Abstract
Objective
To determine pregnancy outcomes in women with subjective sensation of increased fetal movements (IFM).
Methods
A prospective cohort study of women after 20 weeks of gestation who were referred with subjective sensation of IFM (April 2018–April 2019) for assessment. Pregnancy outcome was compared to pregnancies with a normal sensation of fetal movements all through pregnancy who underwent obstetrical assessment at term (37–41 weeks of gestation) matched by maternal age and pre-pregnancy BMI in a 1:2 ratio.
Results
Overall, out of 28,028 women referred to the maternity ward during the study period, 153 (0.54%) presented due to subjective sensation of IFM. The latter mainly occurred during the 3rd trimester (89.5%). Primiparity was significantly more prevalent in the study group (75.5% vs. 51.5%, p = .002). The study group had increased rates of operative vaginal deliveries and cesarean section (CS) due to non-reassuring fetal heart rate (15.1% vs. 8.7%, p = .048). Multivariate regression analysis showed that IFM was not associated with NRFHR affecting the mode of delivery (OR 1.1, CI 0.55 − 2.19), opposed to other variables such as primiparity (OR 11.08, CI 3.21–38.28) and induction of labor (OR 2.46, CI 1.18–5.15). There were no differences in the rates of meconium-stained amniotic fluid, 5 min Apgar score, birth weight, or rates of large/small for gestational-age newborns.
Conclusion
Subjective sensation of IFM is not associated with adverse pregnancy outcomes.
Introduction
Self-monitoring of fetal movements has been established as a strategy to recognize pregnancies at risk for stillbirth [Citation1,Citation2]. While the sensation of reduced fetal movements has been associated with late stillbirth [Citation3], the sensation of increased fetal movements (IFM) was generally referred to as a sign of well-being [Citation4]. According to the American College of Obstetricians and Gynecologists (ACOG), numerous protocols for fetal movement counting have been reported, especially for decreased sensation of fetal movements. However, there are no current guidelines concerning IFM sensation [Citation5].
Previous studies have challenged the widely accepted notion that the sensation of IFM represented reassuring fetal status. While some suggested that episodes of IFM might reflect fetal seizure activity prior to fetal demise due to hypoxia [Citation6–8], others separated sensation of IFM that represented fetal well-being from a single vigorous fetal activity episode that might be associated with increased risk of fetal demise [Citation9,Citation10]. Of note, those were retrospective studies of women that experienced intrauterine fetal demise (IUFD), and were conducted by interview or web-based survey [Citation7–10]. Moreover, some of them were not controlled with matched cases for comparison [Citation7,Citation8].
To date, two prospective studies on IFM sensation [Citation11,Citation12] were published. Extremely different frequency of increased movements (0.45%, 9.6%) was reported. Both studies did not demonstrate any adverse perinatal outcomes associated with IFM, besides a higher prevalence of LGA in one study [Citation11]. No relation was found between the length of increased movement episodes and pregnancy outcome. Thus, we aimed to investigate the prevalence of subjective sensation of IFM and its related pregnancy outcome.
Methods
In a prospective cohort study, all pregnancies after 20 weeks of gestation, that presented to the maternity ward at a tertiary, university-affiliated medical center, due to subjective sensation of IFM from April 2018–April 2019 were enrolled and their complaint was documented in real-time. All women after 24 weeks of gestation were assessed with non-stress test (NST) and biophysical profile (BPP). Pregnancies younger than 24 weeks underwent ultrasound examination and were discharged if objective measures of the fetus were normal (movements, muscle tone and amniotic fluid level). After delivery, demographic data, obstetric history, pregnancy, and delivery characteristics were collected from the hospital-computerized database. Pregnancy characteristics included medications during pregnancy, gestational diabetes mellitus (GDM), fetal growth restriction (FGR), pregnancy-induced hypertension, pre-eclampsia and the presence of chronic hypertension (CHTN). Delivery characteristics included gestational age at delivery, presence of meconium-stained amniotic fluid, need for induction of labor, mode of delivery, indications for either vacuum-assisted delivery or cesarean section (CS), need for manual removal of the placenta or revision of uterine cavity due to suspicion of retained products of placenta, birth weight, and Apgar score. Low Apgar score was defined as <7 at 5 min after birth. Birth weights smaller than the 10th percentile or larger than the 90th percentile according to local birthweight percentiles [Citation13] were considered small for gestational age (SGA) and Large for gestational age (LGA), respectively. CS were further stratified and analyzed by indication to discriminated planed CS and intrapartum, non-elective CS.
The control group was retrospectively matched by maternal age and pre-pregnancy BMI in a 1:2 ratio, and consisted of women in term pregnancies that presented to the maternity ward at the same time period for a regular checkup, a service that is routinely provided to low-risk pregnancies over 39 weeks of gestation. Women were matched by BMI to avoid habitus influence on fetal movements subjective sensation, and age. Pregnancies complicated by fetal anomalies and twin pregnancies were excluded. The study was approved by the local IRB committee (reference number 0284-08-TLV).
Statistical analysis was performed using IBM SPSS statistical software (version 26; IBM Corporation, New York, NY). Fisher’s exact test was performed for categorical, nonparametric variables. Two-sided T-tests were used to compare continuous variables normally distributed. A probability value of <.05 was considered statistically significant.
Binary logistic regression models were used to estimate the relationship between the sensation of IFM and possible associated variables based on the univariate analysis. Similar models were used to test such variables that were possibly associated with non-reassuring fetal heart rate (NRFHR) affecting mode of delivery and the mode of delivery in order to study the association of IFM sensation with those results.
Results
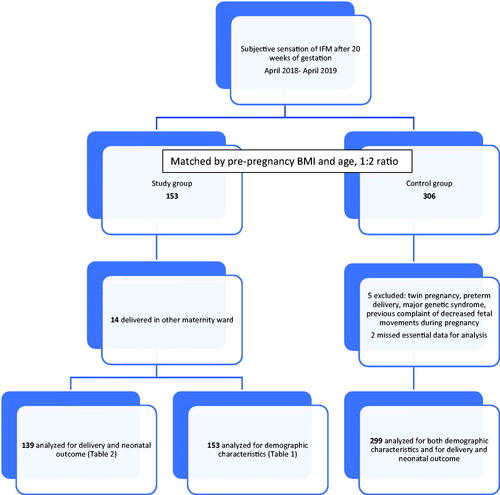
During the study period, 28028 women were referred to the maternity ward. Of them, 153 (0.54%) presented with subjective sensation of increased fetal movements and were matched with 306 controls. Fourteen women from the study group delivered at another hospital and thus delivery and neonatal outcomes were analyzed for 139 women in the study group. We excluded 5 women statistical analysis from the control group due to twin pregnancy [Citation1], preterm delivery [Citation1], major genetic syndrome [Citation1], and previous complaints of decreased fetal movements during pregnancy [Citation2] that were inappropriately matched. Two more controls missed essential data for analysis. Analysis for delivery and neonatal outcome was done on 299 women in the control group and 139 women in the study group ().
Majority of women (89.5%) in the study group were in the third trimester (mean gestational age 35.6 ± 3.6), of the 69 (45.1%) at term (37–41 weeks of gestation). All women in the study group delivered in term (after 37 weeks). A univariate analysis showed that women in the study group were more likely to be primiparous (75.5% vs. 51.5%, p = .002) and less likely to have previous CS (5.9% vs. 14.1%, p = .009), compared to the controls. No differences were found in the previous abortion rate, treatment with SSRI or main pregnancy comorbidities ().
Table 1. Demographic characteristic of the study cohorts.
Women in the study group were more likely to undergo induction of labor (22.3% vs. 15.7%) and labor augmentation (8.6% vs. 3.7%) compared to the control group (p = .005). The indications for induction and augmentation were similar (p = .069) ().
Table 2. Delivery and neonatal outcome of the study cohort.
There was a higher proportion of emergency CS in the study group (12.9% vs. 7.7%, p = .025).
Stratification of the indications for CS found that more women in the study group underwent CS due to NRFHR while more women in the control group underwent elective, planned CS due to a previous CS (p < .001) ().
Regardless to mode of delivery, significantly higher number of women in the study group demonstrated non reassuring fetal heart rate monitoring during labor compared to the control group (15.1% vs. 8.7%, p = 0.048). No significant differences were demonstrated between groups in gestational age at delivery, rate of meconium-stained amniotic fluid, indications for vacuum assisted delivery, need for manual revision of uterine cavity, low Apgar scores, birth weight or proportions of small/large for gestational age newborns ().
Since more women in the study group were found to be primiparous and had less CS in the past we further analyzed demographic characteristics and delivery mode in relation to IFM sensation to understand whether outcomes were associated with IFM or with basic characteristics of the study group. The study group also demonstrated more NRFHR that affected mode of delivery and thus we added regression models to test possible variable associated with those outcomes.
A regression model controlling for the possible variables affecting IFM sensation demonstrated that primiparity was a significant risk factor for presenting with IFM (OR 1.96, CI 1.22–3.12). Maternal age, previous CS and BMI were not associated with IFM ().
Table 3. Regression model for the possible variables associated with IFM sensation.
A regression model controlling for the possible variables associated with NRFHR affecting the mode of delivery demonstrated that IFM sensation did not increase the risk for NRFHR monitoring affecting mode of delivery (OR 1.1, CI 0.55 − 2.19). On the contrary, primiparity (OR 11.08, CI 3.21 − 38.28), maternal age (OR 1.13, CI 1.04 − 1.23) and induction (OR 2.46, CI 1.18–5.15) or augmentation of labor (OR 5.05, CI 1.76-14.5) were found to increase the odds of NRFHR monitoring affecting the mode of delivery ().
Table 4. Regression model for the possible variables associated with NRFHR affecting mode of delivery.
A multinominal regression model for possible variables associated with mode of delivery showed that IFM sensation was not associated with mode of delivery. Maternal age, BMI, previous CS and primiparity were all associated with increased risk for CS. Non spontaneous initiation of labor (induction or augmentation) was associated with significantly higher risk for emergency CS ().
Table 5. Multinominal regression model for the possible variables associated with mode of delivery a.
Discussion
In this study we aimed to learn the delivery and neonatal outcome of women with the sensation of IFM during pregnancy. A prospective cohort of women that referred with sensation of IFM during pregnancy, was compared retrospectively to a matched cohort that was referred to the maternity ward at the same time period. Documentation of subjective sensation of IFM in the study cohort in real-time ensured avoidance of a recall bias during analysis of pregnancy outcome.
We found that IFM incidence was 0.54%. Increased fetal movements were mainly presented during the 3rd trimester and almost half of the cases after 37 weeks of pregnancy. Sensation of IFM was significantly more common among primiparous (OR 1.96) and was not related to previous obstetrical history after controlling for possible confounders. Pregnancies with the sensation of IFM were found to undergo more inductions and augmentations compared to the control group and involved more deliveries due to NRFHR. Yet, in a multivariate analysis, NRFHR in labor was found to be associated with primiparity, maternal age, induction, and augmentation of labor, and not with IFM during pregnancy. All pregnancies with IFM resulted in term deliveries with similar neonatal outcomes to the control group. Mode of delivery was also not associated with IFM during pregnancy.
Our results are in concordance with the study by Sharp [Citation12] who demonstrated similar incidence (0.45%) of IFM. This is in contrast to the study by Huang [Citation11] that reported an incidence of 9.6% of the maternity population. The differences might represent differences in health systems and underestimation due to women’s accessibility to secondary clinics that enabled monitoring without the need for referral to a tertiary hospital. We did not have data from community clinics. Yet, we can assume normal assessment in secondary clinics that neglected the need for a hospital referral. Same as described by Huang [Citation11], the majority of women in the study group were primiparous. This might be related to less familiarity with fetal movements during the first pregnancy or higher levels of anxiety and caution measurements. Primiparity was shown to be associated with higher levels of pregnancy-related anxiety and was suggested as a key sociodemographic variable in antenatal screening [Citation14]. We did not have data on anxiety levels during pregnancy among the study group. Future studies might need to focus on the relation of anxiety to the sensation of increased fetal movements in order to establish this assumption.
Similar to the study by Sharp [Citation12], women with sensation of IFM underwent more induction of labor compared to controls. Yet, we demonstrated similar indications for labor induction in the control group. We also found more cases of delivery due to NRFHR in women with IFM and more emergency CS although overall CS rate was similar. The previous studies described normal CTG at presentation in most cases [Citation12] and less CS compared to controls [Citation11] but did not elaborate the indications for CS. When we analyzed multiple factors associated with emergent CS or NRFHR, IFM sensation was not a significant factor. Being delivered due to NRFHR in labor, undergoing instrumental delivery or CS was explained by other known risk factors such as primiparity, older age, higher BMI and induction or augmentation [Citation15,Citation16] and were not associated with IFM sensation. In light of the findings of the ARRIVE trial [Citation17], we should emphasize that no elective induction was offered at 39 weeks since that policy was not implanted at the study period. Moreover, our study was not designed to examine induction results. Women with IFM also didn’t have more meconium-stained fluid, which was suggested as a possible symptom of asphyxia during delivery [Citation18] and had similar neonatal outcomes as the control group.
Taken all together, the sensation of IFM might be explained by less experience and higher anxiety of primiparity than a pathologic pregnancy.
Our study was limited by the lack of a vaster characterization of the nature, length or intensity of the movements as was suggested to be related to fetal death [Citation20]. We also did not have pathology specimens of the placenta. Yet, a previous prospective study could not find association between the movement’s nature nor placental pathology to outcomes in pregnancies involving IFM [Citation12], as opposed to the association found in pregnancies with RFM [Citation19]. Generalization of the study results must take into account that health services and prenatal care in Israel and specifically in the study’s medical center are very accessible and might not be valid to the population with poorer prenatal care. The strength of our study is the prospective cohort of women with sensation of IFM, which enabled us to avoid a possible bias when reporting retrospectively on sensations after a tragic experience of fetal demise.
In conclusion, the results from our study confirm that IFM has no association with adverse pregnancy and delivery outcome. Any alternation in fetal movements might be assessed by fetal monitoring or BPP to alleviate the mother’s concern.
Additional information
Funding
References
- De Muylder X. Counting active movements of the fetus: could it be useful? Can Med Assoc J. 1982;127(12):1172–1175, 1194.
- Heazell AE, Froen JF. Methods of fetal movement counting and the detection of fetal compromise. J Obstet Gynaecol. 2008;28(2):147–154.
- Royal College of Obstetricians and Gynaecologists (UK). Green -top Guidline No. 31: the investigation and management of small-for-gestational -age-fetus; 2013.
- Froen JF. A kick from with in-fetal movement counting and the cancelled progress in antenatal care. J Perinat Med. 2004;32:13–24.
- Practice bulletin no.145: antepartum fetal surveillance. Obstet Gynecol. 2014;124:182–192.
- Whitehead CL, Cohen N, Visser GHA, et al. Are increased fetal movements always reassuring? J Matern Fetal Neonatal Med. 2020;33(21):3713–3718.
- Linde A, Pettersson K, Radestad I. Women’s experiences of fetal movements before the confirmation of fetal death – contractions misinterpreted as fetal movement. Birth. 2015;42(2):189–194.
- Warland J, O’Brien LM, Heazell AEP, et al. An international internet survey of the experiences of 1,714 mothers with late stillbirth: the STARS cohort study. BMC Pregnancy Chilbirth. 2015;15:172.
- Stacey T, Thompson JMD, Mitchell EA, et al. Maternal perception of fetal activity and late stillbirth risk: findings from the Auckland stillbirth study. Birth. 2011;38(4):311–316.
- Heazell AEP, Warland J, Stacey T, et al. Stillbirth is associated with perceived alternations in fetal activity – findings from an international case control study. BMC Pregnancy Childbirth. 2017;17(1):369.
- Huang C, Han W, Fan Y. Correlation study between increased fetal movement during the third trimester and neonatal outcome. BMC Pregnancy Childbirth. 2019;19(1):467.
- Sharp I, Adeyeye T, Peacock L, et al. Investigation of the outcome of pregnancies complicated by increased fetal movements and their relationship to underlying causes – A prospective cohort study. Acta Obstet Gynecol Scand. 2020;0:1–10.
- Dollberg S, Haklai Z, Mimoiuni FB, et al. Birth weight standarts in the live-born population in Israel. Isr Med Assoc J. 2005;5:311–314.
- Brunton R, Simpson N, Dryer R. Pregnancy-related anxiety, perceived parental self-efficacy and the influence of parity and age. IJERPH. 2020;17(18):6709.
- Roman H, Goffinet F, Hulsey FT, et al. Maternal body mass index at delivery and risk of cesarean due to dystocia in low risk pregnancies. Acta Obstet Gynecol Scand. 2008;87(2):163–170.
- Marrs C, Rosa L, Caughey M, et al. G. Elective induction at 39 weeks of gestation and the implications of a large, multicenter, randomized controlled trial. Obstet Gynecol. 2019;133(3):445–450.
- Grobman WA, Rice MM, Reddy UM, et al. Labor induction versus expectant management in low-risk nulliparous women. N Engl J Med. 2018;379(6):513–523.
- Monen L, Hasaart TH, Kuppens SM. The aetiology of meconium-stained fluid: pathologic hypoxia or physiologic foetal ripening? Early Hum Dev. 2014;90(7):325–328.
- Levy M, Kovo M, Izaik Y, et al. Reduced fetal movements at term in singleton low risk pregnancies – is there association with placental histopathological findings? Acta Obstet Gynecol Scand. 2020;99(7):884–890.
- Sadovsky E, Polishuk WZ. Fetal movements in utero: nature, assessment, prognostic value, timing of delivery. Obstet Gynecol. 1977;50(1):49–55.