Abstract
The issue of international migration and health has received increased attention since its rise due to empirical studies on the immigrant paradox. Less examined has been research focused on countries in the Global South with growing immigrant population share and contentious debates on implications. Using data from the longitudinal National Income Dynamics Study (NIDS) (2008–2017) and panel logistic regression this study focused on evaluating whether reported physical health, mental health, and life satisfaction are all associated with immigrant status in South Africa. Accounting for several sociodemographic factors, results emanating from analysis showed no significant evidence of association between overall immigration status and self-reported health or life satisfaction. This however did not apply to depression as immigrants were found to be significantly less likely to report depressive level scores. Interestingly, preference to migrate was also found to be significantly associated with depression, and life satisfaction. Further evaluation amongst racial groups showed that African immigrants are also significantly more likely to report better health than non-immigrant counterparts. This study argues for the need of contextualisation of the immigrant paradox as evidence thereof varies dependent on specific outcomes and communities. The importance of other associated social determinants of wellbeing is also highlighted since gender, race, age, class, education, relationship status, location, and behavioural factors were found to be significantly associated with wellbeing. Policies should thus be aimed at reducing structural inequalities in broad whilst also introducing social programmes that reduce behavioural or lifestyle activities that have negative implications on wellbeing.
Introduction
Lipoma is the most frequent soft tissue tumor and it can occur wherever there is fat tissue [Citation1] This type of tumor affects mostly women, particularly in their trunks, upper limbs and cervical region [Citation2]. it is estimated that about 1% of global population has a lipoma [Citation3]. Many lipomas are small with diameter of 1-3 cm, but they can enlarge beyond 10 cm and in these cases they are named ‘giant lipoma’ [Citation4, Citation5]. Giant lipomas can cause compression of the veins and then chronic venous insufficiency in particular if they are located in the limbs.
The authors reported a case of giant lipoma sited in left femoral fossa which caused femoral vessels compression.
Case report
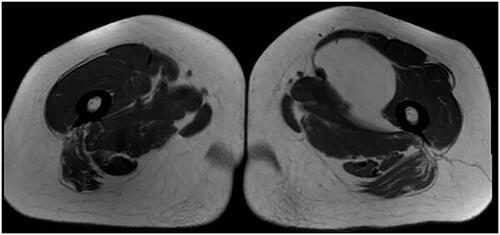
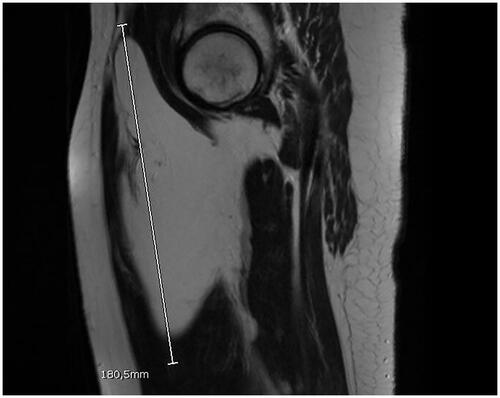
A 56-year-old woman was referred to our department of district general hospital due to the presence of a large mass which was located on the left thigh. The lesion had been steadily increased in size during the last five years. The patient had reported pain, functional impairment and cutaneous oedema during the last 6 months. There was an episode of deep vein thrombosis of right leg in 1998 treated with Warfarin for 6 months. No substance abuse was referred. Previous surgical procedures and chronic pathologies were not reported. On physical examination, a moderate oedema of the left thigh was noted without skin impairment. A lateral displacement of abductor muscles and rectus femoris was noted. No pharmacological allergies were reported. Doppler sonography was performed and further investigated with MRI. ( and ).
Deep vein thrombosis, venous reflux and lymphadenopathy were not detected. Tumor caused compression of the femoral vein without venous obstruction. Radiological aspects suggested a lipoma.
The cross section of the tumor size was 10 cm × 8 cm with an 18 cm long axis length.
The patient underwent surgical procedure of lipoma removal. The surgical equipe included a consultant and a junior trainee two years of surgical resident training. Surgeons planned a possible reconstruction of the artery, vein or femoral nerve which was not needed. Within the femoral fossa, surgeons identified a well demarcated and encapsulated mass. Tumor was dissected out and the vein was decompressed. Lipoma weighed 1,705 g. Two drains were put in aspiration. Histopathology evaluation showed a well circumscribed mass of fatty tissue reported as benign lipoma. The postoperative period was uneventful and after two days of recovery the patient was discharged. Patient was allowed to move with crutches for 6 days. After six months patient was fully satisfied.
Discussion
Although lipomas are common, giant lipomas are relatively rare, especially those that cause symptomatic venous compression [Citation6]. The largest lipoma was reported in 1894; it weighed 22.7 kg and was located on the left scapula of a young man [Citation7]. Lipoma removal is a procedure which usually doesn’t require great surgical skills [Citation8]. This consideration can lead surgeon to underestimate possible surgical complications. The aim of this article is to report our experience about inferior limbs giant lipoma throughout the following considerations.
A well skilled surgeon should lead the surgical procedure. Despite lipomas removal can be performed by unskilled surgeon such as residents, in case of giant lipoma, a consultant is required for the management of possible vascular complications [Citation9].
A detailed radiological investigation should be performed in preoperative time. Soft tissues lipomatous lesions arise from a broad range of tissues and range from benign to malignant. It is mandatory to diagnose possible malignancy [Citation10]. An evaluation of tumor extension and anatomical relationship is fundamental. Surgeon should study the possible impairment of femoral vessels. This could also be suspected during clinical evaluation if vein obstruction signs are noted [Citation6].
Lipoma removal could be performed using helium plasma device or ultrasonic cutting and coagulating device. In our experience [Citation11, Citation12] these technologies gave minor thermal trauma to vessels. Further advantages of these devices including tissue dissection and hemostasis at the same time, no eschar formation over the blade, minimal thermal damage, no smoke formation, no risk of electrical injury, and possibility of use in patients with pacemaker [Citation13]. Its use has been successfully applied in minimally invasive laparoscopic procedures and in head and neck surgery [Citation14].
Radical excision is the principal aim [Citation15]. Some authors suggest that lipoma can be removed throughout laser-assisted procedure [Citation16] but in our opinion surgical treatment is the only therapeutic path, in particular for giant lipoma.
Giant mass removal from thigh leads to extended dead space formation [Citation17]. This virtual cavity could be the setting of hematoma or seroma. In order to avoid these complications, it is suggested to place two drains (one in deep layer and the other in the superficial one). Drains should be kept until their output is below 50 cc in 24 hours [Citation18].
Postoperative compressive dressing is not mandatory to prevent surgical site bleeding or seroma formation [Citation19]. According to the literature [Citation20] we suggest to use a compressive zinc dressing in order to decrease wound complications.
It is important to avoid patient’s leg mobilization and load for at least 5 post-operative days. Differences in seroma or hematoma rates depending on length of immobilization were not found [Citation21–23].
If giant lipoma affects the superficial layer, skin can be stretched with cutaneous thickness reduction. After lipoma asportation skin necrosis’ risk is increased. In order to prevent wound dehiscence, it can be applied negative pressure dressing [Citation24].
Conclusion
Giant lipoma of the thigh is an uncommon pathological condition. Despite little lipomas can usually be treated as outpatients, giant lipomas have to be planned in surgical operatory theatre. Radiological examination is mandatory in order to safety perform the procedure. The possible compression of femoral vessel has to be investigated through pre-operative clinical examination. A careful asportation and accurate post-operative cares are at the basis of a safe procedure with low rate of complications.
Author contributions
Conceptualization: Marta Starnoni, Marco Pappalardo and Giorgio De Santis; Writing original draft preparation: Federico De Maria and Caterina Marra, Data analysis: Claudio Gio Francesco Blessent, Federico De Maria and Caterina Marra. All the authors reviewed, discussed and agree with the final version of the manuscript.
Disclosure statement
Author declares that none have commercial associations (e.g. consultancies, stock ownership, equity interest, patent/licensing arrangement etc.) that might pose a conflict of interest in connection with the submitted article
References
- Rydholm A, Berg NO. Size, site and clinical incidence of lipoma: factors in the differential diagnosis of lipoma and sarcoma. Acta Orthop Scand. 1983;54(6):1–5. doi: 10.3109/17453678308992936.
- Born G. Gigantic lipomas. Plast Reconstr Surg. 1995;96(7):1750–1751. doi: 10.1097/00006534-199512000-00055.
- Tamkus S, Gusho CA, Colman M, et al. A single institutional experience treating adipocytic tumors: incidence, disease-related outcomes, and the clinical significance of MDM2 analysis. Orthop Rev (Pavia). 2020;12(3):8818. doi: 10.4081/or.2020.
- Terzioglu A, Tuncali D, Yuksel A, et al. Giant lipomas: a series of 12 consecutive cases and a giant liposarcoma of the thigh. Dermatol Surg. 2004;30(3):463–467. doi: 10.1111/j.1524-4725.2004.30022.x.
- Aydoğdu ESER, Yýldýrým S, Eker G, et al. Giant lipoma of the back. Dermatologic Surg. 2004;30(1):121–122. doi: 10.1111/j.1524-4725.2004.30026.x.
- Wronski K, Lachowki A. Giant femoral lipoma causing venous obstructing syndrome case report. Ann Ital Chir. 2013;86(4):368–370. http://www.ncbi.nlm.nih.gov/pubmed/26344372.
- Guler O, Mutlu S, Mahirogulları M. Giant lipoma of the back affecting quality of life. Ann Med Surg (Lond). 2015;4(3):279–282. doi: 10.1016/j.amsu.2015.08.001.
- Abensour M, Jeandel C, Heid E. [Cutaneous lipoma and lipomatosis]. Ann Dermatol Venereol. 1987;114(6-7):873–882. http://www.ncbi.nlm.nih.gov/pubmed/3314627.
- Starnoni M, Pinelli M, Porzani S, et al. Standardization and selection of high-risk patients for surgical wound infections in plastic surgery. Plast Reconstr Surg Glob Open. 2021;9(3):e3472. doi: 10.1097/GOX.0000000000003472.
- Burt AM, Huang BK. Imaging review of lipomatous musculoskeletal lesions. Sicot J. 2017;3:34. doi: 10.1051/sicotj/2017015.
- Starnoni M, Pinelli M, De Santis G. Setting of helium plasma device (J-Plasma) in flap elevation. J Vasc Surg Cases Innov Tech. 2020;6(3):446. doi: 10.1016/j.jvscit.2020.07.008.
- Pinelli M, Starnoni M, De Santis G. The use of cold atmospheric plasma device in flap elevation. Plast Reconstr Surg Glob Open. 2020;8(5):e2815. doi: 10.1097/GOX.0000000000002815.
- Starnoni M, De Santis G, Pinelli M. Fibula free flap elevation without tourniquet: are harmonic scalpel shears useful?. Plast Reconstr Surg - Glob Open. 2019;7(9):e2409. doi: 10.1097/GOX.0000000000002409.
- Masghati S, Pedroso J, Gutierrez M, et al. Comparative thermal effects of J-Plasma®, monopolar, argon, and laser electrosurgery in a porcine tissue model. Surg Technol Int. 2019;34:35–39. http://www.ncbi.nlm.nih.gov/pubmed/30825320.
- Starnoni M, De Santis G, Pasini R, et al. Diagnosis and treatment of upper eyelid lipoma: a case report. Am J Ophthalmol Case Rep. 2020;20:100874. doi: 10.1016/j.ajoc.2020.100874.
- Goldman A, Wollina U. Lipoma treatment with a subdermal nd: YAG laser technique. Int J Dermatol. 2009;48(11):1228–1232. doi: 10.1111/j.1365-4632.2008.04007.x.
- Elswick SM, Curiel DA, Wu P, et al. Complications after thigh sarcoma resection. J Surg Oncol. 2020;121(6):945–951. doi: 10.1002/jso.25830.
- Janis JE, Khansa L, Khansa I. Strategies for postoperative seroma prevention. Plast Reconstr Surg. 2016;138(1):240–252. doi: 10.1097/PRS.0000000000002245.
- Christoffersen MW, Olsen BH, Rosenberg J, et al. Randomized clinical trial on the postoperative use of an abdominal binder after laparoscopic umbilical and epigastric hernia repair. Hernia. 2015;19(1):147–153. doi: 10.1007/s10029-014-1289-6.
- Thompson CB, Wiemken TL, Brown TS. Effect of postoperative dressing on excisions performed on the leg: a comparison Between zinc oxide compression dressings Versus standard wound care. Dermatol Surg. 2017;43(11):1379–1384. doi: 10.1097/DSS.0000000000001209.
- Pan X-F, Huan J-L, Qin X-J. Potential risk factors for the development of seroma following mastectomy with axillary dissection. Mol Clin Oncol. 2015;3(1):222–226. doi: 10.3892/mco.2014.430.
- Abe M, Iwase T, Takeuchi T, et al. A randomized controlled trial on the prevention of seroma after partial or total mastectomy and axillary lymph node dissection. Breast Cancer. 1998;5(1):67–69. doi: 10.1007/BF02967417.
- Schultz I, Barholm M, Gröndal S. Delayed shoulder exercises in reducing seroma frequency after modified radical mastectomy: a prospective randomized study. Ann Surg Oncol. 1997;4(4):293–297. doi: 10.1007/BF02303577.
- Ge D. The safety of Negative-Pressure wound therapy on surgical wounds. Adv Skin Wound Care. 2018;31(9):421–428. doi: 10.1097/01.ASW.0000542530.71686.5c.