?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
We aimed to introduce team-based learning (TBL) as one of the teaching methods for diagnostics and to compare its teaching effectiveness with that of the traditional teaching methods.
Methods
We conducted a randomized controlled trial on diagnostics teaching involving 111 third-year medical undergraduates, using TBL as the experimental intervention, compared with lecture-based learning as the control, for teaching the two topics of symptomatology. Individual Readiness Assurance Test (IRAT)-baseline and Group Readiness Assurance Test (GRAT) were performed in members of each TBL subgroup. The scores in Individual Terminal Test 1 (ITT1) immediately after class and Individual Terminal Test 2 (ITT2) 1 week later were compared between the two groups. The questionnaire and interview were also implemented to survey the attitude of students and teachers toward TBL.
Results
There was no significant difference between the two groups in ITT1 (19.85±4.20 vs 19.70±4.61), while the score of the TBL group was significantly higher than that of the control group in ITT2 (19.15±3.93 vs 17.46±4.65). In the TBL group, the scores of the two terminal tests after the teaching intervention were significantly higher than the baseline test score of individuals. IRAT-baseline, ITT1, and ITT2 scores of students at different academic levels in the TBL teaching exhibited significant differences, but the ITT1-IRAT-baseline and ITT2-IRAT-baseline indicated no significant differences among the three subgroups.
Conclusion
Our TBL in symptomatology approach was highly accepted by students in the improvement of interest and self-directed learning and resulted in an increase in knowledge acquirements, which significantly improved short-term test scores compared with lecture-based learning. TBL is regarded as an effective teaching method worthy of promoting.
Introduction
The team-based learning (TBL) model was proposed by Michaelsen et al,Citation1 an educator at the University of Oklahoma, in 2002, with an initial intention of coping with the teaching pressure resulting from the surge of student numbers in the 1970s. TBL adopts group learning, emphasizes collaboration and coordination in adult learning, and advocates classroom tests and previews of study content. The operating characteristics of TBL are that students are main actors who engage in group discussions under the guidance of teachers to promote the students’ self-motivated learning and teamwork.Citation2–Citation4 Compared with the traditional teaching method that is dominated by a teacher’s lectures, TBL more underscores the students’ main actor role in the learning process while teachers act as guides and advisers; TBL attaches more importance to students’ participating and taking the initiative in the teaching process.Citation5,Citation6 Currently, although its teaching effectiveness and applicability remain controversial, the TBL teaching method has been recognized and adopted by medical schools in most countries.Citation7–Citation12 According to a systemic review by Fatmi et al,Citation10 most existing studies have demonstrated that TBL significantly improves students’ knowledge level. However, some investigators found that compared with other teaching methods, TBL exhibited no advantage; in addition, students’ attitudes toward TBL teaching have been mixed. Although TBL has been applied for many years, its impact on teaching effectiveness and recognition by teachers and students still requires more studies to provide more definitive evidence for validation and support.
With the recent implementation of the expansion policy for Chinese medical schools, the number of medical students has surged, leading to a more prominent teacher shortage problem and enormous teaching pressure in medical education. TBL teaching is one of the teaching methods for large classes and has been considered as an effective solution to shortage of teachers in adult education.Citation6 There have been reports regarding the application of TBL in the teaching of courses such as blood system disorders, cardiovascular diseases, and neurology in medical schools in China,Citation11 with uniformly good outcomes. However, TBL has been rarely applied in the teaching of diagnostics, especially in the sections related to symptomatology. Teaching these sections is crucial for nurturing students’ thinking in clinical diagnosis. In this context, we aimed to introduce TBL to the teaching of diagnostics and symptomatology and to compare its teaching effectiveness with that of the traditional teaching methods. In addition, we aimed to investigate the impact of TBL on students at different academic levels, as well as the attitudes and efforts from teachers and students toward TBL teaching, in order to understand the feasibility and value of applying TBL in the teaching of diagnostics and provide theoretical bases for extensive TBL applications in more courses.
Methods
Consent to participate
Experimental protocols and written informed participant’s consent were approved by the Human Subject Ethics Committee of West China Medical Centre, Sichuan University (ethics consent no: HSEC20140788-22479) according to the requirements of the Chinese Prevention of Cruelty to Human Subjects and the Code of Practice for the Care and Use of Human Subjects for Scientific Purposes. All students clearly understood every steps of the study and signed a written informed consent before enrolling themselves in our study.
Study design
A randomized controlled trial (RCT) study was performed using students as the research participants. The entire 111 third-year students majoring in clinical medicine in our medical school (5-year program) participated in this study during the academic year of 2014–2015. The students were further grouped using the computer random digital method into two groups, TBL teaching group (55 students, experiment group) and traditional teaching group (56 students, control group). The basic study design method was according to the guidelines of TBL interventions.Citation13
Textbooks and curriculum setup
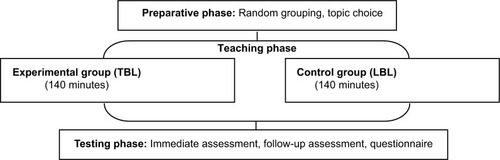
Both the groups used the same standard textbook (Diagnostics, 8th Edition, edited by Professor Xue-hong Wan, People’s Health Publishing House) as well as the same syllabus and practice instruction. The teachers, teaching schedules, and examination forms of the two groups were also kept consistent. For teaching the symptomatology of dyspnea and palpitation, the TBL or lecture-based learning (LBL) method was adopted in the two groups. The reason for selecting these two symptoms was that they are the core and key content of symptomatology in diagnostics and are also crucial for helping students develop clinical thinking in diagnosis and differential diagnosis. The details of the teaching methods are mentioned subsequently ( and ).
TBL method
The experiment group used the TBL method and the following study design:
Teaching preparation stage
Team building: based on the original diagnostics trainee group, the TBL teaching group was divided into eight subgroups, with six or seven students per subgroup; and the students in each subgroup were ensured to have the prerequisites and to become familiar with each other during the early stage of teaching activities, such as group discussions and clinical probation.
Preview: 1 week before class, the teachers clarified the curriculum, informed the students regarding the TBL learning process, and distributed teaching materials and assigned self-learning content to the students.
Preparation stage of effectiveness assessment
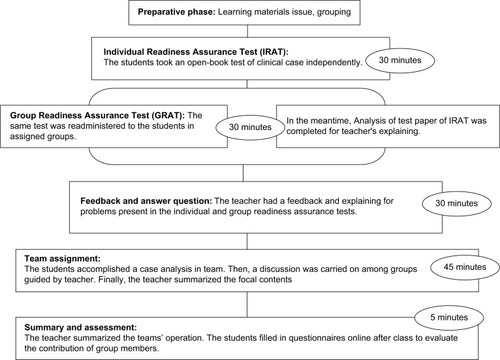
Individual test: first, a 30-minute Individual Readiness Assurance Test-baseline (IRAT-baseline) test was conducted to measure the readiness of the students for the teaching content through self-learning before the class. Each test consisted of 30 multiple-choice questions, all being single-answer questions with each having five-choice answers. The test adopted the open-book examination form, in which students were allowed to use textbooks and online information, but discussion among students was prohibited.
Group test: after the individual test, a 30-minute Group Readiness Assurance Test (GRAT) was performed in which members of each TBL subgroup presented the answer after a discussion. The questions were the same as those used in the individual test, and the same open-book examination form was adopted. After the above-described two preparatory stages, the teachers gave ~30-minute lecture, in which timely feedback was given to the students based on the test results, so that the students had a clear understanding of the learning content.
Team assignment stage: teachers were assigned one medical record analysis question that was closely related to clinical medicine and had a high level of difficulty, and members in each subgroup jointly analyzed and discussed the case based on the knowledge they had acquired. First, the intrasubgroup discussion was organized, which was followed by intersubgroup discussions under teacher guidance. Finally, the teachers presented a lecture on problems raised in the students’ discussions and summarized key and difficult content. This stage took ~45 minutes.
Evaluation and summarization stage: teachers evaluated and summarized the students’ discussions and team effort, noted problems, and proposed recommendations for improvement, which lasted ~5 minutes. After the class, the students were asked to answer an online questionnaire in which a peer review was performed by evaluating the contribution of each member in the subgroup to the team. The score of students in the TBL group is 5 points. TBL score = 30% IRAT + 30% GRAT + 30% ITT1 + 10% peer review.
The teaching effectiveness of TBL and the effort by students in learning were investigated through a questionnaire survey. The feedback survey on teaching effectiveness was performed only in the TBL group. Researchers made questionnaires according to the domestic and foreign literature and combined with our experience of teaching practice. It had 10 items and was scored using a Likert five-level scoring method.Citation14 The information on the students’ learning time and learning method was acquired through the questionnaire. The teachers’ teaching effort and attitudes toward TBL were investigated through interviews. Teacher interviews were conducted by using one-to-one approach, and the interview time was controlled at 15–30 minutes and recorded. In the interview, the teacher talked about the following opinions: the atmosphere of TBL, the teaching effect of TBL, whether recognized and liked TBL, preparation time, and the specific input.
LBL method
The control group used the LBL method in which a 125-minute lecture was first presented, followed by a 15-minute question and answer (Q&A) session focusing on the teaching content. The information on the students’ learning time and learning method was acquired through the questionnaire.
Evaluation method
After completing the teaching, a 30-minute Individual Terminal Test 1 (ITT 1) was conducted in both groups immediately after the class; 1 week later, a 30-minute Individual Terminal Test 2 (ITT 2) was conducted in the two groups. The ITT evaluation contents consisted of multiple-choice questions on clinical cases that had been well prepared by the teachers before the class and were suitable for the teaching content, mainly examining the students’ ability to apply the knowledge learned in the chapter. Each test also consisted of 30 multiple-choice questions, all being single-answer questions with each having five-choice answers; each set of evaluation questions was previously assessed to ensure that the difficulty level was consistent with IRAT-baseline.
The scores of the two terminal tests in the two groups of students were compared and statistically analyzed. For the TBL group, scores before and after the teaching intervention were compared. Meanwhile, the performance changes before and after the intervention of students with different academic levels were also compared at different levels. The academic level of a student was determined using the student’s average score on main courses in the previous academic year: the top 30% were assigned as Level A, the middle 40% as Level B, and the remaining 30% as Level C.
Statistical methods
The SPSS 17.0 statistical software package was used for the statistical analyses. The data are expressed in the form of
, and α = 0.05 was set as the significance level. The measurement data were converted into a normal distribution using the Kolmogorov–Smirnov test, and the homogeneity of variance was tested using Levene’s test for equality of variances; the t-test was used for comparisons, while the Wilcoxon test was used in cases of non-normal distribution. The comparisons of the evaluation scores of the two groups at two time points after the teaching intervention and the learning times spent by the two groups were performed using the independent sample t-test, while the comparison of the evaluation scores of the TBL group at different time points was performed using the paired sample t-test. The comparison of students at different academic levels was conducted using analysis of variance. The χ2 test was used in the case of count data.
Results
Baseline student characteristics
In total, 111 students were enrolled in this study. No student declined participation. There were no significant differences between the TBL and LBL groups in baseline statistics such as age, gender ratio, and average score during the previous academic year ().
Table 1 Baseline student characteristics
Scores of the two groups
There was no significant difference between the two groups in ITT1 (19.85±4.20 vs 19.70±4.61, p=0.851). While for in ITT2, the score of the TBL group was significantly higher than that of the control group (19.15±3.93 vs 17.46±4.65, p=0.042). In the TBL group, the scores of the two terminal tests after the teaching intervention were significantly higher than the baseline test score of individuals (ITT1 vs IRAT-baseline, p<0.001; ITT2 vs IRAT-baseline, p<0.001; ).
Table 2 IRAT-baseline, GRAT, ITT1, and ITT2 scores between two groups
The stratification analysis showed that the IRAT-baseline, ITT1, and ITT2 scores of students at different academic levels in the TBL teaching all exhibited significant differences (p<0.001), and pair-wise comparisons between the A/B/C subgroups using the least significant difference test also showed a significant difference (p<0.05). The ITT1-Individual Readiness Assurance Test (IRAT)-baseline and ITT2-IRAT-baseline showed no significant differences among the three subgroups (p>0.05; ).
Table 3 IRAT-baseline, ITT1, and ITT2 scores in each subgroups of TBL
Students’ feedback on the teaching model
TBL teaching feedback survey: 55 questionnaires were recovered, with a recovery rate of 100%. The survey results showed that the vast majority of students evaluated the TBL teaching model positively. The results are shown in .
Table 4 Students’ feedback on the teaching model
Learning effort between the two groups
Learning times spent by the TBL student group before and after the class (91.09±45.11 minutes and 90.45±37.1 minutes, respectively) were significantly higher than those of the control group (26.61±11.91 minutes and 41.16±18.36 minutes, t=10.256 and 8.847, respectively; p<0.001; ). The survey revealed that the TBL group had more diverse learning methods. In the LBL traditional teaching model, students usually previewed and reviewed by only reading the teaching materials and class notes, while in the TBL teaching model, the students employed more learning methods such as searching for information in databases in the library, having discussions with peers, and taking the initiative to ask senior students.
Table 5 Learning times spent between the two groups
Teaching effort and attitude of the teachers toward TBL
Interviews of the teachers revealed that under the LBL model, because the teachers had previously prepared teaching materials such as teaching plans and handouts, the time spent on the preparation for class for a teaching topic was ~5 hours. In the TBL model, because this was the first time the teaching method was adopted, the time used for class preparation was ~12 hours. However, although the TBL teaching method had a higher class preparation workload compared with LBL teaching, the atmosphere in the TBL classroom was more active and engaging; moreover, the students were more enthusiastic toward learning, evaluated the TBL teaching model positively, and wanted it to be further promoted in future teaching programs.
Discussion
TBL teaching achieved a teaching effectiveness immediately after class, the same as what the conventional LBL teaching do, and showed a better continued effect on teaching effectiveness than LBL. Previous studiesCitation15–Citation19 have demonstrated that TBL training significantly improves a student’s ability to obtain knowledge, and the effectiveness of TBL is superior to that of traditional teaching methods. The results of this study showed that after TBL teaching intervention, the scores of terminal tests of individual students were significantly improved compared with the baseline testing scores, which also confirmed that TBL effectively improved the students’ acquisition of knowledge.
Interestingly, this study revealed that in terms of the test score of the ITT2 that was taken 1 week after the teaching intervention, the TBL group significantly outperformed the LBL group, indicating that within a certain period after the teaching intervention, with elapsed time and the natural attenuation of memory, the test score of the LBL group exhibited a more pronounced downward trend, while that of the TBL group declined more slowly. This finding indicated that the influence of the teaching effectiveness of TBL on the students continued during the short term, generating a prolonged after-effect in the teaching effectiveness of the method. The investigation into the students’ learning effort showed that students from the TBL group spent a longer time reviewing and adopted more diverse learning methods compared with the students from the LBL group, which was likely the reason for the continued effect of the teaching effectiveness of TBL. This effect has not been reported in previous studies. The positive, continued effect of the teaching effectiveness of TBL may produce exciting incentives for the expansion of TBL.
Wiener et alCitation9 reported that students who had a higher academic level benefited more from TBL teaching, which enabled them to achieve a better academic performance. Koles et alCitation20 and Tan et alCitation16 found that students who had a low academic level benefited more from TBL teaching. The results of this study showed that students at different academic levels exhibited no significant difference in performance enhancement after the TBL teaching intervention, suggesting that the intervention itself had no significantly different impact on students at different academic levels.
The questionnaire survey in this study showed that the vast majority of students held a satisfactory opinion of the TBL teaching method. Students generally agreed that TBL could stimulate an interest in learning, guide self-learning, improve the ability to solve problems, and develop teamwork skills. The classroom testing session in the TBL setting was one of the factors promoting the students’ self-learning. Moreover, the teamwork within the TBL group and the competition among TBL groups encouraged students to actively engage in learning, to contribute, and to share personal information, which inevitably elevated the academic performance in the whole group. The positive impact of TBL on abilities other than academic performance found in this study was consistent with the findings in previous studies.Citation21–Citation24 The enhancement of these abilities was likely because the students generally held a satisfactory attitude toward TBL. In this study, interviews of the teachers revealed that they were also satisfied with TBL. The teacher–student interaction during TBL teaching also stimulated the teachers’ enthusiasm, causing an enhanced passion for teaching and improved teaching skills.Citation25
The results of this study showed that compared with that in the traditional teaching method, the time spent on learning by students in TBL teaching was two to three times longer, on average. Moreover, in the questionnaire survey, more than half of the students believed that TBL teaching increased the learning workload, which is consistent with the findings in a previous investigation.Citation15 Interviews of teachers revealed that the teachers’ workload in TBL teaching was heavier than that in traditional LBL teaching. Teachers took more time and effort to become well prepared for the class. This result is consistent with that in previous investigations, suggesting that TBL is labor intensive for training large groups.Citation26 Certainly, the increase in labor input of the teachers was related to the necessity of an adaptation period for a new teaching model. Whether TBL generates a heavier class preparation workload than LBL requires further investigation.
Merits and limitations of this study included that it was conducted under the background that diagnostics has been rarely taught using TBL in China, and the teaching effectiveness of TBL and LBL with respect to the topic of symptomatology was compared through an RCT, which is innovative and has a certain reference value. Furthermore, the continued effect of the TBL teaching effectiveness observed in this investigation likely provides implications for further studies on the effect of the TBL teaching model on individual self-learning and on the cultivation of a long-term learning habit. However, due to the limited class hours in this study, only a relatively restricted content of the course was tested, with a small sample size and short interval time. All these factors likely hinder the demonstration of the advantages of TBL and also weaken the strength of the evidence, which is the shortcoming of this study. Consequently, the results should be further validated through more extensive studies. Furthermore, the heterogeneous grouping principle was not adopted in this study. The composition of each TBL subgroup in terms of academic level, personality traits, was not made equal, likely causing large variations in experience and benefits by the students in each TBL subgroup and a consequently poor representation, which is a shortcoming in the study design.
Conclusion
In a teaching diagnostics course, with respect to knowledge impartation, the TBL method was as effective as the traditional teaching method and showed a certain continued effect of the teaching effectiveness superior to that of LBL. Moreover, TBL was highly accepted by students in the improvement of the medical students’ interest in learning and self-directed learning ability and cultivated teamwork skills. Although the teachers and students spent more time and effort in the TBL method, they still evaluated TBL teaching positively. TBL is regarded as an effective teaching method worthy of promoting.
Acknowledgments
We thank all the students who participated in this program, as well as all staffs of administration center of medicine, School of Clinical Medicine, Sichuan University, and we also thank Medica Communicus Asia, Inc., for translating and editing whole parts of the manuscript. Both Zeng Rui and Xiang Lian-rui should be considered as the first authors. This project was supported by the National Natural Science Foundation of China (grant no 81200153), the Science Foundation of Science and Technology Department, Sichuan Province (grant no 2015SZ0180, 2015SZ0148, and 2015SZ0192), and the Science Foundation of Health Department, Sichuan Province (grant no 20120213).
Disclosure
The authors report no conflicts of interest in this work.
References
- MichaelsenLKBaumanKAFinkLDTeam-Based Learning: A Transformative Use of Small Groups in College TeachingSterling, VAStylus Publishing Press2004
- BurgessAWMcgregorDMMellisCMApplying established guidelines to team-based learning programs in medical schools: a systematic reviewAcad Med201489467868824556770
- MichaelsenLKParmeleeDXMcMahonKKLevineRETeam-Based Learning for Health Professions Education: A Guide to Using Small Groups for Improving LearningSterling, VAStylus Publishing Press2008
- KilgourJMGrundyLMonrouxeLVA rapid review of the factors affecting healthcare students’ satisfaction with small-group, active learning methodsTeach Learn Med2016281152526787081
- ThompsonBMSchneiderVFHaidetPTeam-based learning at ten medical schools: two years laterMed Educ200741325025717316209
- GrayJFanaGTCampbellTBHakimJGBorokMZAagaardEMFeasibility and sustainability of an interactive team-based learning method for medical education during a severe faculty shortage in ZimbabweBMC Med Educ20142811463
- HuntDPHaidetPCoverdaleJHRichardsBThe effect of using team learning in an evidence-based medicine course for medical studentsTeach Learn Med200315213113912708072
- NiederGLParmeleeDStolfiAHudesPDTeam-based learning in a medical gross anatomy and embryology courseClin Anat2005181566315597377
- WienerHPlassHMarzRTeam-based learning in intensive course format for first-year medical studentsCroat Med J2009501697619260147
- FatmiMHartlingLHillierTCampbellSOswaldAEThe effectiveness of team-based learning on learning outcomes in health professions education: BEME Guide No. 30Med Teach2013351216081624
- YangLHJiangLYXuBEvaluating team-based, lecture-based, and hybrid learning methods for neurology clerkship in China: a method-comparison studyBMC Med Educ20142011418
- BorgesNJKirkhamKDeardorffASMooreJADevelopment of emotional intelligence in a team-based learning internal medicine clerkshipMed Teach2012341080280623009257
- HaidetPLevineREParmeleeDXGuidelines for reporting team-based learning activities in the medical and health sciences education literatureAcad Med201287329229922373620
- LikertRA technique for the measurement of attitudesArch Psychol1932221155
- ThomasPABowenCWA controlled trial of team-based learning in an ambulatory medicine clerkship for medical studentsTeach Learn Med2011231313621240780
- TanNCKandiahNChanYHUmapathiTLeeSHTanKA controlled study of team-based learning for undergraduate clinical neurology educationBMC Med Educ20111149122035246
- RobertKSandyCJanilPFrankS21st century learning in medicine: traditional teaching versus team-based learningMed Sci Educ20122215764
- HemmatiMMParizadNZareieFThe impact of team-based learning on nervous system examination knowledge of nursing studentsJ Caring Sci20154433133926744732
- AnwarKShaikhAASajidMRCahusacPAlarifiNAAl ShedoukhyATackling student neurophobia in neurosciences block with team-based learningMed Educ201520428461
- KolesPGStolfiABorgesNJNelsonSParmeleeDXThe impact of team-based learning on medical students’ academic performanceAcad Med201085111739174520881827
- Kühne-EversmannLEversmannTFischerMRTeam- and case-based learning to activate participants and enhance knowledge: an evaluation of seminars in GermanyJ Contin Educ Health Prof200828316517118712804
- ParmeleeDXHudesPTeam-based learning: a relevant strategy in health professionals educationMed Teach201234541141322471918
- BalwanSFornariADiMarzioPUse of team-based learning pedagogy for internal medicine ambulatory resident teachingJ Grad Med Educ20157464364826692979
- HarakuniSUNagamotiJMMallapurMDEffectiveness of team-based learning in microbiology: a non-randomized control studyEduc Health20152814144
- ParmeleeDXMichaelsenLKTwelve tips for doing effective team-based learning (TBL)Med Teach201032211812220163226
- ShellenbergerSSealeJPHarrisDLJohnsonJADodrillCLVelasquezMMApplying team-based learning in primary care residency programs to increase patient alcohol screenings and brief interventionsAcad Med200984334034619240441