ABSTRACT
This study investigates boys’ awareness and thoughts about human papillomavirus (HPV) and HPV vaccination, perceived benefits of vaccinating men, information sources and intention to be vaccinated against HPV. We used a qualitative approach and interviews were conducted with 31 upper secondary school male students. Two main themes 1) Promotion of equal health and 2) Increased knowledge facilitates the decision about HPV vaccination emerged from the analysis. The informants believed that it was important and fair to protect boys and girls equally against HPV. If HPV vaccination could prevent both girls and boys against an HPV-related disease, there was nothing to question or to discuss. It was not a matter of sex; it was a matter of equal rights. Moreover, an important reason for vaccinating boys was to prevent the transmission of the virus. However, the boys felt unsure and stated that they needed to know more. The school nurse and the school health were considered suitable both for distributing information and for providing the vaccinations.
In conclusion, the participants were in favor of introducing HPV vaccination also for boys in the national vaccination program. Sex-neutral HPV vaccinations were viewed both as a way to stop the virus transmission and a means to promote equal health for the entire population.
Introduction
Human papillomavirus (HPV) is one of the most prevalent sexually transmitted infections (STIs) and an underlying cause of a considerable part of the global cancer burden.Citation1 The high-risk HPV types (mainly HPV 16 and 18) can cause lesions that may progress to cancer in both women and men. Cervical cancer is the most common HPV associated cancer among women, whereas boys are often carriers of the virus and are more frequently affected by HPV associated tonsillar and base of tongue squamous cell carcinoma, two diseases that have increased immensely in incidence during recent decades. In addition, in males HPV is related to penile and anal cancer, and both sexes are affected by genital warts.Citation2–Citation6
Many countries worldwide have implemented national HPV vaccination programs. There is a wide variation of vaccine uptake although school-based vaccination programs usually are more efficient.Citation7 In Sweden, girls are mainly offered the quadrivalent vaccine protecting against the most common HPV types (6, 11, 16 and 18). The vaccine has been offered free of charge in the national school-based vaccination program since 2012. Girls 10–12 years of age are the primary target group and girls up to 18 years of age can be offered the vaccine as a catch-up vaccination. School nurses are responsible for all aspects of the HPV vaccinations, including information to parents and pupils, obtaining informed consent from the former, as well as the actual administration of the vaccine. The written information distributed by the nurses is standardized by the government. There is an ongoing discussion about also including boys in the national vaccination program, a strategy to which both the Public Health Agency of Sweden and the school nurses are in favor.Citation8–Citation10
Globally, most national HPV vaccination programs only include girls. However, sex-neutral (gender neutral) vaccinations are considered important and cost-effective cancer-preventive effortsCitation11–Citation13 and are thus recommended by several countries such as Australia, Austria, Barbados, Israel, Liechtenstein, Switzerland, USA and Canada.Citation12 The inclusion of boys in national vaccination programs is in line with the United Nations Convention on the Rights of the Child and the national public health goal of equal health for the entire population.Citation14,Citation15
Several factors are important for acceptance of and attitudes towards HPV vaccination. Among such factors are parental (individual) beliefs, trust in vaccine safety, general vaccine attitudes (i.e. previous acceptance of childhood vaccinations), cultural norms and values related to sexual activity, as well as socio-demographic factors. Healthcare providers (HCPs), i.e. medical doctors and nurses, play a crucial role in successful HPV vaccination programs, especially as regards the provision of information and addressing vaccine hesitancy.Citation16–Citation22
Previous European and American studies indicate low HPV knowledge among adolescents.Citation23–Citation26 According to a systematic review there are also gender differences, boys being less knowledgeable than girls.Citation27 A qualitative UK study gave similar results.Citation28
Recently, we conducted a cluster randomized controlled study with the overall aim to improve primary prevention of HPV infection by promoting vaccination and increased condom use among upper secondary school students.Citation29 The intervention had favorable effects on the adolescents’ beliefs and at follow-up after three months more girls in the intervention group were vaccinated than among the controls. There were also gender differences: boys had lower scores regarding perceived risk (susceptibility) and perceived severity of HPV-related diseases.Citation29
In order to implement a successful national vaccination program, it is essential to explore beliefs among the general population, adolescent boys included. Few studies have been conducted on the beliefs and attitudes of this group, and more specifically about extending the national vaccination program to include boys. So far, almost all studies on males have addressed male college/university students or men who have sex with men.Citation30–Citation33 Since there is little previous knowledge, our aim was to explore awareness and thoughts about HPV and HPV vaccination, information sources, perceived benefits of vaccinating men, and intention to be vaccinated in a group of male upper secondary school students.
Methods
Design
The present study is a qualitative study using semi-structured interviews analyzed by content analysis according to Burnard, and part of the project ‘Prevention of HPV in a school-based setting’Citation29 (trial registration/ClinicalTrials.gov Identifier: NCT02280967). We used the Health Belief Model (HBM) to discuss our findings, described below. In the present manuscript, the term awareness is used as the ability to directly know and perceive, to feel, or to be cognizant of HPV and HPV vaccination. The study follows Standards for Reporting Qualitative ResearchCitation34 and is reported according to COREQ Checklist (Supplemental File).Citation35
Setting, procedure and sample
Sweden is a country of 10 million inhabitants, about 24% of who are first or second generation immigrants. Almost all (95.2% autumn 2017) 16–19-year-olds attend upper secondary school, which comprises theoretical and vocational programs.
The participating boys were selected from a larger sample, described in Grandahl et al.Citation19,Citation29 The three schools chosen represented different geographical areas in central Sweden and included students of different socio-demographic status. The schools offered vocationally, as well as theoretically oriented education. Eligible were boys in the third year of upper secondary school, and were students at the schools that participated in the educational intervention ‘Prevention of HPV in a school-based setting’.Citation19,Citation29 The school nurses approached the boys and asked if they were willing to participate. In total 34 boys agreed to participate, and 31 boys were finally included in the study. Two boys did not participate due to absence from school, and one boy did not show up for the interview. The sample size is based on previous research about low knowledge and awareness about HPV and HPV vaccination, especially among adolescents’ boys in Sweden.Citation19,Citation23,Citation29,Citation36,Citation37 Moreover, we knew that it could be challenging to interview young boys and that the boys might not be so talkative, and that the interviews might be superficial.Citation38,Citation39 Thus, we estimated that we needed to complete about 20–25 interviews before saturation (no new information is revealed during additional interviews). After about 25 interviews, nothing new came up during the interviews, but to be sure that we did not miss any thoughts in the subject we completed another six interviews. No new information was revealed and consequently we had reached saturation powerCitation40 and fulfilled our aim to explore boys’ beliefs and thoughts on the subject.Citation40
Each interview started with verbal information about the aim of the study and the boys were asked to complete a brief background questionnaire focusing on demographics, sexual debut, and HPV vaccination status. Only the researcher (MG or CS) and the informant were present during the interview, which took place in a separate room at the school. The interviews were audio-recorded and lasted in general between 30 and 45 minutes. The boys received a cinema ticket in return for their participation. Interviews were conducted between February 2017 and April 2017, and each interview was transcribed verbatim soon thereafter. No repeated interviews were carried out. The interviewers were PhDs and registered specialist nurses with ample previous experience of the method, the age group of the informants, as well as the topics at hand.Citation34,Citation35
Interview guide
We used a semi-structured interview guide described in . The interview guide is based on the literature,Citation20–Citation22,Citation25–Citation27,Citation31,Citation33,Citation36,Citation37,Citation41 i.e. previous studies in the subject as well as our clinical experience. For validity, we discussed the interview guide in the research group (specialists in HPV virology, pediatrics, adolescents’ sexual health and public health) and with the Public Health Agency of Sweden. Some minor changes were made to the interview guide after these discussions. To make sure the adolescents understood the questions we tested the interview guide on four adolescents’ prior to the study. No changes were made to the interview guide. In summary, the questions focused on the informant’s beliefs concerning HPV and HPV vaccination as well as STIs and vaccinations in general.
Table 1. Interview guide.
Analysis
Since little is known about boys’ beliefs and views of HPV, HPV vaccination and the proposed inclusion of boys in the Swedish national vaccination program, we used an inductive approach and no predetermined theory was considered in the analysis. However, we used HBM theory to understand and discuss the findings.
The interviews were analyzed using thematic content analysis according to Burnard.Citation42 We read the transcripts several times in order to get an overall picture of what was said. Notes, which function as the initial codes, were made in the margin of the transcripts. The codes were then extracted from the transcripts, and a reduction of the number of codes was made by removing duplicates. Categorization was then done by grouping together overlapping or related codes. The transcripts were then read again, and units of information were sorted into suitable categories. Two researchers (MG and CS) individually read the transcripts and identified categories. The process was rigorous and systematic, and the researchers returned to the transcripts to make sure that all data were thoroughly analyzed. All researchers (authors) took part in discussing the categories and themes until a consensus was reached. We did not use any specific software in the analysis. However, we used Excel© to manage the data. An example of the analytical process is presented in .
Table 2. Example of the analytic process.
The criteria for assessing the quality and trustworthiness of the conducted studies, as described by Guba and Lincoln,Citation43 including credibility, dependability, confirmability, and transferability were considered. The results were presented as close to the wordings of the original interviews as possible, and quotations were included to enhance trustworthiness of the analyzed data. The informants did not provide feedback on the results, but respondent validation was performed at the end of each interview when the researcher summarized what the boys had said to ensure that the information had been understood correctly.Citation43,Citation44
The Health Belief Model (HBM)
HBM is useful in understanding factors that influence health behavior and is widely used in studies on beliefs about HPV vaccination.Citation45,Citation46 HBM includes the following central constructs: perceived susceptibility, perceived severity, perceived benefit and perceived barriers. Furthermore, socio-demographic factors such as age, sex, ethnicity and parental education, as well as knowledge, are recognized as factors that indirectly can influence the individual’s behavior. Important concepts in the theory are cues to action, which can motivate individuals to alter their behavior, and self-efficacy – the ability of the individual to perform certain behavior.Citation47
Ethical considerations
We conducted the study according to the Declaration of Helsinki.Citation48 All participants received oral and written information before giving their written consent. The participants were informed that participation was voluntary, that they could withdraw at any time, for any or no given reason, without incurring any negative consequences for themselves. They were also informed that only the researchers would have access to the data and that all data would be presented on a group level. No previous relationship between the researcher and the informant existed. Contact details to the researchers were provided in case of further questions. We asked permission to conduct the study from both the head of the school health in each municipality and from the heads of the individual schools.Citation49 Approval was acquired from The Regional Ethical Review Board of Uppsala University (D.nr.2013/324).
Results
A total of 31 male upper secondary school students (Median age = 18 years) participated in this study. The boys followed both vocational (n = 17) and theoretical (n = 14) programs. Most boys (n = 25/31) were born in Sweden by parents born in Sweden. Six of the boys had an immigrant background. Seven out of 31 had not had their sexual debut, while 24/31 had experienced sexual intercourse. We approached non-HPV vaccinated males, and none of the participating boys was vaccinated against HPV.
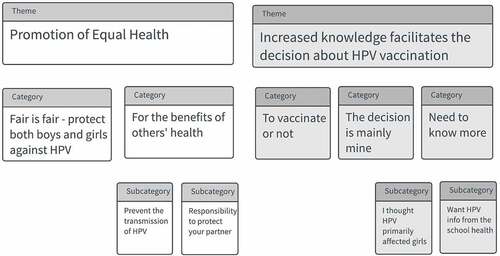
The analysis resulted in two main themes describing the boys’ beliefs about HPV vaccination: 1) Promotion of equal health and 2) Increased knowledge facilitates the decision about HPV vaccination. Each theme consisted of two or three categories, which are presented below and illustrated by quotes. See for an overview of themes and categories.
Promotion of equal health
Fair is fair – protect both girls and boys against HPV
The boys believed that it was important and just to give boys and girls equal protection against HPV. It was considered unfair to only vaccinate girls if boys also could be affected. If the vaccine could protect both girls and boys against an HPV-related disease, there was nothing to question or to discuss: it was not a matter of sex but of equality and equal health.
They believed girls were prioritized due to their risk of cervical cancer and for that reason it was considered accurate to start the vaccination among girls since they were more affected. However, if the vaccine had the same effects among girls and boys, it was beneficial if boys also were included in the national vaccination program.
“If boys can be affected by HPV, then I do not understand why they are not yet offered [the vaccine]. Yes, if the vaccine has a better effect in girls, I may understand that boys are not given priority, but if the vaccine is effective in both … or if both may get ill, then it is clear that both should have access to the vaccine. Anyway, that’s what I think.” #10
For the benefits of others’ health
Prevent the transmission of HPV
To include boys in the national vaccination program was considered beneficial. The most important reason for vaccinating boys was to prevent and stop virus transmission. Vaccinating boys will help prevent a growing number of HPV-related diseases in the population at large. It was important to vaccinate boys in order to help others and protect those from being affected by diseases.
“The main reasons for vaccinating boys? Yes, but it would definitely be to stop the virus from spreading. That’s because everybody is helped if it would go away. Cancer is terrible if it should happen to anyone, regardless of it being a man or a woman. And if you eradicate all forms of it, the faster the better, I’m for it. So that’s why I would like to consider taking the vaccine, if it works.” #11
Responsibility to protect your partner
The boys had different opinions regarding STI prevention. It was considered important to prevent STIs for the sake of the health of both partners. They believed that boys and girls were equally responsible for STI prevention. You had a personal responsibility. It was considered natural to talk about prevention when having sex. However, it was stated that it was easier for girls to talk about these matters. When you were in a relationship you should agree on who is going to use contraception.
“It’s really for both, it fully depends on the girl really, if she is on the pill and then maybe she thinks that you don’t need a condom and then you don’t have to. But then if she’s not, then obviously, you can’t force her to take the pill if she doesn’t want to, then you just have to put it on. So it’s up to both.” #16
If you became infected you had the responsibility to inform your partner. You should be honest and let your partner know. The boys expressed that you always knew and you could feel if you had an STI. Furthermore, the responsibility to protect the partner was thought to be greater for boys than girls. However, sometimes you do not have time to think. If the girl is not on contraceptives, you should use a condom in order to avoid pregnancy. Still, opinions and experiences differed regarding condom use among the informants, as well as whether they believed their friends used it or not. During the interviews, it was revealed that the boys hardly ever used condoms unless they perceived a risk of getting an STI. In addition, if the vaccine prevented HPV infection, HPV vaccination could be helpful in decreasing risks and then it would be less important to use a condom. The condom was considered less enjoyable and was not used if the person you had sex with was known beforehand.
Increased knowledge facilitates the decision about HPV vaccination
To vaccinate or not
The boys were mainly in favor of vaccinations overall and presumed that they were vaccinated according to the general childhood vaccination program. Still, they were unaware of which diseases they were vaccinated against. Moreover, boys who had migrated from other countries had received some additional vaccinations upon arrival in Sweden, but again they were not sure against which diseases.
The informants were in favor of vaccinating against HPV, mainly to prevent cancer. They believed boys also should be covered. Vaccinations were considered beneficial and most boys would accept the vaccine if it was offered. The time aspect was also mentioned; it was important to be vaccinated before it was too late. During the interviews it was stated that they did not see any negative aspects of the vaccination, except that the vaccine might contribute to increased sexual risk-taking. If they were vaccinated they would feel safe and protected. The boys emphasized that they did not want to get an HPV-related disease. Moreover, it was considered better to vaccinate to prevent against an STI instead of treating the actual disease.
“…in that case I only see the benefits. As long as the effect is proven and there are no harmful side effects, then I have nothing against it. It’s just fine then, so I am in favor:” #19
However, some boys were unsure about the vaccine and some were not in favor of vaccinations overall. Moreover, emotional aspects regarding previous vaccinations were mentioned, and fear of needles were stated as a barrier for future vaccinations. An individualized approach from healthcare staff was specified as a factor bridging this barrier.
“…I have needle phobia so I wouldn’t take it. But if I didn’t have that then I would have taken it” #10
“Well, since I don’t know so much I think I would decline. If I had more knowledge then I would have some more freedom of choice.” #17
The safety of the vaccine was a main factor and it was considered important to receive information and gain knowledge about potential side-effects. They wanted to read about the vaccine and increase their research-based knowledge about benefits and barriers before making the decision. It was considered better to vaccinate later, when there would be more knowledge about the vaccine. However, if there were no potential side effects they were in favor of vaccinating.
The decision is mainly mine
Various opinions regarding the decision-making process were revealed during the interviews. The boys stated that the decision was their own to make. They had confidence in themselves and they would not be affected by the opinion of others, neither parents nor friends. Parents did not have a mandate to decide about their lives any longer and consequently they would neither discuss the vaccine with them nor ask for their advice on the subject. Neither would they discuss the vaccine with friends nor would friends’ opinions influence their own decision.
“Well, what I feel is… myself I’m quite open with my parents, but this is perhaps not something you discuss with them. It’s sort of my own decision”…”But if you’re somewhat younger then I think you actually need support from your parents as well, and hear what they think” #6
On the other hand, the opinions of family and friends were important for some boys and would influence their decision. It was considered beneficial if parents were involved in the decision and read the information about the vaccine. These boys were in favor of discussing the vaccine with both parents. However, the preferment of one parent was also given, depending on the informant’s family relations. In addition, parents’ beliefs regarding vaccinations in general had an impact. Parents were supposed to be in favor of vaccinating although a few boys revealed that their parents were not. The boys also believed that most friends would accept the vaccine, if offered. One boy preferred to wait and see what others would do and make his decision thereafter.
“If mum says ‘you should take the vaccine’ then I will do it. Because all of the family does it, yes, if they do then I will as well.” #13
Need to know more
I thought HPV primarily affected girls
The boys had low awareness of the virus and the vaccine and expressed that they needed more information. They stated that they hardly knew anything about HPV and were unsure if HPV was an STI, since the virus was not mentioned during sexual health education in school.
“No, actually, I don’t know what it [HPV] is.” #5
“I would like to above all get information about what it protects against, what … I mean which risks you run and which diseases that this can cause, more about how common it is, …and preferably also comparisons with potential side effects from the vaccine… so that I sort of can understand the benefits and drawbacks of taking the vaccine.” #18
The boys who had received the extra HPV-information (in connection with the educational intervention) during the general health interview with the school nurse stated that this was the only time that they had heard about the virus and the vaccine. They had appreciated the information and considered it appropriate for this occasion. Moreover, the school nurse and school health services were considered adequate arenas for information about HPV and HPV vaccination. However, the boys who had received the extra information expressed that they hardly remembered anything. Still, even though the boys had low awareness of the virus and the HPV vaccine, they were aware of a vaccine against cervical cancer.
There were different views regarding HPV being a female disease or not. The boys thought HPV vaccination was associated with cervical cancer. They had briefly heard about the vaccine in connection with the girls being offered the vaccine in primary school at age 11–12. It was obvious that the boys thought that the virus only or mostly affected girls, whereas other boys believed that HPV was common and could affect everyone. It was also mentioned that there were many different HPV types. However, they believed the virus was more severe when it affected girls.
”Well, to think about… what I’ve heard, what’s its name cervical cancer. Then you think that this is for girls. But yes, if it turns up that guys can also be affected, it makes you wonder.” #8
Want HPV information from the school health
The boys felt unsure and stated that they needed to know more about HPV and HPV vaccination. They preferred to receive the information from someone trustworthy and who had good knowledge on the subject. As mentioned above, the school nurse and school health services were considered suitable information sources. School-based vaccinations were also considered convenient, and it would feel safe to be vaccinated in school by the school nurse. Teachers, primary care centers and midwives working at youth clinics were also mentioned as trustworthy sources of information. It was considered more uncertain to search information online and “to google”. In addition, national e-health webpages such as youth clinic online (UMO.se) and the national care guide (Vårdguiden 1177.se), were regarded as suitable for information about these topics. The informants had different views as to whether information about HPV should be given individually, in group, and/or both and whether it should be given face-to-face and/or in writing. However, it was considered important to receive the information early, starting at primary school, and then repeatedly in different ages.
”That’s fine, here at school or… I know that we have been given lots of information about other sexually transmitted infections, but this has sort of… because this, by you, was the first time I got to know about this so it’s hardly anything that’s… then also, I don’t think you easily stumble upon it on the internet in that way. It’s more like something you need to tell the full population about so that they know it. So at school I think surely, it’s a very good place for that.” #18
Discussion
The central finding of the study is that the participating boys were in favor of vaccination against HPV. They perceived benefits for themselves and would accept the vaccine if it was offered free of charge in the national vaccination program. This is largely in line with previous findings among adolescents and young men.Citation50,Citation51 Still, there were also barriers and some boys had the opposite opinion and were unsure about the vaccine, and one boy stated that he would decline. Vaccine safety concerns and fear of side effects are well-known main barriers for HPV vaccination.Citation21,Citation37 Moreover, fear of needles, was revealed during the interviews. Even if the informants were in favor of vaccinating it should be noticed that there is a difference between beliefs, i.e. intention to vaccinate and actual health behavior, which is in accordance with the tenets of the HBM.Citation47
Notably, boys perceived benefits and would accept the vaccine mainly for altruistic reasons, i.e. for the good of others, to promote public health, and to prevent cancer. It was also a matter of equal rights, especially since boys could also be affected by an HPV associated disease. The ongoing discussion in media (and among politicians) about the goal of equal health for the population might have acted as a cues-to-action and influenced these responses.
The boys had high self-efficacy and were generally convinced the decision on vaccinations would be entirely their own. It was considered convenient and safe to be vaccinated in school, by the school nurse. This echoes the views of both parents and school nurses which we have previously explored.Citation8,Citation9,Citation36 In Sweden, school nurses are the providers and responsible for all aspects of the vaccinations and are available in the schools on a regular basis. Consequently, the school nurse is often a well-known and trusted person among the students. Moreover, school nurses are advocates of children’s health and often a primary source of information about HPV.Citation36,Citation37,Citation52–Citation55 Studies also show that health professionals in general play an important role regarding vaccinations and can act as positive triggers, cues to action, for the decision to vaccinate.Citation56,Citation57
The boys had low susceptibility for contracting an HPV-related disease and were unaware of the link between sexual behavior and HPV-infections. They would vaccinate rather than use a condom. This might reflect the findings in a previous qualitative study among young males in Sweden. The boys did not have health concerns in relation to unprotected sex, perceived low risk for an STI, and preferred not to use condomsCitation38. Moreover, this low susceptibility was in line with previous studies, as well as our own findings in this age group, who often exhibit the vicious combination of high-risk sexual behavior and low HPV awareness.Citation19,Citation23,Citation29 A previous study also shows that boys are less concerned about condom use than girls.Citation58 Traditional norms for male behavior during various stages of the life course might contribute to the boys’ beliefs about sexual risk-taking and low susceptibility for an HPV-infection.Citation59,Citation60 According to gender norms, sexual and reproductive health is considered a female responsibility.Citation59,Citation60 Thus, boys do not feel a need to worry about STI protection and perceive low severity. Still, the participating boys believed that it would be fair and just to vaccinate both boys and girls. They were concerned about the health of others and wanted boys to take their responsibility regarding sexual and reproductive health and thus contribute to more equal health in the society at large. The majority of the participant boys were sexually active, and it is well known that optimal protection against HPV-related disease occurs when vaccination is administered prior to sexual debut. Consequently, it is important to highlight the importance of vaccination to young boys before sexual debut. Therefore, the findings from this study may lend a more unique perspective to the utility of a sex-neutral catch-up vaccination policy in upper secondary schools. In addition, sex-neutral catch-up vaccinations can contribute to the global aim of eliminating HPV-related cancer, starting with the elimination of cervical cancer.
The boys had misconceptions regarding STIs, such as the belief that you can feel if you have an infection. This barrier is not surprising, given the low HPV awareness and knowledge shown in previous studies.Citation23–Citation28 However, it is encouraging that they emphasized that they wanted to know more. They preferred to receive information from someone with good knowledge about HPV, such as the school nurse. The boys who had received extra HPV information two years earlierCitation29 believed it was accurate to inform about this in school and in connection with the general health interview with the school nurse. Still, during the interviews it was revealed that boys who had received this extra HPV-information had largely forgotten what they were told.
Interventions can increase awareness and knowledge and promote favorable beliefs about HPV and HPV vaccination among adolescents on a short-term basis.Citation29,Citation61,Citation62 However, as stated by the boys themselves, the information needs to be repeated and started at an early age. Consequently, even though one single educational intervention, such as the one we earlier performed, Citation29 has favorable short-term effects it is not sufficient in the long run. According to the Health Belief Model (HBM) knowledge is a modifying factor for the individual health beliefs and the actual health behavior.Citation47 The low perceived risk and low knowledge about severity implies the need to start education about HPV early and reinforce it with repetition is necessary in a public health perspective. Even though sexual education is mandatory in school, this does not include information about HPV on a regular basis. Thus, information about HPV needs to be included. This is in accordance with the WHO recommendation about sexuality education in EuropeCitation63 and in the best interest of the individual child as stated in United Nations Convention on the Rights of the Child.Citation14
Strengths and limitations
The interviewers (the authors MG and CS) are specialists both regarding the scientific field (sexual and reproductive health, adolescents’ health) and regarding the qualitative method chosen. The criteria for assessing the quality and trustworthiness of the conducted studies as described by Guba and LincolnCitation43 were considered: credibility, dependability, conformability and transferability. Credibility (internal validity) was obtained by continuously analyzing the data, preliminary categories and the interpretations of others (stakeholders). Confirmability refers to objectivity or neutrality aiming to measure the degree of interpretation from the data and not from the researcher’s interpretations and biases. In order to avoid lone researcher bias two authors individually read the transcripts and identified the categories. The categories and themes were discussed among the authors to gain consensus. In order to gain dependability (reliability, the stability of the data over time and over conditions), the analytical process was rigorous and systematic; the researchers returned to the transcripts to make sure that all the data were thoroughly analyzed. Transferability (generalizability) refers to the extent to which the results can be transferred to other settings. The results have been presented as closely to the original interviews as possible with representative quotations included, as this strengthens transferability.Citation43
The included boys represented schools situated in different socioeconomic and geographic areas and attended both theoretical and vocational programs. This brought a wide perspective to bear on the subject. The boys had low awareness about HPV and HPV vaccination which can make the topic difficult to talk about. However, the knowledge is low overall among adolescents in Sweden so we believe the results are not affected by low awareness. Still, the results might have been slightly different with other informants. It should also be noted that few of the included boys had an immigrant background, and further research should include immigrant boys. The sample size, 31 boys, was sufficient to reach saturation and to provide a better understanding of the informants’ perspectives. As in all qualitative research, the aim is not to generalize; the results may however be transferable to other societies similar to Sweden.
Conclusions and future directions
The participants were in favor of receiving HPV vaccination as part of the national school-based vaccination program. Sex-neutral HPV vaccination was viewed both as a way to stop the virus transmission and a matter of equal health. Still, awareness about the virus was insufficient and there is an urgent need for more information directed to boys. This education should start early, preferably in primary school, and be given repeatedly as the child grows.
Acknowledgments
We thank all the participating boys. A special thanks to the school nurses and the principals of the schools.
Additional information
Funding
References
- Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal AT. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65(2):87–108. doi:10.3322/caac.21262.
- Forman D, de Martel C, Lacey CJ, Soerjomataram I, Lortet-Tieulent J, Bruni L, Vignat J, Ferlay J, Bray F, Plummer M, et al. Global burden of human papillomavirus and related diseases. Vaccine. 2012; 30(Suppl 5): F12–23.doi:10.1016/j.vaccine.2012.07.055.
- Du J, Nordfors C, Ahrlund-Richter A, Sobkowiak M, Romanitan M, Nasman A, Andersson S, Ramqvist T, Dalianis T. Prevalence of oral human papillomavirus infection among youth, Sweden. Emerg Infect Dis. 2012;18(9):1468–1471. doi:10.3201/eid1809.111731.
- Chaturvedi AK, Engels EA, Pfeiffer RM, Hernandez BY, Xiao W, Kim E, Jiang B, Goodman MT, Sibug-Saber M, Cozen W, et al. Human papillomavirus and rising oropharyngeal cancer incidence in the United States. J Clin Oncol. 2011; 29(32): 4294–4301.doi:10.1200/JCO.2011.36.4596.
- Machalek DA, Grulich AE, Jin F, Templeton DJ, Poynten IM. The epidemiology and natural history of anal human papillomavirus infection in men who have sex with men. Sex Health. 2012;9(6):527–537. doi:10.1071/SH12043.
- Young D, Xiao CC, Murphy B, Moore M, Fakhry C, Day TA. Increase in head and neck cancer in younger patients due to human papillomavirus (HPV). Oral Oncol. 2015; 51(8): 727–730. doi: 10.1016/j.oraloncology.2015.03.015.
- Bruni L, Diaz M, Barrionuevo-Rosas L, Herrero R, Bray F, Bosch FX, de Sanjose S, Castellsague X. Global estimates of human papillomavirus vaccination coverage by region and income level: a pooled analysis. Lancet Glob Health. 2016;4(7):e453–63. doi:10.1016/S2214-109X(16)30099-7.
- Grandahl M, Larsson M, Tyden T, Stenhammar C. School nurses’ attitudes towards and experiences of the Swedish school-based HPV vaccination programme - A repeated cross sectional study. PLoS ONE. 2017;12(4):e0175883. doi:10.1371/journal.pone.0175883.
- Grandahl M, Tyden T, Rosenblad A, Oscarsson M, Neveus T, Stenhammar C. School nurses’ attitudes and experiences regarding the human papillomavirus vaccination programme in Sweden: a population-based survey. BMC Public Health. 2014;14:.540. doi:10.1186/1471-2458-14-540.
- Public Health Agency of Sweden [Folkhälsomyndigheten]. Human papilloma virus vaccination of boys in the Swedish national vaccination programme - support for a governmental decision 2017. Report number: 01596-2017. [accessed 2018 Aug 30]. https://www.folkhalsomyndigheten.se/publicerat-material/publikationsarkiv/b/beslutsunderlag-om-hpv-vaccination-av-pojkar-i-det-nationella-vaccinationsprogrammet/.
- Wolff E, Elfstrom KM, Haugen Cange H, Larsson S, Englund H, Sparen P, Roth A. Cost-effectiveness of sex-neutral HPV-vaccination in Sweden, accounting for herd-immunity and sexual behaviour. Vaccine. 2018. doi:10.1016/j.vaccine.2018.07.018.
- Prue G. Vaccinate boys as well as girls against HPV: it works, and it may be cost effective. BMJ. 2014;349:.g4834. doi:10.1136/bmj.g4834.
- Lehtinen M, Luostarinen T, Vanska S, Soderlund-Strand A, Eriksson T, Natunen K, Apter D, Baussano I, Harjula K, Hokkanen M, et al. Gender-neutral vaccination provides improved control of human papillomavirus types 18/31/33/35 through herd immunity: results of a community randomised trial (III). Int J Cancer. 2018; 10.1002/ijc.31618.
- UNICEF. Convention on the Rights of the Child 2015 [updated November 4, 2014], [accessed 2018 Aug 2]. http://www.unicef.org/crc/index_30160.html.
- Beauchamp T, Childress J. Principles of Biomedical Ethics. 6th ed. Oxford, UK: Oxford University Press; 2009.
- Hansen BT, Campbell S, Burger E, Nygard M. Correlates of HPV vaccine uptake in school-based routine vaccination of preadolescent girls in Norway: A register-based study of 90,000 girls and their parents. Prev Med. 2015;77:.4–10. doi:10.1016/j.ypmed.2015.04.024.
- Slåttelid Schreiber S, Juul K, Dehlendorff C, Kjær SK. Socioeconomic Predictors of Human Papillomavirus Vaccination Among Girls in the Danish Childhood Immunization Program. J Adolesc Health. 2015;56(4):402–407. doi:10.1016/j.jadohealth.2014.12.008.
- Grandahl M, Chun Paek S, Grisurapong S, Sherer P, Tyden T, Lundberg P. Parents’ knowledge, beliefs, and acceptance of the HPV vaccination in relation to their socio-demographics and religious beliefs: A cross-sectional study in Thailand. PLoS ONE. 2018;13(2):e0193054. doi:10.1371/journal.pone.0193054.
- Grandahl M, Larsson M, Dalianis T, Stenhammar C, Tyden T, Westerling R, Neveus T. Catch-up HPV vaccination status of adolescents in relation to socioeconomic factors, individual beliefs and sexual behaviour. PLoS ONE. 2017;12(11):e0187193. doi:10.1371/journal.pone.0187193.
- Ferrer HB, Trotter C, Hickman M, Audrey S. Barriers and facilitators to HPV vaccination of young women in high-income countries: a qualitative systematic review and evidence synthesis. BMC Public Health. 2014;14:.700. doi:10.1186/1471-2458-14-700.
- Ogilvie G, Anderson M, Marra F, McNeil S, Pielak K, Dawar M, McIvor M, Ehlen T, Dobson S, Money D, et al. A population-based evaluation of a publicly funded, school-based HPV vaccine program in British Columbia, Canada: parental factors associated with HPV vaccine receipt. PLoS Med. 2010; 7(5): e1000270.doi:10.1371/journal.pmed.1000270.
- Tung IL, Machalek DA, Garland SM, Attitudes K. Factors associated with human papillomavirus (hpv) vaccine uptake in adolescent girls and young Women in Victoria, Australia. PLoS ONE. 2016;11(8):e0161846. doi:10.1371/journal.pone.0161846.
- Mattebo M, Grun N, Rosenblad A, Larsson M, Haggstrom-Nordin E, Dalianis T, Tyden T. Sexual experiences in relation to HPV vaccination status in female high school students in Sweden. Eur J Contracept Reprod Health Care. 2014;19(2):86–92. doi:10.3109/13625187.2013.878021.
- Carlson LM, Gonzalez S. Knowledge of cervical cancer pathology of high school students in San Carlos, Costa Rica. Rev Biol Trop. 2014;62(3):877–886.
- Marek E, Dergez T, Rebek-Nagy G, Kricskovics A, Kovacs K, Bozsa S, Kiss I, Ember I, Gocze P. Adolescents’ awareness of HPV infections and attitudes towards HPV vaccination 3 years following the introduction of the HPV vaccine in Hungary. Vaccine. 2011;29(47):8591–8598. doi:10.1016/j.vaccine.2011.09.018.
- Sopracordevole F, Cigolot F, Gardonio V, Di Giuseppe J, Boselli F, Ciavattini A. Teenagers’ knowledge about HPV infection and HPV vaccination in the first year of the public vaccination programme. Eur J Clin Microbiol Infect Dis. 2012;31(9):2319–2325. doi:10.1007/s10096-012-1571-4.
- Patel H, Jeve YB, Sherman SM, Moss EL. Knowledge of human papillomavirus and the human papillomavirus vaccine in European adolescents: a systematic review. Sex Transm Infect. 2016;92(6):474–479. doi:10.1136/sextrans-2015-052341.
- Hilton S, Patterson C, Smith E, Bedford H, Hunt K. Teenagers’ understandings of and attitudes towards vaccines and vaccine-preventable diseases: a qualitative study. Vaccine. 2013;31(22):2543–2550. doi:10.1016/j.vaccine.2013.04.023.
- Grandahl M, Rosenblad A, Stenhammar C, Tyden T, Westerling R, Larsson M, Oscarsson M, Andrae B, Dalianis T, Neveus T. School-based intervention for the prevention of HPV among adolescents: a cluster randomised controlled study. BMJ Open. 2016;6(1):e009875. doi:10.1136/bmjopen-2015-009875.
- Gerend MA, Madkins K, Phillips G 2nd, Mustanski B. Predictors of human papillomavirus vaccination among young men who have sex with men. Sex Transm Dis. 2016;43(3):185–191. doi:10.1097/OLQ.0000000000000408.
- Cummings T, Kasting ML, Rosenberger JG, Rosenthal SL, Zimet GD, Stupiansky NW. Catching up or missing out? human papillomavirus vaccine acceptability among 18- to 26-year-old men who have sex with men in a us national sample. Sex Transm Dis. 2015;42(11):601–606. doi:10.1097/OLQ.0000000000000358.
- Cheung T, Lau JTF, Wang JZ, Mo PKH, Ho YS. Acceptability of HPV vaccines and associations with perceptions related to HPV and HPV vaccines among male baccalaureate students in Hong Kong. PLoS ONE. 2018;13(6):e0198615. doi:10.1371/journal.pone.0198615.
- Fontenot HB, Fantasia HC, Vetters R, Zimet GD. Increasing HPV vaccination and eliminating barriers: recommendations from young men who have sex with men. Vaccine. 2016;34(50):6209–6216. doi:10.1016/j.vaccine.2016.10.075.
- O’Brien BC, Harris IB, Beckman TJ, Reed DA, Cook DA. Standards for reporting qualitative research: a synthesis of recommendations. Acad Med. 2014;89(9):1245–1251. doi:10.1097/ACM.0000000000000388.
- Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi:10.1093/intqhc/mzm042.
- Gottvall M, Grandahl M, Hoglund AT, Larsson M, Stenhammar C, Andrae B, Tyden T. Trust versus concerns-how parents reason when they accept HPV vaccination for their young daughter. Ups J Med Sci. 2013;118(4):263–270. doi:10.3109/03009734.2013.809039.
- Grandahl M, Oscarsson M, Stenhammar C, Neveus T, Westerling R, Tyden T. Not the right time: why parents refuse to let their daughters have the human papillomavirus vaccination. Acta Paediatr. 2014;103(4):436–441. doi:10.1111/apa.12545.
- Ekstrand M, Tyden T, Larsson M. Exposing oneself and one’s partner to sexual risk-taking as perceived by young Swedish men who requested a Chlamydia test. Eur J Contracept Reprod Health Care. 2011;16(2):100–107. doi:10.3109/13625187.2010.549253.
- Ekstrand Ragnar M, Grandahl M, Stern J, Mattebo M. Important but far away: adolescents’ beliefs, awareness and experiences of fertility and preconception health. Eur J Contracept Reprod Health Care. 2018;23(4):265–273. doi:10.1080/13625187.2018.1481942.
- Malterud K, Siersma VD, Guassora AD. Sample Size in Qualitative Interview Studies: guided by Information Power. Qual Health Res. 2015. doi:10.1177/1049732315617444.
- Hilton S, Smith E. “I thought cancer was one of those random things. I didn’t know cancer could be caught…”: adolescent girls’ understandings and experiences of the HPV programme in the UK. Vaccine. 2011;29(26):4409–4415. doi:10.1016/j.vaccine.2011.03.101.
- Burnard P, Gill P, Stewart K, Treasure E, Chadwick B. Analysing and presenting qualitative data. Br Dent J. 2008;204(8):429–432. doi:10.1038/sj.bdj.2008.292.
- Guba E, Lincoln Y. Fourth Generation Evaluation. Newbury Park (CA): Sage publications; 1989.
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: concepts, procedures and measures to achieve trustworthiness. Nurse Educ Today. 2004;24(2):105–112. doi:10.1016/j.nedt.2003.10.001.
- Donadiki EM, Jimenez-Garcia R, Hernandez-Barrera V, Sourtzi P, Carrasco-Garrido P, Lopez de Andres A, Jimenez-Trujillo I, Eg V. Health belief model applied to non-compliance with HPV vaccine among female university students. Public Health. 2014. doi:10.1016/j.puhe.2013.12.004.
- Krawczyk A, Perez S, King L, Vivion M, Dube E, Rosberger Z. Parents’ decision-making about the human papillomavirus vaccine for their daughters: II. Qualitative results. Hum Vaccin Immunother. 2015;11(2):330–336. doi:10.4161/21645515.2014.980708.
- Champion VL, Skinner Sugg C. The Health Belief Model. In: Glantz. K, BarbaraK. R, Viswanath K editors. Health behavior and health education: theory, resaearch and practice. 4th. San Fransisco (CA. USA): Jossey-Bass; 2008; (pp. 45–65).
- WMA Declaration of Helsinki - Ethical Principles for Research Involving Human Subjects: World Medical Association; 2008 [accessed 2017 Apr 10]. http://www.wma.net/en/30publications/10policies/b3/index.html.
- CODEX rules and guidelines for research Uppsala, Sweden: CODEX, Centre for Research Ethics & Bioethics; 2015 [accessed 2017 Sep 2]. http://www.codex.vr.se/en/manniska1.shtml.
- Marra E, Alberts CJ, Zimet GD, Paulussen TGWM, Heijman T, Hogewoning AA, Sonder GJB, Fennema JS, Hjc DV, Schim van der Loeff MF. HPV vaccination intention among male clients of a large STI outpatient clinic in Amsterdam, the Netherlands. Papillomavirus Res. 2016;2:.178–184. doi:10.1016/j.pvr.2016.11.001.
- Gottvall M, Larsson M, Hoglund AT, Tydén T. High HPV vaccine acceptance despite low awareness among Swedish upper secondary school students. Eur J Contracept Reprod Health Care. 2009;14(6):399–405. doi:10.3109/13625180903229605.
- Hilton S, Hunt K, Bedford H, Petticrew M. School nurses’ experiences of delivering the UK HPV vaccination programme in its first year. BMC Infect Dis. 2011;11:.226. doi:10.1186/1471-2334-11-226.
- Boyce T, Holmes A. Addressing health inequalities in the delivery of the human papillomavirus vaccination programme: examining the role of the school nurse. PLoS ONE. 2012;7(9):e43416. doi:10.1371/journal.pone.0043416.
- Brabin L, Stretch R, Roberts SA, Elton P, Baxter D, McCann R. The school nurse, the school and HPV vaccination: a qualitative study of factors affecting HPV vaccine uptake. Vaccine. 2011;29(17):3192–3196. doi:10.1016/j.vaccine.2011.02.038.
- Rosen BL, Ashwood D, Richardson GB. School nurses’ professional practice in the HPV vaccine decision-making process. J Sch Nurs. 2016;32(2):138–148. doi:10.1177/1059840515583312.
- Barnack JL, Reddy DM, Swain C. Predictors of parents’ willingness to vaccinate for human papillomavirus and physicians’ intentions to recommend the vaccine. Womens Health Issues. 2010; 20(1):28–34. doi:10.1016/j.whi.2009.08.007.
- Scott K, Batty ML. HPV vaccine uptake among Canadian youth and the role of the nurse practitioner. J Community Health. 2016;41(1):197–205. doi:10.1007/s10900-015-0069-2.
- Rich A, Mullan BA, Sainsbury K, Kuczmierczyk AR. The role of gender and sexual experience in predicting adolescent condom use intentions using the theory of planned behaviour. Eur J Contracept Reprod Health Care. 2014;19(4):295–306. doi:10.3109/13625187.2014.917624.
- West C, Zimmerman DH. Doing Gender. Nouvelles Questions Feministes. 2009;28(3):34-+. doi:10.3917/nqf.283.0034.
- Connell R. Gender, health and theory: conceptualizing the issue, in local and world perspective. Soc Sci Med. 2012;74(11):1675–1683. doi:10.1016/j.socscimed.2011.06.006.
- Gottvall M, Tyden T, Hoglund AT, Larsson M. Knowledge of human papillomavirus among high school students can be increased by an educational intervention. Int J STD AIDS. 2010;21(8):558–562. doi:10.1258/ijsa.2010.010063.
- Marek E, Dergez T, Rebek-Nagy G, Szilard I, Kiss I, Ember I, Gocze P, D’Cruz G. Effect of an educational intervention on Hungarian adolescents’ awareness, beliefs and attitudes on the prevention of cervical cancer. Vaccine. 2012;30(48):6824–6832. doi:10.1016/j.vaccine.2012.09.012.
- WHO. Standards for sexuality education in Europe Cologne2010 [accessed 2017 Aug 20]. http://www.bzga-whocc.de.