?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Arabic-speaking immigrants and refugees constitute one of the largest immigrant groups in Sweden. Previous research on Arabic-speaking immigrants indicates elevated levels of psychological disorders, including depression and anxiety. The aim of the present pilot study was to examine the efficacy of an internet-delivered cognitive behavioural treatment (ICBT) in an Arabic-speaking immigrant population. The intervention was individually tailored based on self-described problems and consisted of nine modules targeting areas such as depression, anxiety and insomnia. In total, 59 individuals were included and randomized to either an 8-week treatment or wait-list control. Self-reported symptoms of depression on the PHQ-9 were used as primary outcome measure. Secondary outcome measures of anxiety, stress, insomnia, quality of life and post-traumatic stress were also used. In the intention-to-treat analysis, depressive symptoms were significantly reduced compared to the wait-list control group with a between-group effect at post-treatment of Cohen’s d = 0.85 [0.29, 1.41]. We also found significant between-group effects for symptoms of insomnia and stress, but not for anxiety, post-traumatic stress or quality of life measures. The results indicate that ICBT is a promising treatment approach for treating symptoms of depression, insomnia and stress, in an Arabic-speaking immigrant population. Further studies with larger samples are warranted.
Introduction
The last few years have seen a substantial increase in the number of people applying for asylum in European countries with a majority of asylum-seekers arriving from either Syria, Afghanistan or Iraq (Abbott, Citation2016; Swedish Migration Agency, Citation2017; World Health Organiation, Citation2018). Hence, the majority of these people have come from countries experiencing war or internal turmoil and the term refugee rather than migrant would be applicable for a majority of these individuals (UNHCR, Citation2016). A large proportion of these immigrants or refugees have Arabic as their first language, especially those arriving from Syria or Iraq. In Sweden there has also been a migration from other countries where Arabic is spoken such as Somalia and Eritrea (Statistics Sweden, Citation2018), making it likely that Arabic now is the second most common native language in Sweden after Swedish (Parkvall, Citation2018).
With regard to the mental health of immigrants in general, research findings have been mixed with some studies showing higher rates of mental disorders and others not (Bas-Sarmiento et al., Citation2017; Gilliver et al., Citation2014). However, when it comes to refugees specifically, a clearer picture emerges where refugees demonstrate higher levels of mental disorders such as depression, anxiety, post-traumatic stress and psychosis compared to other immigrants as well as the general population (Fazel et al., Citation2005; Hollander et al., Citation2016). These elevated levels of mental health problems found in refugee populations have been shown to be related to factors such as exposure to armed conflict and torture (Steel et al., Citation2009), as well as various post-displacement factors such as experiencing restricted economic opportunities, living in institutional accommodation and the stress inherent in the asylum-seeking process (Porter & Haslam, Citation2005; Silove et al., Citation1997). Recent research on displaced Syrians confirms the picture painted above, with studies showing increased risk of adverse mental health outcomes, such as depression, anxiety and post-traumatic stress, in this group (Alpak et al., Citation2015; Tinghög et al., Citation2017). These studies also show that exposure to potentially traumatic events, such as interpersonal violence, as well as post-migration stressors, is associated with increased risk of above-mentioned adverse outcomes (Alpak et al., Citation2015; Tinghög et al., Citation2017).
Despite these mental health challenges faced in particular by refugees and to some extent also by other immigrant populations, few intervention studies in Sweden have been conducted targeted specifically towards the mental health of immigrant or refugee populations (Gilliver et al., Citation2014). There is also evidence suggesting that immigrant and refugee populations tend to under-utilize mental health services, possibly due to factors such as low availability of linguistically accessible services, low awareness of available services and stigma associated with mental health problems (Kirmayer et al., Citation2011). In addition, according to the Swedish National Board of Health and Welfare (Citation2013), there is also a limited availability of psychotherapeutic services in Swedish primary care in general, complicating matters even further, and even more so regarding services in Arabic, which is the first language of many newly-arrived refugees and immigrants.
To meet the mental health needs of a growing immigrant population in Sweden and other western countries where many likely suffer from mental health problems, internet-delivered cognitive behavioral therapy (ICBT) could be one part of a solution (Andersson & Titov, Citation2014). Andersson and Titov (Citation2014) suggested that internet-delivered services could enhance treatment-seeking for some groups by providing increased anonymity and accessibility. ICBT is also considered a cost-effective treatment requiring relatively little therapist resources (Andersson et al., Citation2019), which provides a clear advantage given the scarcity of Arabic-speaking psychotherapists currently available, both in Sweden and elsewhere (see, for example, Halaj & Huppert, Citation2017). However, in order to increase engagement and effectiveness, it is also important to culturally adapt the treatment to make it aligned with norms and values of the target population (Chu & Leino, Citation2017) since doing so has been shown to increase treatment effectiveness (Nagayama Hall et al., Citation2016) and possibly also treatment engagement (Huey et al., Citation2014). This adaptation could, for example, both include targeted outreach efforts as well as modifications, additions and/or removal of treatment components to make the treatment better suited to the particular needs of the target population (Chu & Leino, Citation2017).
Culturally adapted ICBT has been tested in at least four previous randomized controlled trials with moderate to large effects relative to control conditions (Choi et al., Citation2012; Ince et al., Citation2013; Knaevelsrud et al., Citation2015; Lindegaard et al., Citation2019), indicating the potential of this treatment format. All of these previous trials have examined the effect of disorder-specific treatment programs. However, given the high level of comorbidity likely present in the study sample (e. g. Fazel et al., Citation2005), we decided to test an individually tailored ICBT intervention, which according to Păsărelu et al. (Citation2017) can be one way to address comorbidity. The individual tailoring means that the patient receives a combination of treatment modules from different CBT treatment packages, based on the specific patients’ symptom presentation and preferences (Păsărelu et al., Citation2017). Although there currently exists a limited amount of individually tailored ICBT studies, existing evidence indicates that individually tailored ICBT-programs are equally effective as disorder-specific programs in treating anxiety, depression and quality of life (Păsărelu et al., Citation2017).
Thus, the aim of the present study was to test whether a culturally adapted, individually tailored ICBT treatment was significantly more effective in reducing symptoms of anxiety and depression compared to a wait-list control. To our knowledge, this was the first study to examine the effect of a culturally adapted ICBT program for an Arabic-speaking immigrant population in a randomized controlled trial.
Method
Study design
The study was a randomized controlled pilot trial where participants were randomly allocated to either an 8-week ICBT treatment or a wait-list control condition in a 1:1 ratio. Primary and secondary outcome measures were administered at the start of treatment, at three weeks after treatment start and at post-treatment. The control group received the same treatment at the end of the study phase. Power calculations indicated that at least 26 participants would have to be included in each arm for a power of 0.80 given an effect of Cohen’s d = 0.70, which could be expected from similar studies (Ince et al., Citation2013; Lindegaard et al., Citation2019). The study received an ethics approval from the Regional Ethical Board in Linköping, Sweden (number 2017/488-31). The trial was preregistered at clinicaltrials.gov, ID number NCT03496350. In the study protocol, we stated that we intended to recruit 120 participants. However, due to difficulties recruiting participants and Arabic-speaking staff, we decided to run a pilot trial with at least 26 participants in each arm based on the power calculation mentioned above. Moreover, in the study protocol, the treatment was branded as transdiagnostic; however, in the write-up, we decided that individually tailored was a more correct description of the treatment. The 1-year follow-up mentioned in the study protocol will be reported in a separate publication.
Participants and recruitment
The recruitment phase began in early 2019. The study was advertised on social media platforms as well as through paid advertisements in popular search engines. The advertisement contained brief information about the study, i.e. that we aimed to test an online CBT intervention for depression and anxiety and that participation was free of charge. The advertisement contained text written in both Arabic and English, both texts clearly stated that the treatment itself was in Arabic. The reason for also having the advertisement in English was to make it possible for non-Arabic speaking individuals to understand the content of the advertisement and to share it on social media. We also tried reaching potential participants by advertising in clinics that specifically target immigrant and refugee mental health. Interested individuals were directed to the study home page where they could read relevant information about the study. The study home page was only available in Arabic. Participants who registered had to sign an online informed consent sheet and then go through a screening where they answered sociodemographic questions as well as filled in the Patient Health Questionaire-9 (PHQ-9; Löwe et al., Citation2004), Generalized Anxiety Disorder-7 (GAD-7; Spitzer et al., Citation2006), Insomnia Severity Index (ISI; Bastien et al., Citation2001), Percieved Stress Scale-14 (PSS-14; Cohen et al., Citation1983), Alcohol Use Disorders Identification Test (AUDIT; Saunders et al., Citation1993), Brunnsviken Brief Quality of Life (BBQ; Lindner et al., Citation2013) and the Impact of Events Scale Revised (IES-R; Weiss & Marmar, Citation1997). Both the informed consent form as well as all questionnaires were provided in Arabic. Once the screening was completed, participants that met inclusion criteria were called up for a short clinical interview. All participants were asked about their main concern that they wanted help with as well as secondary problems. The interview also contained questions about their current life situation and whether they would be able to allocate the time required to complete and make use of the treatment. Finally, we also assessed potential obstacles to participation in the study, such as suicidality, having a severe mental disorder or substance abuse.
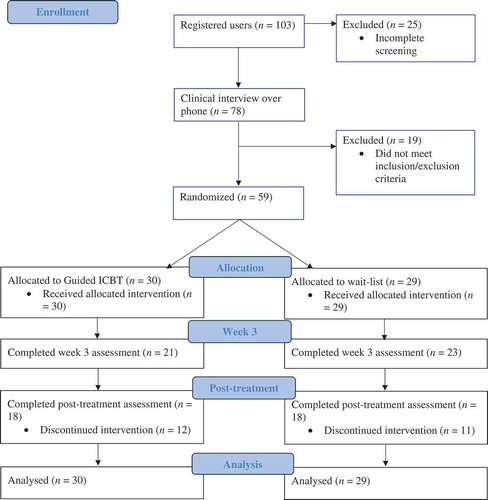
In total, 103 participants registered on the website, however only 78 of these completed the entire screening procedure and were called up for a clinical interview. All interviewed participants were discussed in a case management conference together with the principal investigator (GA), who made the final decision on inclusion and who was clinically responsible for the study. Of all interviewed cases, 59 individuals met the inclusion criteria for the study and were subsequently randomized to either of the two conditions through a random number generator (www.random.org), generated by one of the authors of the study. A flowchart of participant progression throughout the study can be found in , descriptive statistics of included participants can be found in .
Table 1. Socio-demographic characteristics of participants at pre-treatment
Inclusion criteria
In order to be included in the study, participants had to 1) read and write Arabic fluently, 2) have elevated symptoms of depression and/or anxiety as determined by their scores on the PHQ-9 and GAD-7, respectively. However, no specific cut-off point was used; instead, we made a decision based on overall symptom presentation and whether we thought that the intervention could be of use for the participant, considering the participants life situation and if they could allocate the time to complete the intervention 3) currently reside in Sweden and 4) be above 18 years old.
Exclusion criteria
Exclusion criteria for the study included 1) having a severe mental illness such as bipolar disorder or schizophrenia, 2) suicidal ideation, 3) substance or alcohol abuse and 4) ongoing psychological treatment.
Treatment and therapist
The treatment was an adapted version of the self-help material described in Nygren et al. (Citation2018) that contains seven modules targeting the following problem areas: anxiety, depression, insomnia, stress, emotion regulation, worry and intrusive memories/flashbacks, as well as an introductory module and a maintenance module. A number of exercises were added to each module in order to better suit the guided format in the present study. Several changes were also made to the introductory module introducing the participant to the guided ICBT format as well as covering the basics of the ABC model of functional analysis and goal setting for the treatment. The module also contained a goal-setting exercise which together with the clinical interview that was part of the screening procedure was used to individually tailor the treatment to the perceived needs of each participant. For example, for a participant who described problems with low mood and insomnia, we would assign the depression module following the introductory module, and then the insomnia module once the participant had made some progress working with his or her depressive symptoms. However, modifications to the tailoring were also made along the way based on the participants’ response to the treatment. All participants received the introductory module as well as the maintenance module at the end of treatment.
The therapists consisted of two psychologist and two master’s degree-level psychologist students. The therapist provided weekly feedback to the study participants on a weekly basis by way of nonsynchronous text messages sent through the built-in messaging service in the treatment platform. The messages contained feedback on completed homework assignments as well as motivational comments, which have been shown to increase adherence to treatment in previous studies (see, for example; Ebert et al., Citation2018). The therapists received supervision once a week from two licensed clinical psychologists, where one had extensive experience of working with ICBT. A psychiatrist was also available for consultation. For the participants in the wait-list control condition, no therapist contact nor modules were available. However, when the first treatment period ended participants in the control condition received the same treatment for 8 weeks.
All communications between the therapist and the participants, administration of self-report measures as well as distribution of treatment modules were conducted through a secure online platform, for details see Vlaescu et al. (Citation2016).
Cultural and language adaptation
As described in Nygren et al. (Citation2018), the treatment program was developed in an iterative fashion with a developmental process that included feedback from two focus groups and 105 pilot users. Given that Arabic-speaking individuals can have a wide range of different cultural backgrounds, the adaptation process was mainly focused on making the material and case examples easily recognizable and accessible to people from varying cultural backgrounds.
Measures
All measures were administered at pre-treatment, three weeks after treatment start, and post-treatment.
Primary outcome measure
The primary outcome measures were severity of depressive symptoms as measured on the PHQ-9 (Löwe et al., Citation2004). The PHQ-9 was chosen as primary outcome since previous research has shown depressive symptoms to be the most common mental health problem, together with post-traumatic stress, among middle eastern refugees resettled in European countries (Laban et al., Citation2005; Tinghög et al., Citation2017). The PHQ-9 assesses the degree of depression and is scored from 0 to 36. The PHQ-9 has excellent internal consistency, .89 (Löwe et al., Citation2004), and has also shown good validity and compliance with clinical assessments (Spitzer et al., Citation1999). In the present sample, Cronbach’s alpha for the PHQ-9 was 0.86.
Secondary outcome measures
The GAD-7 measures symptoms of anxiety and worry and is scored from 0 to 28 (Spitzer et al., Citation2006). It has been validated against clinical assessments and other measures and has demonstrated high validity, both in research studies (Spitzer et al., Citation2006), and in primary care settings (Löwe et al., Citation2008). In the present sample, Cronbach’s alpha for the GAD-7 was .85. Both measures have been validated in Arabic-speaking populations (AlHadi et al., Citation2017; Sawaya et al., Citation2016).
The PSS-14 is a 14-item self-report measure of symptoms of stress which has demonstrated good psychometric attributes (Cohen et al., Citation1983). The PSS-14 has been validated in an Arabic-speaking population showing adequate reliability and validity (Almadi et al., Citation2012). In the present sample, Cronbach’s alpha for the PSS-14 was .68.
The ISI is a 7-item self-report measure of symptoms of insomnia and is scored from 0 to 28 (Bastien et al., Citation2001). The ISI is considered a valid and sensitive measure (Bastien et al., Citation2001) and preliminary investigations indicate that the Arabic version is reliable and valid (Suleiman & Yates, Citation2011). In the present sample, Cronbach’s alpha for the ISI was .84.
The IES-R is a 22-item self-report measure of symptoms of post-traumatic stress disorder (Weiss & Marmar, Citation1997). The IES-R has demonstrated high internal consistency as well as high test–retest reliability (Weiss & Marmar, Citation1997). The Arabic version of the IES-R has shown good discriminant validity and reliability in a sample of Middle Eastern refugees (Davey et al., Citation2015). In the present sample, Cronbach’s alpha for the IES-R was .90.
The BBQ is a 12-item self-report measure of quality of life scored from 0 to 100 (Lindner et al., Citation2013). It has demonstrated excellent test–retest reliability as well as the sensitivity to distinguish clinical from non-clinical groups (Lindner et al., Citation2013, Citation2016). The BBQ has been translated into Arabic but has yet to be validated in an Arabic-speaking population. However, in the present sample, Cronbach’s alpha for the BBQ was .81.
The AUDIT consists of 10 questions related to alcohol use, dependency symptoms and harmful effects of drinking (Saunders et al., Citation1993). The AUDIT has been subject to extensive evaluation and has consistently shown sound reliability and validity (Reinert & Allen, Citation2007). The Arabic version of the AUDIT has demonstrated good internal reliability and predictive validity in a prison sample in the Arabian Gulf region (Almarri et al., Citation2009). In the present sample, Cronbach’s alpha for the AUDIT was .76. The AUDIT was primarily used as a screening measure for alcohol use and was not analysed as a separate outcome measure.
Data analytic approach
To examine average change rates among participants in the treatment condition compared to the control condition, a latent growth curve model was used (Hesser, Citation2015). This type of model allows for individual differences in initial symptom levels as well as rates of change, which is called random effects in this approach, in addition to modeling group level effects of initial symptom levels and rate of change, called fixed effects (Hesser, Citation2015). The latent growth curve model was implemented using a Structural Equation Modeling (SEM) framework, where the random intercept and random slope are modeled as two latent factors (Wang & Wang, Citation2012). A latent growth curve model enables modeling the effect of different time-variant or time-invariant covariates, such as treatment group or background characteristics, on individual change rates (Wang & Wang, Citation2012). It also takes into account non-independence of observations in repeated measures over time, making this type of model better suited to analysis of longitudinal data compared to more traditional approaches such as repeated-measures ANOVA (Hesser, Citation2015; Kwok et al., Citation2007).
In line with recommendations by Tasca and Gallop (Citation2009), a random intercept model was first specified to calculate an ICC score to examine whether there was a dependency among the observations. Secondly, an unconditional growth model was specified adding time as a predictor. It was decided that time would be modeled linearly given that each measure was only measured at three time points and due to the small sample size. Finally, a conditional growth model was specified adding treatment group, yielding a final model,
Walds test was used to test for the significance of the individual random and fixed effects variables as well as the covariation of the random effects. All calculations were carried out using Mplus version 8 (Muthén & Muthén, Citation2017).
The analysis made use of all available data through the use of full information maximum likelihood estimation (FIML), thus making it a full intention-to-treat analysis. This type of analysis assumes that the data are Missing At Random (MAR), meaning that the probability of missing data is allowed to be dependent on any observed variable but not on the would-be value of the missing datapoint (Schafer & Graham, Citation2002). In principle, it is impossible to test whether the assumption of MAR holds, however, according to Schafer and Graham (Citation2002), serious violations of this assumption is relatively rare. FIML is one of the recommended methods for dealing with missing data (Enders, Citation2010; Hesser, Citation2015; Schafer & Graham, Citation2002) and has been shown to provide reasonably unbiased estimates under the assumption of MAR (Schafer & Graham, Citation2002).
Cohen’s d effect sizes were calculated by dividing the estimated endpoint differences in means between the respective groups with the square root of the sum of the residual plus the estimate of the random intercept (Feingold, Citation2009). Finally, clinically significant change was analyzed using criteria c in Jacobson and Truax (Citation1991) using norm population data from AlHadi et al. (Citation2017) for the PHQ-9. This meant that a participant had to score below 12.2 points on the PHQ-9 at post-treatment in order to be considered as having attained a clinically significant change. We also computed a Reliable Change Index (RCI) in order to analyze if the change was reliable and not a result of measurement error (Jacobson & Truax, Citation1991). A participant was considered having a clinically significant change if they fulfilled above mentioned criteria for either of the two primary outcome measures.
Results
Attrition and adherence
Dropouts were defined as those participants who did not complete the post-treatment assessment. In total, 12 participants in the treatment group and 11 participants in the control group did not complete the post-treatment assessment, yielding a dropout rate of 39%. However, of these 23 participants, 9 completed the assessment at week three while 1 of the participants who did complete the post-treatment assessment did not complete assessment at week three. No differences were found between those who completed the post-treatment assessment and those who did not on any of the pre-treatment or sociodemographic variables using independent t-test and χ2 tests.
With regards to adherence, here defined as having completed at least one of the exercises in a module, on average the participants completed 2.23 treatment modules. Treatment adherence was not related to any of the pre-treatment variables, p > .05, nor did it correlate with change scores on any of the outcome measures, p > .05. For a complete overview of participant adherence, see .
Table 2. Number of completed modules during treatment
Assignment of treatment modules
The anxiety module was the most frequently assigned module (67% of participants) followed by the emotion regulation module (50%), depression (40%), worry (33%), difficult memories (23%), insomnia (23%) and stress (20%).
Analysis of treatment effects
Main outcome measures
provides descriptive statistics for all outcome measures at each assessment point for the two conditions. All regression outputs can be found in Appendix 1. The results from the latent growth curve models revealed significant individual variability in initial symptom level (intercept) but no significant variability in rate of change (slope) on the PHQ-9. There was no significant covariance between the random intercept and random slope, indicating that initial symptom level did not correlate with rate of change.
Table 3. Observed means, standard deviations and Ns for each measure for the two conditions over time
A significant effect was found for Group by Time −0.42 (95% CI [−0.82, −0.02], z = −2.06, p = .039) on the PHQ-9, thus showing that the treatment group improved on average 0.42 points more per week as compared to the control group. The between-group treatment effect was Cohen’s d = 0.85 [0.29, 1.41], which is a large effect size.
Secondary outcome measures
The latent growth curve models for the secondary outcome measures revealed significant individual variability in initial symptom level (intercept) on all outcomes except the PSS-14, but no significant variability in rate of change (slope) on any measure. There was no significant covariance between the random intercept and random slope for any of the measures.
For the GAD-7, no significant effect was found for Group by Time −0.29 (95% CI [−0.62, 0.05], z = −1.68, p = .09), with a moderate between-group effect size of Cohen’s d = 0.62 [0.01, 1.25]. For the PSS-14, a significant effect was found for Group by Time −0.53 (95% CI [−0.94, −0.12], z = −2.51, p = .012). The between-group treatment effect was Cohen’s d = 1.12 [0.4, 1.84], a large effect size. For the ISI, a significant effect was found for Group by Time −0.37 (95% CI [−0.65, −0.09], z = −2.59, p = .01). The between-group treatment effect was Cohen’s d = 0.68 [0.06, 1.30], a moderate effect size. For the IES-R no significant effect was found for Group by Time −0.10 (95% CI [−0.95, 0.76], z = −0.23, p = .59). The between-group treatment effect was Cohen’s d = 0.24 [−0.36, 0.84], a small effect size. For the BBQ, no significant effect was found for Group by Time 1.12 (95% CI [−0.02, 2.47], z = 1.63, p = .10). The between-group treatment effect was Cohen’s d = 0.79 [0.17, 1.4], a moderate effect size.
Clinically significant change and negative effects
Five of the 18 participants in the treatment group who completed the post-treatment assessment had a pre-treatment score below 12.2 points on the PHQ-9 and were thus below the cut-off for clinically significant change. They were therefore excluded from the analysis. Of the remaining 13 participants, five (38%) had a clinically significant change while also having a reliable change. For the control group, three of the 18 participants who completed the post-treatment assessment had a pre-treatment score that was below the cut-off for clinically significant change and were excluded from the analysis. One of the remaining 15 participants (7%) who completed the post-treatment assessment had a clinically significant change while also having a reliable change.
To test if more participants in the treatment group compared to the control group had a clinically significant change, a χ2 test was used, revealing a non-significant difference in favor of the treatment group: χ2 (1) = 1.84, p = 0.066, with the odds ratio (OR) = 8.75, 95% CI [0.86–88.69].
With regards to negative effects experienced during treatment, none of the participants in the treatment group reported experiencing any negative effects of the treatment when asked at the post-treatment assessment. Using the reliable change index, it was calculated that one (6%) of the patients in the treatment group had a reliable deterioration on the GAD-7 and that one (6%) of the patients in the control group had a reliable deterioration on the PHQ-9.
Discussion
The present pilot study is to our knowledge the first to examine the effect of an ICBT intervention for an Arabic-speaking immigrant population in a randomized controlled trial. The effect of the ICBT intervention was in the large range (d = 0.85) for the main outcome measure, the PHQ-9, compared to the wait-list control group. With regards to clinically significant change, a total of 38% of those participants in the treatment group who completed the post-treatment assessment had a clinically significant change, while also having a reliable change according to the RCI, compared to 7% in the control group. In addition, two of the secondary outcome measures reached statistical significance, the PSS-14 (d = 1.12) and the ISI (d = 0.68), while the other three secondary outcome measures, the BBQ (d = 0.79), the GAD-7 (d = 0.62) and the IES-R (d = 0.24), did not. Overall, these results give preliminary indications that the present ICBT program could be an effective intervention for the target population. Thus, in light of both the large number of Arabic-speaking immigrants in Sweden and other European and non-European countries, as well as the tendency among immigrants to under-utilize mental health services, this or similar interventions could be of great importance both for the mental health of these individuals and for a successful integration process into society.
With regard to the main outcome of the study, the present study’s finding that depressive symptoms were successfully reduced is in line with previous research demonstrating the efficacy of ICBT interventions in treating depressive symptoms among immigrant or refugee populations (e.g., Choi et al., Citation2012; Lindegaard et al., Citation2019). It is worth noting that only 40% of participants were assigned the depression module, perhaps indicating that non-specific factors were responsible for part of this effect. Moreover, the fact that depressive symptoms were successfully reduced is highly significant given that depression is the most prevalent mental health problem among refugees (Tinghög et al., Citation2017).
Regarding anxiety, the moderate between-group effect found in the present study is similar to effects obtained in other culturally adapted ICBT interventions which have been in the small to moderate range (Choi et al., Citation2012; Ince et al., Citation2013; Knaevelsrud et al., Citation2015; Lindegaard et al., Citation2019). A more adequately powered study would likely have yielded significant results. However, the effect is still lower than in regular ICBT trials where effects in the large range are usually observed (Andersson et al., Citation2019), despite the fact that it was the most frequently assigned module. This could indicate that the anxiety module needs further adaptation to the target population in order to obtain similar effects as in regular ICBT trials.
Concerning insomnia, the moderate effects obtained in this study are in line with findings from other ICBT trials (Seyffert et al., Citation2016) and indicates that the treatment was effective in reducing symptoms of insomnia. There are, to our knowledge, few studies to date which examine the prevalence of insomnia among immigrant and refugee populations. However, existing studies indicate high prevalence of moderate to severe insomnia (for example, Al-Smadi et al., Citation2019), highlighting the need for effective interventions. Similarly, the large effect on perceived stress mirrors the effects seen in other ICBT trials (Heber et al., Citation2017). The finding that the perceived stress of the participants was lowered after the intervention is significant given that previous research shows that post-migration stress is a significant contributor to the mental health problems of refugees and immigrants (Porter & Haslam, Citation2005). With regard to the lack of effect on the IES-R, it can be seen as an indicator that the current treatment program was not well suited to address the high levels of PTSD symptomatology present in the study sample. It is possible that the effect would have increased if more participants had been assigned the PTSD module as only 23% of participants were given access to this module. The reason for this was that we chose to primarily focus on stabilizing interventions, such as emotion regulation exercises and behavioral activation, before working directly with traumatic memories. However, it is possible that a more direct focus would have improved the efficacy of the treatment. Another reason for the lack of effect in this area could be that many participants were in need of a more comprehensive PTSD-treatment given that they probably had multiple and severe traumas (Tinghög et al., Citation2017). Hence, a treatment focusing on PTSD exclusively might be needed to successfully treat these symptoms (e.g., Knaevelsrud et al., Citation2015). Finally, the moderate effect found on the BBQ in the present trial is similar to what has been observed in previous tailored ICBT trials (Păsărelu et al., Citation2017).
With regards to attrition and adherence, the present study had an attrition rate of 39%, which is somewhat higher than found in most previous ICBT studies (Fernandez et al., Citation2015). Regarding adherence, the participants completed 2.23 modules on average which is substantially lower than what is found in other ICBT studies targeting western populations (Van Ballegooijen et al., Citation2014). One potential explanation for this could be that many participants likely had arrived to Sweden fairly recently and therefore had unstable living conditions, which in turn might have affected their ability to complete the treatment. It is also possible that the target population in this and other ICBT trials targeting immigrant and refugee populations is more distressed compared to western populations targeted in the standard ICBT trial which in turn could explain the lower adherence and higher attrition. Another possibility is that the treatment was not sufficiently adapted to be appealing for the target population which might have adversely affected treatment adherence and attrition (Chu & Leino, Citation2017; Huey et al., Citation2014). As discussed previously, this adaptation process was made more difficult due to the heterogeneity found in the Arabic-speaking population in Sweden where previous research has shown that target population heterogeneity negatively effects the results of culturally adapted treatments (Huey et al., Citation2014). Another explanation for the low number of modules completed is the fact that this was an individually tailored treatment where only a limited number of modules were relevant for each respective participant. We therefore did not expect any participant to complete all nine modules and for some participants only one or two modules were relevant apart from the introduction and maintenance module. The overall adherence was also affected by the nine participants in the treatment group who did not complete a single module. Finally, it is also possible that some to us unknown cultural factor affected treatment adherence and attrition given that similar problems have been encountered in some (e.g., Ince et al., Citation2013) but not all (e.g., Lindegaard et al., Citation2019) previous ICBT trials targeting similar populations.
Concerning negative effects of treatment, none of the participants who answered the post-treatment assessment in the treatment group reported any negative effects of the treatment although one participant (6%) in the treatment group had a reliable deterioration on the GAD-7, similar to the 9.3% deterioration rates found by Rozental et al. (Citation2015) based on four large clinical ICBT trials. However, given the relatively high attrition rate discussed above, it is possible that some of the participants who dropped out of the study experienced negative effects from the treatment.
Regarding the limitations of the present study, it should be mentioned that the use of a wait-list control group limits the ability to make inferences regarding whether the observed treatment effects were due to active ingredients in the treatment or more general effects of being in an active treatment condition. In addition, some previous research also points to the possibility of the wait-list being a nocebo condition, possibly making participants worse (Furukawa et al., Citation2014). If this is the case, it would undermine the conclusion presented here regarding improvement of the treatment group compared to the control group since this improvement could be the result of a deterioration of the control group. However, this is likely not the case in the present study given that participants in the control group did not deteriorate on any outcome measure relative to the pre-treatment assessment. In addition, many if not most previous trials of internet-delivered interventions conducted by our research group have demonstrated either no change or even small to moderate positive improvements in wait-list control conditions (see, for example, Andersson et al., Citation2012; Johansson et al., Citation2017; Silfvernagel et al., Citation2018). Another limitation concerns the fact that there was no follow-up assessment which makes it impossible to know the long-term effects of the intervention. There was also a substantial dropout rate with 30% of participants never completing a single module. In addition, the reliance on self-reported symptoms of depression and anxiety, as opposed to a structured diagnostic procedure could be said to constitute a weakness of the present study. The reason for this was that we had a limited amount of Arabic-speaking clinician time which put constraints on how much resources could be allocated to the pre- and post-treatment assessment. Another limitation concerns the fact that we did not collect any data regarding country of origin of the participants, which limits our knowledge about the cultural heterogeneity of the study sample. It is likely that cultural differences between participants lead to different experiences of the current treatment. Finally, one of the secondary outcome measurements (BBQ) lacked previous validation in an Arabic-speaking population, raising the question regarding its ability to meaningfully capture the construct of quality of life in the present study population.
Conclusion
The present study was a small pilot RCT but gives a preliminary indication of the feasibility of the ICBT treatment approach for symptoms of depression and possibly anxiety among Arabic-speaking individuals in Sweden. The treatment resulted in large reductions in depressive symptoms and moderate reductions in anxiety symptoms, thereby indicating that ICBT interventions such as this one has the potential to increase the chance of successful integration into society and reduce the burden of suffering in a vulnerable population. However, these findings should be replicated in a more well-powered study. In addition, the high level of PTSD symptomatology present in the refugee population is perhaps best addressed with a PTSD-specific treatment, given the lack of effects in the present study.
Acknowledgments
The presented study was sponsored by grants from The Swedish Association of Local Authorities and Regions an in part by the Swedish Science Foundation. The funders had no role in the design or conduct of the study nor in writing the manuscript. We thank George Vlaescu for program and treatment platform management.
Disclosure statement
No potential conflict of interest was reported by the authors.
Data availability statement
The data on which the present study is based are not publicly available due to ethical restrictions; however, the data is available on request from the corresponding author.
Additional information
Funding
References
- Abbott, A. (2016). The mental-health crisis among migrants. Nature, 538, 158–160. https://doi.org/10.1038/538158a
- AlHadi, A. N., AlAteeq, D. A., Al-Sharif, E., Bawazeer, H. M., Alanazi, H., AlShomrani, A. T., Shuqdar, R. M., & AlOwaybil, R. (2017). An arabic translation, reliability, and validation of patient health questionnaire in a Saudi sample. Annals of General Psychiatry, 16(1), 1–9. https://doi.org/10.1186/s12991-017-0155-1
- Almadi, T., Cathers, I., Hamdan Mansour, A. M., & Chow, C. M. (2012). An Arabic version of the perceived stress scale: Translation and validation study. International Journal of Nursing Studies, 49(1), 84–89. https://doi.org/10.1016/j.ijnurstu.2011.07.012
- Almarri, T. S. K., Oei, T. P. S., & Amir, T. (2009). Validation of the alcohol use identification test in a prison sample living in the Arabian gulf region. Substance Use & Misuse, 44(14), 2001–2013. https://doi.org/10.3109/10826080902848533
- Alpak, G., Unal, A., Bulbul, F., Sagaltici, E., Bez, Y., Altindag, A., Dalkilic, A., & Savas, H. A. (2015). Post-traumatic stress disorder among Syrian refugees in Turkey: A cross-sectional study. International Journal of Psychiatry in Clinical Practice, 19(1), 45–50. https://doi.org/10.3109/13651501.2014.961930
- Al-Smadi, A. M., Tawalbeh, L. I., Gammoh, O. S., Ashour, A., Tayfur, M., & Attarian, H. (2019). The prevalence and the predictors of insomnia among refugees. Journal of Health Psychology, 24(8), 1125–1133. https://doi.org/10.1177/1359105316687631
- Andersson, G., Paxling, B., Roch-Nordlund, P., Östman, G., Norgren, A., Almlöv, J., Georén, L., Breitholtz, E., Dahlin, M., Cuijpers, P., Carlbring, P., & Silverberg, F. (2012). Internet-based psychodynamic versus cognitive behavioral guided self-help for generalized anxiety disorder: A randomized controlled trial. Psychotherapy and Psychosomatics, 81(6), 344–355. https://doi.org/10.1159/000339371
- Andersson, G., & Titov, N. (2014). Advantages and limitations of Internet-based interventions for common mental disorders. World Psychiatry, 13(1), 4–11. https://doi.org/10.1002/wps.20083
- Andersson, G., Titov, N., Dear, B. F., Rozental, A., & Carlbring, P. (2019). Internet-delivered psychological treatments: From innovation to implementation. World Psychiatry, 18(1), 20–28. https://doi.org/10.1002/wps.20610
- Bas-Sarmiento, P., Saucedo-Moreno, M. J., Fernández-Gutiérrez, M., & Poza-Méndez, M. (2017). Mental health in immigrants versus native population: A systematic review of the literature. Archives of Psychiatric Nursing, 31(1), 111–121. https://doi.org/10.1016/j.apnu.2016.07.014
- Bastien, C. H., Vallières, A., & Morin, C. M. (2001). Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Medicine, 2(4), 297–307. https://doi.org/10.1016/S1389-9457(00)00065-4
- Choi, I., Zou, J., Titov, N., Dear, B. F., Li, S., Johnston, L., Andrews, G., & Hunt, C. (2012). Culturally attuned internet treatment for depression amongst Chinese Australians: A randomised controlled trial. Journal of Affective Disorders, 136(3), 459–468. https://doi.org/10.1016/j.jad.2011.11.003
- Chu, J., & Leino, A. (2017). Advancement in the maturing science of cultural adaptations of evidence-based interventions. Journal of Consulting and Clinical Psychology, 85(1), 45–57. https://doi.org/10.1037/ccp0000145
- Cohen, S., Kamarck, T., & Mermelstein, R. (1983). A global measure of perceived stress. Journal of Health and Social Behavior, 24(4), 385–396. https://doi.org/10.2307/2136404
- Davey, C., Heard, R., & Lennings, C. (2015). Development of the Arabic versions of the impact of events scale- revised and the posttraumatic growth inventory to assess trauma and growth in middle eastern refugees in Australia. Clinical Psychologist, 19(3), 131–139. https://doi.org/10.1111/cp.12043
- Ebert, D. D., Buntrock, C., Lehr, D., Smit, F., Riper, H., Baumeister, H., Cuijpers, P., & Berking, M. (2018). Effectiveness of web- and mobile-based treatment of subthreshold depression with adherence-focused guidance: A single-blind randomized controlled trial. Behavior Therapy, 49(1), 71–83. https://doi.org/org.e.bibl.liu.se/10.1016/j.beth.2017.05.004
- Enders, C. K. (2010). Applied missing data analysis. Guilford Press.
- Fazel, M., Wheeler, J., & Danesh, J. (2005). Prevalence of serious mental disorder in 7000 refugees resettled in western countries: A systematic review. Lancet, 365(9467), 1309–1314. https://doi.org/10.1016/S0140-6736(05)61027-6
- Feingold, A. (2009). Effect sizes for growth-modeling analysis for controlled clinical trials in the same metric as for classical analysis. Psychological Methods, 14(1), 43–53. https://doi.org/10.1037/a0014699
- Fernandez, E., Salem, D., Swift, J. K., & Ramtahal, N. (2015). Meta‐analysis of dropout from cognitive behavioral therapy: Magnitude, timing, and moderators. Journal of Consulting and Clinical Psychology, 83(6), 1108–1122. https://doi.org/10.1037/ccp0000044
- Furukawa, T. A., Noma, H., Caldwell, D. M., Honyashiki, M., Shinohara, K., Imai, H., Chen, P., Hunot, V., & Churchill, R. (2014). Waiting list may be a nocebo condition in psychotherapy trials: A contribution from network meta‐analysis. Acta Psychiatrica Scandinavica, 130(3), 181–192. https://doi.org/10.1111/acps.12275
- Gilliver, S. C., Sundquist, J., Li, X., & Sundquist, K. (2014). Recent research on the mental health of immigrants to Sweden: A literature review. European Journal of Public Health, 24(suppl 1), 72–79. https://doi.org/10.1093/eurpub/cku101
- Halaj, A., & Huppert, J. D. (2017). Middle east. In S. Hofman (Ed.), International perspectives on psychotherapy (pp. 219–239). Springer International Publishing.
- Heber, E., Ebert, D. D., Lehr, D., Cuijpers, P., Berking, M., Nobis, S., & Riper, H. (2017). The benefit of web- and computer-based interventions for stress: A systematic review and meta-analysis corresponding author. Journal of Medical Internet Research, 19(2), e32. https://doi.org/10.2196/jmir.5774
- Hesser, H. (2015). Modeling individual differences in randomized experiments using growth models: Recommendations for design, statistical analysis and reporting of results of internet interventions. Internet Interventions, 2(2), 110–120. https://doi.org/10.1016/j.invent.2015.02.003
- Hollander, A. C., Dal, H., Lewis, G., Magnusson, C., Kirkbride, J. B., & Dalman, C. (2016). Refugee migration and risk of schizophrenia and other non-affective psychoses: Cohort study of 1.3 million people in Sweden. BMJ (Online), 352, 1–8. https://doi.org/10.1136/bmj.i1030
- Huey, S. J., Tilley, J. L., Jones, E. O., & Smith, C. A. (2014). The contribution of cultural competence to evidence-based care for ethnically diverse populations. Annual Review of Clinical Psychology, 10(1), 305–338. https://doi.org/10.1146/annurev-clinpsy-032813-153729
- Ince, B. Ü., Cuijpers, P., Van’T Hof, E., Van Ballegooijen, W., Christensen, H., & Riper, H. (2013). Internet-based, culturally sensitive, problem-solving therapy for Turkish migrants with depression: Randomized controlled trial. Journal of Medical Internet Research, 15(10), 1–15. https://doi.org/10.2196/jmir.2853
- Jacobson, N. S., & Truax, P. (1991). Clinical significance: A statistical approach to defining meaningful change in psychotherapy research. Journal of Consulting and Clinical Psychology, 59(1), 12–19. https://doi.org/10.1037//0022-006x.59.1.12
- Johansson, R., Hesslow, T., Karlsson, J., Karlsson, J., Karlsson, J., Karlsson, J., Karlsson, J., Hesser, H., Frederick, R. J., Lilliengren, P., Carlbring, P., & Andersson, G. (2017). Internet-based affect-focused psychodynamic therapy for social anxiety disorder: A randomized controlled trial with 2-year follow-up. Psychotherapy, 54(4), 351–360. https://doi.org/10.1037/pst0000147
- Kirmayer, L. J., Narasiah, L., Munoz, M., Rashid, M., Ryder, A. G., Guzder, J., Hassan, G., Rousseau, C., & Pottie, K. (2011). Common mental health problems in immigrants and refugees: General approach in primary care. CMAJ: Canadian Medical Association Journal, 183(12), E959–E967. https://doi.org/10.1503/cmaj.090292
- Knaevelsrud, C., Brand, J., Lange, A., Ruwaard, J., & Wagner, B. (2015). Web-based psychotherapy for posttraumatic stress disorder in war-traumatized Arab patients: Randomized controlled trial. Journal of Medical Internet Research, 17(3), e71. https://doi.org/10.2196/jmir.3582
- Kwok, O., West, S. G., & Green, S. B. (2007). The impact of misspecifying the within-subject covariance structure in multiwave longitudinal multilevel models: A monte carlo study. Multivariate Behavioral Research, 42(3), 557–592. https://doi.org/10.1080/00273170701540537
- Laban, C. J., Gernaat, H. B., Komproe, I. H., Schreuders, B. A., & De Jong, J. (2005). Impact of a long asylum procedure on the prevalence of psychiatric disorders in Iraqi asylum seekers in The Netherlands. Journal of Nervous and Mental Disorders, 192(12), 843–851. https://doi.org/10.1097/01.nmd.0000146739.26
- Lindegaard, T., Brohede, D., Koshnaw., K., Sherzad Osman, S., Johansson, R., & Andersson, G. (2019). Internet-based treatment of depressive symptoms in a Kurdish population: A randomized controlled trial. Journal of Clinical Psychology, 75(6), 985–998. https://doi.org/10.1002/jclp.22753
- Lindner, P., Andersson, G., Öst, L.-G., & Carlbring, P. (2013). Validation of the internet-administered quality of life inventory (QOLI) in different psychiatric conditions. Cognitive Behaviour Therapy, 42(4), 315–327. https://doi.org/10.1080/16506073.2013.806584
- Lindner, P., Frykheden, O., Forsström, D., Andersson, E., Ljótsson, B., Hedman, E., Andersson, G., & Carlbring, P. (2016). The brunnsviken brief quality of life scale (BBQ): Development and psychometric evaluation. Cognitive Behaviour Therapy, 45(3), 182–195. https://doi.org/10.1080/16506073.2016.1143526
- Löwe, B., Decker, O., Müller, S., Brähler, E., Schellberg, D., Herzog, W., & Herzberg, P. (2008). Validation and standardization of the generalized anxiety disorder screener (GAD-7) in the general population. Medical Care, 46(3), 266–274. https://doi.org/10.1097/MLR.0b013e318160d093
- Löwe, B., Kroenke, K., Herzog, W., & Gräfe, K. (2004). Measuring depression outcome with a brief self-report instrument: Sensitivity to change of the patient health questionnaire (PHQ-9). Journal of Affective Disorders, 81(1), 61–66. https://doi.org/10.1016/S0165-0327(03)00198-8
- Muthén, L. K., & Muthén, B. O. (2017). Mplus user’s guide (8th ed.). Muthén & Muthén. https://doi.org/org/
- Nagayama Hall, G. C., Ibaraki, A. Y., Huang, E. R., Marti, C. N., & Stice, E. (2016). A meta-analysis of cultural adaptations of psychological interventions. Behavior Therapy, 47(6), 993–1014. https://doi.org/10.1016/j.beth.2016.09.005
- Nygren, T., Berg, M., Sarkohi, A., & Andersson, G. (2018). Development of an internet-based cognitive behavioral therapy self-help program for Arabic-speaking immigrants: Mixed-methods study. JMIR Research Protocols, 7(12), e11872. https://doi.org/10.2196/11872
- Parkvall, M. (2018). Arabiska Sveriges näst största modersmål [Arabic Sweden’s second largest native language]. https://www.svd.se/arabiska-sveriges-nast-storsta-modersmal/av/mikael-parkvall
- Păsărelu, C. R., Andersson, G., Bergman, N. L., & Dobrean, A. (2017). Internet-delivered transdiagnostic and tailored cognitive behavioral therapy for anxiety and depression: A systematic review and meta-analysis of randomized controlled trials. Cognitive Behavioral Therapy, 46(1), 1–28. https://doi.org/10.1080/16506073.2016.1231219
- Porter, M., & Haslam, N. (2005). Predisplacement and postdisplacement factors associated with mental health of refugees and internally displaced persons: A meta-analysis. The Journal of the American Medical Association, 294(5), 610–612. https://doi.org/10.1001/jama.294.5.602
- Reinert, D. F., & Allen, J. P. (2007). The alcohol use disorders identification test: An update of research findings. Alcoholism: Clinical and Experimental Research, 31(2), 185–199. https://doi.org/10.1111/j.1530-0277.2006.00295.x
- Rozental, A., Boettcher, J., Andersson, G., Schmidt, B., & Carlbring, P. (2015). Negative effects of internet interventions: A qualitative content analysis of patients’ experiences with treatments delivered online. Behaviour Therapy, 44(3), 223–236. https://doi.org/10.1080/16506073.2015.1008033
- Saunders, J. B., Aasland, O. G., Babor, T. F., de la Fuente, J. R., & Grant, M. (1993). Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption. Addiction, 88(6), 791–804. https://doi.org/10.1111/j.1360-0443.1993.tb02093.x
- Sawaya, H., Atoui, M., Hamadeh, A., Zeinoun, P., & Nahas, Z. (2016). Adaptation and initial validation of the patient health questionnaire - 9 (PHQ-9) and the generalized anxiety disorder - 7 questionnaire (GAD-7) in an Arabic speaking lebanese psychiatric outpatient sample. Psychiatry Research, 239, 245–252. https://doi.org/10.1016/j.psychres.2016.03.030
- Schafer, J. L., & Graham, J. W. (2002). Missing data: Our view of the state of the art. Psychological Methods, 7(2), 147–177. https://doi.org/10.1037/1082-989X.7.2.147
- Seyffert, M., Lagisetty, P., Landgraf, J., Chopra, V., Pfeiffer, P. N., Conte, M. L., Rogers, M. A. M., & Ferri, R. (2016). Internet-delivered cognitive behavioral therapy to treat insomnia: A systematic review and meta-analysis. PLoS One, 11(2), e0149139. https://doi.org/10.1371/journal.pone.0149139
- Silfvernagel, K., Westlinder, A., Andersson, S., Bergman, K., Hernandez, R. D., Fallhagen, L., Andersson, S., Lundqvist, I., Masri, N., Viberg, L., Forsberg, M.-L., Lind, M., Berger, T., Carlbring, P., & Andersson, G. (2018). Individually tailored internet-based cognitive behaviour therapy for older adults with anxiety and depression: A randomised controlled trial. Cognitive Behaviour Therapy, 47(4), 286–300. https://doi.org/10.1080/16506073.2017.1388276
- Silove, D., Sinnerbrink, I., Field, A., Manicavasagar, V., & Steel, Z. (1997). Anxiety, depression and PTSD in asylum-seekers: Assocations with pre-migration trauma and post-migration stressors. British Journal of Psychiatry, 170(4), 351–357. https://doi.org/10.1192/bjp.170.4.351
- Spitzer, R. L., Kroenke, K., & Williams, J. W. (1999). Validation and utility of a self-report version of PRIME-MD. The PHQ primary care study. JAMA: Journal Of The American Medical Association, 282(18), 1737–1744. https://doi.org/10.1001/jama.282.18.1737
- Spitzer, R. L., Kroenke, K., Williams, J. W., & Löwe, B. (2006). A brief measure for assessing generalized anxiety disorder: The GAD-7. Archives of Internal Medicine, 166(10), 1092–1097. https://doi.org/10.1001/archinte.166.10.1092
- Statistics Sweden (2018). Folkmängd efter födelseland 1900-2017 [Inhabitants by country of birth 1900-2017]. https://www.scb.se/hitta-statistik/statistik-efter-amne/befolkning/befolkningens-sammansattning/befolkningsstatistik/pong/tabell-och-diagram/helarsstatistik–riket/folkmangd-efter-fodelseland/
- Steel, Z., Chey, T., Silove, D., Marnane, C., Bryant, R. A., & van Ommeren, M. (2009). Association of torture and other potentially traumatic events with mental health outcomes among populations exposed to mass conflict and displacement: A systematic review and meta-analysis. JAMA, 302(5), 537–549. https://doi.org/10.1001/jama.2009.1132
- Suleiman, K. H., & Yates, B. C. (2011). Translating the insomnia severity index into Arabic. Journal of Nursing Scholarship, 43(1), 49–53. https://doi.org/10.1111/j.1547-5069.2010.01374.x
- Swedish Migration Agency (2017). Statistik [Statistics]. https://www.migrationsverket.se/Om-Migrationsverket/Statistik.html
- Tasca, G. A., & Gallop, R. (2009). Multilevel modeling of longitudinal data for psychotherapy researchers: I. the basics. Psychotherapy Research, 19(4–5), 429–437. https://doi.org/10.1080/10503300802641444
- The Swedish National Board of Health and Welfare. (2013). För låg tillgång till psykologisk behandling [too low access to psychological treatment]. https://www.socialstyrelsen.se/nyheter/2013juni/forlagtillgangtillpsykologiskbehandling
- Tinghög, P., Malm, A., Arwidson, C., Sigvardsdotter, E., Lundin, A., & Saboonchi, F. (2017). Prevalence of mental ill health, traumas and postmigration stress among refugees from Syria resettled in Sweden after 2011: A population-based survey. BMJ Open, 7(12), e018899. https://doi.org/10.1136/bmjopen-2017-018899
- UNHCR (2016). UNHCR viewpoint: ‘Refugee’ or ‘migrant’ – Which is right?”. https://www.unhcr.org/55df0e556.html
- Van Ballegooijen, W., Cuijpers, P., Van Straten, A., Karyotaki, E., Andersson, G., Smit, J. H., Riper, H., & García, A. V. (2014). Adherence to internet‐based and face‐to‐face cognitive behavioural therapy for depression: A meta‐analysis. PLoS One, 9(7), e100674. https://doi.org/10.1371/journal.pone.0100674
- Vlaescu, G., Alasjö, A., Miloff, A., Carlbring, P., & Andersson, G. (2016). Features and functionality of the Iterapi platform for internet‐based psychological treatment. Internet Interventions, 6, 107–114. https://doi.org/10.1016/j.invent.2016.09.006
- Wang, J., & Wang, X. (2012). Structural equation modeling: applications using Mplus. Wiley.
- Weiss, D., & Marmar, C. (1997). The impact of event scale -revised. In J. Wilson & T. Keane (Eds.), Assessing psychological trauma and PTSD (pp. 399–411). Guildford.
- World Health Organiation (2018). Report on the health of refugees and migrants in the WHO European Region: No public health without refugee and migrant health. https://apps.who.int/iris/bitstream/handle/10665/311347/9789289053846-eng.pdf?sequence=1&isAllowed=y