen children (77%) still exhibited developmental speech characteristics to some extent at T3. Of those thirteen, all but one child had difficulties with voicing. Further, two of those thirteen had fronting, and one had stopped, alongside voicing difficulties. Retracted oral articulation did not decrease with age () and all but two children (88%) had instances of retracted oral articulation at T3.
Table 2. Frequency of consonant errors (percentage of instances across the material) at different timepoints, presented as median (minimum-maximum) values.
Perceived VP competence
At the group level, VP competence improved from T1 to T3 (). The difference in median VPC-Rate for the whole group was significant both between T1 and T2 (Z = −2.00, p < .05) and between T2 and T3 (Z = −2.64, p < .01). At T3, seven of the seventeen children (41%) were rated as having a competent VP function, while three (18%) had an incompetent VP function.
Table 3. Number and percentage of children with different velopharyngeal-competence rates at each timepoint.
Discussion
Although the children in the present study made impressive progress in their speech development from the age of 3 years, they still had persistent speech difficulties at the age of 7–8 years. In most cases, they were far from the levels expected at that age.
The children made significant progress at the group level in terms of all speech-production variables studied: their PCC scores, consonant inventory and VPC-Rate all improved greatly from the age of 3 years to the age of 7–8 years. Further, the prevalence of speech errors decreased substantially with age for three of the four speech-error types: non-oral articulation, deletion of target consonant and developmental speech characteristics. Factors that may have contributed to this positive development include age, time after primary surgery, secondary VP surgery and speech-therapy interventions. Six children had received secondary VP surgery prior to T3 and most had received speech-therapy interventions before the age of 7–8. However, disentangling the effect, if any, of each such factor is beyond the scope of this study.
Even so, despite such major speech improvements from the age of 3 to the age of 7–8, only one of the seventeen children had an age-appropriate PCC (98.3%) at the age of 7–8 while all the others presented with results more than 2 SD below the age-specific norm. In fact, children aged 7–8 usually obtain PCC values of almost 100%, while the present IA group lagged behind at a median PCC of 79.7%. A PCC score of around 80% corresponds to the typical score of 5-year-old non-adopted (NA) children with UCLP [Citation25]. The PCC scores obtained at T3 by most participants in the present study are 4 SD or more below the typical scores of 7-year-old NA children without CLP [Citation15].
In the norms of the Swedish phonology test LINUS [Citation29], which was based on 495 children aged 3–6 years, all 18 consonant phonemes except /s/ were established at the age of 6 years. By contrast, some of the present children had quite small consonant inventories even at the age of 7–8; the mean consonant inventory of the group at T3 was 15.7 (SD 1.8).
One unexpected finding was that one speech-error type – retracted oral articulation – did not decrease with age. Previous studies have found this error type to be common in NA children with CLP as well [Citation25], especially in those with delayed hard-palate repair [Citation30]. At T3, 12% of the present group’s target consonants were affected by retracted oral articulation, while this was the case for only 6.8% of target consonants at T2. In addition, this was a widespread phenomenon: all but two children (i.e. 88%) manifested retracted oral articulation at T3. However, it should be noted that most of the target consonants which were orally retracted at T3 (mostly fricatives but also plosives) were missing at T2, usually owing to deletion or non-oral (i.e. glottal) articulation. In fact, all children whose prevalence of retracted oral articulation increased from T2 to T3 also had a high prevalence at T2 of deletion and glottal articulation as well as frequent symptoms of VP insufficiency, and those factors may have ‘masked’ (or limited opportunities for) retracted oral articulation at T2. A possible explanation for the high prevalence of retracted oral articulation at T3 could be that most children then still had a residual alveolar cleft which may have influenced the place of articulation.
It is interesting to note that all children had had some sort of speech therapy prior to T3, although the number of ‘speech visits’ varied greatly within this small group. Unfortunately, we do not have any information about what kind of speech therapy had been given to our participants. An important implication for future studies is to include more information regarding speech therapy, but most importantly there is a need for research examining treatment effects.
If all cleft-related consonant errors (i.e. non-oral articulation and retracted oral articulation) are combined into a single category, as they were in the study by Morgan et al. [Citation4], all children except one (i.e. 94%) in our study produced some kind of cleft-related consonant errors at the age of 7–8 years. This proportion is far higher than that found by Morgan et al. [Citation4], who reported that just over 50% of their IA children had ‘cleft-related errors’ at the age of 7–8, including several different types of errors: backing to a palatal place of articulation, backing to a velar place of articulation, backing to glottal and pharyngeal place of articulation and nasal substitution of oral pressure consonants. However, it should be noted that three children in the present study stand out from the rest of those who produced consonant errors in that only 1.7%, 1.7% and 5.1%, respectively, of their target consonants, were affected by cleft-related consonant errors. One of those children had had complete palatal surgery performed in China and was rated at all time points as having a competent VP function. The other two had had all palatal surgical treatment performed in Sweden. One of them was rated as having a competent VP function at T2 and T3 (data were missing at T1). The third child was rated with incompetent VP function at T1 and marginally incompetent at T3. None of those three children had had any secondary VP surgery prior to T3.
The prevalence of developmental speech characteristics (DSCs) decreased from the age of 3 years to the age of 7–8 years, but even so all but four of the children (i.e. 77%) still had DSCs at T3, at varying frequencies. In the study by Morgan et al. [Citation4], 19% of 7–8-year-old IA children with CLP were found to have a speech impairment defined as ‘developmental impairment only’, as against 10% of the NA/CLP group in the same study. Further, 48% of the IA children but only 5% of the NA children manifested difficulties defined as a combined articulation impairment involving both cleft-related errors and developmental errors. Although the variation in the frequency of consonant errors was very wide in the present study, 13 of the 17 children (i.e. 77%) had a combination of cleft-speech consonant errors and DSCs.
In the present sample, the most common DSC at T3 was voicing difficulties. Of the children manifesting DSCs at T3, all but four had voicing error as their sole DSC; the other four had approximation only (n = 1) or voicing difficulties in combination with fronting (n = 2) or stopping (n = 1). Difficulty differentiating between voiced and voiceless consonants is traditionally seen as a developmental phonological pattern typical of young children’s phonological development [Citation31]. This pattern usually disappears around the age of 3 years in Swedish children; at the age of 7–8 years, NA children without CLP typically have no DSCs at all [Citation15]. However, it should be noted that all children in the present study were born in China. Interestingly, the most common language spoken there, Putonghua (standard Mandarin), lacks the distinctive phonological feature of voicing (voiced–unvoiced plosives) [Citation32]. Although we have no information about the native languages of the children in the present study, it is likely that they spent their first years in a Putonghua-speaking environment. This may have exerted an influence on their early phonological learning and there are studies questioning whether the birth language of internationally adopted children is fully ‘lost’ post-adoption [Citation33]. The children in the present study were adopted to Sweden at a median age of 20 months and no child lived in a multilingual environment. This means that many children had limited exposure to Swedish at the time of their first speech assessment (T1, median age: 38 months, range 16–33). However, at T3 the children had a median exposure time of 66 months (range 57–84). Longitudinal follow-ups on speech and language development in internationally adopted children without CLP have found articulation proficiency to be the speech and language skill most easy to acquire regardless of adoption age and exposure time [Citation34]. Thus, it seems unlikely, that the speech errors found at T3 in our study could be explained by age at adoption or exposure time but may instead be a consequence of the CLP. Morgan et al. [Citation4] also reported a high prevalence of voicing difficulties in their sample of IA children with CLP but found almost the same prevalence in their group of NA children with CLP. This may suggest that voicing difficulties are in fact a common type of error in all children with CLP. However, importantly, listener uncertainty when perceptually assessing the feature of voicing may also be part of the explanation.
VP impairment and glottal articulation have previously been reported to be common symptoms of speech disorder in IA children with CLP. The latter symptom is thought to be a consequence of an inability to close the velopharyngeal port [Citation35]. The level of perceived VPC in the present study improved from T1 to T3, and non-oral articulation (in which glottal articulation was included) decreased substantially from the age of 3 to the age of 7–8 years. At the age of 7–8 years, the median percentage of non-oral articulation for the group was 0% although the range was rather wide: from 0% to 18.6%, meaning that most children did not have any non-oral articulation at that age while some had a great deal of it. This finding was expected, given the above-mentioned relationship between VPC and glottal articulation. However, despite the significant overall improvement of perceived VPC, with about 40% of the children rated as having a competent VP function at T3, many children were then still rated as having marginally incompetent (7, i.e. 41%) or incompetent (3, i.e. 18%) VP function.
The findings of our study support a claim made in previous studies [Citation4,Citation5] to the effect that it is highly probable that IA children with CLP risk having speech disorders for many years after their adoption: we found evidence that speech develops slowly relative to age-specific norms. However, to be able to identify IA children with CLP who are at particular risk of persistent speech disorders, so that interventions can be made as early as possible, there is a need for more knowledge about what characterizes high-risk children and what specific areas of speech should be targeted. Having poor speech production at the age of 7–8 years may undoubtedly affect a child’s intelligibility and opportunities to talk with peers and others outside the immediate family. While the issues of intelligibility and communicative ability were outside the scope of the present study, they represent very important areas for further research. In addition, the finding of persistent speech difficulties at the age of 7–8 years needs to be further investigated on the basis of larger samples.
Some weaknesses of the present study need to be pointed out. First, the present study included a small sample of children. Because the sample was so small, we were limited to using simple statistical methods. However, compared with previous longitudinal studies of IA children with CLP, the present one has quite a large sample. In addition, this study is one of the very few longitudinal studies of speech production in IA children with CLP. Second, this study lacks a control group of NA children with CLP. At the start of this project, it was intended to include a group of NA children with UCLP. However, recruitment had to be stopped due to difficulties recruiting NA children with the same cleft type. Consequently, the results were compared only with Swedish test norms. In future research, it would be a good idea to include a comparison group that is properly matched for important variables.
There was a high variability of surgical timing within the group of children in the present study. This is common in studies of IA children with CLP [Citation4,Citation5,Citation36] and is a direct consequence of their varying adoption ages. The clinical impact of the results in the present study must therefore be evaluated in parallel with the fact that there was a high variability of surgical timing among our children. Although we acknowledge these shortcomings, we believe that the present study, with its detailed assessments of speech production, helps to remedy the lack of knowledge about IA children with CLP.
Conclusion
The present study of IA children with UCLP found a significant positive development of speech production between the ages of 3 and 7–8 years. However, even at the age of 7–8, most of the children obtained low scores for consonant proficiency, including PCC, and many of them produced cleft-related and developmental consonant errors. Almost half the group (∼40%) proved to have a competent VP function at 7–8 years of age. A few children were rated as still having an incompetent VP function at this age and many were rated as having a marginally incompetent VP function. In summary, the IA children with UCLP in the present study, although they made impressive progress in their speech development from the age of 3 years, still had persistent speech difficulties at school age and in most cases were far from the levels of speech production expected at that age.
Acknowledgements
We wish to thank all participating children and their parents. We would also like to acknowledge Johnna Sahlsten Schölin, Justin Weinfeld, Ida Johansson, Loisa Sandström, Cecilia Lindberg and Ellen Svensson for their contributions to this project.
Disclosure statement
The authors have no conflicts of interest to report.
Additional information
Funding
Notes on contributors
AnnaKarin Larsson
AnnaKarin Larsson, PhD, is a speech-language pathologist and works at the Speech and Language Pathology Unit, Institute of Neuroscience and Physiology, University of Gothenburg, as well as within the child health services of the Region Västra Götaland. Her research focus is cleft palate, speech and language development, and developmental language disorder.
Carmela Miniscalco
Carmela Miniscalco is Adjunct Professor of Speech Language Pathology at the Gillberg Neuropsychiatry Centre, University of Gothenburg. Her research focus is language development in children with language disorders and the presence of language disorders in various clinical groups, e.g. children with autism. Another area of interest is screening and early identification of language disorders.
Hans Mark
Hans Mark is Associate Professor of Plastic Surgery at the Institute of Clinical Sciences, University of Gothenburg.
Radoslava Jönsson
Radoslava Jönsson is Lecturer and Senior Consultant in ENT and Audiology at the Institute of Clinical Sciences, University of Gothenburg, and at the Sahlgrenska University Hospital. Her research focuses on children and adults with significant hearing loss, rehabilitation and implants.
Christina Persson
Christina Persson is Professor of Speech Language Pathology at the Speech and Language Pathology Unit, Institute of Neuroscience and Physiology, University of Gothenburg, and at the Sahlgrenska University Hospital. Her research focus is speech outcome in children, adolescents and young adults born with cleft palate +/-lip or 22q11.2 deletion syndrome. Another area of interest is methodologies for assessment of articulation and velopharyngeal function.
References
- Lee A, Gibbon FE, Spivey K. Children's attitudes toward peers with unintelligible speech associated with cleft lip and/or palate. Cleft Palate Craniofac J. 2017;54(3):262–268.
- Larsson A, Miniscalco C, Mark H, et al. Internationally adopted children with unilateral cleft lip and palate-consonant proficiency and perceived velopharyngeal competence at the age of 5. Cleft Palate Craniofac J. 2020;57(7):849–859.
- Larsson A, Schölin J, Mark H, et al. Speech production in 3-year-old internationally adopted children with unilateral cleft lip and palate. Int J Lang Commun Disord. 2017;52(5):626–636.
- Morgan A, O'Gara M, Bellucci CC, et al. Speech production skills in children with cleft palate who were internationally adopted. Cleft Palate Craniofac J. 2018;55(9):1225–1235.
- Sahlsten Schölin J, Jonasson A, Axelsson J, et al. Surgical, speech, and hearing outcomes at five years of age in internationally adopted children and Swedish-born children with cleft lip and/or palate. J Plast Surg Hand Surg. 2020;54(1):6–13.
- Scherer N, Baker S, Kaiser A, et al. Longitudinal comparison of the speech and language performance of United States-born and internationally adopted toddlers with cleft lip and palate: a pilot study. Cleft Palate Craniofac J. 2018;55(7):941–953.
- Kummer AW. Evaluation of speech and resonance for children with craniofacial anomalies. Facial Plast Surg Clin North Am. 2016;24(4):445–451.
- Bruneel L, Bettens K, Van Lierde K. The relationship between health-related quality of life and speech in patients with cleft palate. Int J Pediatr Otorhinolaryngol. 2019;120:112–117.
- Harding A, Grunwell P. Characteristics of cleft palate speech. Eur J Disord Commun. 1996;31(4):331–357.
- Bettens K, Alighieri C, Bruneel L, et al. Peer attitudes toward children with cleft (lip and) palate related to speech intelligibility, hypernasality and articulation. J Commun Disord. 2020;85:105991.
- Nyberg J, Hagberg E, Havstam C. "She sounds like a small child or perhaps she has problems"-peers' descriptions of speech in 7-year-olds born with cleft palate. Cleft Palate Craniofac J. 2020;57(6):707–714.
- Swanson JW, Smartt J, Saltzman BS, et al. Adopted children with cleft lip and/or palate: a unique and growing population. Plast Reconstr Surg. 2014;134(2):283e–293E.
- Sullivan SR, Jung YS, Mulliken JB. Outcomes of cleft palatal repair for internationally adopted children. Plast Reconstr Surg. 2014;133(6):1445–1452.
- Allori AC, Kelley T, Meara JG, et al. A standard setof outcome measures for the comprehensive appraisal of cleft care. Cleft Palate Craniofac J. 2017;54(5):540–554.
- Lohmander A, Lundeborg I, Persson C. SVANTE – The Swedish Articulation and Nasality Test – Normativedata and a minimum standard set for cross-linguistic comparison. Clin Linguist Phon. 2017;31(2):137–154.
- Morgan AR, Bellucci CC, Coppersmith J, et al. Language development in children with cleft palate with or without cleft lip adopted from non-English-speaking countries. Am J Speech Lang Pathol. 2017;26(2):342–354.
- Larsson A, Persson C, Klinto K, et al. Internationally adopted children with and without a cleft lip and palate showed no differences in language ability at school-age. Acta Paediatr. 2021;110(1):273–279.
- Selman P. Global Statistics for Intercountry Adoption: Receiving States and States of origin 2000. 2019 2021 [cited 2021 Sept 16]. Available from: https://assets.hcch.net/docs/a8fe9f19-23e6-40c2-855e-388e112bf1f5.pdf.
- Friede H, Lilja J, Lohmander A. Two-stage palatal surgery with early veloplasty and delayed hard palate repair: a balanced view on speech and midfacial growth outcome. In Berkowitz S, editor. Cleft lip and palate: diagnosis and management. Berlin Heidelberg: Springer-Verlag; 2013. p. 413–437.
- Boersma P. Praat, a system for doing phonetics by computer. Glot Int. 2001;5:341–345.
- IPA. IPA Chart; 2018. [cited 2021 Aug 12]. Available from: https://www.internationalphoneticassociation.org/content/ipa-chart.
- ICPLA ICPaLA. Extensions to the International Phonetic Alphabet (extIPA), symbols for disordered speech; 2015. [cited 2021 Aug 12]. Available from: https://www.icpla.info/extIPAChart2015.pdf.
- Shriberg LD, Kwiatkowski J. Phonological disorders iii: a procedure for assessing severity of involvement. J Speech Hear Disord. 1982;47(3):256–270.
- Lohmander A, Hagberg E, Persson C, et al. Validity of auditory perceptual assessment of velopharyngeal function and dysfunction – the VPC-Sum and the VPC-Rate. Clin Linguist Phon. 2017;31(7–9):589–597.
- Willadsen E, Lohmander A, Persson C, et al. Scandcleft randomised trials of primary surgery for unilateral cleft lip and palate: 5. Speech outcomes in 5-year-olds – consonant proficiency and errors. J Plast Surg Hand Surg. 2017;51(1):38–51.
- Dodd B. Differential diagnosis of pediatric speech sound disorder. Curr Dev Disord Rep. 2014;1(3):189–196.
- Sell D, Sweeney T. Percent consonant correct as an outcome measure for cleft speech in an intervention study. Folia Phoniatr Logop. 2020;72(2):143–151.
- IBM. IBM SPSS statistics for windows. 25.0. Armonk, NY: IBM Corp; 2017.
- Lundeborg Hammarström I. LINUS 2.0: LINköpingsUnderSökningen 2.0- Ett fonologiskt bedömningsmaterial för barn från 3 år. Linköpings Universitet; 2019.
- Lohmander A, Friede H, Elander A, et al. Speech development in patients with unilateral cleft lip and palate treated with different delays in closure of the hard palate after early velar repair: a longitudinal perspective. Scand J Plast Reconstr Surg Hand Surg. 2006;40(5):267–274.
- Dodd B, Holm A, Hua Z, et al. Phonological development: a normative study of British English-Speaking children. Clin Linguist Phon. 2003;17(8):617–643.
- McLeod S, Crowe K. Children's consonant acquisition in 27 languages: a cross-linguistic review. Am J Speech Lang Pathol. 2018;27(4):1546–1571.
- Choi J, Broersma M, Cutler A. Early phonology revealed by international adoptees' birth language retention. Proc Natl Acad Sci USA. 2017;114(28):7307–7312.
- Glennen S. A longitudinal study of language and speech in children who were internationally adopted at different ages. Lang Speech Hear Serv Sch. 2014;45(3):185–203.
- Chapman KL, Willadsen E. The development of speech in children with cleft palate. In Howard S, Lohmander A, editors. Cleft palate speech: assessment and intervention. West Sussex, UK: John Wiley & Sons, Ltd; 2011.
- Werker CL, de Wilde H, Mink van Der Molen AB, et al. Internationally adopted children with cleft lip and/or palate: a retrospective cohort study. J Plast Reconstr Aesthet Surg. 2017;70(12):1732–1737.

