ABSTRACT
In a welcome return to a live, in person, same space meeting, albeit with some participants joining virtually, the Fifteenth Annual European Continuing Medical Education (CME) Forum (#15ECF) was hosted in Barcelona, Spain,2-4 November 2022. The meeting began with sessions conducted by three special interest groups affiliated with the European CME Forum, but open to all registrants. The main part of the meeting comprised interactive discussion sessions conducted by presenters from North and South America, Europe, India, and Australia, which were interspersed with breakout workshops that tackled three themes, Innovation and Impact, Attitudes and Culture, and Environment and Community. A featured topic was the patient voice in education and insights were provided by the international delegates on their local frameworks for CME/CPD. Updates were also provided on harmonisation among international accreditors, and an important change to the Journal of European CME, that is closely linked to the European CME Forum, was announced. An oral presentation was made by one of the poster authors, and the perennial favourites “Lunch with the Learners” and the “CME Unsession” werealso included. The level of engagement displayed by the participants would seem to suggest that much of the recent fatigue associated with virtual meetings was mitigated by this live event.
Since its inception in 2008 the European CME Forum has provided a “public square” for the free exchange of ideas and views on current issues related to CME/CPD across borders in Europe and beyond. Over the years the annual meeting has been hosted in various European cities, London (six times), Amsterdam and Manchester (twice each), Berlin and Dublin (once each) and, after an extended period of “Zoom gloom” brought on by having to conduct the 2020 and 2021 meetings in a virtual format due to the COVID-19 pandemic, there was a palpable sense of relief among attendees able to participate in educational and networking sessions in a shared physical space at the 2022 meeting in Barcelona (#15ECF). Some of the sessions were also streamed live to online participants.
Participants were charged with re-evaluating European and global CME-CPD and gathered to consider a different theme on each of the meeting’s three days:
• Day One: Innovation and Impact,
• Day Two: Attitudes and Culture,
• Day Three: Environment and Community.
Discussion of these themes was preceded by sessions conducted by groups that regularly attend the meetings, namely the Good CME Practice Group (https.gcmep.org), the International Pharmaceutical Alliance for Medical Education (iPACME) and a joint session between the Biomedical Alliance in Europe (https.biomedeurope.org) and the AC Forum (www.acforum.net). These groups represented education providers, industry, speciality societies and conference managers. These activities have come to be known as “Day 0” sessions and, in keeping with the Forum’s policy of transparency and interactivity, have been opened to all interested registrants at the meeting.
The opening session of the 15th European CME Forum began with a welcome by its Director, Eugene Pozniak, who outlined the history of the Forum and the range of stakeholders that have participated over the years. He defined the emerging purpose of the meeting as providing a means for interactivity and discussion on “how to do CME/CPD better” and sharing best practices with particular emphasis on the main responses from the annual survey conducted before and after each meeting. The survey results had indicated that more emphasis should be placed on Diversity, Equity and Inclusion and this was set as a fundamental principle for the meeting. The removal of silo thinking and provision of an equal voice for all stakeholders was acknowledged and having explained that there were still barriers to interprofessional CPD in Europe, Pozniak was happy to note that the only group excluded from the meeting were paid speakers! The technology tweaks for 2022 were the use of catch-box microphones (see ) to eliminate any need for standing microphones and the linkage of QR codes for inhouse and virtual participants to access online question and answer, and polling facilities for the meeting. Attendees were also provided with a complimentary registration for the e-book version of Robin Stevenson’s handbook Learning and Behaviour in Medicine: A Voyage Around CME and CPD [Citation1].
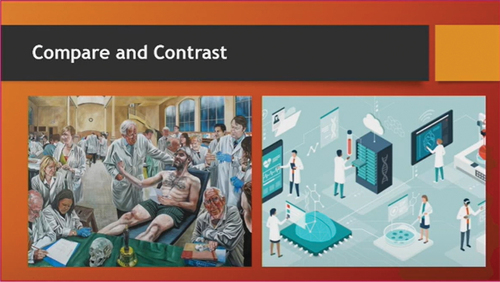
Proceedings then moved to a moderated interactive session led by Kathy Chappell (American Nurses Credentialing Center) and several members of the editorial team for the 2022 Special Collection of articles in the Journal of European CME (JECME) that is closely affiliated with the European CME Forum, the collection having focused on the Day 1 theme of Innovation and Impact. Participants were asked to view an illustration of two different scenarios as shown in and comment on their perceptions of how each represented their view of what CME/CPD might be.
Views that emerged included:
A lack of diversity in each scenario
Patient-centric care (left) versus technology (right)
Emotion (left) and sterility (right)
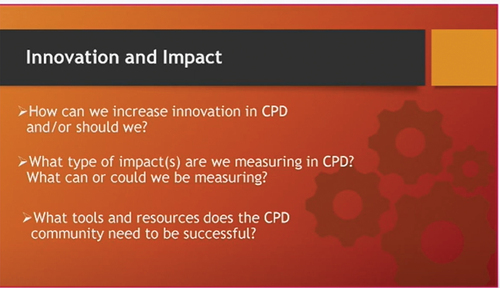
Three groups, including the virtual audience then considered the following questions derived from the 2022 Special Collection as shown in .
Feedback from the groups provided consensus on:
The need to define innovation – not just disruption to current practice, nor just enhanced use of technology,
Ideally education providers should be moving towards measurable impacts on behaviour change at the population level,
Utilising new ways to communicate the value of education,
Accreditors sometimes being a barrier to facilitation of innovation,
The need for development of faculty skills in innovation.
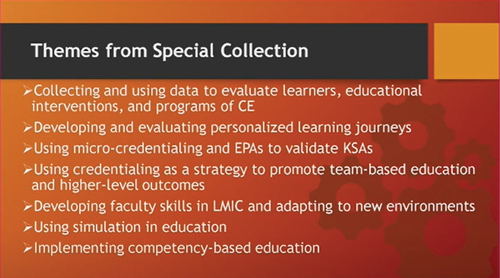
The main themes from the 2022 Special Collection are summarised in and a description of the planning process and the articles can be obtained via the following links:
Podcast: JECME 2022 Special Collection: Innovation and Impact in CME/CPD by European CME Forum (spotify.com)
Articles: Special Collection 2022 | Journal of CME (jcme.org) [Citation2].
Day 1 continued with the Wednesday workshop session where participants’ choice for attendance was partly based on video “teasers” provided by the workshop leaders followed up by live, onsite promotion of their workshops in the style of elevator pitches. The four workshops were as follows:
Stronger together: the power of diversity, equity, and inclusion in reshaping healthcare through medical education
Annette Triebel (Gilead), Amy Bernard (Medscape), Ann Carothers (Medscape) and Julie-Lynn Noël (EUROSPINE)
Participants in this workshop delved into the concepts of diversity, equity, and inclusion (DEI) and unconscious bias. The importance of integrating DEI standards into medical education programmes was emphasised and subsequent potential effects on transforming healthcare. Case studies were provided to demonstrate how CME/CPD stakeholders are making progress by incorporating DEI in their activities and learning from shortcomings that have arisen. The workshop leaders described efforts in their own areas of work to increase diversity in areas such as faculty panels, workforce, and researchers. The growing emphasis placed on health equity outcomes in current Requests for Proposals (RFPs) issued by grantors was highlighted as well as the availability of resources such as those produced by the Accreditation Council for Continuing Medical Education (ACCME) [Citation3].
The Patient Voice in Clinical Education
Dean Beals (DKBmed), Diana Torres (Liberum IME) and Lisa Sullivan (In Vivo Academy)
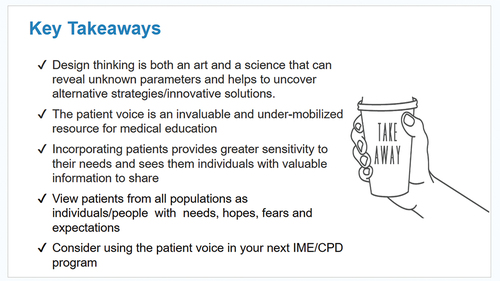
Recognising an acceptance of the need to include patients in a more active role in CME/CPD to align education with more accurate patient experiences and perspectives, this workshop sought to discuss topics such as the source of patients, their specific role in the design and delivery of education for health care professionals (HCPs), and how to develop clinical faculty to interact with patients in an educational setting. It was noted that the ACCME, having identified several benefits from the inclusion of the patient voice in CME activities, now includes the patient perspective in some of its accreditation criteria [Citation4]. The workshop participants considered several case studies and produced outlines of how they could incorporate patient input into some of their own activities. Key takeaways from the workshop are shown in .
How Healthcare Professionals are Learning Differently After the Pandemic
Álvaro Margolis (EviMed) and Diana van Brakel (Kenes Education)
This workshop provided participants with the opportunity to discuss their own experiences in the changes in delivery of CPD/CME activities brought about in just a few years since the onset of the COVID-19 pandemic. They considered some of the challenges associated with the increased use and associated costs of virtual learning platforms and blended formats for educational activities. Examples were provided from both Latin America and Europe of hybrid activities and concerns about the logistics as well as an appreciation of perceived benefits such as the increase in participation by women, and greater geographical reach were expressed.
Culturally Sensitive Communication: How Do We Communicate in the Evolving CME/CPD Community?
Miriam Uhlmann (CK-CARE) and Celeste Kolanko (Liberum IME)
The purpose of this workshop was to provide some definitions of culture in regional, local, and organisational contexts, describe aspects of cultural sensitivity in communication and share experiences of how to communicate with global audiences. Some barriers to effective communication associated with global virtual meetings and working from home scenarios were also identified. One of the main topics that emerged from the workshop was the possibility of communication obstacles in language due to the confluence of native and non-native English speakers in global educational activities that are conducted in English. Some solutions were suggested such as captions, translations, and careful pronunciation of names for interactivity and helping to reduce shyness in contributing by those whose cultural values may lead to such inhibition. The use of the catch-box microphone at the meeting itself was cited as an example of a possible solution.
Day 2 began with a reflection session where the leaders of the previous day’s workshops provided a summary of the discussion points that arose during their workshops. This was followed up by a general discussion among participants that integrated the topics from all the workshops so that all attendees could obtain a flavour of the content of the workshops that they did not attend. Some of the points raised were:
Collaboration on a standardised taxonomy of the demographic variables of individuals,
DEI is context specific and needs to be integrated into the planning of educational activities,
How should “power” be managed (the white middle-aged male vs the rest?),
Resources and infrastructure may not allow DEI to develop,
“Culture eats strategy” for breakfast lunch and dinner,
Hierarchies differ in different cultures so broader society must be considered,
Health equity is becoming a priority so that it may not be quite so problematic as the next generation begins to control HCP education.
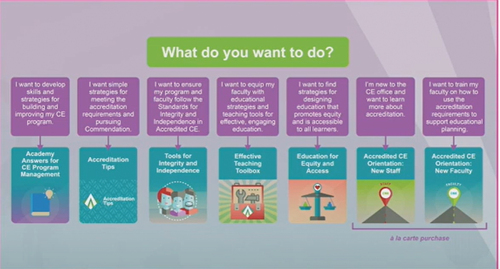
The meeting continued with an update from Kate Regnier on the ACCME’s strategic plan that aims to accelerate the evolution of CME/CPD by nudging providers towards improvement in the quality of their educational offerings but also providing resources to aid this process. She described various tools and resources available. She highlighted the ACCME’s commendation criteria and the CE Educator’s Toolkit that contains evidence-based practical tools. A section of a new online learning portal, the ACCME Academy was also revealed i.e. its question-asking tool as shown in .
The theme for Day 2 was Attitudes and Culture and continued with a panel discussion led by Jonas Nordquist (Karolinska Institutet) and Jeanette Andersen (Lupus Europe) that was the first of two sessions dealing with the incorporation of the patient voice into HCP education. Having indicated that there was little published evidence to show details of outcomes based on patients’ participation in CME/CPD and posing some questions on what role patients should have and how the patient voice should be defined, Nordquist introduced Andersen (see ) who provided a compelling argument for the inclusion of patients in the planning and implementation of educational activities for HCPs. As a patient advocate, Chair of Lupus Europe, an umbrella organisation that coordinates various national lupus patient organisations in Europe, and a lupus patient herself, she brought unique insight into the discussion. Her main take on the role of patients was that their perspective can add value to shared decision making with physicians both in treatment protocols and educational activities on clinical topics. The panel discussion confirmed her assertion that, whilst the patient voice is valuable and to be welcomed, it must be within acceptable parameters to all concerned. A consensus emerged from the panel with the notion that there must be psychological safety for patients involved in educational activities, that they should not just be present as “teaching material” but can play vital roles in the spectrum of HCP education from planning through to delivery.
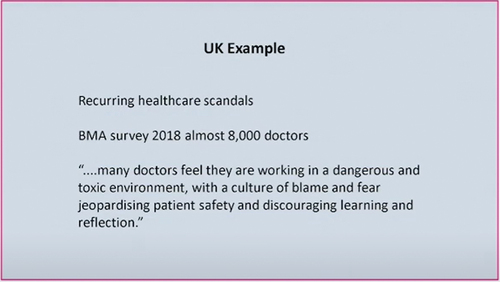
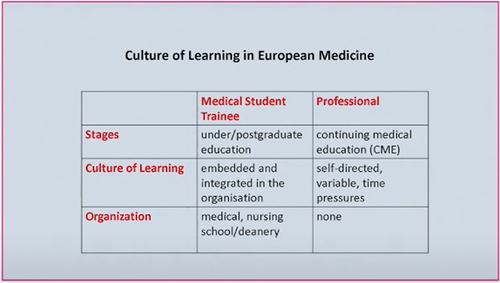
Robin Stevenson followed the patient voice session by moderating a lively discussion that looked at the concept of promoting a “Culture of Learning”. After eliciting a description from the audience of a culture of learning being the presence of resources and solutions to improve learning, he drew out further ideas from the participants relating to their own home countries. This vivid demonstration of interactivity underlined the differences in framework of HCP educational systems around the world. Some pertinent comments that emerged were:
A culture of learning is embedded at most levels in North American healthcare systems,
A culture of learning is country specific in Europe, being mandatory in some locations and voluntary in others,
HCPs may have their own individual culture of learning,
Supportive administrative entities e.g. workplace CME/CPD departments are not as evident in many European countries compared with US,
A “blame and fear” culture in UK (see ) was contrasted with a “just” culture such as a culture of feedback in US where quality improvement departments allow learning from mistakes.
The attendees continued to debate whether CME/CPD should be reparative to address identified needs or curricular as in the pre-professional training outlined in .
This session called attention to the spectrum of approaches and provision of supporting organisational architecture for learning in practice that can ultimately improve public health. The forum and JECME provide a platform for such discussion among influencers in the global enterprise of HCP continuing education.
Lunch with Learners Session
A feature of the European CME Forum that has increased in popularity over the years is the session led by Lawrence Sherman called “Lunch with the Learners” when clinicians from the meeting’s host city take time away from their practice to interact with the participants and answer questions to provide their perspective on the educational opportunities available to them in the local area. See .
During this session three clinicians based in Barcelona, an internal medicine specialist, a nurse specialising in Multiple Sclerosis, and a neurologist highlighted the growing importance of informal education in their practice settings. Although much of their continuing education was still derived from conferences, some of which was organised by pharmaceutical companies, they acknowledged a trend towards more hybrid activities. Responding to an audience question, one learner described the difficulties, echoed in one of the earlier workshops, of accessing English language courses from other countries where subtitles were not provided. A unified response from all three was that they saw little opportunity for team-based education, most of their available education being job-specific.
Attitudes and Culture Workshops
Having considered the elevator pitches, participants chose to attend one of the following workshops which were followed by a further reflection and discussion session for the wider meeting that identified “quality” as a recurring theme in each of the three workshops representing providers, grantors, and accreditors.
Finding the “magic middle” when designing and delivering education
Margarita Velcheva and Diana van Brakel (Kenes Education)
In many ways this was a welcome “back to basics” session looking at the myriad requirements, regulations, and expectations of grantors, accreditors and faculty presenters that must be navigated and negotiated by educational providers in Europe. The workshop aimed to discuss a common-sense approach to these issues and provide participants with some ideas to fulfil the central goal of independence in medical education as illustrated by the word cloud produced during the workshop and shown in .
Some of the salient points that emerged were:
The need for providers to be fully involved at every step in the process of planning and implementing an educational activity,
Educators need to educate faculty on requirements,
Utilise a design model such as the four pillars of the Good CME Practice Group so that education is appropriate, effective, balanced, and transparent,
Collaboration necessary among stakeholders for common goal of improving patient outcomes,
Need for representatives of ALL stakeholder groups e.g. government agencies to interact at the forum.
Life as a Grantor: Expectations Vs. Reality
Pam Beaton (Boehringer Ingelheim) and Elizabeth Kelly (Eli Lilly)
This workshop focused on a grantor’s viewpoint by defining IME quality in terms of:
Measuring real behavioural change,
Seeking good design, appropriate target audiences, and relevant faculty in grant submissions,
Being compliant in any interactions with faculty e.g. requests for presentation materials,
Ensuring “double-dipping” does not occur if providers seek to repurpose previously funded activities,
Placing emphasis on the concept that grantors seek to support activities that are truly fair and balanced and designed to contribute to improvements in patient care.
Challenges and Developments for the Accreditors
Fabíola de Andrade (Independent CME Consultant) with Reinhard Griebenow (ECSF), Arcadi Gual (SACCME) and Jean-Philippe Natali (Agence Nationale du DPC)
The concepts of independence and quality were also addressed during this workshop and led to the following comments:
The reality that accreditation can be robust if all stakeholders stick to their roles,
Independent Medical Education (IME) can be considered as CME except for the credit component,
Accreditors should consider embracing the concept of IME,
There is a pressing need for common terminology,
There is slight movement in Europe towards accreditation of providers rather than activities that mirrors the system of ACCME,
Challenges still exist with the accreditation of micro-learning activities for which learners have expressed preferences.
The workshop leaders also provided a set of resources listed below to help participants follow-up on the discussion.
Additional Resources from the “Challenges and Developments for the accreditors” Workshop
International Standards for Substantive Equivalency Between CPD/CME Accreditation Systems
Criteria to Assess Independence in Continuing Medical Education (CME): Independence through Competence and Transparency
Outcomes in CME/CPD – Special Collection: How to make the “pyramid” a perpetuum mobile
What does CME accreditation stand for?
Independent Medical Education (CME)/Continuing Professional Development (CPD) must deliver unbiased information
Roles and Responsibilities in the Provision of Accredited Continuing Medical Education/Continuing Professional Development
WMA Declaration of Geneva
WMA International Code of Medical Ethics
WMA Declaration of Seoul on Professional Autonomy and Clinical Independence
WMA Declaration of Chicago on Quality Assurance in Medical Education
IACPDA Update
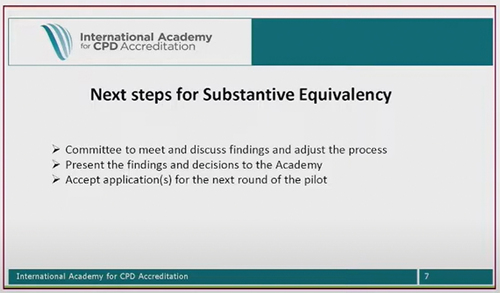
The accreditors’ stakeholder group was further represented with a presentation by Michel Smith of the Royal College of Physicians and Surgeons of Canada joining the meeting virtually to provide an update from the International Academy for CPD Accreditation (IACPDA) with Kate Regnier (ACCME) mainly to do with Substantial Equivalency (SE) among the 30 accreditation systems from 25 different countries that comprise the Academy. They described the recent completion of a pilot phase for implementation of the SE project which will move forward to provide a mechanism for representatives of accreditation systems to review each other and determine whether SE standards have been met. See .
These standards have been developed from an original set of SE guidelines and have now been adopted by many of the Academy members. Further details are available on the Academy website [Citation5].
Day 3 of the meeting was themed around Environment and Community and began with a panel discussion led by Lawrence Sherman that involved international representatives from different parts of the world, namely Dr Álvaro Margolis from Uruguay, Lisa Sullivan from Australia, Vaibhav Srivastava from India, and Professor Rostyslav Marushko from Ukraine, who were warmly welcomed by the attendees. The panellists set the scene for the situations in their specific areas of the world, then discussed potential avenues to explore for providers who might be seeking to disseminate their activities on a global basis.
Marushko started off the session by describing the milieu of CME/CPD in Ukraine that has persisted even during the conflagration in that country. He outlined the framework for CPD that has been created and implemented in recent years in Ukraine by the Ministry of Health. Despite the challenges of the pandemic and the war in Ukraine, there is now a registration system in place for providers and their activities which may be sourced from outside the country as well as on a local basis.
Sullivan indicated that there is little IME in Australia for general practitioners, whose continuing education is mostly derived from industry sources, whereas there is a self-reporting reflection system for specialists who can obtain education from any appropriate source around the world.
Srivastava provided information on the organic nature of CME in India which has a federal system that is flexible and able to provide needs-based education that can be addressed using local and global sources.
Margolis pointed out the diversity of countries in Latin America and the relative lack of coordination and development of CME systems in this heterogeneous region.
Sherman’s questioning drew out a consensus from the panellists that discussion and collaboration with local academic partners is vital to the success of activities produced elsewhere. Appropriate gap analysis, cultural sensitivities and local input were seen as key factors, with mutual respect needed to ensure success. An understanding of the environment and the need for partners was deemed paramount. The possibility of interprofessional education was not regarded as being a main thrust of educational activities outside North America.
Oral Presentation
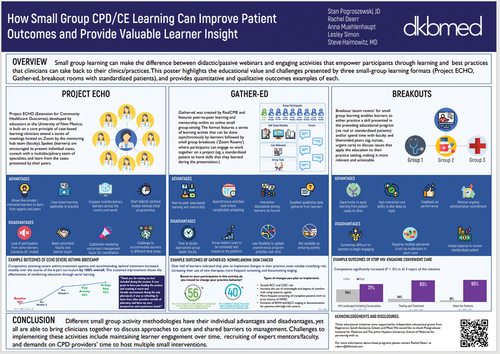
One of the poster authors, Stan Pogroszewski of DKBMED made a live oral presentation to highlight their experience of small group learning based on the poster:
How Small Group CPD/CE Learning Can Improve Patient Outcomes and Provide Valuable Learner Insight
He described how such learning can provide useful outcomes in terms of changes in professional practice but also noted challenges associated with this type of learning. The poster shown in highlights their use of three small-group learning formats i.e. Project ECHO, Gather-ed, and breakout rooms with standardised patients. Each method did show some positive educational outcomes, but the authors also pointed out some challenges in conducting this type of activity such as being able to maintain learner engagement over time, the recruitment and development of skilled presenters, and indeed time pressure on the CPD providers themselves when running multiple small group interventions.
The complete set of posters and associated links follows:
Applying the cognitive theory of multimedia learning to educational animations and explainer videos in CME-CPD
Jayzona Alberto
On-call blip simulation for final-year medical students; a novel teaching experience
Joanna Ismail and Krishan Patel
Thoughts for the future – outcomes and observations of on-line CME activities during the pandemic
Michela Fiuzzi
Using electronic protocols to promote good clinical practice: An example with DNACPR documentation
Anmol Patel
The hidden curriculum of the UK foundation training programme: a trainee perspective
Anmol Patel
Hospital induction and training experiences for international medical graduates new to the NHS
Anmol Patel
How small group CPD/CE learning can improve patient outcomes and provide valuable learner insight
Stan Pogroszewski, Rachel Deerr, Anna Muehlenhaupt, Lesley Simon and Steve Haimowitz
Derail Depression: Assessing the effectiveness of a continuing education quality improvement program
Stan Pogroszewski, Rachel Deerr, Anna Muehlenhaupt, Lesley Simon, Caroline Bamhart, Michael Clark, James Hawthorne, Steve Haimowitz and Dean Beals
Re-imagining educational design in a virtual world: leveraging a small group learning format to educate community-based HCPs on the optimal management of ovarian cancer with PARP inhibitors
Janvi Sharma and Michael Perlmutter
Going beyond knowledge; skills when assessing the impact of an immersive learning program in Myasthenia Gravis (MG) utilising virtual reality (VR); the ENGAGE research design
Ina Weisshardt, Cornelia Reyes, Ivo Vlaev, Natasha Monin and Sophie Barry
Will virtual reality (VR) be able to overcome disconnect in patient-physician communication? Set-up objectives of ENGAGE; an integrated educational program for physicians in Myasthenia Gravis
Ina Weisshardt, Cornelia Reyes, Ivo Vlaev, Sophie Barry and Mihai Streza
Patient Voice 2
A follow-up session on the incorporation of the patient voice into HCP education produced many suggestions and ideas building on the initial session on Day 2. Further discussion ensued on topics such as how and when to include patients, either at planning phase or during the education itself. The question arose as to whether patients should be brought in just to tell their story or to be a teacher. This developed further to consider how to prepare patients for each role and challenges such as language issues and the fact that the patient “on the podium” may not work in all therapeutic areas.
Some practical suggestions were made such as the use of patient surveys or word clouds to inform the content for enduring material or simulation activities. The use of patients in real time or via recorded vignettes was discussed and it was emphasised by the patient representative on the panel that the presence of the patient voice should not simply be an add-on or top up to an activity but should represent real planning and integration. Education providers were urged to have clear expectations of why the patient voice might be required in their activities and to consider two main points raised by patients in this situation.
What do you want from me?
Don’t talk down to me!
The question of how many patients to include was deemed to depend on context, for example, several patients might be needed to show the spectrum of a disease. As an example of a successful use of the patient voice, Jeanette Andersen cited an activity designed solely to demonstrate appropriate communication between patient and clinician.
In Conversation with… Lino Gonçalves (ESC) and João Grenho (UEMS-EACCME)
This conversation between two Portuguese physicians provided an illuminating insight into the current ethos of the European Accreditation Council for Continuing Medical Education (EACCME®), the main pan-European accrediting body. Grenho, who heads up EACCME, was interviewed by Gonçalves who began with the blunt question of “Why do we need EACCME?”
Grenho outlined the European reality or rather the 44 realities based on the number of countries in Europe with different cultures, systems, and ways of doing things related to CME. He suggested that EACCME can provide a means for providers to bring their offerings to the European arena and navigate the minefield of these 44 realities. Grenho accepted that there was valid criticism that little feedback has been given to applicants when an activity was rejected. He further acknowledged the need to produce some online/hybrid seminars to discuss questions from providers and furnish answers in a similar manner to the ACCME educational offerings in US. On the thorny question of provider accreditation which was previously regarded in Europe as “a very bad thing”, he announced a revamp of the Trusted Provider system that is moving towards provider accreditation through EACCME.
The conversation moved on to highlight the fact that the legal power to accredit CME/CPD is at the national not European level and in order to solve this issue EACCME has been working to draw up agreements with different European countries to streamline the application process for accreditation. He noted the existing agreements of mutual recognition of credits with entities in the US and Canada and a separate agreement for the granting of EACCME’s credits to activities under the auspices of an umbrella organisation in Latin America. In response to a question from the audience on the role of industry in CME, Grenho was emphatic in stating that the rules were clear and that activities can be supported by industry with the proviso of “no strings attached”. Grenho envisioned the evolution of EACCME as moving towards the accreditation of activities that were well designed but not necessarily clinical in nature. He also stated that, with the increasing availability and preference for micro-learning activities, it was possible to have 30-minute events accredited.
JECME Update
Robin Stevenson, Editor-in-Chief of the Journal of European CME provided an update on various aspects of the Journal during the previous year. He mentioned the success of the Special Collection on Innovation and Impact edited by Kathy Chappell which included 13 published articles, mainly brief reports but which may have been the impetus for more detailed research articles being submitted that were not destined for the special collection. Furthermore, an increase in the number of downloads of articles has been noticed, mostly from North America and Europe but also with growing numbers from Asia. The 2023 Special Collection was then previewed with the theme of “Voices in CME” and Lisa Sullivan as guest editor.
Stevenson completed the update by announcing a change in the journal’s title to reflect the burgeoning scope of submissions from beyond Europe. It will now be known as the Journal of CME with a broader target audience as the concept of interprofessional education gains more traction, See .
Getting to Our Destination
The final formal session of the meeting was an open Q&A panel discussion where panellists were asked to state one aspect of their work that they would change as a result of attending the meeting (see ).
The provider stated that she would try to “engage patients more systematically for activity development”.
The grantor wanted to fully understand what providers mean by “a global reach” and how they adapt their activities to be relevant to local populations.
An accreditor hoped for better alignment of accreditation systems around the world.
Another accreditor also sought agreement on the harmonisation of systems.
The medical society representative hoped that societies would become more involved with the European CME forum and the Journal of CME.
The patient voice was mentioned as a key component of the meeting and suggestions for addition of other “voices” included payers, local accreditors, a spectrum of health professionals, trainees, and policy makers. Topics for further discussion included the use of digital tools in learning, the need for more inclusivity among the IME community, and a deeper look at the public health perspective linked to CME/CPD. Other topics that were suggested for the next meeting were:
Examples of best practices in regularly scheduled educational activities in European workplaces,
How to access data that can connect CME/CPD to Quality Improvement (QI) and Performance Improvement (PI) initiatives,
Examples of interprofessional education outside US,
The importance of leadership and champions for team-based education.
A wish list for changes in the CME/CPD arena during the coming year yielded these suggestions:
More team-based education
More public and patient education
Provision of safe spaces to promote DEI
EACCME “has to stop being an island” (Quote from João Grenho)
More industry presence at the meeting
More opportunities for patients to be driving the educational process.
Unsession
Lawrence Sherman reprised his role of ringmaster to elicit final comments from the meeting in an unstructured format. Discussion led on from the previous session with suggestions such as:
Provide agreed terminology, e.g., update the glossary of IACPDA perhaps using the Wikipedia model,
Provide a session with examples of in-house education outside US,
How to implement and measure shared decision making,
A workshop on writing for publication and reviewing publications,
Micro-learning examples.
The Take Home Message from #15ECF is Shown in
Figure 16. #15ECF take home message – implicit in theme of 2023 special collection – “listen to the Voices!”.

Details of the 15th European CME Forum presentations are available at the European CME Forum website: www.cmeforum.org
The 16th European CME Forum is due to meet in The Hague, Netherlands at the Hotel NH Den Haag See: https://cmeforum.org/16ECF
Disclosure statement
No potential conflict of interest was reported by the author.
References
- Stevenson R. Learning and behaviour in medicine a voyage around CME and CPD. 1st ed. Boca Raton: CRC Press; 2022.
- JECME special collection 2022: innovation and impact in CME/CPD. [cited 2023 Sep 1]. https://www.jecme.org/special-collection-2022
- Accreditation for continuing medical education: diversity, equity and inclusion resources. [cited 2023September 1]. https://accme.org/diversity-equity-inclusion-resources
- Accreditation for continuing medical education: engages patients/public. [cited 2023 Sep1]. https://accme.org/accreditation-rules/accreditation-criteria/engages-patientspublic
- International academy for CPD accreditation – substantial equivalency. [cited 2023 Sept 1]. https://academy4cpd-accreditation.org