 ?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Biomineralization is a dynamic, complex, lifelong process by which living organisms control precipitations of inorganic nanocrystals within organic matrices to form unique hybrid biological tissues, for example, enamel, dentin, cementum, and bone. Understanding the process of mineral deposition is important for the development of treatments for mineralization-related diseases and also for the innovation and development of scaffolds. This review provides a thorough overview of the up-to-date information on the theories describing the possible mechanisms and the factors implicated as agonists and antagonists of mineralization. Then, the role of calcium and phosphate ions in the maintenance of teeth and bone health is described. Throughout the life, teeth and bone are at risk of demineralization, with particular emphasis on teeth, due to their anatomical arrangement and location. Teeth are exposed to food, drink, and the microbiota of the mouth; therefore, they have developed a high resistance to localized demineralization that is unmatched by bone. The mechanisms by which demineralization–remineralization process occurs in both teeth and bone and the new therapies/technologies that reverse demineralization or boost remineralization are also scrupulously discussed. Technologies discussed include composites with nano- and micron-sized inorganic minerals that can mimic mechanical properties of the tooth and bone in addition to promoting more natural repair of surrounding tissues. Turning these new technologies to products and practices would improve health care worldwide.
Introduction
Enamel, dentin, cementum, and bone are natural composites of both organic and inorganic components. Bone, cementum, and dentin are specialized connective tissues, while enamel has an ectodermal origin. For the specialized connective tissues (bone, cementum, and dentin), collagen type I constitutes ~90% of their organic component;Citation1,Citation2 noncollagenous proteins form the remaining. On the other hand, enamel has little or no collagen, and its organic matrix is made up of noncollagenous protein, which is 90% amelogenin.Citation3 The inorganic component of these hard tissues consists of biological apatite, Ca10(PO4)6(OH)2. Enamel has more inorganic content (~90% prismatic crystals) than dentin and bone (~70%) and cementum (45%). The unit cell of biological apatite is hexagonal in shape; repetitions of the unit cells produce crystals of various sizes. In dentin, the crystals are plate like of 50 nm length, 20 nm width, and 2–5 nm thickness.Citation4 In bone, the crystals are known to be ~2–6 nm thick, 30–50 nm wide, and 60–100 nm long.Citation5 However, they are bigger and highly oriented in enamel than in bone and dentin, making it the hardest tissue in the body. Due to the presence of a variety of substitutions and vacancies within the biological apatite, its calcium–phosphate ratio is different from that of stoichiometric hydroxyapatite (HA, 1.67). Enamel apatite, resembling the stoichiometric HA, has fewer substitutions than bone and dentin mineral.Citation6 Examples of ion substitution that could occur in biological apatite include substitution of calcium ions with magnesium and sodium, substitution of hydroxyl sites with fluoride and chloride, and substitution of both phosphate and hydroxyl sites with carbonate. With ion substitutions, a considerable variation in apatite properties could occur, for example, magnesium substitution inhibits crystal growth, carbonate substitution increases solubility, and fluoride substitution decreases the solubility.Citation3 The carbonate content of bone and teeth HA is 4%–8%; with age, the carbonate content increases but the hydrogen phosphate decreases.Citation3,Citation4 The ratio of inorganic-to-organic contents varies according to the tissue; such variation reflects the properties of each tissue. For example, with high inorganic content, enamel is tougher and more highly resistant to force than any other hard tissues in the body. With high organic content, however, dentin is more resilient than enamel and therefore provides a resilient layer under enamel and cementum.
Furthermore, these hard tissues have different regenerative capacity. Unlike ameloblasts and odontoblasts, which leave no cellular bodies in their secreted products during the later stage of apposition, many cementoblasts and osteoblasts become entrapped by the formed cementum and bone they produce, becoming cementocytes and osteocytes, respectively. Although bone is a highly adaptive tissue (ie, continually undergoing remodeling), cementum has a very slow regenerative capacityCitation7 and is not resorbed under normal conditions. Dentin and enamel develop their definitive structure during odontogensis. Dentin has the capacity to regenerate by the formation of secondary and tertiary dentin, but enamel does not have the regenerative capacity. Unlike skeletal bones, facial bones are derived from both neural crest and paraxial mesoderm and they respond differently to growth factors and mechanical stimuli.Citation8
Mineralization of teeth and bone
Mineralization is a lifelong process, in which an inorganic substance precipitates onto an organic matrix. Normal biological processes include the formation of hard connective tissues, such as bone, dentin, and cementum, in which collagen fibrils form a scaffold for a highly organized arrangement of uniaxially organized calcium phosphate crystals.Citation9 Pathological processes of mineralization result in calcification within blood vessels or in, for example, the kidney or formation of gallstones.Citation10 Understanding the process of mineral deposition is important for the development of treatments for mineralization-related diseases and also for the innovation and development of scaffolds. However, there are still critical gaps in understanding the process. While the structure of mineralized collagen is now well understood, how mineral precipitates with the spatial and hierarchical order found in tissues is still largely unknown. Cells control the mineralization process of crystal morphology, growth, composition, and location. The molecules of the extracellular matrix (ECM) and a series of enzymes, however, direct the entry and fixation of mineral salts (calcium and phosphate ions) in bone, dentin, and enamel.
Teeth
Teeth are composed of enamel, pulp–dentine complex, and cementum. Dentine forms the largest portion of a tooth. It is 70% mineralized by weight, with the organic content accounting for 20% of the matrix, and the remaining 10% being water. Type I collagen is the primary component of the organic portion of dentine, accounting for >85%, with the remaining amounts being collagen types III and V. The noncollagenous part of the organic matrix is composed mainly of dentine phosphoprotein, accounting for ~50% of the noncollagenous part. The remaining inorganic matrix is composed primarily of HA.Citation11 Several studies have suggested that collagen in enamel matrix is completely removed with all other organic components during the course of its mineralization and maturation.Citation12–Citation14 These studies refuted the earlier theories that proposed that a small percentage of collagen is retained after enamel maturation.Citation15,Citation16 A more recent study concluded that there is minimal collagen content, mostly types I and V, found in mineralized and mature enamel in comparison with dentine.Citation17,Citation18 It is commonly believed that HAs are generally encompassed within and coated by the organic material present in the tooth structure. While the physical properties of teeth are largely attributed to the presence of enamel, it is also hypothesized that collagen acts as an active protective protein sheath of the underlying HA crystallite lattice.
Type I collagen, a heterotrimer of two α1(I) chains and one α2(I) chain folded in a triple helix structure, has a rod-like structure of 1.5 nm diameter and >300 nm long. The triple helix domain is flanked by nonhelical N- and C-propetides. This form of collagen, known as procollagen, is secreted from cells, for example, fibroblasts, odontoblasts, and osteoblasts into the extracellular spaces where it is converted into tropocollagen by the removal of N- and C-propeptides. Tropocollagen can then spontaneously self-assemble into fibrils (ie, the fibril is built from the staggered packing of the individual collagen molecules such that there are periodic gaps along the fibril surface and channels extending through the fibrilCitation19). Each collagen unit is ~300 nm long and overlaps neighboring units by ~67 nm.Citation19 Fibrils contain gap regions of 40 nm between end-to-end collagen units. Packing of collagen is stabilized by weak dispersive and hydrogen interactions as well as by strong intermolecular cross-links. This stabilization is essential for the structural stability and insolubility of collagen in water.Citation20 End-to-end elongation and lateral aggregation of collagen fibrils are responsible for increasing its diameter and migrationCitation21 toward the place where they undergo mineralization, for example, movement of collagen fibrils from the proximal to the distal predentin where the mineralization occurs.Citation3 In dentin, collagen type I accommodates ~56% of mineral in its holes and pores of fibrils. The noncollagenous proteins act as inhibitors, promotors, and/or stabilizers of mineral deposition. For example, glycoproteins prevent premature mineralization until the collagen fibrils become mature and attain their correct dimensions. Dentin matrix protein-1, an acidic phosphoprotein, plays an important role in initiation of nucleation and modulation of the morphology of mineral phase.Citation22 During dentinogensis, three types of mineralization usually occur; they include matrix vesicle-derived mineralization (in mantle dentin), ECM molecule-derived mineralization (in majority of dentin), and blood–serum-derived mineralization (in peritubular dentin).Citation23 Odontoblasts secrete an acid mucopolysaccharide, for example, chondroitin sulfate, which is a prerequisite for start of mineralization. This mucopolysaccharide is transported to the site of mineralization in dentin matrix; it attracts calcium and serves to transport minerals from cells to the ECM.Citation24
In enamel, immediately after initial dentin mineralization at the dentinoenamel junction, ameloblast cells secrete enamel matrix proteins (eg, amelogenin, ameloblastin, and enamelin) and proteinases (matrix metalloproteinase-20 and kallikrein-related peptidase-4) at the dentin surface. These proteins and proteinases are responsible for immediate mineralization of ~30% of enamel. The first formed enamel crystals (ribbons) grow between the existing dentin crystals by mineralizing around dentin proteins. These crystal ribbons then elongate at the mineralization front where enamel proteins are secreted. While they are moving away from the dentin surface, the ameloblast start secreting large amounts of enamel matrix proteins. When the entire thickness of enamel is formed, the ameloblasts become protein-resorbing cells (ie, remove enamel matrix proteins); and therefore, additional mineral is required to coincide with the bulk removal of enamel proteins and water to produce enamel with >95% mineral content. The formed crystals are long, thin, and parallel ribbons of 26×368 nm2; ~10,000–40,000 ribbons at packing density of 550 crystallites/µm2 25 form a rod (prism) with ~5 µm diameter.Citation26 Each ameloblast produces one rod; all rods are organized in a three-dimensional structure. The mineral crystals formed within the enamel rods grow in c-axis length parallel to each other all the way from dentinoenamel junction to the tooth surface, while those developed between the rods (ie, interred) have limited lengths and always ordered at angles relative to the rod crystals. Since this process of enamel formation and maturation is a cell-mediated process, completion of mineralization is associated with several morphological changes in ameloblasts; hence, the matrix removal and crystal growth occur efficiently. For calcification, the influx of calcium from the blood to the enamel matrix involves intercellular and transcellular routes. Unlike collagen-based mineralized tissues, no matrix vesicles are associated with mineralization of enamel. The mineral content is reduced from the enamel surface toward the dentinoenamel junction. The position of HA is located between the nanospheres of amelogenin.Citation3,Citation27 Therefore, ameloblasts are not only responsible for secreting the enamel matrix proteins and proteinases but also induce mineral formation and finally organize these minerals into rod and interred patterns.
Bone
During the formation of mineralized bone matrix, osteoblasts first deposit unmineralized osteoid and release mineral-nucleating proteins that catalyze the process where osteoid starts to calcify. Mineralization occurs after ~15 days. The primary phase of mineralization to ~70% of full mineralization is a rapid process, whereas the secondary phase to full mineralization is slower and can last for several months to years. This process of mineral accumulation within each site of newly formed bone together with the activation frequency of remodeling sites causes a specific mineralization pattern in the bone material. As mentioned above, type I collagen is known to be the predominant component of the ECM of bone, calcifying tendon, dentin, and cementum. Crystals may be formed within the individual type I collagen fibrils, with the same periodicity displayed by the collagen, and along the fibril surfaces in the extrafibrillar spaces between packed collagen fibrils of the bone and dentin fibers.Citation28 In 1952, Robinson and WatsonCitation29 showed that carbonated HA crystals exist within collagen (intrafibrillar deposition) with their c-axis nearly parallel with the long axis of the collagen fibril. The crystals are known to be ~2–6 nm thick, 30–50 nm wide, and 60–100 nm long.Citation5 Several studies have shown that the matrix nucleates preferentially form within the gap regions of collagen fibrils, where most crystals are well organized into parallel arrays, in almost continuous dark bands.Citation5,Citation19 While the mineral precipitates preferentially in the gaps between the collagen fibrils, the crystals have been shown to grow and eventually exceed the size of the gap.Citation19 Furthermore, mineral exists both within and external to the collagen fibrils (interfibrillar deposition); however, it is generally accepted that the majority of the mineral exists within the fibrils.Citation30 Interfibrillar mineralization of collagen is directed by the collagen matrix,Citation31 which leads to nanostructured architecture consisting of uniaxially orientated nanocrystals of HA embedded within and roughly aligned parallel to the long collagen fibril axis. Previous studies have suggested that type I collagen polypeptide stereochemistry and other factors are fundamental in the initial events of mineral deposition with the intrafibrillar spaces of the molecule.Citation32,Citation33 The side chains of polypeptide-charged amino acids are thought to contribute binding sites for calcium and phosphate ions found in the circulating supersaturated fluid of the tissues.Citation32 The configurations would conceptually bring these ions into close association and lead to their nucleation. Apatite growth and development would follow initial nucleation events to result in platelet-shaped crystals growing preferentially along collagen assemblies.Citation32,Citation34 It is clear that not all collagenous tissues mineralize and investigating the process in vivo is difficult. Therefore, many of the studies that have investigated the possible physicochemical mechanisms of mineralization used in vitro models.
The control of bone biomineralization is dynamic and complex with many theories, describing the responsible mechanisms, and many factors have been implicated as agonists and antagonists of mineralization; the deregulation of which can lead to pathological extraskeletal mineralization. The crystallization process can be considered from several different perspectives: 1) the development of crystallinity in a mineral phase developed directly from a supersaturated solution of the mineral ions, 2) the presence of polymeric (protein) polyions in the mineralizing system and how they might interact in vitro with the free ions or with nanoclusters of Ca and PO4 ions to modulate the mineralization process, 3) small integrin-binding ligand, N-linked glycoproteins (SIBLINGs) and how they might be delivered in vivo to regulate mineralization at specific sites, including the processes of nucleation, crystal growth, crystal morphology, and size regulation, and 4) the delivery of sequestered, vesicular nanoclusters of Ca and P directly from the cell or the mitochondria to the mineralization front.Citation35 Veis and DorveeCitation35 speculated that it is likely that some common mechanisms may be applicable in all cases.
Mineralization was initially viewed as a classical precipitation and growth of apatite crystals directly from interstitial fluid supersaturated with calcium and phosphate phases. Studies have shown that serum is a metastable solution from which calcium phosphate precipitates in the presence of calcifiable templates such as collagen, elastin, and cell debris.Citation36,Citation37 Recently, it was demonstrated that apatite formation in bone and teeth does not occur directly by the association of ions from solution but is preceded by an amorphous calcium phosphate (ACP) precursor phase that may later transform into octacalcium phosphate before becoming HA,Citation38 although the mechanism of this pathway is under debate.Citation39,Citation40 It has been suggested that calcium phosphate precipitation in vitro is kinetically driven, meaning that the mineral does not crystallize directly into the most thermodynamically stable product but instead precipitates first into the kinetically most accessible form, ACP, which is subsequently transformed into the most thermodynamically stable phase. ACP formation is thought to proceed through subnanometer-sized prenucleation clusters with a chemical composition Ca9(PO4)6, which are stable clusters present in solution before nucleation as was recently demonstrated for CaCO3.Citation41 However, the role of these nanometer-sized clusters as building blocks for ACP formation has been debated for many years.Citation40 The origin of the mineral and how it infiltrates the collagen fibrils are still unknown.
ECM noncollagenous proteins (NCPs, now known as SIBLING) are believed to control several aspects of the mineralization process, specifically through the mechanisms of inhibition and promotion by phosphoproteins, glycoproteins, Gla-containing proteins, and proteoglycans.Citation31 It has been shown that protein concentration and whether the protein is free or immobilized can profoundly affect function in precipitation models. Presently, there is no clear role of these SIBLINGs, although it has been suggested that SIBLINGs regulate solution crystal growth by an epitaxial relationship between specific crystallographic faces and specific protein conformers.Citation31 Osteocalcin and osteopontin are two of the most abundant noncollagenous proteins, and both have been shown to influence the deposition of mineral within the collagen fibril-rich bone ECM. In vitro studies have shown osteocalcin and osteopontin control HA nucleation, size, shape, and orientation.Citation42,Citation43
Regulation of the mineralization process is also known to rely largely on inorganic pyrophosphate (PPi), a potent inhibitor of mineralization. Osteoblast and osteocyte-derived matrix vesicles control extracellular PPi levels with a host of factors, at least three other molecules: nucleotide pyrophosphatase phosphodiesterase 1, ankylosis protein (ANK), and tissue-nonspecific alkaline phosphatase (TNAP). TNAP is an enzyme that hydrolyses and inactivates PPi and is normally expressed at sites of mineralization during development. Loss of TNAP function results in hypomineralized bone.Citation44–Citation46 Conversely, ANK is expressed in nonmineralizing tissues, where it transports PPi to the extracellular space to antagonize mineralization. Loss of functional mutations in ANK causes hypermineralization and the formation of bone spurs or bone-like hardening of tendons and ligaments of the spine.Citation47 Much of the in vivo evidence regarding the role of specific proteins comes from their distribution and genetic knockout studies. However, proteins such as osteopontin have multiple roles, complicating interpretation. Tissue localization can give clues to a role but does not provide any functional information.Citation30
How Ca and PO4 ions are delivered to the mineralization front is still a matter of debate. Pioneering studies have suggested the role of mitochondria in taking in large amounts of Ca and PO4 ions, accumulating them, and delivering calcium phosphate in membrane bound vesicles to the extracellular spaces of mineralizing cartilage and bone.Citation35,Citation48,Citation49 Matrix vesicles are extracellular, membrane-invested vesicles 50–200 nm in diameter and are formed by polarized budding from the surface membrane of chondrocytes, osteoblasts, and odontoblasts. The signals that release matrix vesicles are not well understood, although the concentrations of intracellular calcium and extracellular phosphate may be important.Citation50 Mineralization begins with the formation of HA crystals within matrix vesicles, followed by propagation of HA through the membrane into the ECM. The origin of calcium and phosphate within the vesicles has not been elucidated. When the accumulation of calcium and phosphate exceed the solubility point for calcium phosphate, deposition of HA occurs within the matrix vesicles.Citation50 In the second step, HA crystals penetrate the matrix vesicle membrane and are elongated into the extracellular space. The ratio of phosphate ions to PPi is crucial in the second step of mineralization. PPi, which inhibits the formation of HA,Citation51 is formed by nucleotide pyrophosphatase phosphodiesterase 1. Alkaline phosphatase hydrolyses PPi to generate phosphate ions. The mechanisms by which vesicles may be broken open and their mineral contents transferred and localized to the collagen are still a subject of current study and debate.Citation35 There is abundant evidence that the mineral-containing intracellular vesicles do exist, and their contents in different situations contain ACP or apatite needle-like crystals. Mahamid et alCitation52 showed that mineral is released in globules (presumably ACP) from cells at the growth zone. Further questions that remain unsolved are those surrounding the mechanisms by which the mineral is transformed from the mitochondria to the mineralizing matrix, then reordered, in essence dissolved, and recrystallized on the collagen fibril matrix on the fibril surfaces, or within the fibrils themselves.Citation35
Role of calcium and phosphate ions in teeth and bone
Calcium phosphate is fundamental for the formation of bone and teeth and is essential for achieving optimal peak bone mass in the first 2–3 decades of life and for the maintenance of bone in later life.Citation53 Mineral concentration is a major determinant of the elastic modulus of the bone matrix. As the mineral fraction of the bone ECM increases, hence does the elastic modulus.Citation54 Therefore, different tissues in the body can provide either rigidity (high mineral content) or flexibility (low mineral content).
The HA in teeth varies from empirically derived HA, and HA found in bones, as the dental version, is often calcium deficient due to fluorine substitutions – EquationEquations 1(1) and Equation2
(2) – that shows the stoichiometric formula of HA (EquationEquation 1
(1) ). The formula of HA shows the sites for atomic substitution (EquationEquation 2
(2) ). This HA is calcium deficient and carbonated. X, calcium substitution with metal cation; Y, phosphate substitution with carbonate; and Z, hydroxide substitution with fluoride.Citation55–Citation57
Calcium-deficient carbonated HA comprises the major substitution activity that takes place. Other much smaller number of substitutions occur where calcium ions, ~1%, is replaced by other metal ions, including potassium, sodium, and magnesium.Citation58 The presence of carbonates and other ionic substitutions significantly disrupts the crystal lattice in HA. This weakens the HA, increasing its susceptibility to acid attack and solubility.Citation59 The carbonate content of dentine is 5%–6%, while in enamel it is 3%, and the HA crystal size in dentine is much smaller than those in enamel, thus making dentinal matrix much more vulnerable to acidic attack.Citation60
With age, the crystallinity of dental HA decreased but the carbonate content increased. The α-lattice constant, associated with the carbonate content, decreased while the c-lattice, associated with hydroxyl sites, does not change significantly with age. Increased crystal structure disorder and reduction in crystallinity are expected with higher number of planar carbonate ions substituting for tetrahedral phosphate ions in the apatite structure.Citation61 Both A- and B-type of carbonate substitutions are present but the B-type (carbonate for phosphate) is greater than the A-type (carbonate for hydroxyl).Citation61 Since c-lattice parameter is nearly age independent; this indicates that the phosphate tetrahedron represents the main site of carbonate substitution in the apatite lattice.Citation61 A decrease in crystallinity and increase in carbonate content favor the dissolution of dental apatite. This is a change in material phase and the composition of dental mineral, while also reducing crystal size.Citation61 The carbonate content has a significant effect on the reactivity and solubility of physiological HA.
Calcium, phosphate, and fluoride ions play an important role in the battle between demineralization and remineralization processes and accordingly modify the susceptibility of tooth to caries progression.Citation62 During demineralization, calcium release precedes phosphate release from enamel, dentin, and cementum. Therefore, using calcium rather than phosphate to suppress the demineralization process would be effective.Citation63
Demineralization–remineralization dynamics in teeth
Demineralization is the process of removing minerals ions from HA crystals of hard tissues, for example, enamel, dentin, cementum, and bone. Restoring these mineral ions again to the HA crystals is called remineralization. Both processes occur on the tooth surface, and a substantial number of mineral ions can be lost from HA without destroying its integrity but high sensitivity to hot, cold, pressure, and pain would be expected. Lacking of the integrity of HA latticework, however, produces cavities. Demineralization is a reversible process; hence, the partially demineralized HA crystals in teeth can grow to their original size if they are exposed to oral environments that favor remineralization.Citation64
Demineralization
Similar to bone, teeth are composites comprised of the phosphate-based mineral HA in the enamel, collagen in the dentine, and living tissues.Citation65–Citation67 However, it is the anatomical arrangement and location of teeth that sets them apart from bones.Citation68 Exposed to food, drink, and the microbiota of the mouth, teeth have developed a high resistance to localized demineralization unmatched by other mineralized tissues.Citation59,Citation69 This resistance is chiefly due to the enamel layer that covers the crown of the teeth.Citation70,Citation71
Chemical demineralization of teeth is caused by acidic attack through two primary means: dietary acid consumed through food or drink and microbial attack from bacteria present in the mouth.Citation69,Citation72,Citation73 Published literature in this area seeks to apply chemical theory to the erosion of dental hard tissues, chiefly enamel.Citation59,Citation74,Citation75
During an acidic attack, or a typical demineralization regime, chemical dissolution of both the organic and inorganic matrix components takes place. This is brought about by the water content of enamel and dentine, which facilitate acid diffusion in and mineral content out of tooth.Citation60
Etiology and risk factors: a multifactorial process
Demineralization and the subsequent erosion and/or loss of tooth surface versus remineralization are dynamic processes that are dependent on several modifying factors, as shown in . These factors are split into two main groups, extrinsic and intrinsic, which can be altered by the last group, the modifying factors. Extrinsic factors include diet and medication. Intrinsic factors are mostly diseases that can sometimes be treated with medications that are themselves extrinsic factors of erosion. Modifying factors can be variations in the biochemical characteristics of an intrinsic or extrinsic factor, behavioral patterns such as regular tooth brushing, some of which can also be classed as socioeconomic factors.
Table 1 Interaction of different factors in relation to tooth surface loss
Erosion and carious lesions are the two main consequences of demineralization. Public awareness of dental erosion is still not widespread, and its differential diagnosis among dental professionals has proven to be a challenge.Citation76 The dietary consumption of soft or fruit-based drinks in the developed world is thought to be over half of all of the liquids consumed.Citation77 The spread of the commercialization of the soft drinks market has increased by 56% over the past 10 years and is growing by a rate of 2%–3% yearly.Citation78 In 2002, the consumption of these high acid drinks was predicted to show an increase in dental issues over the following 5 years.Citation74,Citation79 This has been shown to be the case, as repeated studies have shown erosion throughout different demographic groups.Citation55,Citation77,Citation78,Citation80,Citation81
Erosion and its extrinsic causative factors have been included in the UK Children’s Health Survey since 1993, and a trend toward higher prevalence of erosion in those who often consumed carbonated drinks was shown.Citation82 In the UK in 2003, >50% of 5–6 years old had exhibited significant enamel erosion, linked to the consumption of acidic drinks. Furthermore, 25% of 11- to 14-year olds had significant erosion, rising to 77% in 20- to 25-year olds.Citation83,Citation84 A recent study in 2015 showed an increase in pediatric dental hospital admissions, with cases strongly linked to sugar erosion.Citation85 There is a widespread misunderstanding by patients that the extraction of primary teeth is not a matter of concern, since these will be replaced by permanent teeth. This has been repeatedly shown to be false, and the damage done by the primary teeth issues may be affecting the future health of the permanent teeth.Citation66,Citation80,Citation86,Citation87 Previous in vitro models were made on the belief that the tooth–acid interactions last for several minutes. However, more recent in vivo studies suggest that the in vitro tooth–acid models should focus on the acid interaction for 30 seconds. This would better represent in vivo conditions.Citation78,Citation86,Citation88
The most recent study in the US has shown that 79% of adults have at least moderate evidence of tooth decay; regardless of demographic, the key feature was the excessive daily consumption of fruit juices and soft drinks.Citation89 The most recent study in the Peoples’ Republic of China showed 89% tooth wear among 15 years old, with 7% showing dentine exposure; a mark of the severity of the erosion.Citation90 Other studies from Japan and India also showed comparable data for early-stage tooth erosion.Citation91,Citation92 Modifying behavioral factors that affect dietary consumption include types of drinks consumed, method by which a drink is consumed, and frequency of drinking. For example, an increase in agitation when a drink is swished around the mouth will enhance the dissolution process.Citation93 Moreover, several medication and asthmatic inhalers were shown to induce xerostomia by reducing salivary flow, in addition to decreasing its pH; thus, weakening its overall buffering effect against intrinsic and extrinsic acids.Citation94,Citation95 Saliva is considered one of the most important biological factors in dictating the intraoral neutralizing effects of acid exposure. Pathogenesis of dental erosion is directly related to the buffering capacity and rate of secretion of saliva.Citation96
The mineralization percentage of permanent teeth is higher than that of primary teeth;Citation68 nevertheless, adults frequently experience the effects of acid damage on teeth. Mechanically, the teeth are softer and weakened, although there is no change in the brittleness. Intrinsic factors that may lead to erosion include gastroesophageal reflux, often seen in diabetic and obese individuals, bulimia nervosa, and dental rumination. Diseases such as bulimia nervosa have the symptom of self-induced vomiting, which can be a leading cause in dental erosion if occurring often enough. For gastroesophageal reflux, it is defined as a normal physiologic retrograde flow of gastric contents and acid regurgitation into the esophagus and sometimes mouth, which occurs mostly postprandial, after meals, for ~1 hour.Citation97 Irrespective of the cause, excessive stomach acid has a deleterious effect on dental health. Endogenous acids has a pH of 1.2, that is well below the critical pH for fluoroapatite (FAP) and HA dissolution,Citation66,Citation98,Citation99 thus leading to rapid demineralization of tooth surfaces. Regardless of the type of causative factors, teeth eroded by acid are more likely to crack or chip if damaged and are harder to repair.Citation100,Citation101 The areas of structural weakness that have been demineralized are also targets for caries formation.Citation74,Citation102,Citation103 Bacteria can easily colonize the demineralized areas of the tooth and, with a combination of their own acid formation, are able to penetrate into the dentine.Citation81,Citation104 The dentinal contribution of the demineralization-assisted caries is higher than when acid drinks are not involved and is a marker of the severity of the caries.
Bacteria
Dental caries is the most common childhood chronic infectious disease. It is caused by the interaction of bacteria, mostly Streptococcus mutans, and sugar on tooth enamel surface. Bacteria breakdown fermentable carbohydrate such as glucose, sucrose, and fructose and cause an acidic environment that leads to demineralization and resultant carious lesions.Citation98,Citation99 There are several theories proposed as to how oral bacteria are actually acquired. At birth, the oral cavity is known to be effectively sterile; however, acquisition is achieved via transmission from food/milk/water, from parents, or from oral mucosa shedding surface during eruption of primary dentition. The most widely accepted hypothesis with regard to the role of bacteria in acid production and caries formation is the “ecological hypothesis”, where dental plaque is defined as a dynamic microbial ecosystem in which nonmutans bacteria are key players for maintaining dynamic stability.Citation93 S. mutans, Streptococcus sobrinus, and lactobacilli are the main oral cariogenic pathogens due to their ability to produce high levels of lactic acid following sugar fermentation and their resistance to the adverse effects of low pH.Citation105,Citation106 In some studies, S. mutans were seen to be >30% of oral microflora in children with early childhood caries.Citation107 Higher frequency of sugar intake leads to increased risk and susceptibility to caries due to prolonged exposure to acidic conditions, regardless of the amount ingested.
Acid erosion mechanisms
Dental erosion can be defined as being the loss of hard tissues though dissolution by acids of nonbacterial origin or mechanical damage. When exposed to acid, teeth become softer as the HA is solubilized, and therefore, more susceptible to mechanical wear. The two chemical methods by which this can occur are either direct acid attack or chelation.Citation57,Citation74,Citation90
When hydronium ions are formed from an acid in solution, they bind with carbonate or phosphate in HA, releasing the anions into solution in a form of chemical etching. Carbonate is more reactive than phosphate, and requires a lower concentration of hydronium to react with, and is therefore why HA is weaker with excess carbonate.Citation57
Three phases of attack have been identified, based on the pH of the acid.Citation108 Acids with pH <1 can cause surface etching when exposed to teeth for very short time periods. Nanoscale surface softening occurs with short exposure at pH 2–4, but this does not extend to the macroscale.Citation70,Citation109 The third and most common form of acid attack is through weak acid (pH 4.5–6.9) subsurface dissolution. This along with bacteria can lead to the formation of carious lesions and as a result has been well studied.
Exposure to acids with pH >4 is not a common biological occurrence. Emesis is the normal mechanics, whereby stomach acids can come into contact with the teeth. Some patients with the most severe and prolonged hyperemesis episodes, such as those with alcoholism, may subject their teeth to acids with a pH of 1.Citation55 This is well below the demineralization pH and can cause surface etching, which is highly dangerous for teeth. Dentition in patients with intrinsic disease factors such as hyperemesis gravidarum or bulimia may be exposed to low pH acids regularly enough to cause nanoscale surface softening.Citation70,Citation109,Citation110 However, the weak acid dissolution pathway has many possible causes. Fruits commonly have carboxylic or citric acids.Citation87,Citation109 The hydronium ion formed by carboxylic acids readily binds with phosphate, forming phosphate cations.Citation55,Citation111 These cations can form a calcium acid chelation complex, debonding mineral ions in the surrounding lattice causing widespread demineralization.Citation74 Alternatively and more rarely, these can remain in proximity to the HA layer, with minimal demineralization.
Carboxylic acids can also allow for attacks through chelation. Fruit acids such as citric acid (C6H8O7) are commonly found examples of this. In citric acid, the COOH group is dissociated, forming H+ for H3O+ and allowing a COO− anion to cause calcium chelation.Citation87 The direct acid attack, using hydronium ions, has already been described above. Two anions, however, are able to form a soluble chelate complex with three calcium ions. This is dependent on the dissolution strength of the anion relative to the bound calcium in HA and results in the formation of a chelate at pH 3.8–4, the pH of fruit and fruit drinks.Citation93 As the chelate is soluble, this can then be carried from the enamel surface, resulting in a net loss of mineral for the teeth. Although commonly found in fruits and soft drinks, citric acid is particularly damaging teeth, and it can act through two mechanisms to remove both phosphate and calcium from the HA.Citation77,Citation88 Carbonic acid behaves similarly to citric acid; however, the dissolution constant is lower (pKa 3.6) compared with citric acid (pKa 6.4). Carbonic acid can disassociate to form both bicarbonate anions HCO3− and orthocarbonic acid C(OH)4, which increases the risk of acid attack on teeth.Citation57,Citation112 The amount of carbonic acid added to carbonated (“fizzy”) drinks is often too low to have significant effects.
Although the carbonic acid content may be low, the presence of phosphoric acid in soft drinks, especially cola products, is damaging to teeth. Phosphoric acid (H3PO4) does not contain a carboxylic group but still attacks teeth through both the direct pathway and chelation.Citation112,Citation113 Two hydrogens disassociate from phosphoric acid, allowing two hydronium ions to be formed for direct acid attack.Citation18,Citation77 The remaining phosphate ion (PO43−) can chelate with calcium cations at ratio of 2:3, forming soluble calcium phosphate. Some hydrogen phosphate (HPO42−) is also formed that chelates with calcium cations in a 1:1 ratio. Both pathways occur at low pH ranges and contribute to demineralization with acidic and sparkling drinks; the effect of which is seen in .Citation108,Citation113
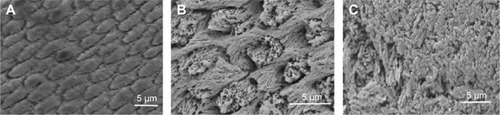
Figure 1 Scanning electron microscopic images showing (A) normal enamel, (B) enamel etched with phosphoric acid at the same concentration as found in drinks, and (C) the recrystallized HA after solubilization (edges of the image) compared to unetched HA (center of the image).
Abbreviation: HA, hydroxyapatite.
Chemical erosion mechanisms
When discussing tooth erosion, pH is important, but it is not necessarily the crucial factor.Citation114,Citation115 The routes of direct acidic attack have been seen at length and are well documented. Irrespective of the exact type of acid in a drink, a lower pH dissolves HA in enamel at a faster rate and more severely than would a higher pH acid drink. Chelation causes a destabilization of the HA surface at low pH, weakening the phosphate coordination bonds.Citation60 Acid concentration in molarity should also be taken into consideration. Titratable acidity, the amount of alkali required to titrate the subject to its natural value, has been used to measure the concentration of acids present in drinks.Citation116 Although the pH ranges that can be tested using this method are often not found in commercial products, nor is the length of exposure relevant to drinking, titratable acidity remains a commonly tested value.Citation117 While pH measures just the dissociated ions in a solution, which could form acids or alkalis, titratable acidity also measures the bound compounds giving a larger overview of the potential acidity of a solution.Citation60,Citation114,Citation117 Although titratable acidity experiments often have experimental drawbacks, an increase in titratable acidity has been shown to be linked to an increase in enamel loss in model studies.Citation80,Citation118
Linked to titratable acidity is the undissociated acid concentration, a measure of the inactive acidity of a solution. This describes solute that does not contribute to the pH of a solution.Citation115 These molecules are also uncharged, which allows for a localized increase in hydrogen ions once diffused into the HA. Acids that have a low pKa have an increased concentration of molecules in a disassociated form.Citation93 These hydrogen ions react with water to form hydronium ions, which are delivered to enamel. This high concentration of hydrogen ions favors dissolution of the enamel, at a layer known as the mineralization front.Citation93 Short-term erosion sides have shown significant reduction in hydrogen when the disassociated value of acids was changed to favor higher pH levels.Citation117 The pH remains the value that is most quoted for expositors to dietary acid over normal eating or drinking timescales.
The equilibrium constant for acid dissociation (Ka) and its logarithmic value (pKa) indicate the ratio of ionized-to-nonionized acid groups in aqueous solution.Citation119 A solution with equal pKa and pH values will have 50% chelator anions and 50% disassociated acid in solution.Citation60 pKa values alter with environment, solvent, and structural changes. The pathway by which an acid is likely to attack HA in teeth can be predicted from the pKa value. A carboxylic acid with a low pKa value in water is likely to produce a high number of chelating ions, while a higher pKa value suggests direct hydrogen ion attack.Citation60 Although citric acid has a low pKa value (3.1) in water compared with hydrochloric acid (−6.1), it does not mean that the carboxylic acids are not damaging.Citation120 Ka or pKa values cannot be used to directly measure the severity of an acid but is crucial in modeling other values.Citation118
Although chemical and mechanical methods of erosion are often considered separately, models such as the differential buffering capacity (DBC) of an acid can predict the mechanical effects of acid demineralization.Citation117,Citation121 DBC is measured as the gradient of a titration curve at a certain pH value and gives the concentration of acid required to lower the pH by 1.Citation122 Acids with lower DBC values have been shown to have more severe effects on enamel for short-term exposure than higher DBC values.Citation117,Citation121 The DBC value of an acid is made up of the pKa and pH values and is therefore considered to be a more reliable marker of erosion properties over long-term exposure, when the pH range is relevant for dietary exposure.Citation122
Temperature has a significant impact on the kinetics of dissolution. In the mouth, the ambient temperature is higher than room temperature, increasing the kinetic rate of reaction.Citation68,Citation110 The ions in solution, which impact the enamel causing dissolution, exceed the total energy required for the dissolution of the calcium. The results in a greater level of demineralization would occur at room temperature but is unavoidable due to physiological conditions.Citation123
All these descriptors factor into the erosion of enamel by dietary acids. However, there is no conclusive study indicating which is more important or representative for dietary conditions.
Remineralization
This section covers both prevention and cure of demineralization that can be arrested or reversed particularly in its early stage. Saliva, fluoride therapy, diet control, and probiotic bacteria are described as preventive regimes for tooth demineralization. Dental composites containing different forms of calcium phosphates (CaPs) are discussed as potentially curative regime for tooth demineralization. The use of nanotechnology in preventive dentistry, as antibacterial nanotherapy and biomimetic remineralization for reversing an incipient caries or recurrent decay, was explained in details in the literature.Citation124
Saliva
As mentioned above, saliva is considered one of the most important biological factors in dictating the intraoral neutralizing effects of acid exposure. Pathogenesis of dental erosion is directly related to the buffering capacity and rate of secretion of saliva.Citation96 In addition to its cleansing and antibacterial action,Citation125 saliva acts as a constant source for calcium and phosphate that helps in maintaining supersaturation with respect to tooth minerals, therefore inhibiting tooth demineralization during periods of low pH, and they promote tooth remineralization when the pH returns to neutral state. Furthermore, when saliva secretion is stimulated, a rapid rise in pH to above neutrality occurs. As a result a complex of calcium phosphate and glycoprotein called salivary precipitin is formed. This complex is readily incorporated into dental plaque. Due to its high solubility of calcium phosphate in salivary proteins (eight to ten times higher than calcium phosphate in tooth), it serves as a sacrificial mineral that dissolves preferentially before tooth mineral, ie, reducing demineralization. It also acts as a source of calcium and phosphate ions that are required for remineralization of decalcified tooth.Citation63,Citation126
Saliva constantly delivers fluoride to the tooth surface; salivary fluoride is a key player in preventing tooth demineralization and enhancing remineralizationCitation125 as described in the “Fluoride therapy” section.
Fluoride therapy
Fluorination of teeth is encouraged;Citation127 the most effective method of caries prevention is through the use of topical fluoride, such as toothpaste and varnish. The calcium in HA is displaced by fluorine, forming FAP, which has a much lower solubility than either the original or calcium-deficient HA. FAP forms a solid-state solution with the phosphate-rich HA, with a hydroxide being displaced.Citation55,Citation77 FAP has two main advantages over HA, and fluorine is often added to drinking water to encourage the conversion.Citation127 First, fluoride acts as a catalyst, assisting in the remineralization enamel with phosphate ions dissolved in saliva.Citation103,Citation128 This can help to counteract any demineralization which has occurred.Citation111 Second, the displacement of hydroxide with fluoride removes a weakness in HA to lactic acid; FAP [Ca10(PO4)6F2] is not dissolved by this in the mouth.Citation74,Citation129,Citation130 For the formation of FAP, for every two fluoride ions, ten calcium ions and six phosphate ions are required. Accordingly, the presence of inadequate calcium and phosphate can limit the remineralization process. Casein phosphopeptide–ACP (CPP-ACP) has been developed for this purpose. Aggregation of CPP with calcium phosphate forms clusters of ACP. This aggregation prevents the precipitation of calcium phosphate and hence results in a state of supersaturation with respect to enamel, thus preventing demineralization and enhancing remineralization.Citation131 Some commercially available dental products contain both CPP-ACP and fluoride, and they are very effective remineralizing agents.Citation132–Citation134 Regardless of the significant effect of fluoride in preventing tooth demineralization, care as to not exceed the maximum recommended dose of fluoride is highly advised. Overconsumption of fluoride through fluoridated water/foods and/or supplements may lead to dental and/or skeletal fluorosis. Dental fluorosis is defined as mineralization defects of enamel, resulting from subsurface porosity below a well-mineralized surface zone.Citation14
Since the recovery of plaque pH to a higher level than the critical pH plays a key role in remineralization process, addition of 1.5% arginine (insoluble calcium compound) to fluoride in tooth dentifrices was more effective in reducing tooth demineralization and progression of caries to cavitation than those containing fluoride alone. The arginine is broken down into ammonia by nonpathogenic arginolytic bacteria; ammonia helps in neutralizing plaque acid and maintaining the plaque biofilm on tooth surface in a healthy state.Citation63,Citation135,Citation136
Diet control and oral hygiene instructions
Additionally, dietary advice, oral hygiene instruction, and application of fissure sealants are still used as further preventive regime to dental caries in both high- and low-risk individuals. In most recent studies, it was shown that the use of nonfermentable sugars in chewing gum, such as xylitol, was seen to inhibit the effect of S. mutans; however, more conclusive evidence is yet to be achieved.
Probiotic bacteria
Probiotic bacteria, defined as “live microorganisms which, when administered in adequate amounts, confer a health benefit on the host” (WHO), are commonly suggested candidates for bacteriotherapy.Citation137 The word probiotics means “for life”, and this is either naturally occurring or genetically engineered bacterial strains that can be used for intervention.Citation137 Examples of probiotics that have the ability to confer oral health benefits for the host include Lactobacillus (eg, salvarius,Citation138 reuteri,Citation139 and rhamnosusCitation140) and Bifidobacterium that are part of normal oral flora.Citation140–Citation142 They can be used as biotherapy for prevention or treatment of dental caries and periodontal diseasesCitation143 by reducing the number of pathogenic bacteria (S. mutans)Citation143,Citation144 or inhibiting the expression of S. mutans virulence genes, for example, GtfB and LuxSCitation140,Citation145 and therefore alter or reduce biofilm formation.Citation138
For administration of probiotic strains, several appropriate vehicles are available; they vary from dairy products, ice cream and curds,Citation146 oral thin film,Citation147 tablets,Citation139,Citation148 and lozenges (eg, PerioBalance).Citation149 The use of probiotic products found a potential use as alternative strategy for displacing pathogenic bacteria with probiotic microorganism and can therefore be exploited for the prevention of enamel demineralization.Citation146
Another avenue to reduce the cariogenicity of S. mutans is the generation of strains without the open reading frame of lactate hydrogenase.Citation150
Electrically assisted enhanced remineralization
A new technology that has been developed by Reminova LtdCitation151 relies on the use of an electric current to reverse tooth decay by boosting remineralization. The use of tiny electric current of few microamperes that cannot be felt by the patient pushes the minerals into the tooth to repair the clean defect. This process requires no injection, no drilling of tooth, and no filling materials and triggers the remineralization from the deeper portion of the lesion. The development of a model ready to use by dentists from the prototype device developed by Reminova Ltd is currently under investigation.Citation151
Dental composites with remineralizing action
Resin-based composites have been used as dental filling materials for >50 years.Citation152 These materials have evolved throughout the years. The most important changes have involved the reinforcing fillers to improve the mechanical properties, polishability, and wear resistance. Recently, the focus has shifted to equipping composite systems with remineralizing and antibacterial properties. Various forms of calcium phosphates (CaP) have been incorporated into resin-based composites to provide mineral release that could potentially remineralize the tooth structure. This section provides an overview on the development of potentially remineralizing composites for tooth repair that have recently been introduced.
Calcium phosphates in different forms have been studied as fillers to make mineral releasing dental composites. This includes ACP, HA, tetracalcium phosphate (TTCP), dicalcium phosphate (DCP) anhydrous, and mono-, di-, and TCPs. These calcium phosphate fillers partially replaced the reinforcing fillers. Unfortunately, this can compromise composite mechanical properties.
Composites containing ACP
ACP has been evaluated as filler for dental composites and adhesives. Skrtic et alCitation153–Citation155 has introduced composite materials containing ACP, which release significant amount of calcium and phosphate ions. It was demonstrated that the remineralizing potential of ACP was enhanced through its hybridization with silicon or zirconium elements. Adding these elements to ACP increased the time of mineral ion release through their ability to slow down the intracomposite ACP to HA conversion.Citation156,Citation157 Mineral ion release from ACP composites was shown to efficiently restore the mineral lost from enamel surfaces following acid attack.Citation158,Citation159 Another study has incorporated ACP into a composite adhesive system. The ACP was shown to infiltrate the dentinal tubules without causing negative effect to bond strength.Citation160
Compared with glass or ceramic-only filled composites, the ACP-filled composites are more hydrophilic and biodegradable. In addition, they exhibit inferior mechanical properties and durability.Citation161 ACP particles aggregation, poor interfacial interaction with matrix, and excessive water sorption contribute to compromising the mechanical properties.Citation155,Citation162,Citation163 Mechanical milling reduced the particles size of ACP-zirconium fillers to ~20 µm, providing more homogeneous filler distribution and a reduction in voids formation was obtained. Biaxial flexural strength was, therefore, increased from 50 to 75 MPa.Citation161,Citation164–Citation166 This is, however, still lower than the strength of commercial dental composites (100–180 MPa), restricting the use of ACP-filled composites as potential direct dental-filling materials.Citation167 A recent study showed that 120 MPa flexural strength could be obtained if the mass fraction of ACP was kept at 10 wt%. However, this significantly reduced the amount of calcium and phosphate ions that could be released.Citation168
Composites containing HA
Coupling agent treatment of calcium phosphate fillers with citric acid, acrylic acid, or methacrylic acid improved the flexural strength of composites containing HA.Citation169,Citation170 However, γ-methacryloxypropyltrimethoxysilane coupling agent had no effect on strength.Citation171 Microscopic HA fillers provided higher strength than nanoscopic fillers.Citation169,Citation170,Citation172 It was also reported that HA fillers in the form of whiskers further enhanced flexural strength.Citation173,Citation174
Water sorption of resin-based composites containing silane coupling agent-treated and -untreated HA fillers was consistent with a diffusion-controlled process. Incorporation of HA reduced the water uptake, and this decreased further upon silane treating of HA fillers,Citation175 which subsequently led to deterioration in CaP release.
In an attempt to improve the mechanical properties, small fraction (3 wt%) of HA filler were impregnated into composites. This low mass fraction of HA was well dispersed, leading to increase in the flexural strength up to 120 MPa. Raising mass fraction of HA to 10 wt% caused to decrease strength to 95 MPa due to the formation of aggregates of HA that served as a defect site.Citation176
Composites containing TTCPs
Recently, TTCP particles were investigated as potentially remineralizing fillers for dental composites. Upon addition of TTCP, the mechanical properties of the composites decreased dramatically. Replacing 50% of TTCP by silicon nitride whiskers increased the strength of the composites from 50 to 100 MPa. Calcium and phosphate ion release, however, was decreased by an order of magnitude.Citation177 Another study showed that flexural strength can reach 80 MPa for composites filled with 40 wt% TTCP. This has increased further upon addition of an antibacterial agent.Citation178
Composites containing mono-, di-, and tricalcium phosphates
Calcium phosphates in the form of monocalcium phosphate (MCPM), DCP, and TCP were also incorporated into dental composites materials. The solubility of these forms of calcium phosphate differs significantly. The mineral ion release from MCPM composite was shown to be dependent on the amount of MCPM added to the formulation. Replacing the MCPM with reinforcing whiskers was shown again to improve mechanical properties but dramatically decrease calcium and phosphate release.Citation179 Replacing MCPM with less soluble DCP enhanced the strength but significantly reduced mineral ions release.Citation180 A study showed that by decreasing the particle size of DCP fillers to ~110 nm, the amount of mineral ions release can be significantly increased.Citation181 It has also confirmed that replacing DCP with silicon nitride whiskers enhanced the strength but at the expense of the mineral ion release. In addition, incorporating whiskers in the composite formulations compromised the optical properties preventing light cure feasibility.
TCP has been added together with MCPM to enable more control on the latter dissolution and composite water sorption.Citation182–Citation185 Highly soluble MCPM on the surface of the composite dissolved but at the core it reacted with β-TCP to form less soluble brushite (DCP dihydrate). Partial replacement of calcium and phosphate with reinforcing opaque fillers improved the strength but these again compromised the mineral ion release and optical properties.Citation182 A recent study has introduced light-cured composites containing both MCPM and TCP with strength within the range expected for commercial composites.Citation183,Citation184 HA precipitation at the surfaces of these composites was used to evaluate the remineralization potential of these materials. These HA layers were formed of calcium and phosphate ions released from within the composite samples.Citation184 Although these results are promising, the ability of these composites to remineralize the demineralized dentine has yet to be demonstrated.
Demineralization–remineralization dynamics in bone
Bone remodeling is a physiologic process that continues within discrete sites following cessation of skeletal growth. During remodeling, packets of bone are laid down and turned over in order to facilitate the repair of damaged older bone. Osteoclasts resorb bone, and these resorption lacunae are subsequently filled with new bone matrix deposited by osteoblasts. As newly formed bone accumulates mineral with time, the most recently deposited bone will generally be less mineralized than bone deposited months or years earlier. Regions with high turnover, containing many newly formed osteons, generally display lower average mineralization than areas of low turnover. During secondary mineralization, the mineral content of an individual unit continuously increases with time (referred to as the mineralization law), with a steep slope in the beginning and a significant reduction in the slope after-ward.Citation186 The weight or volume fraction of mineral in the bone matrix is measured spatially by methods such as plain radiography, dual-energy X-ray absorptiometry, Faxitron X-ray microradiography, synchrotron, microcomputed tomography, and quantitative backscattered electron microscopy.
Bone remodeling is essential for the required tooth movement during orthodontic treatment. The interaction between the receptor activator of nuclear factor κB (RANK) that is expressed on osteoclast precursor cells, its ligand (RANKL) that is expressed on osteoblast cells, and osteoprotegerin is responsible for the regulation of bone remodeling process. Binding of RANKL to RANK results in differentiation of precursor osteoclast cells to mature osteoclasts. Osteoprotegerin competes with RANK for RANKL binding and inhibits osteoclast differentiation. The balance of these trimolecular control factors maintains physiologic bone remodeling.Citation187
Any imbalance between bone formation and resorption has undesirable consequences.
Demineralization (hyper- and hypomineralization)
The mineralization density at the tissue level reflects the contribution of all osteons with different degrees of mineralization and disruptions in the physiological and biochemical processes that regulate the deposition and removal of calcium apatite in a tissue may be caused by age,Citation188 disease, and drug treatment.Citation189 Small increases in mineralization lead to relatively large increases in the strength of bone, although levels ~>66% mineralization have been shown to lead to brittleness and a reduction in bone strength.Citation190
Hypermineralization and hypomineralization are deviations that occur within the mineral content of fully mineralized bone. Only a pathologically altered organic matrix and/or abnormalities in crystal size and shape can lead to a hypermineralization, a mineralization density exceeding that of fully mineralized normal bone matrix. In contrast, hypomineralization results when the organic matrix is not fully mineralized due to a lack of time for secondary mineralization and/or by a pathologically altered bone matrix, affecting normal mineralization kinetics.Citation189 Bone diseases such as rickets and osteoporosis cause a significant reduction in bone mineralization and bone mineral density, which lead to functional consequences in terms of increased fracture risk and skeletal deformity, respectively.Citation188 Mild primary hyperthyroidism is characterized by abnormally elevated parathyroid hormone serum levels accompanied by hypercalcemia, which also results in a low bone mineralization density that is thought to be due to an increased bone turnover and bone formation rate.Citation186
Osteogenesis imperfecta is a genetic disorder associated with increased bone fragility. Studies indicate a shift toward a higher mineralization density of bone tissue, only marginally exceeding that of normal adults.Citation191 Weber et alCitation192 suggested that the higher mineral content was not exclusively due to an altered collagen structure but may also be caused by an accelerated mineralization process. Alterations in bone mineral density have also been measured in male osteoporosis, idiopathic osteoporosis, patients with collagen I polymorphisms,Citation193 osteomalacia,Citation194 hypophosphatemia, Paget’s disease, Bruck’s syndrome, myopathy, renal osteodystrophy,Citation195 and liver transplantation.Citation196 All showed a shift to lower mineralization density, while pycnodysostosis,Citation197 hypoparathyroidism, osteopetrosis, and osteonecrosis all led to an increased mineralization density.Citation189
Remineralization
Some drugs have been developed to either reduce bone resorption (eg, bisphosphonatesCitation198) or promote bone formation (hormonal replacement,Citation199 calcium, and vitamin D supplements). Combination and sequential treatment using both bone formation stimulator and bone resorption inhibitors have been attempted. Combination treatment using both bone resorption inhibitors and bone-formation stimulators has not showed any additional benefit over the use of each medication alone. The use of bone-formation stimulators is independent on the previous use of bone resorption inhibitor. The use of bone resorption inhibitors; however, maintains the benefit of the former bone formation stimulator.Citation199 Generally, serious side effects, however, have now been associated with the extensive use of these drugs.Citation198,Citation200,Citation201 This, however, is not the main focus of this review. Only the materials with remineralizing action will be covered in details.
Bone cements/composites with remineralizing action
Poly(methylmethacrylate) (PMMA) has been widely used in orthopedic surgeries as anchoring agent in hip and knee replacement to repair vertebral fractures and skull defects.Citation202 To overcome the disadvantages of conventional PMMA cements such as lack of adhesion to bone and heat generation during polymerization, calcium phosphate cements and polymeric cements with mineralizing fillers have been investigated as alternatives.
Various forms of calcium phosphates have been studied as bone cements due to their excellent biocompatibility.Citation203 The main shortcomings of these materials, however, are the mechanical properties. These properties were improved through formation of polymer composites containing calcium phosphate. The polymer matrix reinforced with glass or ceramic fillers and contain CaP fillers can potentially provide remineralizing materials with good mechanical properties. This includes calcium phosphates in the forms of HA, β-TCP, and biphasic calcium phosphate.
Nondegradable cements/composites
Cements/composites containing HA. HA was used as filler in self-curing two paste bone cements. Upon immersion in simulated body fluid, the materials were shown to form an apatite layer. This feature has been associated with bone bonding ability.Citation202 Bioactive glass, HA, and β-TCP have also been used to develop bone cements that have been reported to exhibit bone-bonding properties.Citation204,Citation205 Enhanced cellular activity has been associated with increased levels of HA fillers in the composite materials.Citation206 Ultimate tensile strength, however, decreased with increased HA content.
A combination of strontium and HA containing bone cement was reported to provide superior bone-bonding strength to that with conventional PMMA cement.Citation207 Addition of HA to PMMA also enhanced the biocompatibility and osteoconductivity of the cement.Citation208
Cements/composites containing β-TCP. Composite bone cements containing β-TCP were also reported to be biocompatible, and osteoconduction was attained within 4 weeks of direct contact with bone.Citation209 A study showed that resin composite bone cements contain either bioactive glass ceramics or β-TCP that induces bone formation at the interface.Citation210 However, the mechanical properties of the former were higher than the latter.
Biodegradable calcium and phosphate cements
Calcium and phosphate cements have been investigated as synthetic materials to fill bone defects and cavities due to their excellent biocompatibility and osteoconductivity.Citation203,Citation211 The formation of these materials is activated by mixing various calcium phosphate phases with a liquid phase at a specific pH. The pH of the chemical reaction dictates the type of final product; HA forms at pH >4.2 or brushite at pH <4.2.Citation211,Citation212 Unlike brushite (CaHPO4⋅2H2O), HA-based cements were shown to have poor solubility at a physiological pH.Citation213 Calcium and phosphate cements are brittle with low strength and can only be used in nonload-bearing applications.Citation211
Apatite cements
Commercially available apatite cements were developed using different chemical formulations containing more than one type of calcium phosphates such as α-TCP, MCPM, and TTCP. Precipitated HA or calcium-deficient HA can be formed by hydrolyzing calcium phosphate or by mixing two calcium phosphate powders with Ca:P ratio lower than the stoichiometric ratio for HA (Ca:P =1.67).Citation214 These materials were shown to have poor solubility and subsequently reduced chances of replacement with natural bone tissues.
Brushite cement
These cements have been developed to take advantage of their high solubility in order to increase the amount of regenerated tissues.Citation211 In a physiological condition, brushite dissolves providing calcium and phosphates ions, in addition, to their high biocompatibility and osteoconductivity.Citation215 Mechanical properties of brushite cements, however, are lower than apatite cements. Today, research is focused on improving the overall performance of brushite by balancing resorbability and mechanical properties.
Throughout this review, the mechanisms of demineralization–remineralization in both teeth and bone as well as therapies that boost remineralization have been thoroughly discussed. Understanding these processes is also important for the innovation and development of scaffolds or implant surfaces that are able to stimulate mineralization or osseointegration. The interaction of biomaterials with host tissues is an important issue that has to be addressed during designing scaffolds or implants for biomedical use. The topography, chemical, and mechanical properties of the materials from which scaffolds or implants has been made have fundamental influence on the host response. Some innovative approaches seem to be promising in designing scaffolds or implants with topographical features that favor osteogenic differentiation. Electrospinning, rapid prototyping,Citation216 and two-photon polymerizationCitation217 could be promising in designing scaffolds with biomimetic architecture, required for nutrient supply and diffusion, as well as with instructive surface properties required for directing cells into the proper lineage. Osteoprints, bioinspired two-photon polymerized 3D trabecular-like structures, deeply influenced cellular behavior, enhanced osteogenic differentiation, and increased HA production.Citation217 Direct laser writing/atomic layer deposition,Citation218 lithography, ionic implantation, anodization,Citation219 radio frequency plasma treatments,Citation220–Citation223 and surface treatment (eg, glow discharge, acid etching, or UV irradiation)Citation224 have been used to tailor implants’ surface topography in favor of osseointegration.Citation225,Citation226 Controlling the surface topography at nanoscale level or chemistry of scaffolds or implants could influence cells spreadingCitation222 and differentiation.Citation220,Citation221 Modification of chitosan scaffolds with barium titanate nanoparticles or strontium phosphate favored the osteogenic differentiation of mesenchymal stem cells.Citation227,Citation228 Nanoarrays from tantala improved adhesion, proliferation, and differentiation of osteoblast cells on implant surface.Citation229 Biofunctionalization, that is, immobilization of specific active biomolecules known with their effective role on osteogensis on the surface of scaffolds or implants, has also been attempted to improve their long-term acceptance.Citation230 Examples include ECM proteins,Citation231 adhesion molecule (arginyl-glycyl-aspartic),Citation232 and bone morphogenic protein.Citation233
Concluding remarks and future prospects
Demineralization–remineralization is a dynamic process, and there is always a battle between them. Both processes can occur on the hard tissues surface to some extent. They therefore have an impact on the health of hard tissues, and the surrounding environment plays a key role in determining which process wins the battle. Therefore, the main aim would be maintaining the environment that prevents demineralization but encourages remineralization.
The understanding of the process of demineralization and remineralization in teeth is very well understood. However, despite efforts by researchers and clinicians, maintaining a good oral and dental health throughout patients’ life remained a big challenge. The constant change in diet associated with the more and more widespread accessibility of fizzing sugary drinks is putting pressure on the whole dental profession to safeguard good oral and dental health, even in wealthy country. A University College London survey at the London 2012 Olympic Games found that 18% of athletes said that their oral health had a negative impact on their performance and 46.5% had not been to the dentist in the past year. In terms of dentistry, the challenge in the next decade is to either promote a change in the habits of population or for scientists to develop new products that may counter the demineralization process that results from the consumption of these fizzing sugary drinks. The more and more widespread prevalence of dental caries is a direct consequence of this growing population behavior, and it will become ever more important to involve the public and patients to devise strategies to overcome this growing health burden. The wider use of gums that promote salivary release or neutralized the mouth pH is also explored and would help toward building sufficient sacrificial amorphous enamel layer. The development of smart restorative materials has made tremendous progress in the field of dentistry, but their translation to market is slower than in medicine, maybe due to the reticence of dental practitioners to adopt these novel materials. It is likely that in the next few years, new generation of restorative materials will become accessible that will make traditional mechanical drilling redundant. The challenge for bone remains to find long-term solution to conditions associated with persistent bone loss such as osteoporosis. Research in this area is still very active, but it has yet to find a sustainable approach to reverse the slow resorption of bone, which consequently may fracture and impact greatly upon the patients’ quality of life. Similarly, the development of smart materials in dentistry, a similar approach exists for bone with the genesis of bone cements that are becoming available for repairing spinal cord injuries, for example. Unlike dentistry, the causative effects of bone demineralization are not patients’ behavior driven except for reduced physical activity. Coupling these strategies for earlier diagnostics of bone fragility or dental demineralization would greatly enhance patients’ recovery. Thus, research is currently being carried out across the world to offer new diagnostic tools for clinical use to help with the early detection. Few of these tools, such as Bio-Dent and dental optical coherence tomography, are currently on the market, and it will take a few more years for their acceptance by clinical colleagues. Ultimately, although scientists and/or clinicians may discover new understanding, develop new technologies, and products, it is still the responsibility of the patients to adapt their personal behaviors to minimize the risk factors associated with bone or dental surface loss.
Disclosure
The authors report no conflicts of interest in this work.
References
- GelseKPoschlEAignerTCollagens-structure, function, and biosynthesisAdv Drug Deliv Rev200355121531154614623400
- LinCDouglasWHErlandsenSLScanning electron microscopy of type I collagen at the dentin-enamel junction of human teethJ Histochem Cytochem19934133813888429200
- NanciATen Cate’s Oral Histology: Development, Structure, and FunctionMaryland Heights, MOMosby2008
- Vallet-RegíMGonzález-CalbetJMCalcium phosphates as substitution of bone tissuesProg Solid State Chem2004321–2131
- BeniashEBiominerals-hierarchical nanocomposites: the example of bone wiresNanomed Nanobiotechnol2011314769
- BoskeyAYoungMKiltsTVerdelisKVariation in mineral properties in normal and mutant bones and teethCells Tissues Organs20051813–414415316612080
- DuailibiMTDuailibiSEYoungCSBartlettJDVacantiJPYelickPCBioengineered teeth from cultured rat tooth bud cellsJ Dent Res200483752352815218040
- HerringSWOchareonPBone – special problems of the craniofacial regionOrthod Craniofac Res20058317418216022719
- NudelmanFPieterseKGeorgeAThe role of collagen in bone apatite formation in the presence of hydroxyapatite nucleation inhibitorsNat Mater20109121004100920972429
- DorozhkinSEppleMBiological and medical significance of calcium phosphatesAngew Chem Int Ed Engl200241173130314612207375
- HartSHartTDisorders of human dentinCells Tissues Organs20071861707717627120
- SasagawaIFine structure of the cap enameloid and of the dental epithelial cells during enameloid mineralisation and early maturation stages in the tilapia, a teleostJ Anat1997190Pt 45896009183681
- FelszeghySHollóKMódisLLammiMType X collagen in human enamel development: a possible role in mineralizationActa Odontol Scand200058417117611045371
- RobinsonCConnellSKirkhamJBrookesSShoreRSmithMThe effect of fluoride on the developing toothCaries Res200438326827615153700
- EastoeJEnamel protein chemistry – past present and futureJ Dent Res197958Spec Issue B753764368095
- WeidmannSEyreDAmino acid composition of enamel protein in the fully developed human toothCaries Res1967143493555241874
- BarronMMcDonnellSMackieIDixonMHereditary dentine disorders: dentinogenesis imperfecta and dentine dysplasiaOrphanet J Rare Dis200833119021896
- ZhengXHuJChenYZhuYChenHAFM study of the effects of collagenase and its inhibitors on dentine collagen fibrilsJ Dent201240216317122198196
- LandisWJSongMJLeithAMcEwenLMcEwenBFMineral and organic matrix interaction in normally calcifying tendon visualized in 3 dimensions by high-voltage electron-microscopic tomography and graphic image-reconstructionJ Struct Biol1993110139548494671
- Abou NeelEABozecLKnowlesJCCollagen – emerging collagen based therapies hit the patientAdv Drug Deliv Rev201365442945622960357
- BirkDSilverFCollagen fibrillogenesis in vitro: comparison of type I, II and IIArch Biochem Biophys198423511781856437334
- MartinezEda SilvaLFuruseCde AraújoNde AraújoVDentin matrix protein 1 (DMP1) expression in developing human teethBraz Dent J200920536536920126903
- GoldbergMKulkarniABYoungMBoskeyADentin: structure, composition and mineralization: the role of dentin ECM in dentin formation and mineralizationFront Biosci (Elite Ed)2011371173521196346
- BevelanderGNakaharaHThe formation and mineralization of dentinAnat Rec20051563303324
- KerebelBDaculsiGKerebelLUltrastructural studies of enamel crystallitesJ Dent Res197958Spec Issue B844851283126
- MeckelAGriebsteinWNealRStructure of mature human dental enamel as observed by electron microscopyArch Oral Biol19651057757835226910
- BartlettJDDental enamel development: proteinases and their enamel matrix substratesISRN Dent2013201368460724159389
- OrgelJSan AntonioJAntipovaOMolecular and structural mapping of collagen fibril interactionsConnect Tiss Res2011521217
- RobinsonRWatsonMCollagen-crystal relationships in bone as seen in the electron microscopeAnat Rec1952114338340912996880
- NudelmanFLauschASommerdijkASoneEIn vitro models of collagen biomineralizationJ Struct Biol2013183225826923597833
- OlsztaMJChengXJeeSSBone structure and formation: a new perspectiveMater Sci Eng R20075877116
- SilverFLandisWDeposition of apatite in collagenous extracellular matrices: identification of possible nucleation sites on type I collagenConn Tis Res2011523242252
- WangYAzaïsTRobinMThe predominant role of collagen in the nucleation, growth, structure and orientation of bone apatiteNat Mater201211872473322751179
- LandisWJacquetRAssociation of calcium and phosphate ions with collagen in the mineralization of veterbrate tissuesCalcif Tis Int2013934329337
- VeisADorveeJBiomineralization mechanisms: a new paradigm for crystal nucleation in organic matricesCalcif Tissue Int201393430731523241924
- UrryDOn the molecular basis for vascular calcificationPerspect Biol Med197418168844471706
- WestenfeldRSchaferCKrugerTFetuin-A protects against atherosclerotic calcification in CKDJ Am Soc Nephrol20092061264127419389852
- BeniashEMetzlerRLamRGilbertPTransient amorphous calcium phosphate in forming enamelJ Struct Biol2009166213314319217943
- ReyCCombesCDrouetCGlimcherMBone mineral: update on chemical composition and structureOsteoporos Int20092061013102119340505
- DeyABomansPMullerFThe role of prenucleation clusters in surface-induced calcium phosphate crystallizationNat Mater20109121010101421076415
- PougetEBomansPGoosJFrederikPMde WithGSommerdijkNThe initial stages of template-controlled CaCO3 formation revealed by cryo-TEMScience200932359201455145819286549
- HunterGHauschkaPPooleARosenbergLGoldbergHNucleation and inhibition of hydroxyapatite formation by mineralized tissue proteinsBiochem J1996317Pt 159648694787
- QiuSWierzbickiAOrmeCMolecular modulation of calcium oxalate crystallization by osteopontin and citrateProc Natl Acad Sci U S A200410171811181514766970
- MurshedMMcKeeMMolecular determinants of extracellular matrix mineralization in bone and blood vesselsCurr Opin Nephrol Hypertens201019435936520489614
- HessleLJohnsonKAndersonHTissue-nonspecific alkaline phosphatase and plasma cell membrane glycoprotein-1 are central antagonistic regulators of bone mineralizationProc Natl Acad Sci U S A200299149445944912082181
- AllistonTBiological regulation of bone qualityCurr Osteoporos Rep201412336637524894149
- HoAJohnsonMKingsleyDRole of the mouse ank gene in control of tissue calcification and arthritisScience2000289547726527010894769
- BonnucciEFine structure of early cartilage calcificationJ Ultra Res19672013350
- AndersonHMatsuzawaTSajderaSAliSMembranous particles in calcifying cartilage matrixTrans N Y Acad Sci19703256196305291227
- OrimoHThe mechanism of mineralization and the role of alkaline phosphatase in health and diseaseJ Nippon Med Sch201077141220154452
- AddisonWAzariFSorensonEKaartinenMMcKeeMPyrophosphate inhibits mineralization of osteoblast cultures by binding to mineral, upregulating osteopontin and inhibiting alkaline phosphatase activityJ Biol Chem200728221158721588317383965
- MahamidJSharirAGurDZelzerEAddadiLBone mineralization proceeds through intracellular calcium phosphate loaded vesicles: a cryo electron microscopy studyJ Strut Biol20111743527535
- MaJJohnsRStaffordRAmericans are not meeting current calcium recommendationsAm J Clin Nutr20078551361136617490974
- CurreyJThe mechanical consequences of variation in the mineral content of boneJ Biomech19692111116335107
- Almeida e SilveJSBaratieriLAraujoEWidmerNDental erosion: understanding this pervasive conditionJ Esthet Restor Dent201123420521621806751
- BralyADarnellLMannATeafordMWeihsTThe effect of prism orientation on the indentation testing of human molar enamelArch Oral Biol200752985686017449008
- WiegandAAttinTOccupational dental erosion from exposure to acids – a reviewOccup Med (Lond)200757316917617307767
- LeGerosRCalcium phosphates in enamel, dentine and boneMyresHCalcium Phosphates in Oral Biology15th edBaselKarger1991108129
- RenYFDental erosion: etiology, diagnosis and preventionDental Hygenist20117584
- FeatherstoneJDLussiAUnderstanding the chemistry of dental erosionMonogr Oral Sci200620667616687885
- LeventouriTAntonakosAKyriacouAVenturelliRLiarokapisEPerdikatsisVCrystal structure studies of human dental apatite as a function of ageInt J Biomater2009200969854720130802
- HaraAZeroDThe caries environment: saliva, pellicle, diet, and hard tissue ultrastructureDent Clin North Am201054345546720630189
- CumminsDThe development and validation of a new technology, based upon 1.5% arginine, an insoluble calcium compound and fluoride, for everyday use in the prevention and treatment of dental cariesJ Dent2013412S1S1123985433
- Higham S [webpage on the Internet]Caries Process and Prevention Strategies: Demineralization/Remineralization Available from: http://www.dentalcare.com/media/en-US/education/ce372/ce372.pdfAccessed June 23, 2016
- JiWYangFMaJBiomaterials Incorporation of stromal cell-derived factor-1 a in PCL/gelatin electrospun membranes for guided bone regenerationBiomaterials201334373574523117215
- ShepherdTJDirksWManmeeCReconstructing the life-time lead exposure in children using dentine in deciduous teethSci Total Environ201242521422222475218
- VanderbyRProvenzanoPPCollagen in connective tissue: from tendon to boneJ Biomech200336101523152714499301
- BurrDBAnatomy and physiology of the mineralized tissues: role in the pathogenesis of osteoarthrosisOsteoarthr Cartil200412A2030
- ScaramucciTCarvalhoJCHaraATZeroDTCauses of Dental Erosion: Extrinsic FactorsBerlinSpringer International Publishing20156996
- BarbourMEFinkeMParkerDMHughesJAAllenGCAddyMThe relationship between enamel softening and erosion caused by soft drinks at a range of temperaturesJ Dent200634320721316112333
- MeredithNSherriffMSetchellDJSwansonSAMeasurement of the microhardness and young’s modulus of human enamel and dentine using an indentation techniqueArch Oral Biol19964165395458937644
- KwangSAbbottPThe presence and distribution of bacteria in dentinal tubules of root filled teethInt Endod J201447660061024111689
- ScaramucciTCarvalhoJCHaraATZeroDTCauses of Dental Erosion: Intrinsic FactorsBerlinSpringer International Publishing20153567
- LussiAJaeggiTErosion – diagnosis and risk factorsClin Oral Investig200812S1513
- YouravongNTeanpaisanRNorénJGChemical composition of enamel and dentine in primary teeth in children from Thailand exposed to leadSci Total Environ20083892–325325817910978
- WheaterPBurkittHDanielsVFunctional Histology: A Text and Colour AtlasBaltimore, MDUrban & Schwarzenberg1987
- TahmassebiJFDuggalMSMalik-KotruGCurzonMEJSoft drinks and dental health: a review of the current literatureJ Dent200634121116157439
- HooperSMNewcombeRGFallerREversoleSAddyMWestNXThe protective effects of toothpaste against erosion by orange juice: studies in situ and in vitroJ Dent200735647648117329006
- LussiAJaeggiTSchaffnerMDiet and dental erosionNutr Oral Health2002182780781
- JohanssonKSorvariRBirkhedDMeurmanJHDental erosion in deciduous teeth – an in vivo and in vitro studyJ Dent200129533334011472805
- LowIMAlhuthaliAIn-situ monitoring of dental erosion in tooth enamel when exposed to soft drinksMater Sci Eng C200828813221325
- NunnJGordonPMorrisAPineCWalkerADental erosion – changing prevalence? A review of British National childrens’ surveysInt J Paediatr Dent20031329810512605627
- DalyBNewtonTJFaresJDental tooth surface loss and quality of life in university studentsPrim Dent Care2011181313521214977
- Department of Health [UK]National Children’s Dental Health Survey2003 Available from: http://www.dh.gov.uk/en/Publicationsandstatistics/Bulletins/Chiefdentalofficersbulletin/Browsable/DH_4860753Accessed July 22, 2016
- RCS [webpage on the Internet]State of Children’s Oral Health in England2015 Available from: https://www.rcseng.ac.uk/fds/policy/documents/fds-report-on-the-state-of-childrens-oral-healthAccessed June 23, 2016
- O’SullivanEMilosevicADiagnosis, prevention and management of dental erosionR Coll Surg200714117 Available from: https://www.rcseng.ac.uk/fds/publications-clinical-guidelines/clinical_guidelines/documents/erosion_guideline.pdfAccessed July 22, 2016
- TajiSSeowWKA literature review of dental erosion in childrenAust Dent J201055435836721133936
- MannCRanjitkarSLekkasDThree-dimensional profilometric assessment of early enamel erosion simulating gastric regurgitationJ Dent201442111411142124995810
- OkunseriCWongMCYauDTMcGrathCSzaboAThe relationship between consumption of beverages and tooth wear among adults in the United StatesJ Public Health Dent201575427428125919191
- ZhangJDuYWeiZTaiBJiangHDuMThe prevalence and risk indicators of tooth wear in 12- and 15-year-old adolescents in Central ChinaBMC Oral Health201515112026453049
- KannanAAdil AhmedMADuraisamyPManipalSAdusumil-lilPDental hard tissue erosion rates and soft drinks – a gender based analysis in Chennai city, IndiaSaudi J Dental Res2014512127
- KitasakoYSasakiYTakagakiTSadrATagamiJAge-specific prevalence of erosive tooth wear by acidic diet and gastroesophageal reflux in JapanJ Dent201543441842325684603
- ShellisRPFinkeMEisenburgerMParkerDMAddyMRelationship between enamel erosion and liquid flow rateEur J Oral Sci2005113323223815953248
- KargulBTanbogaIErgeneliSKarakocFDagliEInhaler medicament effects on saliva and plaque pH in asthmatic childrenJ Paedatric Dent1198222137140
- SivasithamparamKYoungWGJirattanasopaVDental erosion in asthma: a case-control study from south east QueenslandAust Dent J200247429830312587764
- MeurmanJHten CateJPathogenesis and modifying factors of dental erosionEur J Oral Sci1996104Pt 21992068804887
- Fenoglio-PreiserCMNoffsingerAEStemmermannNLantzPListromMThe non-neoplastic esophagusFenoglio-PreiserCMGastrointestinal Pathology: An Atlas and TextPhiladelphiaLippincott-Raven19993191
- CaufieldPWGriffenALDental caries. An infectious and transmissible diseasePediatr Clin North Am20044751001101911059347
- DouglassJDouglassASlikHA practical guide to infant oral healthAm Fam Physician200470112113212015606059
- TantbirojnDHuangAEricsonMDPoolthongSChange in surface hardness of enamel by a cola drink and a CPP-ACP pasteJ Dent2008361747918045766
- ZhengJXiaoFZhengLQianLMZhouZRErosion behaviors of human tooth enamel at different depthTribol Int201043712621267
- HabelitzSMaterials engineering by ameloblastsJ Dent Res201594675976725800708
- RiosDHonórioHMFrancisconiLFMagalhãesACde Andrade Moreira MachadoMABuzalafMARIn situ effect of an erosive challenge on different restorative materials and on enamel adjacent to these materialsJ Dent200836215215718191012
- ReginaGAlmeidaCDSousaCDScience of the total environment lead contents in the surface enamel of primary and permanent teeth, whole blood, serum, and saliva of 6- to 8-year-old childrenSci Total Environ2011409101799180521353293
- HardieJThe microbiology of dental cariesDent Update1982941992086959931
- NurelhudaNMAl-HaroniMTrovikTBakkenVCaries experience and quantification of Streptococcus mutans and Streptococcus sobrinus in saliva of Sudanese schoolchildrenCaries Res201044440240720714152
- LoescheWJNutrition and dental decay in infantsAm J Clin Nutr19854124234353918434
- LussiAVon Salis-MarincekMGanssCHellwigECheaibZJaeggiTClinical study monitoring the pH on tooth surfaces in patients with and without erosionCaries Res201246650751222813943
- ZhengJHuangHShiMYZhengLQianLMZhouZRIn vitro study on the wear behaviour of human tooth enamel in citric acid solutionWear20112719–1023132321
- RytomaaIJarvinenVKanervaRHeinonenOPBulimia and tooth erosionActa Odontol Scand199856136409537733
- HillRGGillamDGChenXThe ability of a nano hydroxyapatite toothpaste and oral rinse containing fluoride to protect enamel during an acid challenge using 19 F solid state NMR spectroscopyMater Lett20151566971
- LussiAMegertBPeter ShellisRWangXAnalysis of the erosive effect of different dietary substances and medicationsBr J Nutr20121070225226221733310
- Torres-GallegosIZavala-AlonsoVPatiño-MarínNMartinez-CastañonGAAnusaviceKLoyola-RodríguezJPEnamel roughness and depth profile after phosphoric acid etching of healthy and fluorotic enamelAust Dent J201257215115622624754
- CairnsMWatsonMCreanorSLFoyeRHThe pH and titratable acidity of a range of diluting drinks and their potential effect on dental erosionJ Dent2002307–831331712554112
- SadlerGDMurphyPApH and Titratable AcidityNew York, NYSpringer Science2010
- SinghSJindalREvaluating the buffering capacity of various soft drinks, fruit juices and teaJ Conserv Dent201013312913121116386
- BarbourMEShellisRPAn investigation using atomic force microscopy nanoindentation of dental enamel demineralization as a function of undissociated acid concentration and differential buffer capacityPhys Med Biol200752489991017264360
- BenjakulPChuenarromCAssociation of dental enamel loss with the pH and titratable acidity of beveragesJ Dent Sci201163129133
- PerrinDDBuffers of low ionic strength for spectrophotometric pK determinationsAust J Chem1963164572578
- AttinTBeckerKWiegandATaubockTTWegehauptFJTauböckTTImpact of laminar flow velocity of different acids on enamel calcium lossClin Oral Investig2013172595600
- ShellisRPDibdinGHAnalysis of the buffering systems in dental plaqueJ Dent Res198867243844611039053
- FinkeMHughesJParkerDMJandtKDMechanical properties of in situ demineralised human enamel measured by AFM nanoindentationSurf Sci20014913456467
- WestNXHughesJAddyMThe effect of pH on the erosion of dentine and enamel by dietary acids in vitroJ Oral Rehabil200128986086411580825
- Abou NeelEABozecLPerezRAKimH-WKnowlesJCNanotechnology in dentistry: prevention, diagnosis, and therapyIntell Surf20151063716394
- DowdFSaliva and dental cariesDent Clin North Am199943457959710553245
- KleinbergIA new saliva-based anti-caries compositionDent Today19991829810310765818
- JensenOGabrePSköldUMBirkhedDIs the use of fluoride toothpaste optimal? Knowledge, attitudes and behaviour concerning fluoride toothpaste and toothbrushing in different age groups in SwedenCommunity Dent Oral Epidemiol201240217518422211763
- KoulouridesTRemineralization methodsAnn N Y Acad Sci196815384101
- BertassoniLEMarshallGSwainMVMechanical heterogeneity of dentin at different length scales as determined by AFM phase contrastMicron201243121364137122575216
- JensdottirTBardowAHolbrookPProperties and modification of soft drinks in relation to their erosive potential in vitroJ Dent200533756957516005796
- ReynoldsECaiFCochraneNFluoride and casein phosphopeptide–amorphous calcium phosphateJ Dent Res200887434434818362316
- ReynoldsECCaiFShenPWalkerGDRetention in plaque and remineralization of enamel lesions by various forms of calcium in a mouthrinse or sugar-free chewing gumJ Dent Res200382320621112598550
- KarlinseyRLMackeyACWalkerERFrederickKESurfactant-modified beta-TCP: structure, properties, and in vitro remineralization of subsurface enamel lesionsJ Mater Sci Mater Med20102172009202020364363
- KarlinseyRPfarrerAFluoride plus functionalized b-TCP: a promising combination for robust remineralizationAdv Dent Res2012242485222899679
- ten CateJCumminsDFluoride toothpaste containing 1.5% arginine and insoluble calcium as a new standard of care in caries preventionJ Clin Dent2013243798724660269
- ZhengXChengXWangLCombinatorial effects of arginine and fluoride on oral bacteriaJ Dent Res201594234435325477312
- TwetmanSAre we ready for caries prevention through bacteriotherapy?Braz Oral Res201226Suppl 1647023318746
- WuCCLinCTWuCYPengWSLeeMJYCTInhibitory effect of Lactobacillus salivarius on Streptococcus mutans biofilm formationMol Oral Microbiol2015301162624961744
- KellerMNøhrLKarlssonITwetmanSEffect of tablets containing probiotic bacteria (Lactobacillus reuteri) on early caries lesions in adolescents: a pilot studyBenef Microbes20145440340724889893
- LeeSKimYA comparative study of the effect of probiotics on cariogenic biofilm model for preventing dental cariesArch Microbiol2014196860160924919536
- HaukiojaAProbiotics and oral healthEur J Dent20104334835520613927
- SchwendickeFHorbKKneistSDörferCParisSEffects of heat-inactivated Bifidobacterium BB12 on cariogenicity of Streptococcus mutans in vitroArch Oral Biol201459121384139025214308
- SahaSTomaro-DuchesneauCRodesLMalhotraMTabrizianMPrakashSInvestigation of probiotic bacteria as dental caries and periodontal disease biotherapeuticsBenef Microbes20145444746025006013
- CildirSGermecDSandalliNReduction of salivary mutans streptococci in orthodontic patients during daily consumption of yoghurt containing probiotic bacteriaEur J Orthod200931440741119193706
- AhmedADachangWLeiZJianjunLJuanjuanQYiXEffect of Lactobacillus species on Streptococcus mutans biofilm formationPak J Pharm Sci2014275 Spec1523152825176247
- ChinnappaAKondeHKondeSRajSBeenaJPProbiotics for future caries control: a short-term clinical studyIndian J Dent Res201324554754924355952
- SahaSTomaro-DuchesneauCDaoudJTTabrizianMPrakashSNovel probiotic dissolvable carboxymethyl cellulose films as oral health biotherapeutics: in vitro preparation and characterizationExpert Opin Drug Deliv201310111471148223713443
- NishiharaTSuzukiNYonedaMHirofujiTEffects of Lactobacillus salivarius-containing tablets on caries risk factors: a randomized open-label clinical trialBMC Oral Health20141411025178882
- CannonMTrentBVorachekAKramerSEsterlyREffectiveness of CRT at measuring the salivary level of bacteria in caries prone children with probiotic therapyJ Clin Pediatr Dent2013381556024579284
- HillmanJMoJMcDonellECvitkovitchDHillmanCModification of an effector strain for replacement therapy of dental caries to enable clinical safety trialsJ Appl Microbiol200710251209121917448156
- Stock M [webpage on the Internet]Dental Device Promises Pain-Free Tooth Repair2015 Available from: http://www.reuters.com/article/us-dental-device-idUSKCN0QU21C20150825Accessed June 23, 2016
- FerracaneJLResin composite – state of the artDent Mater2011271293821093034
- SkrticDAntonucciJMMcDonoughWGLiuDWEffect of chemical structure and composition of the resin phase on mechanical strength and vinyl conversion of amorphous calcium phosphate-based compositesJ Biomed Mater Res A200468A476377214986331
- SkrticDAntonucciJMEanesEDAmorphous calcium phosphate-based bioactive polymeric composites for mineralised tissue regenerationJ Res Natl Inst Stand Technol200310816718227413603
- SkrticDAntonucciJMEanesEDEichmillerFCSchumacherGEPhysicochemical evaluation of bioactive polymeric composites based on hybrid amorphous calcium phosphatesJ Biomed Mater Res200053438139110898879
- SkrticDAntonucciJMEanesEDBrunworthRTSilica- and zirconia-hybridized amorphous calcium phosphate: effect on transformation to hydroxyapatiteJ Biomed Mater Res200259459760411774320
- ZhaoJLiuYSunWBZhangHAmorphous calcium phosphate and its application in dentistryChem Cent J2011514021740535
- LanghorstSEO’DonnellJNRSkrticDIn vitro remineralization of enamel by polymeric amorphous calcium phosphate composite: quantitative microradiographic studyDent Mater200925788489119215975
- WeirMDChowLCXuHHKRemineralization of demineralized enamel via calcium phosphate nanocompositeJ Dent Res2012911097998422933607
- MeloMASChengLZhangKWeirMDRodriguesLKAXuHHKNovel dental adhesives containing nanoparticles of silver and amorphous calcium phosphateDent Mater201329219921023138046
- O’DonnellJNRAntonucciJMSkrticDAmorphous calcium phosphate composites with improved mechanical propertiesJ Bioact Compat Polym200621316918418688290
- ReynoldsECCalcium phosphate – based remineralization systems: scientific evidence?Aust Dent J200853326827318782374
- SchumacherGEAntonucciJMO’DonnellJNRSkrticDThe use of amorphous calcium phosphate composites as bioactive basing materials: their effect on the strength of the composite/adhesive/dentin bondJ Am Dent Assoc2007138111476148417974645
- CombesCReyCAmorphous calcium phosphates: synthesis, properties and uses in biomaterialsActa Biomater2010693362337820167295
- LeeSYRegnaultWFAntonucciJMSkrticDEffect of particle size of an amorphous calcium phosphate filler on the mechanical strength and ion release of polymeric compositesJ Biomed Mater Res B Appl Biomater2007801111716649181
- SkrticDAntonucciJMLiuDWEthoxylated bisphenol dimethacrylate-based amorphous calcium phosphate compositesActa Biomater200621859416701862
- AntonucciJMSkrticDFine-tuning of polymeric resins and their interfaces with amorphous calcium phosphate. A strategy for designing effective remineralizing dental compositesPolymers (Basel)20102437839221283507
- XuHHKMoreauJLSunLChowLCNanocomposite containing amorphous calcium phosphate nanoparticles for caries inhibitionDent Mater201127876276921514655
- ArcísRWLópez-MacipeAToledanoMMechanical properties of visible light-cured resins reinforced with hydroxyapatite for dental restorationDent Mater2002181495711740964
- DomingoCArcísRWOsorioEHydrolytic stability of experimental hydroxyapatite-filled dental composite materialsDent Mater200319647848612837395
- SantosCLuklinskaZBClarkeRLDavyKWMHydroxyapatite as a filler for dental composite materials: mechanical properties and in vitro bioactivity of compositesJ Mater Sci Mater Med200112756557315348248
- DomingoCArcísRWLópez-MacipeADental composites reinforced with hydroxyapatite: mechanical behavior and absorption/elution characteristicsJ Biomed Mater Res200156229730511340602
- LiuFWangRChengYJiangXZhangQZhuMPolymer grafted hydroxyapatite whisker as a filler for dental composite resin with enhanced physical and mechanical propertiesMater Sci Eng C Mater Biol Appl20133384994500024094216
- ZhangHDarvellBWMechanical properties of hydroxyapatite whisker-reinforced bis-GMA-based resin compositesDent Mater201228882483022578662
- SantosCClarkeRLBradenMGuitianFDavyKWMWater absorption characteristics of dental composites incorporating hydroxyapatite fillerBiomaterials20022381897190411950060
- ChenLYuQWangYLiHBisGMA/TEGDMA dental composite containing high aspect-ratio hydroxyapatite nanofibersDent Mater201127111187119521937098
- XuHHKWeirMDSunLCalcium and phosphate ion releasing composite: effect of pH on release and mechanical propertiesDent Mater200925453554219101026
- ChengLWeirMDLimkangwalmongkolPTetracalcium phosphate composite containing quaternary ammonium dimethacrylate with antibacterial propertiesJ Biomed Mater Res B Appl Biomater2012100372673422190356
- XuHHKWeirMDSunLTakagiSChowLCEffects of calcium phosphate nanoparticles on Ca-PO4 compositeJ Dent Res200786437838317384036
- XuHHKWeirMDSunLStrong nanocomposites with Ca, PO4, and F release for caries inhibitionJ Dent Res2010891192819948941
- XuHHKWeirMDSunLNanocomposites with Ca and PO4 release: effects of reinforcement, dicalcium phosphate particle size and silanizationDent Mater200723121482149117339048
- MehdawiIPrattenJSprattDAKnowlesJCYoungAMHigh strength re-mineralizing, antibacterial dental composites with reactive calcium phosphatesDent Mater201329447348423434447
- AljaboAXiaWLiaqatSConversion, shrinkage, water sorption, flexural strength and modulus of reactive calcium phosphate-containing dental compositesDent Mater201531111279128926361809
- AljaboAAbou NeelEAKnowlesJCYoungAMDevelopment of dental composites with reactive fillers that promote precipitation of antibacterial-hydroxyapatite layersMater Sci Eng C Mater Biol Appl20166028529226706532
- YounWGKhanFSites of dental erosion are saliva-dependentJ Oral Rehabil2002291354311844030
- BoivinGMeunierPChanges in bone remodeling rate influence the degree of mineralization of boneConnect Tissue Res2002432–353553712489211
- SarvrajSKVirinderSKRole of RANKL–RANK/osteoprotegerin molecular complex in bone remodeling and its immunopathologic implicationsIndian J Endocrinol Metab201115317518121897893
- MeunierPBoivinGBone mineral density reflects bone mass but also the degree of mineralization of bone: therapeutic implicationsBone19972153733779356729
- RoschgerPPaschalisEFratzlPKlaushoferKBone mineralization density distribution in health and diseaseBone200842345646618096457
- BonfieldWClarkEElastic deformation of compact boneJ Mater Sci197381115901594
- BoydeATraversRGlorieuxFJonesSThe mineralization density of iliac crest bone from children with osteogenesis imperfectaCalcif Tissue Int199964318519010024373
- WeberMRoschgerPFratzl-ZelmanNSchöberlTRauchFGlorieuxFPamidronate does not adversely affect bone intrinsic material properties in children with osteogenesis imperfectBone200639361662216644299
- RoschgerSMisofBMannVAssociation of COL1A1Sp1 alleles are associated with defective bone mineralization in vivo and in vitroCalcif Tissue Int200477211311815895281
- RoschgerPGuptaHBerzlanovichAConstant mineralization density distribution in cancellous human boneBone200332331632312667560
- HaasMLeko-MohrZRoschgerPKletzmayrJSchwarzCMitterbauerCZoledronic acid to prevent bone loss in the first six months after renal transplantationKidney Int20036331130113612631097
- BodingbauerMWekerleTPakrahBProphylactic bisphosphonate treatment prevents bone fractures after liver transplantationAm J Transplant2007771763176917511759
- Fratzl-ZelmanNValentaARoschgerPNaderAGelbBFratzlPDecreased bone turnover and deterioration of bone structure in two cases of pycnodysostosisJ Clin Endocrinol Metab20048941538154715070910
- ImelEEckertGModiAProportion of osteoporotic women remaining at risk for fracture despite adherence to oral bisphosphonatesBone20168326727526657827
- AudreyNJean-YvesRBone-forming agents in the management of osteoporosisBest Pract Res Clin Endocrinol Metab200822586988319028361
- ModiASirisESTangJSajjanSSenSSGastrointestinal events and association with initiation of treatment for osteoporosisClinicoecon Outcomes Res2015760361326648746
- FaviaGTempestaALimongelliLCrincoliVMaioranoEMedication-related osteonecrosis of the jaw after once-a-year intravenous zoledronic acid infusion for osteoporosis: report of eight casesQuintessence Int201647543344026665262
- DebSAiyathuraiLRoetherJALuklinskaZBDevelopment of high-viscosity, two-paste bioactive bone cementsBiomaterials200526173713371815621261
- Wagoner JohnsonAJHerschlerBAA review of the mechanical behavior of CaP and CaP/polymer composites for applications in bone replacement and repairActa Biomater201171163020655397
- KobayashiMNakamuraTOkadaYBioactive bone cement: comparison of apatite and wollastonite containing glass-ceramic, hydroxyapatite, and beta-tricalcium phosphate fillers on bone-bonding strengthJ Biomed Mater Res19984222232379773818
- TamuraJKawanabeKKobayashiMMechanical and biological properties of two types of bioactive bone cements containing MgO-CaO-SiO2-P2O5-CaF2 glass and glass-ceramic powderJ Biomed Mater Res199630185948788109
- RoederRKConverseGLKaneRJYueWHydroxyapatite-reinforced polymer biocomposites for synthetic bone substitutesJ Min Metals Mater Soc20086033845
- NiGXChiuKYLuWWStrontium-containing hydroxyapatite bioactive bone cement in revision hip arthroplastyBiomaterials200627244348435516647752
- ItokawaHHiraideTMoriyaMA 12 month in vivo study on the response of bone to a hydroxyapatite-polymethyl-methacrylate cranioplasty compositeBiomaterials200728334922492717707904
- GotoKShinzatoSFujibayashiSThe biocompatibility and osteoconductivity of a cement containing beta-TCP for use in vertebroplastyJ Biomed Mater Res A200678362963716788976
- KobayashiMNakamuraTTamuraJKokuboTKikutaniTBioactive bone cement: comparison of AW-GC filler with hydroxyapatite and beta-TCP fillers on mechanical and biological propertiesJ Biomed Mater Res19973733013139368135
- CamaGCalcium Phosphate Cements for Bone Regeneration. Biomaterials for Bone RegenerationSawstonWoodhead Publishing Limited2014325
- CamaGGharibiBSaitMA novel method of forming micro- and macroporous monetite cementsJ Mater Chem201317958969
- VereeckeGJacquesLCalculation of the solubility diagrams in the system Ca (OH)2-H3PO4-KOH-HNO3-CO2-H2OJ Cryst Growth19901044820832
- FernándezEGilFGinebraMDriessenFPlanellJBestSCalcium phosphate bone cement for clinical application. Part II: precipitate formation during setting reactionsJ Mater Sci Mater Med199910317718315348166
- ZhangJLiuWSchnitzlerVTancretFBoulerJCalcium phosphate cements for bone substitution: chemistry, handling and mechanical propertiesActa Biomater20141031035104924231047
- MoroniLde WijnJRvan BlitterswijkCAIntegrating novel technologies to fabricate smart scaffoldsJ Biomater Sci Polym Ed200819554357218419938
- MarinoAFilippeschiCGenchiGGMattoliVMazzolaiBCiofaniGThe Osteoprint: a bioinspired two-photon polymerized 3-D structure for the enhancement of bone-like cell differentiationActa Biomater201410104304431324907661
- RainerWErikWGeorgVFRudolfSDirect laser writing-mediated generation of standardized topographies for dental implant surface optimizationJ Laser Appl2012244042011
- LanZYongHEffect of nanostructured titanium on anodization growth of self-organized TiO2 nanotubesNanotechnology201021505560220023303
- BrammeraKOhdSCobbaCBjurstenbLvan der HeydecHJinSImproved bone-forming functionality on diameter-controlled TiO2 nanotube surfaceActa Biomater2009583215322319447210
- OhaSBrammeraKJulie LibYStem cell fate dictated solely by altered nanotube dimensionProc Natl Acad Sci USA200910672130213519179282
- Cavalcanti-AdamEVolbergTMicouletAKesslerHGeigerBSpatzJCell spreading and focal adhesion dynamics are regulated by spacing of integrin ligandsBiophys J20079282964297417277192
- OgawaTSaruwatariLTakeuchiKAitaHOhnoNTi nanonodular structuring for bone integration and regenerationJ Dent Res200887875175618650547
- GotoTOsseointegration and dental implantsClin Calcium201424226527124473360
- AlbrektssonTSennerbyLWennerbergAState of the art of oral implantsPeriodontol 2000200847152618412571
- MendonçaGMendonçaDAragãoFCooperLAdvancing dental implant surface technology-from micron- to nanotopographyBiomaterials200829283822383518617258
- CiofaniGRicottiLCanaleCEffects of barium titanate nanoparticles on proliferation and differentiation of rat mesenchymal stem cellsColloids Surf B Biointerfaces201310231232023006571
- SuW-TWuP-SKoC-SHuangT-YOsteogenic differentiation and mineralization of human exfoliated deciduous teeth stem cells on modified chitosan scaffoldMater Sci Eng Mater Biol Appl C201441152160
- TimothyRJoshuaRPNagehKAXinjianFCraigAGKetulCPNanostructured tantala as a template for enhanced osseointegrationNanotechnology200920404510219417310
- AminianAPardunKVolkmannEEnzyme-assisted calcium phosphate biomineralisation on an inert alumina surfaceActa Biomater20151333534325462843
- StadlingerBHintzeVBierbaumSBiological functionalization of dental implants with collagen and glycosaminoglycans – a comparative studyJ Biomed Mater Res B Appl Biomater2012100B233134122102613
- SchliephakeHScharnweberDDardMSewingAArefARoesslerSFunctionalization of dental implant surfaces using adhesion moleculesJ Biomed Mater Res B Appl Biomater200573B1889615786448
- PuleoDKisslingRSheuMA technique to immobilize bioactive proteins, including bone morphogenic protein-4 (BMP-4), on titanium alloyBiomaterials20022392079208711996050
- KapustinADaviesJReynoldsJCalcium regulates key components of vascular smooth muscle cell–derived matrix vesicles to enhance mineralizationCirc Res20151091e1e1221566214

