?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
The potential of gold nanoparticles (GNPs) as radiosensitizers for the treatment of malignant tumors has been limited by the large quantities of GNPs that must be administered and the requirement for low-energy X-ray irradiation to optimize radiosensitization. In this study, we enhance the radiosensitivity of HCT116 human colorectal cells with tiopronin-coated GNPs (Tio-GNPs) combined with a low-energy X-ray (26 keV effective energy) source, similar to the Papillon 50 clinical irradiator used for topical irradiation of rectal tumors. Sensitizer enhancement ratios of 1.48 and 1.69 were measured in vitro, when the HCT116 cells were incubated with 0.1 mg/mL and 0.25 mg/mL of Tio-GNPs, respectively. In nude mice bearing the HCT116 tumor, intra-tumoral (IT) injection of Tio-GNPs allowed a 94 times higher quantity of Tio-GNPs to accumulate than was possible by intravenous injection and facilitated a significant tumor response. The time following irradiation, for tumors growing to four times their initial tumor volume (4Td) was 54 days for the IT injection of 366.3 μg of Tio-GNPs plus 10 Gy, compared to 37 days with radiation alone (P=0.0018). Conversely, no significant improvement was obtained when GNPs were injected intravenously before tumor irradiation (P=0.6547). In conclusion, IT injection of Tio-GNPs combined with low-energy X-rays can significantly reduce the growth of colorectal tumors.
Introduction
High-Z nanomaterials have gained much attention for the radiation dose enhancement properties associated with their strong absorption of ionizing radiation and propensity to generate copious amounts of secondary electrons. In the past decade, while a substantial number of studies have investigated radiosensitization by gold nanoparticles (GNPs) in vitro, little has been published on their radiosensitizing properties in vivo.Citation1–Citation10 Tumor growth retardation or improvements in animal survival were observed only at very high doses of GNPs (∼2 g/kg) administered intravenously (IV) prior to tumor irradiation.Citation5,Citation8 With much lower doses, ie, 13.5 mg of GNPs injected IV, no tumor growth retardation was measured in mice bearing murine mammary carcinoma.Citation9
The need to treat with such high doses of GNP renders problematic transition from animal studies into the clinic. Moreover, GNPs injected IV accumulate largely in liver and kidneys and when administered orally accumulate mostly in spleen, liver, stomach, small intestine, and kidneys.Citation11,Citation12 Studies of acute toxicity, particularly liver toxicity, indicate that to be nontoxic the size of GNPs should be controlled to be smaller than 4.8 nm.Citation13–Citation16 It is also unclear whether GNPs can cause long-term adverse effects, since no such study has been performed. Moreover, since GNPs are expensive, patients’ treatment costs are another factor that must be considered. Considering these aspects, it is thus appropriate to ask whether it is possible to decrease the dose of GNPs and retain their radiosensitizing effect.
To overcome these obstacles, Bobyk et alCitation10 injected GNPs directly into the F98 glioma tumor implanted in the brain of Fischer rats by intra-tumoral (IT) convection-enhanced delivery (CED). This procedure increased the tumoral uptake of GNPs, and consequently only 250 μg per rat (0.96–1.14 mg GNPs per kg) was necessary to significantly improve animal survival. The optimal radiosensitizing effect of GNPs in soft tissue is expected to be observed with an X-ray irradiation energy of ∼80 keV.Citation17 However, the mean free path of 80 keV photons is <35 mm, which is too short to treat efficiently most brain tumors in humans.Citation5 Nevertheless, the work of Bobyk et alCitation10 clearly showed that, for superficial tumors, efficient radiosensitization can be achieved by combining GNPs with low-energy X-ray irradiation.
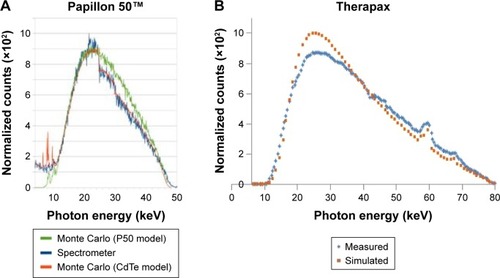
The current study explores the treatment with GNPs of colorectal cancers, which are the fourth most common cancer and the second most common cause of cancer death.Citation18 In its early stage, colorectal cancer can be treated by topical irradiation with the Papillon 50 irradiator. However, topical X-ray therapy alone may not be sufficient, since the long-term control of patients is 90% for T1N0 stage, 80% for T2N0 stage, and only 50% for early T3 stage.Citation19 The mean energy of this X-ray source is 26.5 keV, and the maximum energy is 50 keV, which provides a 50% depth of the absorbed dose at ∼6.5–7 mm.Citation19 To further increase the efficiency of the Papillon 50 technique, we propose to combine it with the endoscopic IT injection of GNPs.Citation20–Citation23 In the current study, male nu/nu mice bearing HCT116 human colorectal tumor were treated by IT injection of tiopronin-coated GNPs (Tio-GNPs) and then irradiated with an X-ray source, which has a similar energy spectrum compared to that of the Papillon 50 X-ray unit ().Citation24,Citation25
Figure 1 Comparison between the X-ray beam spectra from a Papillon 50 system used for the treatment of colorectal cancer and the Therapax source used in this study.
Notes: (A) Papillon 50 X-ray beam spectra simulated with PENELOPE for the Papillon 50 geometry (green curve), simulated with Papillon 50 geometry including the CdTe detector geometry (red curve), and measured using CdTe detector (blue curve) (modified from Radiat Phys Chem, 81/6, Croce O, Hachem S, Franchisseur E, Marcie S, Gerard J, Bordy J, Contact radiotherapy using a 50 kV X-ray system: Evaluation of relative dose distribution with the Monte Carlo code PENELOPE and comparison with measurements., 609–617, Copyright (2012), with permission from Elsevier.Citation25). (B) Therapax SXT 150 X-ray beam spectra simulated with SpectrumGUI software and measured using CdTe detector for beam effective energies of 26 keV (modified from Lessard et al.Citation24).
Abbreviation: CdTe, cadmium telluride.
The ligand that coats the GNP must be carefully chosen. Long ligands can attenuate the low-energy photoelectrons emitted from the GNPs after radiation, which could then lead to a considerable decrease in any radioenhancement effect.Citation26 The short ligand citrate is frequently used to prepare citrate-coated GNPs.Citation7,Citation27 However, such GNPs will aggregate in solution when their concentration exceeds only a few 100 μg/mL. Since only a small volume of GNPs-containing solution can be injected IT, this tendency to aggregate prevents high concentrations of GNPs from reaching the tumor. To overcome these limitations, Tio-GNPs were chosen because 1) the short length of the tiopronin ligand (9.15 Å, calculated by Accelrys Materials Studio) minimizes absorption in the coating of photoelectrons emitted from the gold and 2) their higher stability against aggregation permits the use of higher GNP concentrations.Citation28 Radiosensitization by Tio-GNPs was first assessed in vitro in HCT116 human colorectal cancer cells, and the induction of double-strand breaks (DSBs) was measured. The antitumor potential of Tio-GNPs was then studied in HCT116 human colorectal tumor-bearing nude mice.
Materials and methods
Preparation of Tio-GNPs
Tio-GNPs were prepared as described by Templeton et al.Citation28 Briefly, 0.1033 g (0.27 mmol, 1 equiv) of gold(III) chloride trihydrate and 0.1267 g (0.80 mmol, 3 equiv) of tiopronin (Sigma-Aldrich Co., St Louis, MO, USA) were codis-solved in 11.67 mL of 6:1 methanol:acetic acid. Then, 0.2 g (5.33 mmol, 20 equiv) of sodium borohydride (Sigma-Aldrich Co.) was added and stirred for 45 minutes. Next, the solvent was removed under vacuum and purified by dialysis for 72 hours (Spectra/Por CE, MWCO 10 000; Spectrum® Laboratories, Inc., Rancho Dominguez, CA, USA). Tio-GNPs were lyophilized and stored at room temperature until being used. GNPs concentrations were measured by inductively coupled plasma mass spectrometry (ICP-MS, ELAN DRC-II; PerkinElmer Inc., Waltham, MA, USA).
Cellular uptake of Tio-GNPs
HCT116 cells at 70% confluence were incubated with 0.25 mg/mL of Tio-GNPs in minimum essential medium (MEM) without fetal bovine serum for 4–48 hours. Cells were washed twice with phosphate-buffered saline (PBS), trypsinized, and counted. Then, the cells were digested in 2 mL of 30% hydrogen peroxide and 2 mL of 70% nitric acid, and the concentration of gold was determined by ICP-MS analysis.Citation29
Subcellular localization of Tio-GNPs
HCT116 cells were incubated with 0.25 mg/mL of Tio-GNPs for 24 hours, and then rinsed with 0.1 M phosphate buffer, fixed with ice-cold 2% paraformaldehyde for 20 minutes, and washed twice with 0.1 M phosphate buffer. The samples were kept in 0.2 M citrate buffer, pH 7.4. To detect GNPs with more efficiency, their size was increased using the protocol of Silver Enhancer Kit for Microscopy (Cytodiagnostics, Burlington, ON, Canada).Citation30 Afterward, the cells were washed twice with citrate buffer, rinsed with 0.1 M phosphate buffer, and stained with 1% osmium tetroxide for 90 minutes. The samples were then dehydrated with increasing ethanol concentrations and covered with Epon 812 resin mixture (Electron Microscopy Sciences, Hornby, ON, Canada) twice within 3 hours. The resin was allowed to polymerize at 60°C for 48 hours. Sections of 80 nm were prepared using a Leica Ultracut UCT Ultramicrotome (Leica Microsystems, Wetzlar, Germany), contrasted with uranyl acetate (Electron Microscopy Sciences), and visualized under Hitachi H-7500 transmission electron spectroscope.
Cytotoxicity of Tio-GNPs assessed with a clonogenic assay
Clonogenic assay was performed as described by Tippayamontri et alCitation31 with some modifications. Briefly, 1,000 HCT116 cells were plated in 100 mm Petri dishes for 24 hours. For the group receiving only radiation, doses ranging from 1 Gy to10 Gy of X-rays were delivered to the cells. The X-ray source was operated at 4 mA, 80 kV, with an average energy of 26 keV (Pantak Therapax 3 series). For the group treated only with Tio-GNPs, increasing concentrations of Tio-GNPs were incubated with the HCT116 cells for 24 hours. The combination of Tio-GNPs plus radiation was performed by adding either 0.1 mg/mL or 0.25 mg/mL of Tio-GNPs to the MEM without fetal bovine serum for 24 hours and then irradiating (with 1–10 Gy). During the 7-day incubation, the MEM was not renewed to prevent the detachment of cells from colonies that might then produce new colonies leading to erroneous results. After 7 days of incubation in completed MEM, colonies were fixed, stained, and counted.
Analysis of DNA DSBs by immunofluorescence assay for γH2A.X
HCT116 cells were plated on coverslips and then treated 24 hours later with either 0.25 mg/mL of GNPs alone, 2 Gy alone, or 0.25 mg/mL of GNPs plus 2 Gy radiation. One hour after treatment, cells were fixed in 4% paraformaldehyde, permeabilized by 0.1% of Triton X-100, quenched by 1 mM glycine, and blocked by 10% dried powdered milk in PBS. Then, primary antibody phospho-histone H2A.X (Ser139) (20E3) rabbit mAb (Cell Signaling Technology, Inc. Beverly, MA, USA) 1:400 in 10% dried powdered milk in PBS was incubated with cells overnight at 4°C. Afterward secondary antibody anti-rabbit IgG (H + L), F(ab′)2 fragment (Alexa Fluor® 488 Conjugate; Cell Signaling Technology, Inc.) 1:1,000 in 10% dried powdered milk in PBS was incubated with cells for 2 hours in a humidified chamber, followed by the incubation of 286 nM 4′,6-diamidino-2-phenylindole at room temperature for 15 minutes. Then, the cells were rinsed and viewed under an Olympus FLUOVIEW FV1000 confocal laser scanning microscope (Olympus Corporation, Tokyo, Japan). Foci were counted by ImageJ.Citation32
Animal model
Male nu/nu nude mice at the age of 4–6 weeks were purchased from Charles River Laboratory (Saint-Constant, QC, Canada). HCT116 cells (2×106/100 μL MEM) were inoculated subcutaneously into each rear flank. Tumor size was first measured once tumors reached a volume of ∼100 mm3, and subsequently, continued twice weekly. Tumor volumes were calculated with the following formula:
Antitumor effect
Mice were randomized into six groups (IV Tio-GNPs, IV Tio-GNPs + radiation therapy (RT), IT Tio-GNPs, IT Tio-GNPs + RT, IT PBS, and IT PBS + RT) with minimum of five mice per group. Tio-GNPs were delivered either IV (732.6 μg/10 μL) or IT (366.3 μg/10 μL in each tumor). A radiation dose of 10 Gy was delivered 8 hours later with the X-ray unit at an effective energy of 26 keV. The tumor was placed in the center of a 1 cm-diameter X-ray applicator.
Tumor uptake of Tio-GNPs
Once tumor volumes reached 100 mm3, Tio-GNPs were injected in mice bearing two tumors, either IV at its maximal relevant concentration (732.6 μg/10 μL) or IT at 366.3 μg/10 μL into each tumor. Eight hours later, the mice were euthanized, tumors were extracted, weighed, digested, and the amounts of gold were determined by ICP-MS analysis.
Statistical analysis
From survival fraction curves, sensitizer enhancement ratio (SER) was calculated by dividing the area under the curve, which represents mean inactivation dose of the radiation group, by results of the radiation plus Tio-GNPs group.Citation33 For the in vivo study, the time required for the tumor volume to increase by a factor 4 (4Td) was chosen as a defining characteristic of each experiment. They were plotted by Kaplan–Meier curve, and log-rank test to analyze the differences between groups. One-way ANOVA was performed to analyze the cellular uptake of Tio-GNPs at different incubation times and the number of γH2A.X foci. Two-way ANOVA was performed to analyze the cell survival obtained by clonogenic assays. Unpaired t-test was performed to analyze the tumor uptakes of Tio-GNPs. All of statistical analyses were performed using Graphpad Prism 6 (GraphPad Software, Inc., La Jolla, CA, USA) except for the in vitro survival fraction curve, which was fitted by Origin-Pro 2015 using a Levenberg–Marquardt iteration algorithm with unequal weighting of each data point (OriginLab Corp., Northampton, MA, USA). P<0.05 was considered significantly different. Clonogenic assays were performed in triplicate, three times. For the in vivo tumor growth study, a minimum of five tumors were followed. All other studies were carried out in triplicates.
Results
Characterization of Tio-GNPs
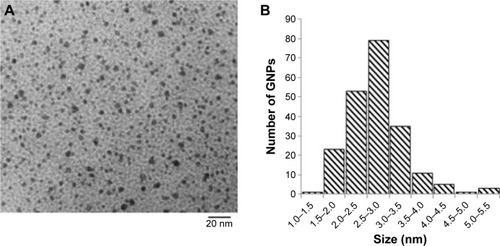
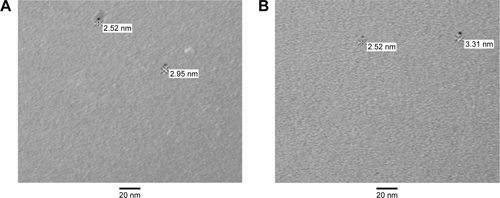
Tio-GNPs dissolved in water were dried on transmission electron microscopy grids and visualized under transmission electron microscopy to determine the distribution of their diameters (). Diameters ranged from 1.21 nm to 5.41 nm, for a mean diameter of 2.77±0.69 nm (). The size of Tio-GNPs remained constant when remeasured in the MEM at concentrations of 0.1 mg/mL and 0.25 mg/mL ().
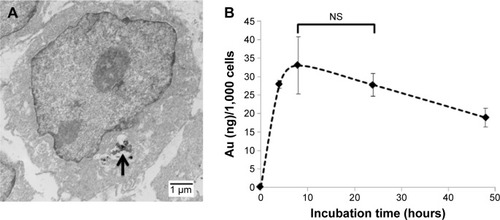
Localization and uptake of Tio-GNPs in HCT116 cells
All Tio-GNPs were located in the cytoplasm and appeared in vesicle-like structures, suggesting that Tio-GNPs are taken up by cells through an endocytosis-dependent mechanism ().Citation34 The cellular uptake of Tio-GNPs increased to a maximum at 8 hours (33±7.7 ng Au/1,000 cells), then gradually decreased to reach significantly lower concentration at 48 hours (). An 8-hour interval between the introduction of Tio-GNPs and radiation was then chosen in subsequent in vitro assays.
Figure 3 Subcellular localization and cellular uptake of Tio-GNPs.
Notes: (A) TEM image of subcellular localization of Tio-GNPs in HCT116 cells. Tio-GNPs in the cytoplasm were located in vesicles (black arrow). HCT-116 cells were incubated with 0.25 mg/mL of Tio-GNPs for 24 hours. Tio-GNPs were visualized using silver enhancement under TEM (scale bar =1 μm). (B) The uptake of GNPs in HCT116 cells after different times of incubation (0 hour, 4 hours, 8 hours, 24 hours, and 48 hours). HCT116 cells were incubated with 0.25 mg/mL of GNPs. Data are expressed as mean ± SEM. A significant increase in cellular uptake was measured compared to control, at 8 hours, 24 hours, and 48 hours after incubation (One-way ANOVA, 4 hours, P<0.01; 8 hours, P<0.001; 24 hours, P<0.01; 48 hours, P<0.05). No significant differences were found after 8 hours and 24 hours of incubation (P>0.05). Magnification: 3,500×.
Abbreviations: NS, not significant; SEM, standard error of the mean; TEM, transmission electron microscopy; Tio-GNPs, tiopronin-coated gold nanoparticles.
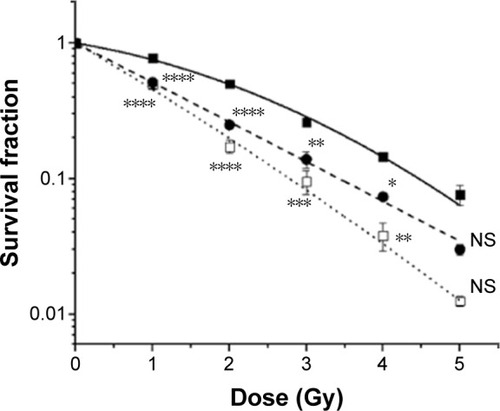
In vitro radiosensitization of HCT116 cells by Tio-GNPs
Clonogenic assays were performed to determine the radioenhancement induced by Tio-GNPs in HCT116 cells (). Tio-GNPs alone were not toxic at the concentrations used. A significant reduction in cell survival was found when Tio-GNPs were combined with 1–4 Gy of radiation. Tio-GNPs incubated at 0.1 mg/mL and 0.25 mg/mL resulted in an SER of 1.48 and 1.69, respectively.
Figure 4 Survival curve of HCT116 cells treated with (■) radiation alone (SF = e(−0.217D−0.067D2), adjusted R2=0.9986, 50% cell survival, LD50 =1.98 Gy), (●) Tio-GNPs 0.1 mg/mL + radiation (SF = e(−0.669D−0.001D2), adjusted R2=0.9881, LD50 =1.03 Gy), and (□) Tio-GNPs 0.25 mg/mL + radiation (SF = e(−0.767D−0.022D2), adjusted R2=0.9943, LD50 =0.88 Gy).
Notes: Results are in response to a Two-way ANOVA. *Significant at P<0.05, **significant at P<0.01, ***significant at P<0.001, ****significant at P<0.0001.
Abbreviations: D, dose; NS, not significant; SF, survival fraction; Tio-GNPs, tiopronin-coated gold nanoparticles.
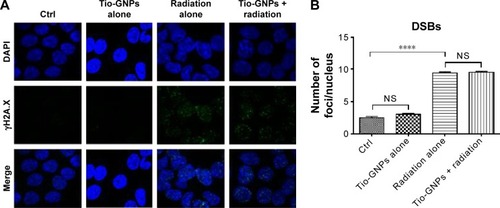
Assessment of DSBs in HCT116 cells
The level of the DSBs marker, γH2A.X, was measured to determine whether the dose-enhancing effect of Tio-GNPs was associated with an increase in this type of DNA lesion in HCT116 cells (). No significant induction of γH2A.X was found when Tio-GNPs at 0.25 mg/mL were incubated without irradiation. As expected, when the HCT116 cells were exposed to 2 Gy, the number of γH2A.X increased by 3.8-fold compared to the untreated cells (control group: 2.51±0.19, n=397; 2 Gy: 9.44±0.170, n=672; P<0.0001), consistent with DSB induction being associated with a reduction in cell survival. However, combining Tio-GNPs with radiation did not correlate with a greater induction of this type of DNA damage (2 Gy: 9.44±0.17, n=672; Tio-GNPs +2 Gy: 9.53±0.16, n=842; P=0.7).
Figure 5 γH2A.X immunofluorescence study in HCT116 cells.
Notes: (A) γH2A.X immunofluorescence from DSBs induced by different treatments. (B) γH2A.X foci of control, Tio-GNPs alone, X-ray alone, and Tio-GNPs + X-ray. Two-way ANOVA was performed to analyze the difference between groups. Results are in response to a One-way ANOVA. ****Significant at P<0.0001.
Abbreviations: DSBs, double-strand breaks; NS, not significant; Tio-GNPs, tiopronin-coated gold nanoparticles.
Radioenhancement by Tio-GNPs of HCT116 tumor implanted in nude mice
The relative efficiency of Tio-GNPs injected IV and IT to increase the radiosensitization was assessed in nude mice implanted with a HCT116 tumor (). Tumor growth after IV or IT injection with Tio-GNPs was similar to that of implanted tumors in untreated animals (IT Tio-GNPs vs control, P=0.3755; IV Tio-GNPs vs control, P=0.1106). These results indicate that Tio-GNPs were not toxic under the current experimental conditions.
Figure 6 In vivo study of tumor growth delay after different treatments and tumor uptake of Tio-GNPs measured after IV or IT injection.
Notes: (A) The tumor growth delay after the initial treatment of nude mice bearing HCT116 colorectal tumor with IT PBS, IT Tio-GNPs, IT PBS plus radiation, IT Tio-GNPs plus radiation, and IV Tio-GNPs plus radiation. Tumor growth delay is reported as Vt/V0 ratio, where Vt is the mean tumor volume on a given day during the treatment and V0 is the mean tumor volume at the beginning of the treatment. Each symbol represents the mean ± SEM of the results obtained with at least five tumors. (B) Kaplan–Meier curve of mice whose tumors have reached the 4Td. An event is defined as the tumor size reached four times of its original size (4Td), (n=5) (C) Tumor uptake of Tio-GNPs at 8 hours after IT or IV after injecting 20 μL at a concentration of 36.63 mg/mL of Tio-GNPs/rat. Unpaired t-test was performed to analyze the difference between tumor uptake of Tio-GNPs by IT and IV injection. Results are in response to a log-rank test. *Significant at P<0.05, **Significant at P<0.01.
Abbreviations: IT, intra-tumoral; IV, intravenous; NS, not significant; PBS, phosphate-buffered saline; Tio-GNPs, tiopronin-coated gold nanoparticles; SEM, standard error of the mean.
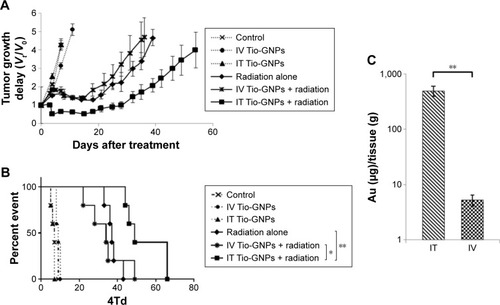
An irradiation with 10 Gy significantly reduced the tumor growth. The time required to increase by fourfold the initial tumor volume (4Td) was 37 days, ie, 30 days longer than the untreated tumor that reached the 4Td at a median time of only 7 days. When tumors were injected IV with Tio-GNPs and then irradiated 8 hours later, tumor growth was not significantly slower than that seen for the radiation-alone group (median 4Td of 32 days, P=0.6547). A significant radiosensitization was obtained only with IT injection of Tio-GNPs. The tumor growth retardation was then significantly greater (4Td =54 days) than that seen in the radiation-alone group (P=0.0018) or when Tio-GNPs were injected IV plus radiation (P=0.038).
Tumor uptake of Tio-GNPs
The tumor uptake of Tio-GNPs obtained after IV and IT injections was measured at 8 hours. As expected, a significant higher tumor uptake of Tio-GNPs was achieved by IT injection (496±106 μg Au/tissue [g]) than by IV injection (5.27±1.17 μg Au/g; ).
Discussion
A decade ago, Hainfeld et alCitation8 presented the first animal studies using GNPs as an agent capable of enhancing the radiation dose locally. In the intervening years, the biological effects of different sizes, coatings, and concentrations of GNPs, as well as different methods of delivery and radiation energies, have been investigated.Citation6–Citation8,Citation10,Citation15,Citation33,Citation35 In the current study, we carefully chose appropriate experimental parameters based on the previous results: 2.77 nm Tio-GNPs coated with tiopronin which were delivered via the IT route to mice bearing HCT116 colorectal tumors before irradiation with 26 keV effective energy X-rays.
The tiopronin molecule has a length of ∼9.15 Å. GNPs coated with this short ligand are expected to permit a larger number of damaging low-energy electrons to traverse the coating than would occur with GNPs coated with longer molecules. Low-energy electrons have short thermalization distances, and thus their transmission through the coating is dependent on the length of the ligand.Citation26 In the study by Xiao et al, four types of GNPs having ligands of different lengths were dried on DNA films and irradiated with 60 keV electrons. The yields of DNA single-strand breaks and DSBs induced by radiation were found to be roughly inversely proportional to the length of ligands. The DSB yields induced by radiation in the absence or presence of GNPs coated with dithiolated diethylenetriamine pentaacetic acid (DTDTPA) or DTDTPA-Gd were the same. In contrast, irradiation of DNA in the presence of naked GNPs doubled the DSB yields relative to radiation alone.Citation26 The concept that some coatings are too thick to allow radiosensitization by photoelectrons is also consistent with the results of Hébert et al,Citation9 in which no median survival improvement was observed for irradiation with 150 kVp 20 minutes after IV injection of 0.675 g/kg DTDTPA-Gd-coated GNPs into mice bearing MC7-L1 murine mammary ductal carcinomas. However, in this latter case, factors other than GNP coating cannot be excluded. In a Monte Carlo simulation study, it was demonstrated that following a single ionizing event from 40 keV primary radiation, 2 nm GNPs deposit a larger dose per gold atoms in the vicinity of the nanoparticle than do larger GNPs. This implies that Tio-GNPs of ∼2 nm are more effective in inducing a radioenhancement than larger Tio-GNPs.Citation36 This result may be explained by the fact that in larger GNPs, it is more likely that Au photoelectrons within the nanoparticle will be inelastically scattered to energies below the vacuum level and thus more likely to stay within the GNP. Inelastically scattered photoelectrons that do escape the GNP core will likely have reduced energy, which further decreases their chances to escape the tiopronin layer. Such computational results are also supported by the work of Misawa and Takahashi,Citation37 which studied 5–250 nm-diameter GNPs and demonstrated a higher production of reactive oxygen species with smaller size of GNPs. However, Chithrani et alCitation7 demonstrated that among GNPs of diameters 14 nm, 50 nm, and 74 nm, the 50 nm GNPs exhibited the highest radiation enhancement factor, but this was likely due to the higher cellular uptake of the latter GNPs. Similarly, Zhang et alCitation15 showed that 12.1 nm GNPs provided a better tumor growth control compared to the 4.8 nm, 27.3 nm, and 46.6 nm GNPs because of the higher tumor accumulation of the 12.1 nm GNPs when delivered IV. These points, particularly the Monte Carlo simulation and the reactive oxygen species generation studies, justify our choice of the small 2.77 nm Tio-GNPs to produce a high local radioenhancement.
Significantly, Tio-GNPs can be produced at very high concentrations. This is an essential factor when applying GNPs to in vivo studies. Indeed, previous studies have shown that large quantities of GNPsCitation5,Citation8–Citation10 were necessary to achieve observable CED radioenhancementCitation10 in glioma-bearing Fischer rats. In this latter study, two doses of GNPs were investigated: 125 μg and 250 μg. The high dose group demonstrated an increased median survival time of 41 days compared to the 35 days of the radiation-alone group (P=0.05), while the low-dose group did not show a significant improvement (P=0.47).
In our in vitro cytotoxicity study, a higher radioenhancement (SER of 1.69) was produced with a dose of 0.25 mg/mL of Tio-GNPs than was obtained with a dose of 0.1 mg/mL (SER of 1.48). The yield of DSBs was studied to better identify the mechanisms of radioenhancement. We found that DSB damage did not increase for the GNPs plus radiation group relative to the radiation-alone group. Therefore, this radioenhancement is not related to an increase in DSB damage, but rather to the localization of Tio-GNPs in the cytoplasm (presumably by endocytosis, and the formation of endocytotic vesicles), which is shown in . This result supports the hypothesis that radiosensitization can occur without the induction of additional DSBs. Our results are also in accordance with the previous work of Jain et al,Citation33 who observed that GNPs enhanced the efficiency of radiotherapy without causing additional DNA damage. Other possible mechanisms such as changes in biological pathways and targeting of hypoxic cells were proposed.
Our in vivo study compares the tumor uptake of GNPs via IV injection to that via IT injection, with tumor growth retardation upon combination with radiation. At 8 hours postinjection, it is clearly shown that for equal quantities of GNPs, IV injection was not able to attain as high a tumor concentration as did IT injection. This is consistent with our results indicating that growth retardation is greater with IT delivery. Furthermore, the IT injection of 366.3 μg of GNPs required to observe radiosensitization agrees well with the value of 250 μg used in the experiments of Bobyk et al.Citation10 These results support the view that the maximum quantity of GNPs that can be delivered IV is not sufficient to reach a concentration in the tumor that could significantly improve the radiosensitivity of HCT116 human colorectal tumor. GNPs can significantly increase radiosensitivity, but only when they accumulate at the high levels obtainable with IT injection.
Other than GNPs, nanomaterials such as hafnium nano-particles, gadolinium nanoparticles, and titanium nano-particles are also candidate radiosensitizers, each having their own advantages.Citation38 Hafnium oxide nanoparticles are more chemically inert than GNPs and have shown a major radioenhancement effect under Cobalt-60 source activation in HT1080 and A673 mesenchymal tumors and in HCT116 human colorectal tumor xenografted in nude mice.Citation39 In that study with HCT116 tumor, IT injection of nanoparticles plus 8 Gy gamma radiation suppressed tumor growth in the measured 25 days, while treatment with radiation alone showed less suppression. In our study with Tio-GNPs, tumors remained at their original size for up to 28 days after treatment. Townley et alCitation40 studied rare earth-doped titania nano-particles designed to possess a broader absorption spectrum to better match with that produced by the X-ray source. In their experiments, the size of A549 lung adenocarcinoma in mice treated with an IT injection of 1 mg/kg of nanoparticles plus 200 kV X-ray radiation was at 22 days, approximately half the size of tumors in mice that received radiation alone. In this study, we obtained similar results with the Tio-GNPs; at 21 days post irradiation, tumor size was also approximately half that of the radiation-alone group. Le Duc et alCitation41 studied gadolinium-based nanoparticles in 9 L gliosarcoma-bearing mice; with irradiation 20 minutes after IV injection of 40 mM of nanoparticles, median survival time increased from 47 days in the radiation-alone group to 90 days. These nanoparticles can also be followed by magnetic resonance imaging.
Although similar radiosensitization effects and efficiencies have thus been reported in the literature for a variety of nanoparticles, due to the diverse nature of the experimental procedures and parameters (eg, animal model, efficacy evaluation method, radiation dose, and energy) it is not really possible to conclude which nanomaterial is superior as regards the radiosensitization efficiency. In theory, however, from among the abovementioned materials, gold almost always has the highest mass attenuation coefficient for X-rays in the 3 keV to MeV range. Assuming similar numbers of secondary electrons emitted per unit of photon energy absorbed, then for the abovementioned nanomaterials, the radiosensitization efficiency of GNPs may be expected to be the highest.Citation17,Citation42
In the clinic, chemotherapeutic drugs are currently administered by CED. However, the endoscopic injection of therapeutic agents has only been applied in treating vesicoureteral reflux, esophageal tumor, and gastric cancer.Citation20–Citation23 It is therefore conceivable that upon further development, this route of injection could be applied to the direct injection of GNPs into early-stage colorectal tumors. Low-energy photons are necessary to reach maximum radioenhancement by GNPs,Citation5,Citation8–Citation10,Citation17 but, in practice, treatments with such radiation are problematic. Owing to their limited penetration depth in soft tissue, low-energy photons are only used in the clinic for a small number of diseases located at or near the surface of the body, such as melanomas, and it is very difficult to translate their use to most other cancer treatments. However, colorectal cancer could benefit from such a treatment. Certain colorectal cancers, dependent on stage, location, and age of the patient, can be treated by contact X-ray radiotherapy using the 50 kV X-ray Papillon 50 technique, which introduces an X-ray applicator inside the rectum to deliver high-dose radiation directly to colorectal tumors. Depending on the tumor, node, and metastasis stage of the tumor, patients will receive three fractions of a total dose of 50 Gy for T1 patients, or higher if the tumor staging is higher.Citation19 The energy spectrum of the Papillon 50 X-rays is similar to that of the X-ray source used in our study (). In the clinic, the long-term control of T1N0 stage is 90% and that of T2N0 is 80%, but it is only 50% for early T3.Citation19 Based on our results, these numbers could be improved if GNPs were delivered by endoscopic IT injection to the tumor before irradiation.
Conclusion
IT injection of small Tio-GNPs, combined with an X-ray beam at an effective energy of 26 keV, can significantly reduce the growth of a colorectal tumor in a preclinical model.
Acknowledgments
We would like to thank Doctor AD Bass for helpful suggestions and corrections, François Lessard for providing the original data of the Therapax SXT 150 X-ray beam spectra, Doctor J Constanzo for the technical support in foci counting, and the Electron Microscopy and Histology Research Core of the Faculty of Medicine and Health Science at the Université de Sherbrooke for their electron microscopy services. This work was supported by the Canadian Institutes of Health Research (grant # PPP-122899). Louis Gendron, Brigitte Guérin, Léon Sanche, and Benoit Paquette are members of the Centre de Recherche du CHUS supported by the Fonds de la Recherche du Québec – Santé.
Supplementary material
Figure S1 Tio-GNPs in MEM at concentrations of 0.1 mg/mL (A) and 0.25 mg/mL (B) without FBS were visualized under TEM.
Notes: Magnification of S1A and B: 100,000×.
Abbreviations: FBS, fetal bovine serum; MEM, minimum essential medium; TEM, transmission electron microscopy; Tio-GNPs, tiopronin-coated gold nanoparticles.
Disclosure
The authors report no conflicts of interest in this work.
References
- ChienCCWangCHHuaTESynchrotron X-ray synthesized gold nanoparticles for tumor therapyAIP Conf Proc200787919081911
- KongTZengJWangXEnhancement of radiation cytotoxicity in breast-cancer cells by localized attachment of gold nanoparticlesSmall2008491537154318712753
- ZhangXXingJZChenJEnhanced radiation sensitivity in prostate cancer by gold-nanoparticlesClin Invest Med2008313E160E16718544279
- RoaWZhangXGuoLGold nanoparticle sensitize radiotherapy of prostate cancer cells by regulation of the cell cycleNanotechnology2009203737510119706948
- HainfeldJFDilmanianFAZhongZSlatkinDNKalef-EzraJASmilowitzHMGold nanoparticles enhance the radiation therapy of a murine squamous cell carcinomaPhys Med Biol201055113045305920463371
- LiuCJWangCHChenSTEnhancement of cell radiation sensitivity by pegylated gold nanoparticlesPhys Med Biol201055493194520090183
- ChithraniDBJelvehSJalaliFGold nanoparticles as radiation sensitizers in cancer therapyRadiat Res2010173671972820518651
- HainfeldJFSlatkinDNSmilowitzHMThe use of gold nanoparticles to enhance radiotherapy in micePhys Med Biol20044918N309N31515509078
- HébertEMDebouttièrePJLepageMSancheLHuntingDJPreferential tumour accumulation of gold nanoparticles, visualised by magnetic resonance imaging: radiosensitisation studies in vivo and in vitroInt J Radiat Biol201086869270020586540
- BobykLEdouardMDemanPPhotoactivation of gold nano-particles for glioma treatmentNanomedicine2013971089109723643529
- KhlebtsovNDykmanLBiodistribution and toxicity of engineered gold nanoparticles: a review of in vitro and in vivo studiesChem Soc Rev20114031647167121082078
- HillyerJFAlbrechtRMGastrointestinal persorption and tissue distribution of differently sized colloidal gold nanoparticlesJ Pharm Sci200190121927193611745751
- AlkilanyAMMurphyCJToxicity and cellular uptake of gold nano-particles: what we have learned so far?J Nanopart Res20101272313233321170131
- ChoWSChoMJeongJAcute toxicity and pharmacokinetics of 13 nm-sized PEG-coated gold nanoparticlesToxicol Appl Pharmacol20092361162419162059
- ZhangXDWuDShenXSize-dependent radiosensitization of PEG-coated gold nanoparticles for cancer radiation therapyBiomaterials201233276408641922681980
- ChenYSHungYCLiauIHuangGSAssessment of the in vivo toxicity of gold nanoparticlesNanoscale Res Lett20094885886420596373
- HainfeldJFDilmanianFASlatkinDNSmilowitzHMRadiotherapy enhancement with gold nanoparticlesJ Pharm Pharmacol200860897798518644191
- SiegelRMaJZouZJemalACancer Statistics, 201464TorontoCanadian Cancer Society2014
- GérardJPMyintASCroceORenaissance of contact X-ray therapy for treating rectal cancerExpert Rev Med Devices20118448349221728733
- MoreiraLSDaniRTreatment of granular cell tumor of the esophagus by endoscopic injection of dehydrated alcoholAm J Gastroenterol19928756596611595659
- HiraoMMasudaKAsanumaTEndoscopic resection of early gastric cancer and other tumors with local injection of hypertonic saline-epinephrineGastrointest Endosc1987343264269
- YasuiTAkitaHSasakiSHayashiYKohriKEndoscopic injection of Teflon for correction of primary vesicoureteral reflux in childrenInt J Urol1997443493519256322
- PuriPChertinBVelayudhamMDassLColhounETreatment of vesicoureteral reflux by endoscopic injection of dextranomer/hyaluronic acid copolymer: preliminary resultsJ Urol20031704 pt 21541154414501655
- LessardFArchambaultLPlamondonMValidating plastic scintillation detectors for photon dosimetry in the radiologic energy rangeMed Phys20123995308531622957599
- CroceOHachemSFranchisseurEMarcieSGerardJBordyJContact radiotherapy using a 50 kV X-ray system: evaluation of relative dose distribution with the Monte Carlo code PENELOPE and comparison with measurementsRadiat Phys Chem2012816609617
- XiaoFZhengYCloutierPHeYHuntingDSancheLOn the role of low-energy electrons in the radiosensitization of DNA by gold nanoparticlesNanotechnology2011224646510122024607
- ChangMYShiauALChenYHChangCJChenHHWuCLIncreased apoptotic potential and dose-enhancing effect of gold nano-particles in combination with single-dose clinical electron beams on tumor-bearing miceCancer Sci20089971479148418410403
- TempletonAACChenSGrossSMMurrayRWHillCCarolinaNWater-soluble, isolable gold clusters protected by tiopronin and coenzyme A monolayersLangmuir199915136676
- CharestGPaquetteBFortinDMathieuDSancheLConcomitant treatment of F98 glioma cells with new liposomal platinum compounds and ionizing radiationJ Neurooncol201097218719319760366
- GendronLLucidoALMennickenFMorphine and pain-related stimuli enhance cell surface availability of somatic delta-opioid receptors in rat dorsal root gangliaJ Neurosci200626395396216421315
- TippayamontriTKotbRPaquetteBSancheLSynergism in concomitant chemoradiotherapy of cisplatin and oxaliplatin and their liposomal formulation in the human colorectal cancer HCT116 modelAnticancer Res201232104395440423060564
- SchneiderCARasbandWSEliceiriKWNIH Image to ImageJ: 25 years of image analysisNat Methods20129767167522930834
- JainSCoulterJAHounsellARCell-specific radiosensitization by gold nanoparticles at megavoltage radiation energiesInt J Radiat Oncol Biol Phys201179253153921095075
- ChithraniDBIntracellular uptake, transport, and processing of gold nanostructuresMol Membr Biol201027729931120929337
- WangLLiuYLiWSelective targeting of gold nanorods at the mitochondria of cancer cells: implications for cancer therapyNano Lett201111277278021186824
- McMahonSJHylandWBMuirMFBiological consequences of nanoscale energy deposition near irradiated heavy atom nanoparticlesSci Rep201111822355537
- MisawaMTakahashiJGeneration of reactive oxygen species induced by gold nanoparticles under X-ray and UV IrradiationsNanomedicine20117560461421333754
- RetifPPinelSToussaintMNanoparticles for radiation therapy enhancement: the key parametersTheranostics2015591030104426155318
- MaggiorellaLBarouchGDevauxCNanoscale radiotherapy with hafnium oxide nanoparticlesFuture Oncol2012891167118123030491
- TownleyHEKimJDobsonPJIn vivo demonstration of enhanced radiotherapy using rare earth doped titania nanoparticlesNanoscale20124165043505022767269
- Le DucGMiladiIAlricCToward an image-guided microbeam radiation therapy using gadolinium-based nanoparticlesACS Nano20115129566957422040385
- HubbellJHSeltzerSMTables of X-Ray Mass Attenuation Coefficients and Mass Energy-Absorption Coefficients from 1 keV to 20 MeV for Elements Z =1 to 92 and 48 Additional Substances of Dosimetric InterestGaithersburg, MDNational Institute of Standards and Technology1996