Abstract
Brain-based explanations of addiction have been promoted for several decades. Their utility, however, is controversially discussed in the scientific community. While existing literature documents how stakeholders such as treatment providers, affected persons, and the public view their utility, views of the addiction research community are rarely represented. We aimed to complement existing studies by surveying researchers on their perspectives on the needs of addicted individuals, the utility of neuroscientific research for prevention and treatment, and future research priorities. 1440 international addiction researchers from many disciplines were invited to participate in a LimeSurvey. Their views on the treatment requirements of persons with addictions were assessed with a Likert scale and an open-ended question. The utility of neuroscientific research for prevention and treatment and the desired future priorities in addiction research were surveyed with open-ended questions. Quantitative items were analyzed descriptively. The qualitative content analysis of the free-text contributions followed an iterative inductive approach. Additionally, future research priorities were categorized deductively according to the underlying direction. 190 researchers from 29 countries participated (13.2%). Most considered various treatment and support options helpful and approaches tailored to the needs of individuals to be the most promising. The utility of neuroscientific research was evaluated critically by several, but benefits in terms of pharmacological treatment and the possibility to identify risk groups were acknowledged. Future areas of inquiry for addiction research mentioned were heterogenous and included neuroscientific/genetic/medications development (13%), psychosocial aspects (19%), and integrated bio-psycho-social approaches (45%). A corresponding reconsideration of treatment, support, and research seems warranted.
Introduction
If addiction were a brain disease, would it matter? The considerable paradigm shift from a moral to a medical, brain-based conceptualization of addiction, centered primarily on relatively recent neuroscientific findings, has sparked a multitude of hopes and expectations. In his 1997 milestone article ‘Addiction is a brain disease, and it matters’, the then director of the National Institute on Drug Abuse (NIDA), Alan Leshner, envisioned that brain disease explanations would result in less stigma and improved access to treatment (Leshner Citation1997). In line with these optimistic prospects, further researchers expected the implementation of more effective preventive measures, public health policies, and treatment options (Dackis and O'Brien Citation2005; Volkow and Koob Citation2015; Volkow et al. Citation2016; Volkow and Boyle Citation2018; Uhl et al. Citation2019). The so-called ‘brain disease model of addiction’ (BDMA) has since been strongly promoted by influential researchers and institutions such as NIDA (National Institute on Drug Abuse (NIDA) Citation2020).
The brain as the core of addiction problems and, consequently, the primary target of strategies to address them (Leshner Citation1997) has been the widely advocated approach for decades now. However, the debate on the utility and implications of brain-based explanations of addiction is still ongoing (Room Citation2021; Heilig et al. Citation2021a, Citation2021b). Especially the use of neuroscientific findings for the prevention and treatment of addiction is heavily contested (Bell et al. Citation2014; Blomqvist et al. Citation2014; Barnett et al. Citation2015; Hall et al. Citation2015a; Peele Citation2016; Volkow et al. Citation2016; Volkow and Boyle Citation2018; Hellman et al. Citation2022, p. 135ff). Furthermore, the focus of addiction research on neuroscientific approaches (Nature Citation2014) has been questioned. In particular, the perceived underinvestment in research into factors other than brain changes seems to be of concern (Tomlinson et al. Citation2009; Hall et al. Citation2015b, Citation2003). A publication in the journal Nature stating that neuroscientific explanations of addiction were not particularly controversial in the scientific community provoked strong opposition. Ninety-four researchers signed a letter to the editor criticizing this notion (Heim Citation2014). They subsequently founded the Addiction Theory Network with the aim to oppose the dominant influence of the BDMA (Heather et al. Citation2018).
Various stakeholder groups have since been consulted regarding their opinions about the utility of neuroscientific research findings. In particular, treatment providers have been found to hold mixed views about addiction (Barnett et al. Citation2015, Citation2018). A qualitative study involving six Australian clinicians found that brain-based explanations were seen as relevant for some types of patients but lacked relevance to others. They were integrated into some therapies, but at the risk of ignoring key social, psychological, and environmental factors (Barnett et al. Citation2015). Overall, a great need for research assessing the views of treatment providers on the clinical impact of a BDMA was identified (Barnett et al. Citation2018).
Studies of affected persons’ (Hammer et al. Citation2012; Koski-Jännes et al. Citation2012; Wiens and Walker Citation2015; Morphett et al. Citation2017, Citation2018; Jack et al. Citation2019), family members’ (Meurk et al. Citation2016) and the general public's (Koski-Jännes et al. Citation2012; Meurk et al. Citation2014) views found mixed results of the usefulness of a medical conception of addiction.
Researchers’ perspectives, however, are also important. They play a fundamental role in determining research priorities and developing possible solutions to problems (Pickard and Ahmed Citation2020, p. 1). The impact of their work includes directly research-related issues, such as the type of problem/knowledge investigated and the methods used, as well as service impact, e.g. the type and management of services and evidence-based practice. In addition, the political and societal impact of research endeavors must always be considered (Kuruvilla et al. Citation2006). Given the multiple consequences of their work - for affected persons and others - and the amount of research available on other stakeholders’ perceptions of addictions, researchers in this field are a significantly under-researched group to date.
To our knowledge, only two studies investigated addiction researchers’ perspectives on the consequences of brain-based explanations of addictions. In one of them, 31 Australian addiction neuroscientists were asked about the clinical impact of a BDMA. Among other things, they were concerned about focusing on medical interventions and neglecting social components. Both, expectations of potential benefits for affected persons’ motivation and behavior and worries about adverse consequences were reported (Bell et al. Citation2014).
In a second study, Dingel et al. assessed the opinions of 20 US-American scientists investigating neurogenetic links to nicotine addiction (Dingel et al. Citation2012). Most participants had a medicalized understanding of addiction and highlighted the prospect of neuroscience aiding the development of better prevention and cessation therapies. They were, however, concerned that a biomedical model might over-emphasize pharmaceutical approaches, thus leading to a reallocation of resources from traditional public health programs and therapies (Dingel et al. Citation2012; Citation2012). They also expressed concern that a disease model of addiction could lead young people to underestimate the difficulty of quitting smoking (Dingel et al. Citation2012).
This study builds on these previous efforts. After a considerable time promoting brain-based explanations of addiction, it explores the current perspectives of international addiction researchers from a broad range of disciplines. First, the perceived needs of individuals with addictions were examined using a mixed quantitative and qualitative approach, ‘mixed methods light’ (Creswell and Plano Clark Citation2018, p. 492). Second, views about the contribution of neuroscientific research results on addictions to prevention and treatment were examined, and third, desired future research priorities were explored qualitatively.
Methods
The study is part of the project ‘Addiction in the Brain: Ethically Sound Implementation in Governance’ (A-BRAIN). Ethics approval was granted by the University of Bremen/Germany on 6 December 2018.
Participants
In August 2018, a sample of international addiction researchers was compiled using a purposeful and feasible approach to include as many academic disciplines and opinions as possible. For that purpose, the editorial board members of all journals listed in the Journal Citation Report 2018 (JCR) of Clarivate Analytics (Clarivate Analytics Citation2020) in the categories ‘substance abuse’ (scie & ssci) and ‘medical ethics (scie) (n = 2586), and the members of the ‘International Society of Addiction Journal Editors’ (ISAJE) (International Society of Addiction Journal Editors, Citation2020) (n = 51) were identified.
Additionally, advisors of the National Institutes of Health (NIH; ‘National Advisory Council on Drug Abuse’ (NACDA)) (National Institute on Drug Abuse (NIDA)) Citation2018) (n = 20), reviewers from the National Institute on Drug Abuse (NIDA; ‘Pathophysiological Basis of Mental Disorders and Addictions Study Section, Center for Scientific Review’ (PMDA)) (National Institutes of Health (NIH)) Citation2018) (n = 18), signatories of the letter to the editor of the journal Nature ‘Addiction: Not just brain dysfunction’ (Heim Citation2014) (n = 94), and speakers from the interdisciplinary ‘Addiction, the Brain and Society Conference 2009’ (n = 26) (Dunbar et al. Citation2010) were added to the list. Furthermore, respondents were asked to name other researchers they thought should be invited to participate (snowball sampling).
After checking for duplicates, the sample was finalized by excluding (a) members of the A-BRAIN consortium, (b) deceased persons, (c) persons with less than three publications on addiction-related themes in the past 15 years (possibly other research focus), (d) persons with invalid mail addresses (no contact possible), and (e) those who stated that they did not consider themselves to be addiction researchers. The sample population thus compiled comprised 1440 potential participants from 49 countries.
Instrument and procedure
The major themes discussed in the context of brain-based explanations of addiction to be included in the questionnaire were identified through a literature review. The disciplinary diversity in the field of addiction research was accounted for by utilizing the databases PubMed (medical focus), PsychInfo (psychological focus), and Sociological Abstracts (sociological focus). Publications from 2007 (first edition of NIDA’s ‘Drugs, Brains, and Behavior’ (National Institute on Drug Abuse (NIDA) Citation2020)) to May 2018 in all languages were searched for using the search terms ‘brain disease model of addiction’, ‘brain disease’ AND ‘addiction’, and ‘brain disease’ AND ‘SUD’ in titles and abstracts. The themes extracted from 71 identified papers were subsequently incorporated into the questionnaire. This paper focuses on the questions (a) What are the needs of individuals with addictions regarding treatment approaches and support? (b) What is the use of neuroscientific research on substance use disorders for prevention and treatment? (c) What should be the future foci in addiction research and research funding?
Basic demographic information of the researchers was also collected, i.e. gender, age, country of workplace, and academic background (academic degrees, grouped according to the main categories of the bepress Digital Commons Three-Tired Taxonomy of Academic Disciplines (bepress Citation2019)).
The questionnaire was set up as a LimeSurvey and distributed to the potential participants via e-mail. One personal invitation and up to two reminders were sent out beginning in February 2019. The data collection period ended two weeks after the point when no further responses were received after the last reminder. This was the case at the Ende of August 2019.
Data and analysis
The questions reported in this paper were assessed using quantitative and qualitative approaches. To answer question (a) ‘Persons with substance use disorders need…’, participants were asked to indicate their (dis-)agreement with 26 statements ( and Table S1) by selecting one option from a 6-point Likert-like scale (very strongly disagree, strongly disagree, partially disagree, partially agree, strongly agree, very strongly agree) or ‘I don’t know’ for each of the statements. Additionally, a free text field allowed for further suggestions and comments. Questions (b) ‘How do you envision neuroscientific research results being used for prevention and treatment of substance use disorders?’ and (c) ‘What should, in your opinion, be the future focus/foci of research and research funding in the field of substance use disorders?’ were open-ended.
Figure 1. Needs of addicted persons regarding treatment approaches according to addiction researchers.
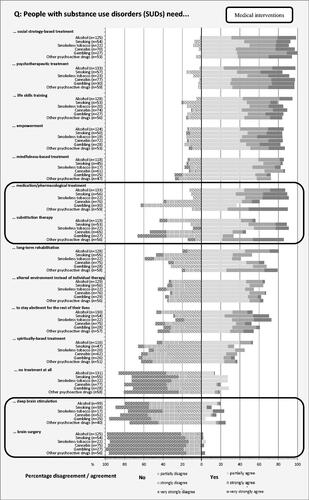
Figure 2. Needs of addicted persons regarding support and other societal responses according to addiction researchers.
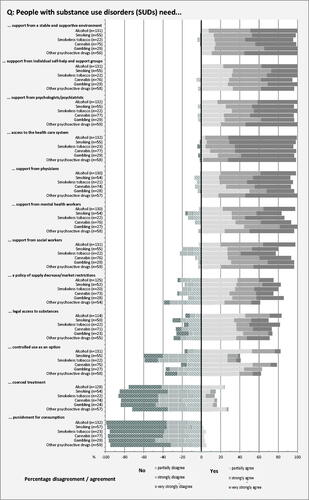
Table 1. Participants’ characteristics.
From the Likert-type scale answers, absolute and relative frequencies were calculated using IBM SPSS statistics 24 software.
The qualitative content analysis (Mayring Citation2015; Bengtsson Citation2016) of the free-text answers followed a general inductive approach (Thomas Citation2006; Mayring Citation2015, p. 152). The target group is experts in their fields. Also, participant-generated textual data produce more standardized responses (Braun and Clarke Citation2013, pp. 135, 137). We have thus used an analytical approach on a semantic level (Braun and Clarke Citation2006, Citation2013, p. 207). Our analyses enable statements on the relative weight of the themes based on their frequency (Thomas Citation2006; Neale et al. Citation2014; Mayring Citation2015, pp. 13, 65). In combination with the reporting of qualitative anecdotes, they help to convey a more balanced picture (Seale Citation1999, p. 129). Additionally, a deductive coding scheme was applied to the answers to question (c) on future research priorities. Depending on the underlying methodological approach, the responses were categorized as either ‘neuroscientific/genetic’, ‘psychosocial’, ‘integrated, multi-scientific’, or ‘unclear/other’. DO and JF independently coded the texts using MAXQDA 10 software, discussed the results, and resolved discrepancies.
Results
190 addiction researchers (66.8% males, 32.1% females, 1.1% unknown, 13.2% response rate) from 29 countries participated in the survey. Most participants came from North America (45.3%) and Europe (42.6%). Anglophone countries accounted for just over 60% of responses. This distribution was similar to the invited primary sample (details in Supplementary Table S1). However, invited researchers from several smaller countries, especially from the African continent, did not respond. The gender distribution was also imbalanced: slightly less than two-thirds of the invited researchers and slightly more than two-thirds of the participants were men (Supplementary Table S1). Details on the composition of the sample are presented in . Age was excluded due to the high proportion of missing values (25.3%). Null-results from inferential test analyses of associations between participants’ opinions and their gender, country, or academic discipline were severely limited due to the insufficient size of some cells. They were thus not included here as results.
(a) Needs of individuals with addictions
The perspectives of the responding researchers regarding the perceived needs of addicted individuals in terms of treatment strategies are displayed in . Participants’ views generally did not differ much between the substances/behavior, except for the questions about medication, substitution therapy, and long-term rehabilitation. Therefore, the results reported here are summarized for all substances. In addition, the level of (dis)agreement with the need of addicted persons for a range of treatment and support options was assessed using Likert-type scales (very strongly, strongly, and partially (dis)agree). The textual presentation below combined the results into agreement and disagreement, respectively. Detailed information on the different levels and the substances can be found in and Supplementary Table S2.
Table 2. Addiction researchers’ opinions on future research priorities.
The overall assessment shows that the participating researchers generally were positively inclined toward a lot of approaches. Notable exceptions were the invasive medical interventions ‘brain surgery’ and ‘deep brain stimulation’. Only very few participants indicated agreement with the need for these options. Also, only about 20% of the participants thought that no treatment at all, and about 40% that spiritually-based treatment was needed by persons with addictions. Highest approval rates were achieved for social and psychological approaches such as social strategy-based treatment, psychotherapeutic treatment, life skills training, empowerment, and mindfulness-based treatment. More than 80% of the respondents considered them helpful for persons with addictions. The noninvasive medical interventions ‘medication/pharmacological treatment’ and ‘substitution therapy’ were also regarded as helpful by a majority of respondents for some types of addiction. Overall, however, it cannot be said that these options were deemed the most important by the participants.
In general, no substantial differences were found in our data between different types (substances and behaviors) of addictions in terms of the treatment needs of affected individuals. Exceptions, however, were the noninvasive medical interventions ‘medication’ and ‘substitution therapy’. Medication for alcohol, cannabis, and gambling addiction, as well as substitution therapy for persons addicted to alcohol, were not considered helpful by the majority of respondents in this survey. In contrast, they were found to be useful for individuals with the other addictions mentioned. In addition, significantly fewer participants felt that tobacco users (smoking and smokeless tobacco) needed long-term rehabilitation than all other types of addicted individuals.
The evaluation of the question gauging support options for addicted individuals and of other societal responses () showed that almost all participating researchers thought that persons with addictions need support in many different ways. Respondents, in this way, indicated their agreement with several different approaches that included various professional groups, the affected persons’ environment, self-help groups, and also access to the health care system. In contrast, the vast majority of participants rejected punishment and coerced treatment as responses to substance use problems. The policy measures ‘supply decrease/market restrictions’ and ‘legal access to substances’ were deemed helpful by about 70% of the researchers. No significant differences were found between the different types of addictions here, too. An exception, however, was the extent to which participants agreed that controlled consumption was needed. Its benefit was assessed differently depending on the type of substance/behavior under consideration. About 40% of the participants agreed that it was useful for smoking and smokeless tobacco, about 60% for gambling and other psychoactive drugs, and about 80% for alcohol and cannabis.
The free-text comments provided by the participants predominantly emphasized the need to tailor treatment and support to the particular requirements and circumstances of the affected individual (n = 22) and to integrate different approaches and providers (n = 4). Individual participants also mentioned the need for prevention, access to vaping for smokers, formalized cessation, a block-modular program built on functional diagnostics of mental medicine, and the provision of support through registered, specialized clinical and practice nurses.
(b) Use of neuroscientific research results for prevention and treatment of addiction
The open-ended question on the use of neuroscientific research results for the prevention and treatment of SUDs was answered by 133 participants. Thirty of them thought that this body of knowledge has so far only been of limited practical use. For example, a respondent remarked that: ‘After 90 years, very limited successful transfer of findings from neuroscience to effective treatment, and limited prospects at the moment’ (respondent S101). Further, eleven participants expressed concerns about the possible use of neuroscientific findings in a way they would disapprove of. Some expressed this in general terms, such as: ‘Not in any way I approve of’ (S102). Others specified in what ways they felt it was not helpful, like for instance the following participant: ‘Very unhelpful, as there is far too great a bias toward neuro research and hence insufficient funding for the massive range of other ideas, most of which are also important.’ (S103).
Regarding the use of neuroscientific approaches for the prevention of addiction, 35 respondents saw some benefit. The most important factors mentioned by the participants were the possibility of identifying risk groups and targeting measures accordingly. One respondent, for example, stated that he thought ‘… neuroscientific research can help identify those more at risk for use and difficulties, perhaps those who most benefit from prevention and treatment.’ (S132). Another area where some participants saw benefits as improvements related to policy information. One comment in this regard was: ‘Inform better policies around SUD prevention and treatment’ (S183).
Improved treatment approaches based on neuroscientific findings were thematized by 65 participants. The main areas mentioned addressed pharmacological treatment (n = 25), targeted interventions (n = 11), and integrated bio-psycho-social approaches (n = 21). Some respondents also mentioned marginal themes which cannot be reported here. Expected advances in pharmacological, genetic, and brain-intervention approaches were particularly related to the safety and efficacy of medications. One participant expressed it as follows: ‘discovery of new safe and effective medications other than additional treatment strategies.’ (S107). Further, the possibility to develop targeted interventions was identified as an essential benefit of neuroscientific research on addictions. This was predominantly seen as a result of an improved understanding of basic neurological mechanisms. The contribution of one respondent in this sense read: ‘Personalized medicine! If we could understand the underlying pathology and neural dysfunctions then we could intervene where it is needed most. Current treatments are ‘kitchen sink’ approaches and treat all people with SUD the same.’ (S40). Finally, the role of neuroscientific treatment and/or prevention approaches as one component of an integrated bio-psycho-social strategy was also considered important. For example, one participant noted that ‘Treatments will always consist of multiple components … and even new revolutionary pharmaceuticals will only be one part of successful treatment.’ (S143). At the same time, concerns were raised that a possible over-simplification of the phenomenon would impair the usefulness of neuroscientific research on addiction. In particular, the need to also consider other approaches was highlighted in this context. This was summarized by one participant as ‘It could be so helpful as long as it doesn’t oversimplify the problem and neglect alternative approaches.’ (S51).
(c) Future foci in addiction research
Participants’ opinions about what addictions research and its funding should focus on in the future yielded a wide range of issues and approaches. Given the heterogeneity of the answers of 133 participants, a deductive coding scheme was applied based on the underlying research orientation of the issues mentioned. Respondents’ answers were categorized into either (a) neuroscientific & genetic approaches, (b) psychosocial approaches, (c) integrated/both, bio-psycho-social approaches, or (d) other contributions which could not be classified under the above topics (). Almost half of the respondents, 45.1%, mentioned either integrated bio-psycho-social approaches or a combination of both, psycho-social and neuro-scientific. Less than 20% mentioned exclusively psycho-social orientations of future research, and even fewer, just under 13%, wanted merely neuroscientific, genetic, or pharmaceutical research priorities.
When looking more closely at the themes specified by the participants, it is noticeable that most of them were mentioned by a few or single respondents. This makes detailed qualitative analyses difficult, as it is not possible to form meaningful categories with sufficiently frequent mentions. Therefore, the results are reported here only in a narrative summary. Some participants, for instance, were particularly interested in investigating specific phases, such as the transition from use to disorder, craving, recovery and remission, and relapse. Others wanted to focus on issues related to treatment, such as immunotherapies and vaccinations, medication and neuroscience-based approaches, integrated psychosocial-medication-based treatment, psychosocial approaches, harm reduction, efficacy and best practice, targeted approaches, and the effects of no treatment at all. The respondents who listed methodological procedures mentioned mixed methods, qualitative research, longitudinal/population studies, implementation research, clinical studies, and RCTs. Further, service and access were noted by some respondents, as well as the society-related themes of stigma reduction, public education, policies, and availability control. Finally, some participants added general comments, such as the necessity of an increase in research funding and the perceived current overfunding of neuroscientific research.
Discussion
Brain-based explanations of addiction have now been promoted for a considerable period of time (Leshner Citation1997; Volkow et al. Citation2016; National Institute on Drug Abuse and (NIDA) Citation2020). This study examined the current views of a comparatively large sample of 190 international addiction researchers from a broad range of disciplines. It focused on treatment and support for those affected, prevention, and the future direction of research.
A large proportion of the respondents to this survey emphasized the need to integrate neuroscientific findings into broader prevention and treatment strategies. This is in line with previous research on smaller samples of neuroscientists from the USA and researchers from the field of genetic nicotine research from Australia (Dingel et al. Citation2012; Citation2012; Bell et al. Citation2014). In particular, what the current study adds to these earlier efforts is that it showed that socially and psychologically based approaches to treatment and further support received the highest approval rates from the participants. However, medication, substitution therapy, and support from physicians also played an important role. In contrast, most respondents rejected invasive therapeutic options such as brain surgery and deep brain stimulation, as well as punishment and coercive treatment.
Furthermore, the use of neuroscientific research results for the prevention and treatment of addiction was assessed in a differentiated manner. While some participants saw no or limited use, others considered the development of medications and targeted interventions to be promising. It was, however, also highlighted that these need to be integrated as just one element of a multi-faceted approach. This indicates that neither highly optimistic nor very critical hopes and expectations regarding brain-based explanations of addiction were shared. In particular, the notion that ‘basic research’ as a fundamental basis for successful addiction prevention and treatment essentially involves genetic and neurobiological approaches (Volkow and Boyle Citation2018) was not shared by the majority of respondents in this study. The brain was not seen as the primary target to address addiction problems (Leshner Citation1997). However, the inclusion of brain-based explanations of addiction was also mentioned by participants in this study as a component of treatment, but without neglecting other approaches. This is in line with, for instance, findings from Australian addiction neuroscientists (Bell et al. Citation2014) and treatment providers (Barnett et al. Citation2015).
Regarding future research directions, the multitude of approaches listed by the respondents seems to reflect the heterogeneity and multidisciplinary composition of the sample. However, neuroscience/genetics/pharmacology was the preferred future research direction by only a minority. This strongly challenges a neuro-centric orientation of addiction research, as has been criticized, for example, by Hall and colleagues (Hall et al. Citation2003; Citation2015a, Citation2015b) and Hammer and colleagues (Hammer, 2013). Our work, in this way, indicates that integrative approaches are the ones considered the most promising by the markedly largest proportion of participating researchers. It clearly argues for a reorientation of addiction research toward approaches that include psycho-social factors as well as the brain.
The limitations of this study include the definition and identification of the target group. The inhomogeneous backgrounds of ‘addiction researchers’ as well as possibly diverging opinions were accounted for by including as many disciplines as possible from multiple sources. Participation bias cannot be completely ruled out either. Thus, the sample cannot be regarded as representative of the whole addiction research community.
Additionally, while the response proportion of 13.2% is slightly higher than in other studies on the same target group and with comparable data collection strategies (Mulligan et al. Citation2013), it remains relatively low. The study is thus exploratory in nature. Inferential analyses were not possible because some cells were too small in size. Future studies with larger samples are needed to investigate potential differences in respondents’ opinions as a function of gender, country, and academic discipline. Further, the dominance of researchers from Anglophone countries in the sample might reflect the situation in the addiction research community but limits the generalizability to other countries.
The qualitative method chosen to analyze the data focuses on the relative importance of a theme based on the frequency of mentions (Neale et al. Citation2014). It thus neglects marginal themes and does not necessarily reflect the importance to, for example, affected persons (Braun and Clarke Citation2006; Kuckartz Citation2018).
Finally, exploring opinions via multiple-choice questions helps provide an overview but is inherently simplistic. Partial (dis-)agreement thus has to be interpreted with caution. Also, a forced-choice approach was chosen; therefore, a neutral attitude could not be expressed. To increase the depth of understanding, an opportunity to frame the results and add further aspects into a free text field was provided (Rhodes and Coomber Citation2010; Creswell and Plano Clark Citation2018, p. 492).
In summary, our study provides interesting insights into the current views of 190 international addiction researchers from a broad range of disciplines. After a considerable period of promoting and funding research on brain-based explanations of addiction, the majority of the participants do not consider the hopes and expectations placed in this approach fully met (Leshner Citation1997; Volkow et al. Citation2016; Volkow and Boyle Citation2018). The critical arguments published in the literature (Heim Citation2014; Hall et al. Citation2015a, Citation2015b; Heather et al. Citation2018) were shared by many. However, it is essential to note that the value of neuroscientific contributions to research, prevention, and therapy of addictions was also acknowledged. In particular, it becomes apparent that monocausal approaches are not considered appropriate by the majority of the respondents. This applies to prevention and treatment strategies as well as other support measures - and to future research priorities. Medical approaches, however, are not rejected entirely but are included as one, if not the most important, topic in both therapy and research.
We conclude that a broad discussion of the orientation of prevention and treatment strategies and the appropriate role that neuroscientific approaches should have in these is still warranted. Likewise, research priorities need to be critically evaluated. The Tomlinson et al. study of global mental health research priorities (Tomlinson et al. Citation2009) may provide guidance in this regard. Based on the findings of this study, a modification of current addiction research to include a broad range of aspects and disciplines at an appropriate scale is needed. Neuroscience research has its place in this, but not necessarily the first.
Ethics approval & informed consent
Ethics approval, including the data protection concept, was granted from the University of Bremen/Germany, on 6 Dec 2018.
Participants were comprehensively informed about the content, methodology and purpose of the study at the beginning of the LimeSurvey. They were asked to declare their consent before the survey could be started.
Statements and declarations
The work described has not been published before and is not under consideration for publication anywhere else. Its publication has been approved by all authors.
Ochterbeck_Supplementary_table_S2_support_needs.docx
Download MS Word (60.5 KB)Ochterbeck_Supplementary_tables_S1_sample_characteristics.docx
Download MS Word (21.1 KB)Acknowledgements
The authors would like to express their sincere thanks to Dr. Christoph Buck (Leibniz Institute for Prevention Research and Epidemiology – BIPS, Bremen/Germany) for the support provided with the statistics, and Dr. Florence Samkange-Zeeb (Leibniz Institute for Prevention Research and Epidemiology – BIPS, Bremen/Germany) for her valuable language editing and comments.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Barnett A, Hall W, Fry CL, Dilkes-Frayne E, Carter A. 2018. Drug and alcohol treatment providers’ views about the disease model of addiction and its impact on clinical practice: a systematic review. Drug Alcohol Rev. 37(6):697–720.
- Barnett Anthony, Fry CL. 2015. The clinical impact of the brain disease model of alcohol and drug addiction: exploring the attitudes of community-based AOD clinicians in Australia. Neuroethics. 8(3):271–282.
- Bell S, Carter A, Mathews R, Gartner C, Lucke J, Hall W. 2014. Views of addiction neuroscientists and clinicians on the clinical impact of a ‘brain disease model of addiction.’. Neuroethics. 7(1):19–27.
- Bengtsson M. 2016. How to plan and perform a qualitative study using content analysis. NursingPlus Open. 2:8–14.
- bepress 2019. Disciplines: digital commons three-tiered taxonomy of academic disciplines. Berkley (USA): Bepress. https://www.bepress.com/reference_guide_dc/disciplines/
- Blomqvist J, Koski-Jännes A, Cunningham J. 2014. How should substance use problems be handled? Popular views in Sweden, Finland, and Canada. Drugs and Alcohol Today. 14(1):19–30.
- Braun V, Clarke V. 2006. Using thematic analysis in psychology. Qual Res Psychol. 3(2):77–101.
- Braun V, Clarke V. 2013. Successful qualitative research: a practical guide for beginners. Los Angeles: SAGE.
- Clarivate Analytics 2020. InCites. Journal Citation Reports. https://jcr.clarivate.com/JCRLandingPageAction.action?Init=Yes&SrcApp=IC2LS&SID=H2-df99yIL4cJl6UwfMeLJ4aGhm4LxxfYKbxx-18x2dw2WrWm8OCrVTPTpUU0DGKQx3Dx3DfSGlX5b5cUHfUSkbx2BdEkmgx3Dx3D-qBgNuLRjcgZrPm66fhjx2Fmwx3Dx3D-h9tQNJ9Nv4eh45yLvkdX3gx3Dx3D.
- Creswell JW, Plano Clark VL. 2018. Designing and conducting mixed methods research (Third Edition). Los Angeles (CA): SAGE.
- Dackis C, O'Brien C. 2005. Neurobiology of addiction: treatment and public policy ramifications. Nat Neurosci. 8(11):1431–1436.
- Dingel MJ, Hicks AD, Robinson ME, Koenig BA. 2012. Integrating genetic studies of nicotine addiction into public health practice: stakeholder views on challenges, barriers and opportunities. Public Health Genom. 15(1):46–55.
- Dingel MJ, Karkazis K, Koenig BA. 2012. Framing nicotine addiction as a ‘disease of the brain’: social and ethical consequences. Soc Sci Q. 92(5):1363–1388.
- Dunbar D, Kushner HI, Vrecko S. 2010. Drugs, addiction and society. BioSocieties. 5(1):2–7.
- Hall W, Carter A, Forlini C. 2015a. The brain disease model of addiction: is it supported by the evidence and has it delivered on its promises? The Lancet. Psychiatry. 2(1):105–110.
- Hall W, Carter A, Forlini C. 2015b. Brain disease model of addiction: misplaced priorities? The Lancet. Psychiatry. 2(10):867.
- Hall W, Carter L, Morley KI. 2003. Addiction, neuroscience and ethics. Addiction. 98(7):867–870.
- Hammer R, Dingel MJ, Ostergren JE, Nowakowski KE, Koenig BA. 2012. The experience of addiction as told by the addicted: incorporating biological understandings into self-story. Cult Med Psychiatry. 36(4):712–734.
- Heather N, Best D, Kawalek A, Field M, Lewis M, Rotgers F, Wiers RW, Heim D. 2018. Challenging the brain disease model of addiction: European launch of the addiction theory network. Addict Res & Theory. 26(4):249–255.
- Heilig M, MacKillop J, Martinez D, Rehm J, Leggio L, Vanderschuren LJMJ. 2021a. Addiction as a brain disease revised: why it still matters, and the need for consilience. Neuropsychopharmacology. 46(10):1715–1723.
- Heilig M, MacKillop J, Martinez D, Rehm J, Leggio L, Vanderschuren LJMJ. 2021b. Response to ‘Addiction is a social disease: just as tenable as calling it a brain disease. Neuropsychopharmacology:. 46(10):1713–1714.
- Heim D. 2014. Addiction: not just brain malfunction. Nature. 507(7490):40.
- Hellman M, Egerer M, Stoneham J, Forberger S, Ochterbeck D, Rundle S. 2022. Addiction and the brain: knowledge, beliefs and ethical considerations from a social perspective. Springer Nature, Singapore: Palgrave Macmillan.
- International Society of Addiction Journal Editors 2020. ISAJE home. London (UK): ISAJE. https://www.isaje.net/.
- Jack Oller D, Kelly JF, Magidson JF, Wakeman SE. 2019. Asking how our patients understand addiction. Am JlMed. 132(3):269–271.
- Koski-Jännes A, Hirschovits-Gerz T, Pennonen M. 2012. Population, professional, and client support for different models of managing addictive behaviors. Subst Use Misuse. 47(3):296–308.
- Kuckartz U. 2018. Qualitative Inhaltsanalyse: methoden, Praxis, Computerunterstützung (4. Auflage). Beltz Juventa.
- Kuruvilla S, Mays N, Pleasant A, Walt G. 2006. Describing the impact of health research: a research impact framework. BMC Health Serv Res. 6:134.
- Leshner AI. 1997. Addiction is a brain disease, and it matters. Science. 278(5335):45–47.
- Mayring P. 2015. Qualitative Inhaltsanalyse: Grundlagen und Techniken (12., überarbeitete Auflage). Weinheim & Basel: Beltz Verlag.
- Meurk C, Fraser D, Weier M, Lucke J, Carter A, Hall W. 2016. Assessing the place of neurobiological explanations in accounts of a family member’s addiction. Drug Alcohol Rev. 35(4):461–469.
- Meurk C, Partridge B, Carter A, Hall W, Morphett K, Lucke J. 2014. Public attitudes in Australia towards the claim that addiction is a (brain) disease: is addiction a (brain) disease? Drug Alcohol Rev. 33(3):272–279.
- Morphett K, Carter A, Hall W, Gartner C. 2017. Framing tobacco dependence as a ‘brain disease’: implications for policy and practice. Nicotine Tob Res. 19(7):774–780.
- Morphett K, Carter A, Hall W, Lucke J, Partridge B, Gartner C. 2018. Do neurobiological understandings of smoking influence quitting self-efficacy or treatment intentions? Nicotine Tob Res. 20(7):827–835.
- Mulligan A, Hall L, Raphael E. 2013. Peer review in a changing world: an international study measuring the attitudes of researchers. J Am Soc Inf Sci Technol. 64(1):132–161.
- National Institute on Drug Abuse (NIDA). 2018. Membership roster NACDA (National Advisory Council on Dug Abuse). https://www.drugabuse.gov/about-nida/advisory-boards-groups/national-advisory-council-drug-abuse-nacda/council-roster.
- National Institute on Drug Abuse, (NIDA) 2020. Drugs, Brains, and Behavior: The Science of Addiction; Drugs and the Brain. National Institute on Drug Abuse. https://www.drugabuse.gov/publications/drugs-brains-behavior-science-addiction/drugs-brain.
- National Institutes of Health (NIH). 2018. Membership roster PDMA (Pathophysiological Basis of Mental Disorders and Addictions Study Section Center For Scientific Review). Pathophysiological Basis of Mental Disorders and Addictions Study Section Center For Scientific Review (PDMA): Membership Roster. https://internet.csr.nih.gov/Rosters/MemberRoster.aspx?s=PMDA.
- Nature E. 2014. Animal farm. Nature. 506(7486):5–5.
- Neale J, Miller P, West R. 2014. Reporting quantitative information in qualitative research: guidance for authors and reviewers. Addiction. 109(2):175–176.
- Peele S. 2016. People control their addictions: no matter how much the ‘chronic’ brain disease model of addiction indicates otherwise, we know that people can quit addictions - with special reference to harm reduction and mindfulness. Addict Behav Rep. 4:97–101.
- Pickard, H., & Ahmed, S. H. (Eds.) 2020. The Routledge handbook of philosophy and science of addiction (First issued in paperback). London (NY): Routledge, Taylor & Francis Group.
- Rhodes T, Coomber R. 2010. Qualitative methods and theory in addictions research. In P. G. Miller, J. Strang, & P. M. Miller (Eds.), Addiction research methods. (p. 59–78. Oxford (UK): Wiley-Blackwell.
- Room R. 2021. No level has primacy in what is called addiction: ‘addiction is a social disease’ would be just as tenable. Neuropsychopharmacology 46(10):1712.
- Seale C. 1999. The quality of qualitative research. London: Sage Publications.
- Thomas DR. 2006. A general inductive approach for analyzing qualitative evaluation data. Am JEval. 27(2):237–246.
- Tomlinson M, Rudan I, Saxena S, Swartz L, Tsai AC, Patel V. 2009. Setting priorities for global mental health research. Bull. World Health Organ. 87(6):438–446.
- Uhl GR, Koob GF, Cable J. 2019. The neurobiology of addiction. Ann N. Y Acad of Sciences. 1451(1):5–28.
- Volkow ND, Boyle M. 2018. Neuroscience of addiction: relevance to prevention and treatment. Am J Psychiatry. 175(8):729–740.
- Volkow ND, Koob G. 2015. Brain disease model of addiction: why is it so controversial? The Lancet. Psychiatry. 2(8):677–679.
- Volkow ND, Koob GF, McLellan AT. 2016. Neurobiologic advances from the brain disease model of Addiction. N Engl J Med. 374(4):363–371.
- Wiens TK, Walker LJ. 2015. The chronic disease concept of addiction: helpful or harmful? Addict Res Theory. 23(4):309–321.

