Abstract
Osteoporosis (OP) affects millions of people worldwide, especially postmenopausal women and the elderly. Although current available anti-OP agents can show promise in slowing down bone resorption, most are not specifically delivered to the hard tissue, causing significant toxicity. A bone-targeted nanodrug delivery system can reduce side effects and precisely deliver drug candidates to the bone. This review focuses on the progress of bone-targeted nanoparticles in OP therapy. We enumerate the existing OP medications, types of bone-targeted nanoparticles and categorize pairs of the most common bone-targeting functional groups. Finally, we summarize the potential use of bone-targeted nanoparticles in OP treatment. Ongoing research into the development of targeted ligands and nanocarriers will continue to expand the possibilities of OP-targeted therapies into clinical application.
Introduction
Osteoporosis (OP) is one of the most prevalent bone diseases characterized by a loss of bone calcium and matrix, leading to a decrease in bone density and degradation of bone tissue microstructure.Citation1,Citation2 This condition can cause lower back pain, stooped posture, height loss, and fractures. Due to the loss of bone mass, patients with OP have an increased risk for bone fragility and fracture. If left unprevented or untreated, OP can progress painlessly and cause severe wrist, hip, and spinal fractures, leading to disability and death in the elderly.Citation3,Citation4 Because bone and cartilage health are closely related, OP may affect the occurrence and development of osteoarthritis (OA). The decreased bone density and insufficient mineralization of bone trabeculae caused by OP can affect the normal structure of cartilage and subchondral bone. Therefore, treating OP is also necessary for preventing and treating OA.Citation5 As the population ages, osteoporosis is gradually becoming a serious global health problem, affecting over 200 million people worldwide, according to statistics from the International OP Foundation.Citation6 The etiology of OP is complex and involves a delicate balance between osteoblasts and osteoclasts in the body and multiple regulatory factors released by the osteocyte network that maintains bone remodeling homeostasis. The imbalance in any of these factors can lead to OP,Citation7 highlighting the need for a clear understanding of its etiology to explore effective treatment options.
Currently, two main approaches are used to treat OP in clinical practice. These include preventing bone resorption using drugs like bisphosphonates, calcitonin, denosumab, and selective estrogen receptor modulators and directly increasing bone density using parathyroid hormone (PTH).Citation8,Citation9 However, these commonly used drugs have limited efficacy and can result in inevitable toxic side effects. summarizes their mechanisms and side effects. These drugs’ limitations restrict their efficacy in the body. On the one hand, these drugs have low biocompatibility once entering the body, making them susceptible to rejection reactions and difficult to transport to bone tissues.Citation10–12 On the other hand, most drugs lack targeting specificity and can not specifically recognize bone tissues, leading to high accumulation in organs, such as the liver and kidneys, causing toxic side effects and negatively impacting their therapeutic effectiveness.Citation13,Citation14 Therefore, there is an urgent need to develop more refined and efficient treatment methods for OP.
Table 1 Characteristics and Side Effects of Various Drugs for OP Treatment
Nanotechnology is a rapidly growing research field that provides promising options for disease treatment. Currently, dozens of nanodrugs have been approved for clinical use, such as liposome-encapsulated doxorubicin (Doxil; Johnson & Johnson) for the treatment of ovarian cancer and Kaposi’s sarcoma,Citation35 while hundreds of other nanodrugs are in preclinical evaluation.Citation36 Nanomaterials are synthetic structures composed of inorganic or organic substances with at least two dimensions between 1 and 1000 nanometers.Citation36 The small size of nanoparticles (NPs) enables them to pass through biological barriers and reach ideal areas in the body, resulting in higher therapeutic efficiency. In addition, loading into nanomaterials can improve drugs’ solubility, thus greatly increasing drugs’ bioavailability.Citation37–39 By modifying NPs for drug delivery, they can be targeted to disease sites and released in specific locations.Citation40,Citation41 This approach changes drugs’ pharmacokinetic characteristics, increases their time of existence in the disease area, and extends their biological effects.Citation42 Because bone itself is a nanocomposite material, NPs have similarities with bone tissues and high surface areas and roughness, which facilitate protein and cell adsorption in bone tissue. Currently, strategies for targeting bone tissue focus on the bone surface, bone marrow and its endothelial cells. While more than 40 types of first-generation nanomaterials have been applied in clinical practice,Citation43 research on nanodrugs is still in its early stages, and future development and improvement of nanodrugs will require a massive undertaking. This review summarizes recent research progress on nanomaterials in OP treatment and mainly discusses two aspects of using nanomaterials for OP treatment: (i) various nanomaterials used for osteoporosis treatment, including liposomes, exosomes (Exos), Polymeric NPs such as poly (DL-lactide-co-glycolide) (PLGA) nanoparticles and Inorganic NPs, and (ii) exploring the potential of using various bone tissue-targeting modified nanomaterials for targeted drug delivery in OP treatment. Additionally, the potential challenges and prospects of using such nanomaterials for targeted OP treatment are also discussed.
Nanocarriers for OP
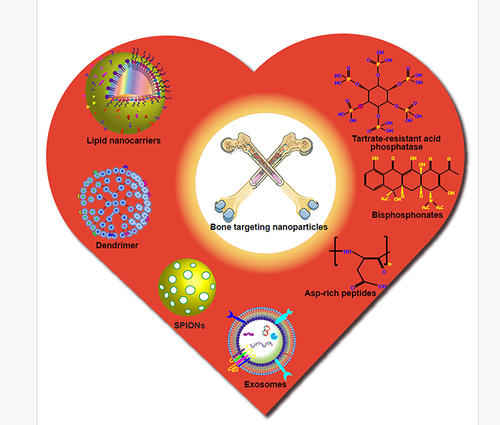
The development of nanotechnology has opened exciting possibilities for the treatment of OP, with nanomaterials severing as effective delivery vehicles for growth factors, nucleic acids, and proteins that have demonstrated therapeutic benefits.Citation44–48 Such delivery can be achieved through various methods, including oral administration, injection, or local injection. High-quality nanocarriers offer several excellent characteristics, such as (1) protecting drugs from degradation, (2) enhancing their penetration into the body, (3) targeted delivery of therapeutic substances and improved topical drug penetration and release in the affected area, and (4) excellent biocompatibility and biodegradability.Citation48 These unique properties make nanotechnology a promising player in the development of effective treatments for OP. Nanomaterials-based therapies offer several advantages in biomedical applications. Firstly, their smaller size allows for enhanced drug penetration and mobility within the body, leading to improved therapeutic outcomes. Secondly, their natural structure and good biocompatibility make them less susceptible to immune responses and degradation, leading to longer circulation time in the body. Lastly, their relative non-toxicity compared to conventional drug delivery systems can result in fewer side effects and improved patient safety. Moreover, modifying nanocarriers makes drug delivery more efficient and precise.Citation49–51 Currently, there are several types of nanocarriers employed for treating OP, including lipid carriers, Exos, and various synthetic NPs. While each of these nanocarriers has unique advantages, combining their advantages through particle modification or nanocomposite assembly is a promising direction for future research. and provides an overview of the characteristics of various nanocarriers and related research. By developing more sophisticated and effective nanocarrier systems, researchers can potentially enhance drug delivery and improve the outcomes of OP treatments.
Table 2 Various Nanocarriers and Their Applications in the Treatment of OP
Figure 1 NPs are classified into different categories according to their properties, shape or size. Each class of NPs has several subclasses, with advantages and limitations are presented here.

Lipid Nanocarriers
Lipid nanocarriers are a type of drug delivery system primarily composed of solid lipid matrices with hydrophilic and lipophilic phases, offering excellent drug-loading capacity and easy modification. They represent the second generation of lipid-based drug delivery systems, aiming to overcome the limitations of previous systems.Citation55,Citation83 Among them, liposomes are the most widely used lipid nanocarriers in clinical applications. These spherical vesicles can encapsulate hydrophilic or hydrophobic therapeutic molecules, exhibit good biocompatibility and biodegradability, and possess easily modifiable structures, improved drug solubility and pharmacokinetics, and reduced drug toxicity.Citation84–87
In 1995, the US Food and Drug Administration (FDA) approved the first clinical nanodrug for chemotherapy, Doxil®,Citation88 which is a pegylated liposome formulation of doxorubicin. The drug has proven effective in reducing the cardiotoxicity associated with doxorubicin.Citation89 Other liposome formulations subsequently approved for clinical use include Myocet™Citation90 and Marqibo®.Citation91 Extensive research has been conducted on modifying lipid nanocarriers, providing inspiration for developing lipid nanocarriers for treating OP. One interesting development is the use of liposome-based thermosensitive nanocarriers that release loaded drugs at high temperatures. ThermoDox, a lipid-based thermosensitive nanocarrier containing doxorubicin, is currently undergoing Phase II trials for the treatment of breast cancer and liver metastases and Phase III trials for the treatment of liver cancer.Citation92
For bone diseases, researchers hope to develop lipid nanocarriers targeting bone tissue. Song et alCitation93 and Ferreira et alCitation94 have respectively developed pamidronate-conjugated liposomes and alendronate salt-conjugated PEGylated liposomes and demonstrated that the former exhibited an increased affinity for bone tissue, and the latter had the bone-targeting ability. Currently, researchers are exploring the use of liposomes to treat OP. A recent study utilized modified liposomes to load antagomir-148a, a miRNA modulator that suppresses the osteoclastogenic miR-148a (a miRNA modulator suppressing the osteoclastogenic miR-148a) and found that the modified liposomes accumulated mainly in bone and downregulated miR-148a expression in osteoclasts, inhibiting bone absorption in mice with OP.Citation52 In another study on lipid nanoparticle delivery of nucleic acids, the authors used LNP delivery of siRNA to silence the GNAS gene in MSCs. Ex vivo and in vivo experiments demonstrated that this LNP-siRNA delivery system effectively silenced the GNAS gene and enhanced the potential of MSCs to differentiate into osteoblasts. This delivery strategy provides promise option for the treatment of OP.Citation53 A novel ionizable lipid with a C18 tail and ionizable head group was developed for delivery of bone morphogenetic protein-9 (BMP-9) gene for OP treatment. In this study, Ionizable LNP showed excellent delivery efficacy, and ex vivo and in vivo experiments confirmed the transfection efficiency and safety of the BMP-9 gene for the reversal of OP.Citation54
While drugs commonly used to orally treat OP have good pharmacological advantages, their gastrointestinal effects often lead to lower bioavailability and toxic side effects.Citation95 Researchers have designed a lipid nanocarrier to simultaneously carry Raloxifene (RLX) hydrochloride and Vitamin D (Vit.D), two classic drugs, to address the low bioavailability of these drugs. After testing the pharmacokinetic parameters of healthy volunteers who took the drugs orally, they found that compared to traditional commercial products, these nanolipid carriers increased the bioavailability of RLX by 385.6%, and the average level of Vit.D metabolites from 91±29 nmol/L to 174±36 nmol/L. The increased bioavailability of these drugs may be due to the lipid carriers being absorbed via the interaction of the drug and bile salts after being decomposed by enzymes in the intestine, which protects the drug from premature metabolism.Citation55 Similarly, to enhance the bioavailability of RLX hydrochloride, researchers invented a double emulsion solvent evaporation (DESE) to encapsulate RLX hydrochloride into solid lipid nanoparticles (SLNPs). This drug-loading method can encapsulate RLX hydrochloride in SLNPs with appropriate physicochemical and biological properties, which enhances the drug’s effect.Citation56 Another lipid NP is a bioadhesive nanoparticle composed of Carbopol 940, glyceryl distearate, and TGPS. This lipid nanodelivery system was able to firmly encapsulate RLX internally and demonstrated higher biological utilization in rat experiments, suggesting an excellent OP drug delivery vehicle.Citation57 Simvastatin (SIM), which has been shown to treat OP through osteoblast differentiation and mineralization, has poor bone targeting and low bioavailability for in vivo application. However, the in vivo application of SIM has poor bone targeting and low bioavailability. Therefore, LNP, which is combined with a targeting peptide, was used as a carrier to deliver SIM to the bone tissue and to enhance the bone-enhancing effect of SIM. This demonstrated that LNP is an effective carrier for the treatment of OP.Citation58
In a separate study, researchers added bile salts and cholesterol to lipids and designed a new type of lipid nanocarrier called bilosomes. They then evaluated the advantages of bilosomes carrying sodium alendronate. Compared with regular liposomes, the addition of cholesterol and bile salts improved the stability of the bilosomes, protecting them from external digestive damage and reducing the toxicity of oral drugs. This significantly enhanced the efficacy of sodium alendronate in treating OP.Citation59
Exosomes
Exos are lipid bilayer-enclosed structures with diameters ranging from 40 to 160 nm.Citation96 Scientists believe that cells use Exos to package proteins, mRNA, microRNAs (miRNAs), and lipids for intercellular communication.Citation97,Citation98 Due to their natural communication carrier properties, researchers are considering developing drug delivery systems based on Exos. In addition to the advantages of small size, structural stability, and low toxicity possessed by nanomaterials, as previously mentioned, Exos are widely available and exist in all bodily fluids and tissues.Citation97 This provides a continuous source of carriers, and delivering drugs through autologous Exos does not raise ethical issues or cause immune rejection reactions.Citation60 Another advantage of using Exos as drug carriers is their ability to exert regulatory effects. Specifically, Exos secreted by bone marrow stromal cells (BMSCs), osteoclasts, and osteoblasts have been shown to participate in bone regulation.Citation99 Exos derived from osteoclasts have bone-inhibiting effects,Citation100,Citation101 while those from BMSCs and osteoblasts can enhance bone formation.Citation102 Another key element is that Exos can be highly engineered. After engineering, Exos have cell and tissue specificity, making them better suited for drug delivery.Citation63,Citation103–109
Researchers are investigating the potential of engineered Exos carrying therapeutic molecules as a new treatment option for osteoporosis. In one study, researchers developed a delivery system based on Exos derived from human induced pluripotent stem cells (iPSCs) to combat OP. They used these MSC-derived Exos to fight against OP and modified them to target and deliver siRNA of the Shn3 gene (siShn3) to osteoblasts. This downregulated the expression of the Shn3 gene in osteoblasts, enhanced osteoblast differentiation, and decreased the expression of receptor activator of nuclear factor-κB ligand (RANKL), thereby inhibiting osteoclast formation from achieving an anti-osteoporotic effect.Citation60 Similarly, stem cell-derived exosomes were chosen as the subject by Lu et al. In their work, BMSC-derived exosomes loaded with miR-29a showed potent osteogenic capacity, suggesting the potential for therapeutic OP.Citation62 In addition, a new study selected red blood cell derived extracellular vesicles as delivery vehicles and achieved the targeting of osteoclasts with a bifunctional peptide to deliver anti-miR-214. The experimental results suggested the bone-targeting ability of the delivery vehicle, as well as the inhibition of osteoclasts and the enhancement of osteogenesis. The use of red blood cell derived extracellular vesicles as carriers for OP treatment is a promising direction.Citation63 Hu et al fused Exos with liposomes to form hybrid Exos and delivered antagomir-188 to the skeleton via C-X-C motif chemokine receptor 4 (CXCR4), which promotes BMSC osteoblastic differentiation, thus reversing the age-related loss of trabecular bone.Citation61
Superparamagnetic Iron Oxide Nanoparticles
In the 1970s, Freeman et al were the first to combine magnetism with medical applications, and since then, extensive research on magnetic NPs has been conducted.Citation110 Superparamagnetic iron oxide nanoparticles (SPIONs) have become one of the most widely studied targeted nanomaterials due to their many advantages. Firstly, SPIONs are synthesized from a single raw material and are easy to synthesize, with good chemical stability.Citation111 SPIONs also exhibit good biocompatibility and biological safety and are relatively non-toxic compared to nanoparticles containing manganese and gadolinium.Citation112,Citation113 Furthermore, SPIONs exhibit excellent superparamagnetic, allowing them to be accumulated in a designated area through an external magnetic field.Citation114 These magnetic particles lose their magnetism and scatter when the external magnetic field disappears, thus avoiding possible immune system attacks and enhancing local effects and half-life in circulation.Citation115 Currently, SPIONs have mainly been applied in two areas of clinical biomedical research. One is in magnetic resonance imaging (MRI), where SPIONs serve as contrast agents to assist in diagnosing early diseases.Citation116 The other area of interest is using SPIONs as excellent drug-target delivery vehicles, especially for tumor-targeted radiotherapy and chemotherapy.Citation117,Citation118
While acting as carriers, SPIONs also play an essential role in anti-OP. Previous in vitro studies have shown that SPIONs can promote osteoblast differentiation and inhibit osteoclast formation. In vivo experiments have demonstrated that these nanoparticles can accelerate bone defect repair and prevent bone loss.Citation111,Citation119,Citation120 These studies further illustrate the advantages of using SPIONs for the treatment of OP. SPIONs can deliver bioactive molecules (such as antibodies, proteins, drugs, etc.) or cells, which opens up more possibilities for bone regenerative medicine.Citation121
Marycz et al designed a dual-target scaffold carrier doped with SPIONs and HAP nanoparticles (nHAP) for delivering miR-21 and miR-124.Citation64 Under the action of the carrier and the magnetic field, miRNA targets accumulate and then release, increasing osteoblast activity and inhibiting osteoclast activity, enhancing the regeneration of osteoporotic bone. In another study, researchers incorporated SPIONs into silk fibroin/hydroxyapatite scaffolds and implanted BMSCs into the backs of nude mice using this scaffold. The results showed that BMSCs could adhere and grow well and promote bone formation. SPIONs not only enhance the stability of silk fibroin/hydroxyapatite scaffolds but also show a stronger bone-forming effect by incorporating magnetic particles. In addition, bone regeneration can be monitored non-invasively by MRI.Citation65
Hydroxyapatite Nanoparticles
Hydroxyapatite (HAP), with the chemical formula of Ca10(OH)2(PO4)6, has a unique structure that closely resembles bone tissue, making it a promising material for biomedical applications in bone diseases. One potential application of HAP is as a bone cement and bone graft due to its osteoconductive and injectable properties, as proposed by Ginebra et al (1999). Numerous studies have explored the use of bone cement to strengthen osteoporotic bones.Citation122–126 HAP-based bone cement offers several advantages, such as low-temperature solidification reactions and inherent porosity, which enable it to carry drugs or active ingredients for joint action.Citation127 Panzavolta et alCitation128,Citation129 have successfully combined bisphosphonates with HAP, resulting in drug-carrying bone cement with good mechanical properties. This combination of drugs and HAP has the potential to resist bone resorption, which can be beneficial in relieving osteoporosis.
Recently, researchers have synthesized HAP nanoparticles (nHAP) and combined them with various polymers to create bio composite materials with enhanced osteoconductive properties.Citation122,Citation130 These nanoscale biomaterials are crucial in orthopedic surgery as they have a small size and possess structure and chemical properties similar to natural bone, which allows them to remain stable in the acidic and alkaline environment of the body and resist degradation by enzymes. In addition, the inherent degradation products of Ca2+ and PO43- in the body are not non-toxic and do not cause immune reactions.
Researchers are hopeful that nHAP can serve as a carrier for delivering drugs and therapeutic proteins for the treatment of OP.Citation131–133 Besides its role as a drug carrier, nHAP is also expected to supplement bone defects. Dave et al synthesized nHAP carriers loaded with PTH, achieving targeted delivery of PTH to osteoporotic bones.Citation66 The nanocarriers dissolve in the osteoporotic bone, enhancing the matrix components of the bone while playing a role in PTH synthesis and metabolism locally. Furthermore, nHAP has been combined with recombinant human bone morphogenetic protein-2 (rhBMP-2) in another study. The nanocarrier carrying rhBMP-2 was implanted into rabbits’ unilateral radial bone defects, and it was found that nHAP with growth factors could stimulate more bone formation, highlighting its excellent growth factor carrier performance.Citation67 The advantages of bisphosphonates in the treatment of OP have become the focus of research by scientists. Delivery of bisphosphonates with nHAP as a carrier has a favorable anti-OP effect. In vitro experiments confirmed that nHAP could enhance the function of bisphosphonates to inhibit osteoclast formation, and the combination with hydrogel could induce mineralization, which is a new bone repair material.Citation68 Surface-stabilized nHAP prepared by aqueous precipitation was used to deliver salmon calcitonin (SCT), and the nHAP showed high loading efficiency, permeability, and stability. In an osteoporotic rat model, the nHAP delivered SCT demonstrated excellent bone repair ability and is an injectable treatment for OP.Citation69 Similarly, by loading novel zoledronic acid (ZOL) in nHAP (ZOL-nHAP) by the classical adsorption method, researchers explored the role of ZOL-nHAP in osteoporotic rats. After three months of treatment, it was found that treating OP rats with nHAP-delivered ZOL was more effective than ZOL alone. Apparently, ZOL-nHAP better reversed bone loss, better preserved trabecular structure and improved mechanical strength in the OP rat model.Citation70
In addition, researchers are keen on modifying various substances in combination with nHAP to enhance the performance of nanoparticles on the original basis. For example, zinc is a suitable combination with nHAP. For example, Risedronate (RDN), which is a high-quality osteogenic drug, was loaded onto zinc-nHAP by researchers through adsorption. Using an animal model of OP, the researchers compared the effects of zinc-nHAP delivered RDN and RDN alone for the treatment of OP. The results strongly suggest that preparations of zinc-nHAP-delivered RDN have a therapeutic advantage over administration alone, with better preservation of cortical and trabecular bone structures.Citation71
Overall, the potential applications of nHAP in orthopedic surgery are vast and promising, and ongoing research may uncover additional benefits.
PLGA Nanoparticles
Poly(DL-lactide-co-glycolide) (PLGA) is a biocompatible material that has been used as a growth factor carrier in the 1990s.Citation134 It can be easily synthesized and modified to optimize polymer degradation and drug release kinetics.Citation135 With advances in nanotechnology, PLGA NPs are being extensively investigated as drug delivery carriers.Citation136 For instance, to improve the bioavailability of hydrophobic drugs, Xi et al successfully encapsulated Astragaloside (AS) in the hydrophobic core of PLGA NPs and enabled them bone-targeting properties by conjugated PLGA nanocarrier with Alendronate (AL) sodium via polyethylene glycol.Citation72 In vivo and in vitro experiments have demonstrated the improved oral bioavailability and anti-OP effect of this nanocarrier, with the addition of AL further enhancing its bone targeting properties.
PLGA nanoparticles are also being explored as carriers for simvastatin, a drug that enhances bone formation and density but has limited use due to its hydrophobic and non-targeted nature.Citation137,Citation138 To overcome this, researchers have combined PLGA NPs with tetracycline to give the nanocarrier bone targeting properties. In vivo experiments have shown that simvastatin-loaded tetracycline-modified PLGA NPs significantly increase bone density in osteoporotic rats compared to free simvastatin and non-targeted NPs.Citation73 Similarly, using PLGA NPs as carriers, the researchers delivered estradiol to OP rats and administered the drug via iontophoresis. The results showed that the negative ions on the surface of the PLGA NPs combined with the special delivery method could enhance the concentration of estradiol in the blood and treat the OP rats more effectively.Citation74 Zhang et al loaded secretome (Sec) from MSC into PLGA NPs and endowed the carrier with bone targeting via CXCR4. In the OP rat model, they found that this NP accumulated in the bone and exhibited inhibition of osteoclast differentiation and promotion of osteoblast proliferation, which reduced bone attenuation from the surgical model.Citation75
In another study, composite nanocarriers of PLGA/HAP were implanted subcutaneously in mice to deliver BMPs, resulting in increased mouse bone formation.Citation76 The PLGA/HAP nanofiber exhibited good morphology and mechanical strength and using it as a carrier allowed BMP to be released while maintaining good biological activity in vivo.Citation139
Chitosan Nanoparticles
Chitosan, a natural polysaccharide derived from chitin found in crustaceans, insects, and fungi, is known for its hydrophilicity, biocompatibility, and biodegradability.Citation77,Citation140,Citation141 Chitosan nanoparticles (CS-NPs) have gained popularity as drug carriers due to their small size, high encapsulation efficiency, and loading capacity,Citation142–144 and ability to combine with a wide range of molecules, including plant components, nanomaterials, hormones, and proteins.Citation145,Citation146
To overcome the low bioavailability and toxic side effects of drugs commonly used in clinics, like RLX, lipid nanocarriers have been effectively used for delivery. Saini et al used CS-NPs to deliver RLX, which improved its oral bioavailability.Citation77 Similarly, PEGylated chitosan nanoparticles were used to deliver PTH, yielding similar effects.Citation78 CS-NPs were also used to deliver bisphosphonates, resulting in a significant improvement in bone density and microstructure in osteoporotic rats, while cortical porosity on bone surfaces decreased.Citation79 CS-NPs were used to load Human Parathyroid hormone 1–34 (PTH1-34), and the experimental results suggested the biocompatibility and high encapsulation efficiency of this delivery strategy. In addition, the researchers affirmed the efficiency of oral CS-NPs in delivering PTH1-34, and this strategy is a potential way to treat OP in the future.Citation80 Shilajit is a class of natural minerals whose extracts (SWE) have been shown to affect bone development. In a study, researchers utilized CS-NPs encapsulated with SWE and evaluated the efficacy of the pair combination in OP rats.The results suggested that CS-NPs encapsulated SWE could enhance the anti-OP effects of SWE.CS NPs delivered SWE could be recommended as a potential treatment for OP.Citation81
In another study, researchers sought to deliver RDN and TPD together in a targeted manner using CS-NPs as carriers, with the carrier surface modified with hyaluronic acid. This carrier, which loaded both RDN and TPD, could be stably preserved at low temperatures and exhibited stronger bone regeneration effects, indicating a promising new strategy for treating OP.Citation82
Bone-Targeted Nanoparticles for the Treatment of Osteoporosis
In clinical practice, there are several drugs available for the treatment of OP, as outlined in . However, these drugs face limitations when administered orally or intravenously, as they struggle to target specific tissues for release. Most drugs are absorbed or excreted by other organs in circulation, making it difficult to achieve the therapeutic effect.Citation147–149 Consequently, higher drug doses or more frequent administration may be required, leading to adverse reactions and organ toxicity. To overcome these limitations, targeted drug delivery strategies are required, with the combination of targeted delivery and nanotechnology offering a more effective approach. For OP, scientists need to focus on bone targeting as the primary strategy. Since the concept of “bone targeting” was first proposed in 1986 by Pierce et al,Citation150 research in this area has developed rapidly.
Bone tissue has a surface-mineralized extracellular matrix primarily that primarily consists of HAP and hosts a variety of movements, such as ion exchange, crystal growth, dissolution, and combinations of foreign molecules on the bone surface. Therefore, this mineralized component offers an option for bone targeting.Citation14,Citation151 Studies indicate that the crystal size of HAP in the bone tissue of osteoporotic patients is larger,Citation152 making targeted treatment of the bone surface with drugs more feasible.
Bone targeting strategies involve binding the target molecule to HAP in bone, enabling NPs carrying the drug to aggregate and exert their effects on bone tissue.Citation151 The surface of these NPs can also be modified with cell/tissue-targeting groups, such as bisphosphonates or osteoclast/osteoblast-targeting peptides, to enhance the biological distribution of the drug in bone tissue. Additionally, bone marrow presents itself as a potential target for bone-targeting delivery systems. illustrates the bone targeting strategy, which, when combined with nanocarrier delivery systems, can offer a more satisfactory drug treatment for OP. Understanding the bone targeting strategy is essential to develop effective targeted drug delivery systems for OP. summarizes typical examples of the targeted strategy of nanoparticles to enhance the treatment of OP.
Table 3 Targeting Group-Modified Nanoparticles Enhance the Therapeutic Potential of Drugs to Treat OP
Figure 2 Targeted ligands and their targets for the treatment of OP. Bone-targeted nano-delivery systems can be specifically delivered to bone matrix, bone marrow, osteoblasts, and osteoclasts by using various targeting ligands, including BPs, peptides, antibodies, and many other synthetic chemical molecules.

Tartrate-Resistant acid Phosphatase
Tartrate-resistant acid phosphatase (TRAP) is an acid hydrolysis enzyme mainly found in osteoclasts, making it a useful indicator for identifying these cells.Citation153,Citation154 Moreover, TRAP is secreted by osteoclasts towards the bone surface and can be detected on the bone surface and in the bone matrix,Citation155,Citation156 making it a potential therapeutic target. Wang et al designed a peptide TPLSYLKGLVTVG with a high affinity for TRAP and coupled it to the corona of a nanosphere.Citation157 They delivered a GSK-3β inhibitor to the site of bone fractures in mice, resulting in higher drug accumulation, activation of the β-catenin pathway in MSCs and osteoblasts, increased formation of bone bridges and deposition of bone mass. This targeted approach enhanced the healing ability of bone fractures. As mentioned above, a bifunctional peptide, TBPCP05, binds to the surface of EVs, causing them to display TRAP-binding peptides on the surface, and in vivo and in vitro experiments have demonstrated the ability of such EVs to target osteoclasts. This vector carrying anti-miR-214 can focus on osteoclasts and exert anti-OP effects.Citation63
Although targeting TRAP is still in its early stages of research, these successful examples provide valuable insight for future directions in using TRAP-based peptide and NP coupling for drug delivery to treat bone diseases.
Tetracycline
Tetracycline is a yellow crystalline amphipathic substance derived from the metabolism of Streptomyces rimosus, and it was first used as a broad-spectrum antibiotic in the 1940s.Citation158,Citation159 It is effective in inhibiting bacterial growth at high concentrations and plays an important role in the prevention and treatment of human and animal infections.Citation160 Shortly after tetracycline was used in medicine, an interesting phenomenon was discovered where bright yellow fluorescence could be observed under UV light in the bones of animals treated with tetracycline.Citation161 This fluorescent property of tetracycline made it a target marker carrier.Citation162 Tetracycline’s ability to deposit in bone tissue also sparked an interest. Initially, it was thought that tetracycline interacted with the organic matrix of bones, but later evidence showed that it mainly binds to HAP on the bone surface.Citation163,Citation164 Tetracycline’s bone-binding ability is a double-edged sword. On the one hand, pigmentation was observed in the teeth of young people who had taken tetracycline, which may lead to a decrease in tooth hardness and enamel damage, limiting its clinical use.Citation165 On the other hand, due to tetracycline’s high affinity for HAP, researchers began exploring its potential as an effective compound for bone targeting.
In recent years, the drug delivery strategy for OP based on the combination of tetracycline bone-targeting agents and nanocarriers has been widely studied. Que et al used TC-mPEG-PLGA to establish a bone-targeting nanodrug delivery system and loaded it with astragaloside to treat OP.Citation166 In vivo and in vitro results showed that TC-mPEG-PLGA effectively increased the accumulation of astragaloside in bone and improved bone density in ovariectomized rats compared to free astragaloside. Similarly, Wang et al used TC-PLGA NPs to load SIM to treat OP and demonstrated higher bone-targeting efficiency and improved efficacy in restoring bone density.Citation73 In addition, tetracycline can also serve as a bone-targeting agent for another type of nanocarrier. Researchers have constructed tetracycline-modified and SIM-loaded amorphous calcium carbonate (ACC) hybrid nanoparticles (TC/ACC/SIM) and found that TC/ACC/SIM can enhance its accumulation in osteoporotic sites and synergistically promote bone formation with calcium supplementation and SIM.Citation167
Although tetracycline combined with nanocarriers has shown good results in treating OP, its side effects, complex chemical structure, and poor stability during chemical modification seem to hinder further utilization of tetracycline as a bone-targeting agent.Citation168 Therefore, researchers hope to develop molecules with similar tetracycline-like abilities but with fewer side effects and greater stability. As a result, a minimized chemical structure B (3-amino-2,6-dihydroxy-benzamide) derived from tetracycline was designed, which has significantly fewer side effects compared to tetracycline while retaining 50% of its bone-binding ability.Citation168 Moreover, molecule C, which is a derivative of B with a succinate linker, has an even greater bone-binding ability than tetracycline. The structures of tetracycline and modified tetracycline molecules are shown in .
Bisphosphonates and Analogues
Bisphosphonates (BPs) are a class of drugs that inhibit bone resorption and are widely used in skeletal diseases such as OP.Citation169,Citation170 At the cellular level, the mechanism of action of BPs, especially their effect on osteoclasts, is mainly manifested as the inhibition of cell activity, shortening of cell lifespan, and inhibition of their recruitment and adhesion to the mineral matrix.Citation171 Additionally, BPs act as bone-targeting agents.Citation172 Studies have shown that BPs are similar to pyrophosphates (P-O-P), which naturally exist in the bone matrix. Pyrophosphate is a non-metabolic endogenous substance composed of an oxygen atom and two phosphate groups, while BPs are composed of a carbon atom and two phosphate groups (P-C-P).Citation173 The molecular structures of BPs and their analogs are shown in . The two phosphonate groups on BPs have a strong affinity for Ca2+ in HAP and can bidentate bind to the bone. For most BPs, if R1 is a hydroxyl or amino group, it can trigger tridentate binding to HAP, which makes it have a higher bone-binding affinity.Citation174,Citation175 With the deepening exploration of BPs, three generations of BPs have been approved for clinical use. The second generation contains nitrogen-containing BPs, such as alendronate (ALN), and the third generation contains nitrogen-containing heterocycles, such as risedronate. The nitrogen-containing group on the R2 side chain exhibits a higher affinity for HAP through hydrogen bonding.Citation176 Therefore, BPs have the dual advantages of being bone-targeting agents and anti-bone resorption agents and are widely used as targeting ligands for anti-OP NPs. For example, Hoque et al used ALN as a bone-targeting agent for the nanocarrier loaded with adenosine, which was administered systemically to ovariectomized mice.Citation177 Compared with the non-targeted nanocarrier, ALN could guide more than 45% of the nanocarrier to accumulate in the mouse vertebrae and restore the trabecular bone characteristics of ovariectomized mice to the level of the healthy group. Furthermore, similar to the study of TC-mPEG-PLGA loaded with astragaloside discussed in the previous chapter, researchers replaced the targeting agent from tetracycline with ALN. The targeted nanocarrier greatly improved the affinity and bone tissue concentration of astragaloside to HAP, and the oral bioavailability of astragaloside was significantly improved. The addition of ALN made the prevention and treatment of OP more effective.Citation72
Targeting Other Bone-Formation Surfaces
In addition to the typical targeting of bone surface ligands mentioned above, the affinity between certain bone proteins and HAP in nature has also sparked interest in bone-targeting strategies. Some studies have found that non-collagenous proteins in the bone matrix, such as bone sialoprotein and osteopontin, play important regulatory roles in the growth and dissolution of HAP and have an affinity for HAP to bind to it.Citation178 These proteins share a common feature of repetitive acidic amino acid sequences of L-aspartic acid (L-Asp) and L-glutamic acid (L-Glu).Citation179 In 2000, Kagugai et al found that when administered systemically, peptides containing repeating Asp or Glu amino acid residues can selectively deliver drugs to bone tissue.Citation180 Compared with peptides and proteins, oligopeptides have higher stability, better tissue penetration, and lower immunogenicity.Citation181 Compared with BPs containing P-C-P bonds, oligopeptides have a shorter half-life, do not produce long-term adverse reactions, and do not form micelles with metal ions, making them easier to be enzymatically metabolized into non-toxic substances.Citation12
Using acidic oligopeptides as bone-targeting agents to modify NPs also shows promising prospects. Sun et al designed a five-amino acid motif oligopeptide Ser-Asp-Ser-Ser-Asp (SDSSD), which has a binding affinity with osteoblast membrane inhibitor (also known as osteoblast-specific factor 2, OSF-2) expressed by osteoblasts.Citation182 They combined it with polyurethane (PU) nanomicelles to create a targeted nanocapsule, SDSSD-PU, that can target the bone formation surface to deliver anti-miR-214 to osteoblasts. This can increase bone formation, improve bone microstructure, and increase bone mass in ovariectomized osteoporotic mice without causing obvious toxicity or triggering an immune response in the body. Similarly, using this bone-targeting oligopeptide to modify MSC-Exos and loading siRNA targeting Shn3 can specifically inhibit the expression of the Shn3 gene in osteoblasts and inhibit osteoclast formation, providing inspiration for cell-free therapy for OP.Citation60 Kagugai et al found that fluorescently labeled Asp6 only accumulated in bone and teeth after systemic administration to rats for 24 hours.Citation180 Using the targeting ability of the peptide, a novel drug conjugated with L-Asp-hexapeptide and estradiol exhibited a good anti-OP treatment effect in the ovariectomized mice.Citation183 Tao et al used L-aspartic acid oligopeptide Asp6 as a bone-targeting peptide to deliver SIM-loaded novel LNPs to the osteoporotic bone, significantly enhancing the therapeutic effect of OP and demonstrating the advantages of bone-targeted drug delivery systems.Citation58
In addition, Zhang et al found that aspartic acid, serine, and six repeat sequences of serine (AspSerSer)6 have a very high affinity for mineralized nodules of osteoblasts and amorphous calcium phosphate. They connected these sequences to DOTAP cationic liposomes to develop a targeted delivery system that can specifically deliver siRNA to the surface of bone formation. The Plekho1 gene is an intracellular negative regulator of bone formation. Zhang et al encapsulated Plekho1-siRNA in liposomes connected to (AspSerSer)6 for targeted delivery. In vivo experiments found that the siRNA selectively accumulated on the bone surface, reduced the levels of Plekho1mRNA and protein in selective osteoblasts, significantly promoted bone formation, enhanced bone microstructure, and increased bone mass in healthy and osteoporotic rats. Bioimaging analysis further showed that this method was effective.Citation184
Similarly, Liang et al screened for a specific adapter molecule, CH6, for osteoblasts and developed a CH6-lipid nanoparticle (LNP)-Plekho1-siRNA delivery system for targeted Plekho1 delivery. By functionalizing the LNP with the adapter molecule CH6, the system achieved specific delivery of Plekho1-siRNA to osteoblasts. The CH6-LNP-siRNA targeting system showed higher accumulation in bone tissue, and its application in osteoporotic rats that underwent ovariectomy revealed significantly improved bone mineral density (BMD), relative bone mass (BV/TV), trabecular thickness (Tb.Th), trabecular separation (Tb.Sp), trabecular number (Tb.N), and structure model index (SMI), demonstrating good osteoblast specificity.Citation185
Overall, targeted group-modified nanodelivery systems can improve microstructure, increase bone mass, enhance bone mechanical properties, and significantly reduce side effects in OP models. Gene targeting modification can further enhance the function of targeted delivery systems from tissue specificity to cellular specificity, making it more precise and effective, which is beneficial for the clinical application of osteoporosis metabolism therapy.
Another interesting discovery is that bones are rich in Ca2+ and carry positive charges, making an ideal material for targeting bone surfaces with negative charges, which facilitates its affinity with positively charged bone. Researchers found that nHAP-loaded PTH with negative zeta potential can promote its affinity for Ca2+-rich bone tissue, enabling targeted localization and exerting anti-OP effects.Citation66
Targeting Bone Marrow
The development of bone-targeted delivery systems has the potential to improve the treatment of OP by targeting both bone surface and bone marrow. It is essential to have a clear understanding of the relationship between bone marrow and OP to achieve this. Increasing evidence suggests that bone loss in postmenopausal women and ovariectomized animals is always accompanied by abnormal accumulation of marrow adipose tissue (MAT).Citation186–189 Anti-OP drugs such as BPs, RLX, and TPD have been shown to reduce bone marrow adiposity.Citation187,Citation189,Citation190 The bone marrow microenvironment contains various types of cells, including adipocytes, stromal matrix cells, hematopoietic cells, osteoblasts, and osteoclasts, and can secrete various cytokines to regulate bone remodeling,Citation191 highlighting the importance of targeting the bone marrow.
NPs with a neutral surface charge and small size are promising candidates for targeted drug delivery to the bone marrow, where they can accumulate and release drugs over an extended period.Citation192 Researchers have identified various potential targeting ligands for bone marrow receptors, including pregnancy zone protein (PZP) in the exosomes secreted by endothelial cellsCitation193 and E-selectin expressed on the surface of bone marrow endothelial cells.Citation194 Although the use of PZP to treat bone tumors has been explored, the use of PZP and E-selectin to treat osteoporosis has not been investigated and might become a novel direction for future research. Researchers have also modified LNPs with anionic amphiphiles. The hydrophilic head group on the modified NP can be recognized by scavenger receptors expressed on bone marrow macrophages, providing another potential target for the bone marrow.Citation195,Citation196
It has been found that stromal cell-derived factor 1 (SDF1) in the bone marrow has been found to recruit CXCR4+ hematopoietic stem cells (HSCs) and promote bone metastasis of CXCR4+ tumor cells. In a prospective study, researchers have used this finding to develop a targeted drug delivery approach, as discussed in the exosome section.Citation61 Hu et al genetically engineered NIH-3T3 cells to secrete Exos with high CXCR4 expression. They found that these Exos are selectively accumulated in the bone marrow. They then fused these Exos with liposomes carrying antagomir-188 to form hybrid Exos, which could accumulate antagomir-188 in the bone marrow. This approach promoted osteogenesis and inhibited BMSCs from differentiating into adipocytes, thereby reversing age-related bone loss.
Based on the receptor-ligand binding theory and inspired by the molecular mechanism of prostate cancer bone metastasis, scientists have expressed GLG1 (Golgi glycoprotein) on the surface of Exos and collected GLG1+ Exos from a tool cell line to construct GLG1+ drug-loaded nanoparticles (GLG1-NP) carrying Wnt pathway activator Wnt agonist 1. The results showed that peripheral administration of GLG1-NP achieved specific distribution in bone tissue. In a mouse model of OP induced by chronic colitis, GLG1-NP significantly improved bone mass, mechanical properties, BMSC osteogenic differentiation, and bone formation. Additionally, GLG1-NP promoted fracture healing in mice with ulcerative colitis and reduced bone marrow fat accumulation, achieving significant therapeutic effects in bone complications of mice with ulcerative colitis.Citation197
In summary, the utilization of NPs to enhance drug delivery across biological barriers and improve the efficacy of precision medicine holds the potential to accelerate the clinical translation of targeted NPs for the treatment of OP. Developing nanobiomaterials for precision medicine in OP requires carefully designed methods to adjust the composition of NPs, examine the pharmacokinetics of therapeutic drugs, and optimize drugs’ solubility, administration, and biological distribution. This highly customizable platform has the potential to accelerate the clinical translation of targeted NPs for OP treatment.
Conclusion and Outlook
The high prevalence of OP is a significant health concern, posing a tremendous burden on patients, their families, and society. Although current conventional clinical medications provide some symptomatic relief, their limitations and adverse effects remain unresolved, severely restricting their use. Therefore, finding low-toxic, stable, specific and efficient drug delivery methods for the treatment of osteoporosis has become a key area of research. Fortunately, in the past few decades, the development of nanomedicine has created new possibilities for the diagnosis and treatment of many diseases. In particular, the application of nanotechnology for bone targeting has been successful in the field of bone tumors, but the application of nanocarrier bone-targeted drug delivery in osteoporosis treatment is still at an early stage.
In this review, we introduce bone-targeted nano-delivery carriers, modification strategies for bone targeting, and their applications in OP therapy. Currently, the most studied nanocarriers for OP include LPS, Exos, SPIONs, PLGA NPs, nHAP, and CS-NPs. Among them, Exos, as cell-derived nanomaterials with low immunogenicity, good barrier penetration, and targeting properties, is expected to overcome the disadvantages of traditional nanomaterials such as potential cytotoxicity, poor biodegradability, and uncontrolled drug release and other drawbacks, showing great promise for effective treatment of OP. In addition, the plasticity of nanocarriers allows us to integrate their advantages to create more desirable nanocarriers, such as the fusion of multiple nanocarriers (eg, hybrid liposomes and Exos), which is a future direction for the optimization of biocompatible nanocarriers. However, these nanodrug release mechanisms need to be further explored, and we need to fully understand the effect of magnetic field variations on drug release, but many other factors such as temperature, pH, light, linkage modifications between the drug and the carrier, and bone-specific enzymes may also regulate drug release. Future studies should focus on these factors to better understand drug release from bone-targeted nanocarriers. Follow-up studies are needed to accurately address all aspects of a mature bone-targeted nanodrug delivery system if clinical applications are to be realized as soon as possible. We eagerly anticipate that bone-targeted delivery of nanomedicines will benefit every osteoporosis patient in the future.
Disclosure
The authors declare that they have no competing interests.
Additional information
Funding
References
- Osterhoff G, Morgan EF, Shefelbine SJ, et al. Bone mechanical properties and changes with osteoporosis. Injury. 2016;47 Suppl 2:S11–20. doi:10.1016/S0020-1383(16)47003-8
- Compston JE, McClung MR, Leslie WD. Osteoporosis. Lancet. 2019;393(10169):364–376. doi:10.1016/S0140-6736(18)32112-3
- Ensrud KE, Crandall CJ. Osteoporosis. Ann Intern Med. 2017;167(3):ITC17–ITC32. doi:10.7326/AITC201708010
- Kirk B, Zanker J, Duque G. Osteosarcopenia: epidemiology, diagnosis, and treatment-facts and numbers. J Cachexia, Sarcopenia Muscle. 2020;11(3):609–618. doi:10.1002/jcsm.12567
- Karsdal MA, Bay-Jensen AC, Lories RJ, et al. The coupling of bone and cartilage turnover in osteoarthritis: opportunities for bone antiresorptives and anabolics as potential treatments? Ann Rheum Dis. 2014;73(2):336–348. doi:10.1136/annrheumdis-2013-204111
- Tella SH, Gallagher JC. Prevention and treatment of postmenopausal osteoporosis. J Steroid Biochem Mol Biol. 2014;142:155–170. doi:10.1016/j.jsbmb.2013.09.008
- Luhmann T, Germershaus O, Groll J, Meinel L. Bone targeting for the treatment of osteoporosis. J Control Release. 2012;161(2):198–213. doi:10.1016/j.jconrel.2011.10.001
- Canalis E. Wnt signalling in osteoporosis: mechanisms and novel therapeutic approaches. Nat Rev Endocrinol. 2013;9(10):575–583. doi:10.1038/nrendo.2013.154
- Kawai M, Modder UI, Khosla S, Rosen CJ. Emerging therapeutic opportunities for skeletal restoration. Nat Rev Drug Discov. 2011;10(2):141–156. doi:10.1038/nrd3299
- Low SA, Kopecek J. Targeting polymer therapeutics to bone. Adv Drug Deliv Rev. 2012;64(12):1189–1204. doi:10.1016/j.addr.2012.01.012
- Hirabayashi H, Takahashi T, Fujisaki J, et al. Bone-specific delivery and sustained release of diclofenac, a non-steroidal anti-inflammatory drug, via bisphosphonic prodrug based on the Osteotropic Drug Delivery System (ODDS). J Control Release. 2001;70(1–2):183–191. doi:10.1016/s0168-3659(00)00355-2
- Murphy MB, Hartgerink JD, Goepferich A, Mikos AG. Synthesis and in vitro hydroxyapatite binding of peptides conjugated to calcium-binding moieties. Biomacromolecules. 2007;8(7):2237–2243. doi:10.1021/bm070121s
- Katsumi H, Yamashita S, Morishita M, Yamamoto A. Bone-Targeted Drug Delivery Systems and Strategies for Treatment of Bone Metastasis. Chem Pharm Bull. 2020;68(7):560–566. doi:10.1248/cpb.c20-00017
- Rotman SG, Grijpma DW, Richards RG, et al. Drug delivery systems functionalized with bone mineral seeking agents for bone targeted therapeutics. J Control Release. 2018;269:88–99. doi:10.1016/j.jconrel.2017.11.009
- Dodson TB, Guralnick WC, Donoff RB, Kaban LB. Massachusetts General Hospital/Harvard Medical School MD oral and maxillofacial surgery program: a 30-year review. J Oral Maxillofac Surg. 2004;62(1):62–65. doi:10.1016/j.joms.2002.12.002
- Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg. 2003;61(9):1115–1117. doi:10.1016/s0278-2391(03)00720-1
- Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg. 2004;62:527–534. doi:10.1016/j.joms.2004.02.004
- Sellmeyer DE. Atypical fractures as a potential complication of long-term bisphosphonate therapy. JAMA. 2010;304(13):1480–1484. doi:10.1001/jama.2010.1360
- Odvina CV, Zerwekh JE, Rao DS, et al. Severely suppressed bone turnover: a potential complication of alendronate therapy. J Clin Endocrinol Metab. 2005;90(3):1294–1301. doi:10.1210/jc.2004-0952
- Wysowski DK. Reports of esophageal cancer with oral bisphosphonate use. N Engl J Med. 2009;360(1):89–90. doi:10.1056/NEJMc0808738
- Lin JH. Bisphosphonates: a review of their pharmacokinetic properties. Bone. 1996;18(2):75–85. doi:10.1016/8756-3282(95)00445-9
- Khajuria DK, Razdan R, Mahapatra DR. Drugs for the management of osteoporosis: a review. Rev Bras Reumatol. 2011;51(4):365–371, 379–382.
- Camacho PM, Petak SM, Binkley N, et al. American Association of Clinical Endocrinologists and American College of Endocrinology Clinical Practice Guidelines for the Diagnosis and Treatment of Postmenopausal Osteoporosis - 2016. Endocr Pract. 2016;22:1–42. doi:10.4158/EP161435.GL
- Compston J, et al. UK clinical guideline for the prevention and treatment of osteoporosis. Arch Osteoporos. 2017;12:43. doi:10.1007/s11657-017-0324-5
- Tarantino U, Iolascon G, Cianferotti L, et al. Clinical guidelines for the prevention and treatment of osteoporosis: summary statements and recommendations from the Italian Society for Orthopaedics and Traumatology. J Orthop Traumatol. 2017;18(S1):3–36. doi:10.1007/s10195-017-0474-7
- Viereck V. Raloxifene concurrently stimulates osteoprotegerin and inhibits interleukin-6 production by human trabecular osteoblasts. J Clin Endocrinol Metab. 2003;88(9):4206–4213. doi:10.1210/jc.2002-021877
- Black DM, Rosen CJ. Clinical Practice. Postmenopausal Osteoporosis. N Engl J Med. 2016;374:254–262. doi:10.1056/NEJMcp1513724
- Tseng CH. Synthesis and anti-osteoporotic evaluation of certain 3-amino-2-hydroxypropoxyisoflavone derivatives. Eur J Med Chem. 2009;44:3621–3626. doi:10.1016/j.ejmech.2009.02.025
- Rachner TD, Khosla S, Hofbauer LC. Osteoporosis: now and the future. Lancet. 2011;377:1276–1287. doi:10.1016/S0140-6736(10)62349-5
- Cummings SR, Martin JS, McClung MR, et al. Denosumab for prevention of fractures in postmenopausal women with osteoporosis. N Engl J Med. 2009;361(8):756–765. doi:10.1056/NEJMoa0809493
- Wada S, Udagawa N, Nagata N, Martin TJ, Findlay DM. Physiological levels of calcitonin regulate the mouse osteoclast calcitonin receptor by a protein kinase Alpha-mediated mechanism. Endocrinology. 1996;137:312–320. doi:10.1210/endo.137.1.8536630
- Karsdal MA, Sondergaard BC, Arnold M, Christiansen C. Calcitonin affects both bone and cartilage: a dual action treatment for osteoarthritis? Ann N Y Acad Sci. 2007;1117:181–195. doi:10.1196/annals.1402.041
- Okazaki R. Osteosarcoma in rats receiving long-term PTH injection. Clin Calcium. 2003;13:42–44.
- Arceo-Mendoza RM, Camacho PM. Postmenopausal Osteoporosis: latest Guidelines. Endocrinol Metab Clin North Am. 2021;50(2):167–178. doi:10.1016/j.ecl.2021.03.009
- Safra T, Muggia F, Jeffers S, et al. Pegylated liposomal doxorubicin (doxil): reduced clinical cardiotoxicity in patients reaching or exceeding cumulative doses of 500 mg/m2. Ann Oncol. 2000;11(8):1029–1033. doi:10.1023/a:1008365716693
- Schroeder A, Heller DA, Winslow MM, et al. Treating metastatic cancer with nanotechnology. Nat Rev Cancer. 2011;12:39–50. doi:10.1038/nrc3180
- Cheng H, Chawla A, Yang Y, et al. Development of nanomaterials for bone-targeted drug delivery. Drug Discov Today. 2017;22(9):1336–1350. doi:10.1016/j.drudis.2017.04.021
- Cheng Y, Xu T. The effect of dendrimers on the pharmacodynamic and pharmacokinetic behaviors of non-covalently or covalently attached drugs. Eur J Med Chem. 2008;43(11):2291–2297. doi:10.1016/j.ejmech.2007.12.021
- Yang W, Li Y, Cheng Y, et al. Evaluation of phenylbutazone and poly(amidoamine) dendrimers interactions by a combination of solubility, 2D-NOESY NMR, and isothermal titration calorimetry studies. J Pharm Sci. 2009;98(3):1075–1085. doi:10.1002/jps.21519
- Park JH, et al. Cooperative nanoparticles for tumor detection and photothermally triggered drug delivery. Adv Mater. 2010;22:880–885. doi:10.1002/adma.200902895
- von Maltzahn G, Centrone A, Park J-H, et al. SERS-Coded Gold Nanorods as a Multifunctional Platform for Densely Multiplexed Near-Infrared Imaging and Photothermal Heating. Adv Mater. 2009;21(31):3175–3180. doi:10.1002/adma.200803464
- Gabizon A, Shmeeda H, Barenholz Y. Pharmacokinetics of pegylated liposomal Doxorubicin: review of animal and human studies. Clin Pharmacokinet. 2003;42(5):419–436. doi:10.2165/00003088-200342050-00002
- Duncan R, Gaspar R. Nanomedicine(s) under the microscope. Mol Pharm. 2011;8:2101–2141. doi:10.1021/mp200394t
- Wang J, Tian S, Petros RA, Napier ME, Desimone JM. The complex role of multivalency in nanoparticles targeting the transferrin receptor for cancer therapies. J Am Chem Soc. 2010;132(32):11306–11313. doi:10.1021/ja1043177
- Li Z, Xiang J, Zhang W, et al. Nanoparticle delivery of anti-metastatic NM23-H1 gene improves chemotherapy in a mouse tumor model. Cancer Gene Ther. 2009;16(5):423–429. doi:10.1038/cgt.2008.97
- Davis ME, Zuckerman JE, Choi CHJ, et al. Evidence of RNAi in humans from systemically administered siRNA via targeted nanoparticles. Nature. 2010;464(7291):1067–1070. doi:10.1038/nature08956
- Ma L, Young J, Prabhala H, et al. miR-9, a MYC/MYCN-activated microRNA, regulates E-cadherin and cancer metastasis. Nat Cell Biol. 2010;12(3):247–256. doi:10.1038/ncb2024
- Vo TN, Kasper FK, Mikos AG. Strategies for controlled delivery of growth factors and cells for bone regeneration. Adv Drug Deliv Rev. 2012;64:1292–1309. doi:10.1016/j.addr.2012.01.016
- Choi SW, Kim JH. Design of surface-modified poly(D,L-lactide-co-glycolide) nanoparticles for targeted drug delivery to bone. J Control Release. 2007;122:24–30. doi:10.1016/j.jconrel.2007.06.003
- Chen Y, Wu X, Li J, et al. Bone-Targeted Nanoparticle Drug Delivery System: an Emerging Strategy for Bone-Related Disease. Front Pharmacol. 2022;13:909408. doi:10.3389/fphar.2022.909408
- Ordikhani F, Zandi N, Mazaheri M, et al. Targeted nanomedicines for the treatment of bone disease and regeneration. Med Res Rev. 2021;41(3):1221–1254. doi:10.1002/med.21759
- Liu J, Dang L, Li D, et al. A delivery system specifically approaching bone resorption surfaces to facilitate therapeutic modulation of microRNAs in osteoclasts. Biomaterials. 2015;52:148–160. doi:10.1016/j.biomaterials.2015.02.007
- Basha G, Cottle AG, Pretheeban T, et al. Lipid nanoparticle-mediated silencing of osteogenic suppressor GNAS leads to osteogenic differentiation of mesenchymal stem cells in vivo. Mol Ther. 2022;30(9):3034–3051. doi:10.1016/j.ymthe.2022.06.012
- Vhora I, Lalani R, Bhatt P, Patil S, Misra A. Lipid-nucleic acid nanoparticles of novel ionizable lipids for systemic BMP-9 gene delivery to bone-marrow mesenchymal stem cells for osteoinduction. Int J Pharm. 2019;563:324–336. doi:10.1016/j.ijpharm.2019.04.006
- Hosny KM, Bahmdan RH, Alhakamy NA, et al. Physically Optimized Nano-Lipid Carriers Augment Raloxifene and Vitamin D Oral Bioavailability in Healthy Humans for Management of Osteoporosis. J Pharm Sci. 2020;109(7):2145–2155. doi:10.1016/j.xphs.2020.03.009
- Nabi-Meibodi M, Vatanara A, Najafabadi AR, et al. The effective encapsulation of a hydrophobic lipid-insoluble drug in solid lipid nanoparticles using a modified double emulsion solvent evaporation method. Colloids Surf B Biointerfaces. 2013;112:408–414. doi:10.1016/j.colsurfb.2013.06.013
- Du X, Gao N, Song X. Bioadhesive polymer/lipid hybrid nanoparticles as oral delivery system of raloxifene with enhancive intestinal retention and bioavailability. Drug Deliv. 2021;28(1):252–260. doi:10.1080/10717544.2021.1872742
- Tao S, Chen S-Q, Zhou W-T, et al. A novel biocompatible, simvastatin-loaded, bone-targeting lipid nanocarrier for treating osteoporosis more effectively. RSC Adv. 2020;10(35):20445–20459. doi:10.1039/d0ra00685h
- Elnaggar YSR, Omran S, Hazzah HA, Abdallah OY. Anionic versus cationic bilosomes as oral nanocarriers for enhanced delivery of the hydrophilic drug risedronate. Int J Pharm. 2019;564:410–425. doi:10.1016/j.ijpharm.2019.04.069
- Cui Y, Guo Y, Kong L, et al. A bone-targeted engineered exosome platform delivering siRNA to treat osteoporosis. Bioact Mater. 2022;10:207–221. doi:10.1016/j.bioactmat.2021.09.015
- Hu Y, Li X, Zhang Q, et al. Exosome-guided bone targeted delivery of Antagomir-188 as an anabolic therapy for bone loss. Bioact Mater. 2021;6(9):2905–2913. doi:10.1016/j.bioactmat.2021.02.014
- Lu GD, Cheng P, Liu T, Wang Z. BMSC-Derived Exosomal miR-29a Promotes Angiogenesis and Osteogenesis. Front Cell Dev Biol. 2020;8:608521. doi:10.3389/fcell.2020.608521
- Xu L, Xu X, Liang Y, et al. Osteoclast-targeted delivery of anti-miRNA oligonucleotides by red blood cell extracellular vesicles. J Controlled Release. 2023;358:259–272. doi:10.1016/j.jconrel.2023.04.043
- Marycz K, Smieszek A, Marcinkowska K, et al. Nanohydroxyapatite (nHAp) Doped with Iron Oxide Nanoparticles (IO), miR-21 and miR-124 Under Magnetic Field Conditions Modulates Osteoblast Viability, Reduces Inflammation and Inhibits the Growth of Osteoclast - A Novel Concept for Osteoporosis Treatment: part 1. Int J Nanomed. 2021;16:3429–3456. doi:10.2147/IJN.S303412
- Liu Q, Feng L, Chen Z, et al. Ultrasmall Superparamagnetic Iron Oxide Labeled Silk Fibroin/Hydroxyapatite Multifunctional Scaffold Loaded With Bone Marrow-Derived Mesenchymal Stem Cells for Bone Regeneration. Front Bioeng Biotechnol. 2020;8:697. doi:10.3389/fbioe.2020.00697
- Dave JR, Dewle AM, Mhaske ST, et al. Hydroxyapatite nanorods loaded with parathyroid hormone (PTH) synergistically enhance the net formative effect of PTH anabolic therapy. Nanomedicine. 2019;15(1):218–230. doi:10.1016/j.nano.2018.10.003
- Zhu W, Wang D, Zhang X, et al. Experimental study of nano-hydroxyapatite/recombinant human bone morphogenetic protein-2 composite artificial bone. Artif Cells Blood Substitutes Immobilization Biotechnol. 2010;38(3):150–156. doi:10.3109/10731191003712756
- Kettenberger U, Luginbuehl V, Procter P, Pioletti DP. In vitro and in vivo investigation of bisphosphonate-loaded hydroxyapatite particles for peri-implant bone augmentation. J Tissue Eng Regen Med. 2017;11(7):1974–1985. doi:10.1002/term.2094
- Kotak DJ, Devarajan PV. Bone targeted delivery of salmon calcitonin hydroxyapatite nanoparticles for sublingual osteoporosis therapy (SLOT). Nanomedicine. 2020;24:102153. doi:10.1016/j.nano.2020.102153
- Khajuria DK, Razdan R, Mahapatra DR. Development, in vitro and in vivo characterization of zoledronic acid functionalized hydroxyapatite nanoparticle based formulation for treatment of osteoporosis in animal model. Eur J Pharm Sci. 2015;66:173–183. doi:10.1016/j.ejps.2014.10.015
- Khajuria DK, Disha C, Vasireddi R, Razdan R, Mahapatra DR. Risedronate/zinc-hydroxyapatite based nanomedicine for osteoporosis. Mater Sci Eng C Mater Biol Appl. 2016;63:78–87. doi:10.1016/j.msec.2016.02.062
- Xi Y, Wang W, Ma L, et al. Alendronate modified mPEG-PLGA nano-micelle drug delivery system loaded with astragaloside has anti-osteoporotic effect in rats. Drug Deliv. 2022;29(1):2386–2402. doi:10.1080/10717544.2022.2086942
- Wang H, Liu J, Tao S, et al. Tetracycline-grafted PLGA nanoparticles as bone-targeting drug delivery system. Int J Nanomed. 2015;10:5671–5685. doi:10.2147/IJN.S88798
- Takeuchi I, Fukuda K, Kobayashi S, Makino K. Transdermal delivery of estradiol-loaded PLGA nanoparticles using iontophoresis for treatment of osteoporosis. Biomed Mater Eng. 2016;27:475–483. doi:10.3233/BME-161601
- Zhang C, Zhang W, Zhu D, et al. Nanoparticles functionalized with stem cell secretome and CXCR4-overexpressing endothelial membrane for targeted osteoporosis therapy. J Nanobiotechnology. 2022;20(1):35. doi:10.1186/s12951-021-01231-6
- Kang JM, Kang SW, La WG, Yang YS, Kim BS. Enhancement of in vivo bone regeneration efficacy of osteogenically undifferentiated human cord blood mesenchymal stem cells. J Biomed Mater Res A. 2010;93(2):666–672. doi:10.1002/jbm.a.32282
- Saini D, Fazil M, Ali MM, Baboota S, Ali J. Formulation, development and optimization of raloxifene-loaded chitosan nanoparticles for treatment of osteoporosis. Drug Deliv. 2015;22(6):823–836. doi:10.3109/10717544.2014.900153
- Narayanan D, Anitha A, Jayakumar R, Chennazhi KP. In vitro and in vivo evaluation of osteoporosis therapeutic peptide PTH 1-34 loaded pegylated chitosan nanoparticles. Mol Pharm. 2013;10:4159–4167. doi:10.1021/mp400184v
- Santhosh S, Mukherjee D, Anbu J, Murahari M, Teja BV. Improved treatment efficacy of risedronate functionalized chitosan nanoparticles in osteoporosis: formulation development, in vivo, and molecular modelling studies. J Microencapsul. 2019;36(4):338–355. doi:10.1080/02652048.2019.1631401
- Narayanan D, Anitha A, Jayakumar R, Nair SV, Chennazhi KP. Synthesis, characterization and preliminary in vitro evaluation of PTH 1-34 loaded chitosan nanoparticles for osteoporosis. J Biomed Nanotechnol. 2012;8:98–106. doi:10.1166/jbn.2012.1367
- Alshubaily FA, Jambi EJ. Correlation between Antioxidant and Anti-Osteoporotic Activities of Shilajit Loaded into Chitosan Nanoparticles and Their Effects on Osteoporosis in Rats. Polymers. 2022;14(19):3972. doi:10.3390/polym14193972
- Abourehab MAS. Hyaluronic Acid Modified Risedronate and Teriparatide Co-loaded Nanocarriers for Improved Osteogenic Differentiation of Osteoblasts for the Treatment of Osteoporosis. Curr Pharm Des. 2019;25(27):2975–2988. doi:10.2174/1381612825666190801140703
- Gaba B, Fazil M, Ali A, et al. Nanostructured lipid (NLCs) carriers as a bioavailability enhancement tool for oral administration. Drug Deliv. 2015;22(6):691–700. doi:10.3109/10717544.2014.898110
- Jeong K, Kang CS, Kim Y, et al. Development of highly efficient nanocarrier-mediated delivery approaches for cancer therapy. Cancer Lett. 2016;374(1):31–43. doi:10.1016/j.canlet.2016.01.050
- Bawarski WE, Chidlowsky E, Bharali DJ, Mousa SA. Emerging nanopharmaceuticals. Nanomedicine. 2008;4(4):273–282. doi:10.1016/j.nano.2008.06.002
- Pattni BS, Chupin VV, Torchilin VP. New Developments in Liposomal Drug Delivery. Chem Rev. 2015;115(19):10938–10966. doi:10.1021/acs.chemrev.5b00046
- Min Y, Caster JM, Eblan MJ, Wang AZ. Clinical Translation of Nanomedicine. Chem Rev. 2015;115(19):11147–11190. doi:10.1021/acs.chemrev.5b00116
- Barenholz Y. Doxil(R)--The first FDA-approved nano-drug: lessons learned. J Control Release. 2012;160(2):117–134. doi:10.1016/j.jconrel.2012.03.020
- Zhao Y, Alakhova DY, Kabanov AV. Can nanomedicines kill cancer stem cells? Adv Drug Deliv Rev. 2013;65(13–14):1763–1783. doi:10.1016/j.addr.2013.09.016
- Allen TM, Cullis PR. Liposomal drug delivery systems: from concept to clinical applications. Adv Drug Deliv Rev. 2013;65:36–48. doi:10.1016/j.addr.2012.09.037
- Rexeisen EL, Fan W, Pangburn TO, et al. Self-assembly of fibronectin mimetic peptide-amphiphile nanofibers. Langmuir. 2010;26(3):1953–1959. doi:10.1021/la902571q
- Mura S, Nicolas J, Couvreur P. Stimuli-responsive nanocarriers for drug delivery. Nat Mater. 2013;12(11):991–1003. doi:10.1038/nmat3776
- Song H, Zhang J, Liu X, et al. Development of a bone targeted thermosensitive liposomal doxorubicin formulation based on a bisphosphonate modified non-ionic surfactant. Pharm Dev Technol. 2016;21(6):680–687. doi:10.3109/10837450.2015.1045617
- Ferreira Ddos S, Boratto FA, Cardoso VN, et al. Alendronate-coated long-circulating liposomes containing 99mtechnetium-ceftizoxime used to identify osteomyelitis. Int J Nanomed. 2015;10:2441–2450. doi:10.2147/IJN.S76168
- Rawat P. Revisiting bone targeting potential of novel hydroxyapatite based surface modified PLGA nanoparticles of risedronate: pharmacokinetic and biochemical assessment. Int J Pharm. 2016;506(1–2):253–261. doi:10.1016/j.ijpharm.2016.04.049
- Kalluri R, LeBleu VS. The biology, function, and biomedical applications of exosomes. Science. 2020;367(6478). doi:10.1126/science.aau6977
- Liang Y, Duan L, Lu J, Xia J. Engineering exosomes for targeted drug delivery. Theranostics. 2021;11(7):3183–3195. doi:10.7150/thno.52570
- Xu X, Iqbal Z, Xu L, et al. Brain-derived extracellular vesicles: potential diagnostic biomarkers for central nervous system diseases. Psychiatry Clin Neurosci. 2023;78(2):83–96. doi:10.1111/pcn.13610
- Xu X, Xu L, Xia J, et al. Harnessing knee joint resident mesenchymal stem cells in cartilage tissue engineering. Acta Biomater. 2023;168:372–387. doi:10.1016/j.actbio.2023.07.024
- Sun W, Zhao C, Li Y, et al. Osteoclast-derived microRNA-containing exosomes selectively inhibit osteoblast activity. Cell Discov. 2016;2(1):16015. doi:10.1038/celldisc.2016.15
- Li D, Liu J, Guo B, et al. Osteoclast-derived exosomal miR-214-3p inhibits osteoblastic bone formation. Nat Commun. 2016;7(1):10872. doi:10.1038/ncomms10872
- Cui Y, Luan J, Li H, Zhou X, Han J. Exosomes derived from mineralizing osteoblasts promote ST2 cell osteogenic differentiation by alteration of microRNA expression. FEBS Lett. 2016;590(1):185–192. doi:10.1002/1873-3468.12024
- Xu X, Liang Y, Li X, et al. Exosome-mediated delivery of kartogenin for chondrogenesis of synovial fluid-derived mesenchymal stem cells and cartilage regeneration. Biomaterials. 2021;269:120539. doi:10.1016/j.biomaterials.2020.120539
- Liang Y, Xu X, Li X, et al. Chondrocyte-Targeted MicroRNA Delivery by Engineered Exosomes toward a Cell-Free Osteoarthritis Therapy. ACS Appl. Mater. Interfaces. 2020;12(33):36938–36947. doi:10.1021/acsami.0c10458
- Liu Q, Li D, Pan X, Liang Y. Targeted therapy using engineered extracellular vesicles: principles and strategies for membrane modification. J Nanobiotechnology. 2023;21(1):334. doi:10.1186/s12951-023-02081-0
- Xu X, Xu L, Wen C, et al. Programming assembly of biomimetic exosomes: an emerging theranostic nanomedicine platform. Mater Today Bio. 2023;22:100760. doi:10.1016/j.mtbio.2023.100760
- Liang Y, Iqbal Z, Lu J, et al. Cell-derived nanovesicle-mediated drug delivery to the brain: principles and strategies for vesicle engineering. Mol Ther. 2023;31(5):1207–1224. doi:10.1016/j.ymthe.2022.10.008
- Iqbal Z, Rehman K, Xia J, et al. Biomaterial-assisted targeted and controlled delivery of CRISPR/Cas9 for precise gene editing. Biomater. Sci. 2023;11(11):3762–3783. doi:10.1039/d2bm01636b
- Liang Y, Xu X, Xu L, et al. Chondrocyte-specific genomic editing enabled by hybrid exosomes for osteoarthritis treatment. Theranostics. 2022;12(11):4866–4878. doi:10.7150/thno.69368
- Freeman MW, Arrott AS, Watson JHL. Magnetism in Medicine. J Appl Phys. 1960;31(5):S404–S405. doi:10.1063/1.1984765
- Li Y, Ye D, Li M, Ma M, Gu N. Adaptive Materials Based on Iron Oxide Nanoparticles for Bone Regeneration. Chemphyschem. 2018;19(16):1965–1979. doi:10.1002/cphc.201701294
- Dadfar SM, Roemhild K, Drude NI, et al. Iron oxide nanoparticles: diagnostic, therapeutic and theranostic applications. Adv Drug Deliv Rev. 2019;138:302–325. doi:10.1016/j.addr.2019.01.005
- Zhi D, Yang T, Yang J, Fu S, Zhang S. Targeting strategies for superparamagnetic iron oxide nanoparticles in cancer therapy. Acta Biomater. 2020;102:13–34. doi:10.1016/j.actbio.2019.11.027
- Yuan Y, He Y, Bo R, et al. A facile approach to fabricate self-assembled magnetic nanotheranostics for drug delivery and imaging. Nanoscale. 2018;10(46):21634–21639. doi:10.1039/c8nr05141k
- Wahajuddin A, Arora S. Superparamagnetic iron oxide nanoparticles: magnetic nanoplatforms as drug carriers. Int J Nanomed. 2012;7:3445–3471. doi:10.2147/IJN.S30320
- Amstad E, Zurcher S, Mashaghi A, et al. Surface functionalization of single superparamagnetic iron oxide nanoparticles for targeted magnetic resonance imaging. Small. 2009;5(11):1334–1342. doi:10.1002/smll.200801328
- Sengupta S, Sasisekharan R. Exploiting nanotechnology to target cancer. Br J Cancer. 2007;96(9):1315–1319. doi:10.1038/sj.bjc.6603707
- Ruoslahti E, Bhatia SN, Sailor MJ. Targeting of drugs and nanoparticles to tumors. J Cell Biol. 2010;188(6):759–768. doi:10.1083/jcb.200910104
- Yang J, Wu J, Guo Z, Zhang G, Zhang H. Iron Oxide Nanoparticles Combined with Static Magnetic Fields in Bone Remodeling. Cells. 2022;11(20):3298. doi:10.3390/cells11203298
- Liu L, Jin R, Duan J, et al. Bioactive iron oxide nanoparticles suppress osteoclastogenesis and ovariectomy-induced bone loss through regulating the TRAF6-p62-CYLD signaling complex. Acta Biomater. 2020;103:281–292. doi:10.1016/j.actbio.2019.12.022
- Iyer SR, Xu S, Stains JP, Bennett CH, Lovering RM. Superparamagnetic Iron Oxide Nanoparticles in Musculoskeletal Biology. Tissue Eng Part B Rev. 2017;23(4):373–385. doi:10.1089/ten.TEB.2016.0437
- Zhou H, Lee J. Nanoscale hydroxyapatite particles for bone tissue engineering. Acta Biomater. 2011;7(7):2769–2781. doi:10.1016/j.actbio.2011.03.019
- Bai B, Jazrawi LM, Kummer FJ, Spivak JM. The use of an injectable, biodegradable calcium phosphate bone substitute for the prophylactic augmentation of osteoporotic vertebrae and the management of vertebral compression fractures. Spine. 1999;24(15):1521–1526. doi:10.1097/00007632-199908010-00004
- Schildhauer TA, Bennett AP, Wright TM, Lane JM, O’Leary PF. Intravertebral body reconstruction with an injectable in situ -setting carbonated apatite: biomechanical evaluation of a minimally invasive technique. J Orthop Res. 1999;17(1):67–72. doi:10.1002/jor.1100170111
- Maestretti G, Cremer C, Otten P, Jakob RP. Prospective study of standalone balloon kyphoplasty with calcium phosphate cement augmentation in traumatic fractures. Eur Spine J. 2007;16(5):601–610. doi:10.1007/s00586-006-0258-x
- Libicher M, Hillmeier J, Liegibel U, et al. Osseous integration of calcium phosphate in osteoporotic vertebral fractures after kyphoplasty: initial results from a clinical and experimental pilot study. Osteoporos Int. 2006;17(8):1208–1215. doi:10.1007/s00198-006-0128-8
- Ginebra MP, Canal C, Espanol M, Pastorino D, Montufar EB. Calcium phosphate cements as drug delivery materials. Adv Drug Deliv Rev. 2012;64(12):1090–1110. doi:10.1016/j.addr.2012.01.008
- Panzavolta S, Torricelli P, Bracci B, Fini M, Bigi A. Alendronate and Pamidronate calcium phosphate bone cements: setting properties and in vitro response of osteoblast and osteoclast cells. J Inorg Biochem. 2009;103(1):101–106. doi:10.1016/j.jinorgbio.2008.09.012
- Panzavolta S, Torricelli P, Bracci B, Fini M, Bigi A. Functionalization of biomimetic calcium phosphate bone cements with alendronate. J Inorg Biochem. 2010;104(10):1099–1106. doi:10.1016/j.jinorgbio.2010.06.008
- Sun F, Zhou H, Lee J. Various preparation methods of highly porous hydroxyapatite/polymer nanoscale biocomposites for bone regeneration. Acta Biomater. 2011;7(11):3813–3828. doi:10.1016/j.actbio.2011.07.002
- Maia ALC, Ferreira CDA, Barros ALBD, et al. Vincristine-loaded hydroxyapatite nanoparticles as a potential delivery system for bone cancer therapy. J Drug Target. 2018;26(7):592–603. doi:10.1080/1061186X.2017.1401078
- Noor Z. Nanohydroxyapatite application to osteoporosis management. J Osteoporos. 2013;2013:679025. doi:10.1155/2013/679025
- Mora-Raimundo P, Lozano D, Manzano M, Vallet-Regi M. Nanoparticles to Knockdown Osteoporosis-Related Gene and Promote Osteogenic Marker Expression for Osteoporosis Treatment. ACS Nano. 2019;13(5):5451–5464. doi:10.1021/acsnano.9b00241
- Isobe M, Amagasa T, Oida S-I, et al. Bone morphogenetic protein encapsulated with a biodegradable and biocompatible polymer. J Biomed Mater Res. 1996;32(3):433–438. doi:10.1002/(SICI)1097-4636(199611)32:3<433::AID-JBM17>3.0.CO;2-H
- Walmsley GG, McArdle A, Tevlin R, et al. Nanotechnology in bone tissue engineering. Nanomedicine. 2015;11(5):1253–1263. doi:10.1016/j.nano.2015.02.013
- Lo KW, Ulery BD, Ashe KM, Laurencin CT. Studies of bone morphogenetic protein-based surgical repair. Adv Drug Deliv Rev. 2012;64(12):1277–1291. doi:10.1016/j.addr.2012.03.014
- Naito Y, Terukina T, Galli S, et al. The effect of simvastatin-loaded polymeric microspheres in a critical size bone defect in the rabbit calvaria. Int J Pharm. 2014;461(1–2):157–162. doi:10.1016/j.ijpharm.2013.11.046
- Jia Z, Zhang Y, Chen YH, et al. Simvastatin prodrug micelles target fracture and improve healing. J Control Release. 2015;200:23–34. doi:10.1016/j.jconrel.2014.12.028
- Fu YC, Nie H, Ho ML, Wang CK, Wang CH. Optimized bone regeneration based on sustained release from three-dimensional fibrous PLGA/HAp composite scaffolds loaded with BMP-2. Biotechnol Bioeng. 2008;99:996–1006. doi:10.1002/bit.21648
- Lau WM, Khutoryanskiy VV. Chitosan and Its Derivatives for Application in Mucoadhesive Drug Delivery Systems. Polymers. 2018;10. doi:10.3390/polym10030267
- Sivanesan I, Gopal J, Muthu M, et al. Green Synthesized Chitosan/Chitosan Nanoforms/Nanocomposites for Drug Delivery Applications. Polymers. 2021;13(14):2256. doi:10.3390/polym13142256
- Ali A, Ahmed S. A review on chitosan and its nanocomposites in drug delivery. Int J Biol Macromol. 2018;109:273–286. doi:10.1016/j.ijbiomac.2017.12.078
- Zhuo F, Abourehab MAS, Hussain Z. Hyaluronic acid decorated tacrolimus-loaded nanoparticles: efficient approach to maximize dermal targeting and anti-dermatitis efficacy. Carbohydr Polym. 2018;197:478–489. doi:10.1016/j.carbpol.2018.06.023
- Pandey M, Choudhury H, Gunasegaran TAP, et al. Hyaluronic acid-modified betamethasone encapsulated polymeric nanoparticles: fabrication, characterisation, in vitro release kinetics, and dermal targeting. Drug Deliv Transl Res. 2019;9(2):520–533. doi:10.1007/s13346-018-0480-1
- Quinones JP, Peniche H, Peniche C. Chitosan Based Self-Assembled Nanoparticles in Drug Delivery. Polymers. 2018;10(3):235. doi:10.3390/polym10030235
- Zhao D, Yu S, Sun B, et al. Biomedical Applications of Chitosan and Its Derivative Nanoparticles. Polymers. 2018;10(4):462. doi:10.3390/polym10040462
- Hirabayashi H, Fujisaki J. Bone-specific drug delivery systems: approaches via chemical modification of bone-seeking agents. Clin Pharmacokinet. 2003;42(15):1319–1330. doi:10.2165/00003088-200342150-00002
- Stepensky D, Kleinberg L, Hoffman A. Bone as an effect compartment: models for uptake and release of drugs. Clin Pharmacokinet. 2003;42(10):863–881. doi:10.2165/00003088-200342100-00001
- Khosla S, Hofbauer LC. Osteoporosis treatment: recent developments and ongoing challenges. Lancet Diabetes Endocrinol. 2017;5(11):898–907. doi:10.1016/S2213-8587(17)30188-2
- Pierce WM, Waite LC. Bone-targeted carbonic anhydrase inhibitors: effect of a proinhibitor on bone resorption in vitro. Proc Soc Exp Biol Med. 1987;186(1):96–102. doi:10.3181/00379727-186-42590a
- Wang D, Miller SC, Kopeckova P, Kopecek J. Bone-targeting macromolecular therapeutics. Adv Drug Deliv Rev. 2005;57(7):1049–1076. doi:10.1016/j.addr.2004.12.011
- Thompson DD, Posner AS, Laughlin WS, Blumenthal NC. Comparison of bone apatite in osteoporotic and normal Eskimos. Calcif Tissue Int. 1983;35(1):392–393. doi:10.1007/BF02405064
- Hayman AR, Bune AJ, Cox TM. Widespread expression of tartrate-resistant acid phosphatase (Acp 5) in the mouse embryo. J Anat. 2000;196(Pt 3):433–441. doi:10.1046/j.1469-7580.2000.19630433.x
- Tiffee JC, Aufdemorte TB. Markers for macrophage and osteoclast lineages in giant cell lesions of the oral cavity. J Oral Maxillofac Surg. 1997;55(10):1108–1112. doi:10.1016/s0278-2391(97)90291-3
- Baron R, Neff L, Brown W, et al. Polarized secretion of lysosomal enzymes: co-distribution of cation-independent mannose-6-phosphate receptors and lysosomal enzymes along the osteoclast exocytic pathway. J Cell Biol. 1988;106(6):1863–1872. doi:10.1083/jcb.106.6.1863
- Wergedal JE, Baylink DJ. Distribution of acid and alkaline phosphatase activity in undemineralized sections of the rat tibial diaphysis. J Histochem Cytochem. 1969;17(12):799–806. doi:10.1177/17.12.799
- Wang Y. Fracture-Targeted Delivery of beta-Catenin Agonists via Peptide-Functionalized Nanoparticles Augments Fracture Healing. ACS Nano. 2017;11:9445–9458. doi:10.1021/acsnano.7b05103
- Kunin CM. The tetracyclines. Pediatr Clin North Am. 1968;15(1):43–55. doi:10.1016/s0031-3955(16)32087-9
- Da Cunha V, Davies MR, Douarre P-E, et al. Streptococcus agalactiae clones infecting humans were selected and fixed through the extensive use of tetracycline. Nat Commun. 2014;5(1):4544. doi:10.1038/ncomms5544
- Nguyen F, Starosta AL, Arenz S, et al. Tetracycline antibiotics and resistance mechanisms. Biol Chem. 2014;395(5):559–575. doi:10.1515/hsz-2013-0292
- Rall DP, Loo TL, Lane M, Kelly MG. Appearance and persistence of fluorescent material in tumor tissue after tetracycline administration. J Natl Cancer Inst. 1957;19:79–85.
- Tam CS, Anderson W. Tetracycline labeling of bone in vivo. Calcif Tissue Int. 1980;30(1):121–125. doi:10.1007/BF02408616
- Ibsen KH, Urist MR. The biochemistry and the physiology of the tetracyclines: with special reference to mineralized tissues. Clin Orthop Relat Res. 1964;32:143–169.
- Skinner HC, Nalbandian J. Tetracyclines and mineralized tissues: review and perspectives. Yale J Biol Med. 1975;48(5):377–397.
- Sanchez AR, Rogers RS, Sheridan PJ. Tetracycline and other tetracycline-derivative staining of the teeth and oral cavity. Int J Dermatol. 2004;43(10):709–715. doi:10.1111/j.1365-4632.2004.02108.x
- Que Y, Yang Y, Zafar H, Wang D. Tetracycline-grafted mPEG-PLGA micelles for bone-targeting and osteoporotic improvement. Front Pharmacol. 2022;13:993095. doi:10.3389/fphar.2022.993095
- Wang J, Tao S, Jin X, et al. Calcium Supplement by Tetracycline guided amorphous Calcium Carbonate potentiates Osteoblast promotion for Synergetic Osteoporosis Therapy. Theranostics. 2020;10(19):8591–8605. doi:10.7150/thno.45142
- Neale JR, Richter NB, Merten KE, et al. Bone selective effect of an estradiol conjugate with a novel tetracycline-derived bone-targeting agent. Bioorg Med Chem Lett. 2009;19(3):680–683. doi:10.1016/j.bmcl.2008.12.051
- Mukherjee S, Song Y, Oldfield E. NMR investigations of the static and dynamic structures of bisphosphonates on human bone: a molecular model. J Am Chem Soc. 2008;130:1264–1273. doi:10.1021/ja0759949
- Szabo CM, Martin MB, Oldfield E. An investigation of bone resorption and Dictyostelium discoideum growth inhibition by bisphosphonate drugs. J Med Chem. 2002;45:2894–2903. doi:10.1021/jm010279
- Rodan GA, Reszka AA. Bisphosphonate mechanism of action. Curr Mol Med. 2002;2(6):571–577. doi:10.2174/1566524023362104
- Cole LE, Vargo-Gogola T, Roeder RK. Targeted delivery to bone and mineral deposits using bisphosphonate ligands. Adv Drug Deliv Rev. 2016;99:12–27. doi:10.1016/j.addr.2015.10.005
- Van Acker HH, Anguille S, Willemen Y, Smits EL, Van Tendeloo VF. Bisphosphonates for cancer treatment: mechanisms of action and lessons from clinical trials. Pharmacol Ther. 2016;158:24–40. doi:10.1016/j.pharmthera.2015.11.008
- Russell RG, Watts NB, Ebetino FH, Rogers MJ. Mechanisms of action of bisphosphonates: similarities and differences and their potential influence on clinical efficacy. Osteoporos Int. 2008;19(6):733–759. doi:10.1007/s00198-007-0540-8
- Yewle JN, Puleo DA, Bachas LG. Enhanced affinity bifunctional bisphosphonates for targeted delivery of therapeutic agents to bone. Bioconjug Chem. 2011;22(12):2496–2506. doi:10.1021/bc2003132
- von Moos R, Costa L, Gonzalez-Suarez E, et al. Management of bone health in solid tumours: from bisphosphonates to a monoclonal antibody. Cancer Treat Rev. 2019;76:57–67. doi:10.1016/j.ctrv.2019.05.003
- Hoque J, Shih Y-RV, Zeng Y, et al. Bone targeting nanocarrier-assisted delivery of adenosine to combat osteoporotic bone loss. Biomaterials. 2021;273:120819. doi:10.1016/j.biomaterials.2021.120819
- Bennick A, Cannon M, Madapallimattam G. The nature of the hydroxyapatite-binding site in salivary acidic proline-rich proteins. Biochem J. 1979;183(1):115–126. doi:10.1042/bj1830115
- Butler WT. The nature and significance of osteopontin. Connect Tissue Res. 1989;23(2–3):123–136. doi:10.3109/03008208909002412
- Kasugai S, Fujisawa R, Waki Y, Miyamoto K, Ohya K. Selective Drug Delivery System to Bone: small Peptide (Asp) 6 Conjugation. J Bone Miner Res. 2000;15(5):936–943. doi:10.1359/jbmr.2000.15.5.936
- Sekido T, Sakura N, Higashi Y, et al. Novel drug delivery system to bone using acidic oligopeptide: pharmacokinetic characteristics and pharmacological potential. J Drug Target. 2001;9(2):111–121. doi:10.3109/10611860108997922
- Sun Y, Ye X, Cai M, et al. Osteoblast-Targeting-Peptide Modified Nanoparticle for siRNA/microRNA Delivery. ACS Nano. 2016;10(6):5759–5768. doi:10.1021/acsnano.5b07828
- Yokogawa K, Miya K, Sekido T, et al. Selective delivery of estradiol to bone by aspartic acid oligopeptide and its effects on ovariectomized mice. Endocrinology. 2001;142(3):1228–1233. doi:10.1210/endo.142.3.8024
- Liang C, Guo B, Wu H, et al. Aptamer-functionalized lipid nanoparticles targeting osteoblasts as a novel RNA interference-based bone anabolic strategy. Nature Med. 2015;21(3):288–294. doi:10.1038/nm.3791
- Zhang G, Guo B, Wu H, et al. A delivery system targeting bone formation surfaces to facilitate RNAi-based anabolic therapy. Nature Med. 2012;18(2):307–314. doi:10.1038/nm.2617
- Li S, Jiang H, Wang B, et al. Effect of Leptin on Marrow Adiposity in Ovariectomized Rabbits Assessed by Proton Magnetic Resonance Spectroscopy. J Comput Assist Tomogr. 2018;42(4):588–593. doi:10.1097/RCT.0000000000000725
- Beekman KM, Veldhuis-Vlug AG, den Heijer M, et al. The effect of raloxifene on bone marrow adipose tissue and bone turnover in postmenopausal women with osteoporosis. Bone. 2019;118:62–68. doi:10.1016/j.bone.2017.10.011
- Beekman KM, Zwaagstra M, Veldhuis-Vlug AG, et al. Ovariectomy increases RANKL protein expression in bone marrow adipocytes of C3H/HeJ mice. Am J Physiol Endocrinol Metab. 2019;317(6):E1050–E1054. doi:10.1152/ajpendo.00142.2019
- Yang Y, Luo X, Yan F, et al. Effect of zoledronic acid on vertebral marrow adiposity in postmenopausal osteoporosis assessed by MR spectroscopy. Skeletal Radiol. 2015;44(10):1499–1505. doi:10.1007/s00256-015-2200-y
- Yang Y, Luo X, Xie X, et al. Influences of teriparatide administration on marrow fat content in postmenopausal osteopenic women using MR spectroscopy. Climacteric. 2016;19(3):285–291. doi:10.3109/13697137.2015.1126576
- Li J, Chen X, Lu L, Yu X. The relationship between bone marrow adipose tissue and bone metabolism in postmenopausal osteoporosis. Cytokine Growth Factor Rev. 2020;52:88–98. doi:10.1016/j.cytogfr.2020.02.003
- Adjei IM, Sharma B, Peetla C, Labhasetwar V. Inhibition of bone loss with surface-modulated, drug-loaded nanoparticles in an intraosseous model of prostate cancer. J Control Release. 2016;232:83–92. doi:10.1016/j.jconrel.2016.04.019
- Song H, Li X, Zhao Z, et al. Reversal of Osteoporotic Activity by Endothelial Cell-Secreted Bone Targeting and Biocompatible Exosomes. Nano Lett. 2019;19(5):3040–3048. doi:10.1021/acs.nanolett.9b00287
- Mann AP, Tanaka T, Somasunderam A, et al. E-selectin-targeted porous silicon particle for nanoparticle delivery to the bone marrow. Adv Mater. 2011;23(36):H278–282. doi:10.1002/adma.201101541
- Sou K, Goins B, Takeoka S, Tsuchida E, Phillips WT. Selective uptake of surface-modified phospholipid vesicles by bone marrow macrophages in vivo. Biomaterials. 2007;28(16):2655–2666. doi:10.1016/j.biomaterials.2007.01.041
- Sou K, Goins B, Leland MM, Tsuchida E, Phillips WT. Bone marrow-targeted liposomal carriers: a feasibility study in nonhuman primates. Nanomedicine (Lond). 2010;5(1):41–49. doi:10.2217/nnm.09.78
- Guo J, Wang F, Hu Y, et al. Exosome-based bone-targeting drug delivery alleviates impaired osteoblastic bone formation and bone loss in inflammatory bowel diseases. Cell Rep Med. 2023;4(1):100881. doi:10.1016/j.xcrm.2022.100881
- Xing X, Tang Q, Zou J, et al. Bone-targeted delivery of senolytics to eliminate senescent cells increases bone formation in senile osteoporosis. Acta Biomater. 2023;157:352–366. doi:10.1016/j.actbio.2022.11.056
- Ren M, Li Y, Zhang H, et al. An oligopeptide/aptamer-conjugated dendrimer-based nanocarrier for dual-targeting delivery to bone. J Mat Chem B. 2021;9(12):2831–2844. doi:10.1039/D0TB02926B