Abstract
Purpose
The aim of this study was to describe the trajectory of emergency caesarean deliveries for foetal distress at Chris Hani Baragwanath Academic Hospital (CHBAH).
Patients and Methods
A retrospective, contextual, descriptive study, using consecutive convenience sampling was done reviewing all the records of emergency caesarean deliveries for foetal distress at CHBAH in February 2019 until a minimum sample size of 385 was reached.
Results
During the study period, a total of 617 caesarean deliveries were done, of which 572 (92.7%) were emergencies. Foetal distress accounted for 395 (69.1%) of the emergency caesarean deliveries. No emergency caesarean delivery for foetal distress conformed to the 30-minute DDI and the mean (SD) DDI was 411 (291) minutes. The mean (SD) 5-minute and 10-minute Apgar scores were 8.4 (1.6) and 9.6 (1.3), respectively. There was a significant difference between the type of anaesthetic (general or neuraxial), with those receiving general anaesthesia having shorter anaesthetic start to cut time (p=0.0110). However, those delivered following neuraxial anaesthesia had better 5-minute (p=0.0002) and 10-minute (p=0.0175) Apgar scores.
Conclusion
This study showed that a DDI of 30-minutes, was not achieved at CHBAH during the study period. Most babies diagnosed with foetal distress pre-delivery had 5-minute and 10-minute Apgar scores inconsistent with this diagnosis. This over-diagnosis of foetal distress in some cases could have led to delays in delivery of babies who had actual foetal distress and where a 30-minute DDI could have improved outcome.
Introduction
Foetal distress occurs when the foetus becomes hypoxic during the antenatal or intrapartum periodCitation1 and requires immediate intrauterine resuscitation and caesarean delivery.Citation2 Effective diagnosis and management of foetal distress have short and long-term implications for not only the neonate but also for the family, the health care system and the community.Citation3 However, the accurate diagnosis and effective management of foetal distress remain complexCitation4 challenging and inexact.Citation5
Clinically foetal distress may be suspected by decreased foetal movement reported by the mother,Citation6 meconium in the amniotic fluid,Citation7 a non-reassuring pattern on electronic foetal monitoringCitation8 and biochemical signs such as foetal metabolic acidosis or elevated foetal blood lactate level.Citation9 The pathogenesis of foetal distress is multifactorial and can be due to processes such as uteroplacental deficiency, foetal sepsis and cord compression.Citation10 During the foetal distress pathogenesis, increased ischemic modified albumin levels maybe the best indicator of an underlying non – acute ischemic condition.Citation11 Hypoxia during intrapartum causes difficulties in nearly 1% of labours and results in mortality in almost 0.5 in 1000 pregnancies as well as cerebral palsy, a long-term neurological sequelae of intrapartum hypoxia, in a similar number of pregnancies.Citation12
For the obstetric anaesthetist, emergency caesarean deliveries for foetal distress can be challenging given the limited time, the increased threat to the foetus and the well-being of the mother. Therefore, the technique of anaesthesia chosen has clinical significance.Citation13 For elective caesarean delivery, neuraxial anaesthesia is recommended over general anaesthesia since there is less aspiration risk.Citation14 For emergency caesarean delivery, neuraxial anaesthesia should be used provided it does not delay the commencement of surgery.Citation15 Limited data exist regarding the best anaesthetic practice for emergency caesarean deliveries for foetal distress.Citation13
The Royal College of Obstetricians and Gynaecologists (RCOG)Citation16 and National Institute for Clinical Excellence (NICE)Citation17,Citation18 state that “where the indication to deliver is an immediate threat to the life of the mother or the foetus, delivery should occur within 30 minutes of the decision”. They further state “that for emergency deliveries, where there is no immediate threat to maternal or foetal health, delivery should occur within 75 minutes”. The reason for this classification is because the period of in-utero foetal hypoxia is considered as an important factor for the development of permanent foetal hypoxic-ischemic brain damage.Citation19 These various decisions to delivery time intervals (DDI) have been recommended by international professional organisationsCitation17 as a target and are key for clinical governance and risk management. Nevertheless, evidence that a 30- or 75-minute DDI is a clinically significant threshold lacks both in theory and practice.Citation20 It has been shown that the 30-minute DDI is not always met in obstetric units.Citation21–24 It is, therefore, important to determine whether the stipulated DDIs are being met in different settings. The DDI of emergency caesarean delivery for foetal distress at Chris Hani Baragwanath Academic Hospital (CHBAH) is not known and the aim of this study was to describe this trajectory.
Materials and Methods
A retrospective, contextual and descriptive research design was followed. Approval to conduct the study was obtained from the Human Research Ethics Committee (Medical) (M190615) of the University of the Witwatersrand and other relevant authorities. To ensure the anonymity of the data, the name of the patient and anaesthetist was not recorded. Every patient was allocated a study number. A list with patient study number was generated and filed separately. Confidentiality was maintained as only the authors had access to the raw data.
This study was conducted according to the principles of the Declaration of Helsinki and the South African Guidelines for Good Clinical Practise.
Ethics Committee of the University of Witwatersrand did not require patient consent since data was collected retrospectively from patient records.
The study population consisted of the records of all emergency caesarean deliveries for foetal distress at CHBAH in February 2019. The records consisted of the maternal register, labour ward booking lists, the theatre utilisation sheets and the birth register. In consultation with a biostatistician, it was determined that the minimum sample size needed to estimate the true population proportion of foetal distress at CHBAH with the required margin of error (5%) and confidence level (95%) and a power of greater than 80% was 385. A consecutive, convenience sampling method was used. Illegible records and records of women with a multiple pregnancy, known foetal anomalies and gestational age below 24 weeks were excluded from this study.
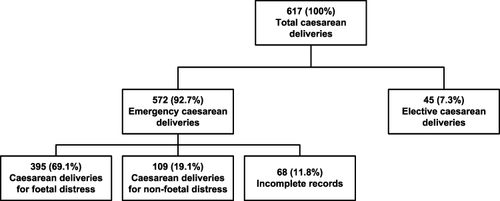
A draft data collection sheet was compiled following a literature review, thereby ensuring content validity. The draft data collection sheet was reviewed by three anaesthesiologists with an interest in obstetric anaesthesia, ensuring content and face validity. A summary of the collected data is shown in . The total number of emergency caesarean deliveries during the study period and the total number of emergency caesarean deliveries for foetal distress were documented ().
At CHBAH foetal distress is diagnosed using cardiotocography (CTG). However, no specific standard diagnostic criteria are used to categorise foetal distress. Therefore, in this study, a caesarean delivery booked for foetal distress was regarded as an emergency caesarean delivery. The DDI was the interval in minutes from the time of the decision to carry out the caesarean delivery to the time of delivery of the baby. The anaesthetic starting time to cut time was the time in minutes from the start of the anaesthetic to the skin incision and included the cleaning and draping time.
The data were analysed in consultation with a biostatistician using the statistical program STATA version 14.2 (StataCorp, USA). Categorical variables were described as frequencies and percentages and continuous variables as means and standard deviations if normally distributed or medians and interquartile ranges if not. The comparisons between the anaesthetic starting time and cut time and 5- and 10-minute Apgar scores between those receiving neuraxial anaesthesia and those receiving general anaesthesia were done using the Mann–Whitney U-test. A p-value of < 0.05 was considered statistically significant.
Results
A total of 617 caesarean deliveries were done during the study period, of which 572 (92.7%) were emergencies. There were 68 incomplete patient records that were excluded resulting in a sample of 395 (69.1%). Foetal distress accounted for 395 (69.1%) of the emergency caesarean deliveries. The characteristics of these 395 mothers are shown in . In terms of Robson Ten’s group classification, the high caesarean delivery rate in our institution is due to the women with previous caesarean delivery at term (Group 5) and nulliparous patients in spontaneous labour at 37 weeks (Group 1). One hundred and fifty-eight (40.0%) mothers had additional indications for caesarean delivery documented, of which 144 (91.1%) had 1 indication and 7 (4.4%) had 2 indications documented. Nine (2.3%) mothers had indications for caesarean delivery that were an immediate threat to the life of the mother or foetus, which were imminent eclampsia 5 (55.6%), eclampsia 1 (11.1%), HELLP syndrome 1 (11.1%) placental abruption 1 (11.1%) and antepartum haemorrhage 1 (11.1%).
Table 1 Characteristics of the Mothers
The 7 other additional conditions included 2 (22%) failed vaginal births after previous caesarean delivery, 2 (22%) preterm rupture of membranes, 2 (22%) post-dates and 1 (10%) intrauterine growth retardation. The DDI trajectory is shown in . The DDIs in 30-minute time intervals for the 395 mothers are shown in .
Table 2 Trajectory from Decision to Delivery Time Interval
Table 3 Decision to Delivery Time Intervals
Of the babies, 190 (48.1%) were males and 205 (51.9%) females. The mean (SD) weight of the babies was 2899 (674.6) g, with a minimum of 765 g and a maximum of 4450 g. Of the 392 (99.2%) babies discharged alive from theatre, 145 (37.0%) were admitted to the neonatal nursery following delivery for further observation and triage and 247 (63.0%) babies were discharged to the ward with the mother.
Only 6 (1.5%) babies had 1-minute Apgar scores recorded. The median (IQR) score for these babies was 5 (2.8–7.3). The mean (SD) 5-minute and 10-minute Apgar scores were 8.4 (1.6) and 9.6 (1.3) respectively. The 5-minute and 10-minute Apgar scores of the babies are shown in . Three babies were not successfully resuscitated by 10 minutes. Two of these babies had foetal distress of undocumented aetiology and one had foetal distress following placental abruption. At 5 minutes, 36 (9.1%) babies had an Apgar score of ≤6 and at 10 minutes 6 (1.5%) babies had an Apgar score of ≤6 and 3 (0.8%) were declared dead.
Table 4 The 5-Minute and 10-Minute Apgar Scores
The comparisons between the anaesthetic start to cut time, the 5-minute and the 10-minute Apgar scores between the group receiving neuraxial anaesthesia and the group receiving general anaesthesia are shown in . All were significantly different with those receiving a general anaesthetic having a shorter anaesthetic start to cut time and those delivered following neuraxial anaesthesia having slightly better Apgar scores.
Table 5 Comparisons Between Variables for Neuraxial and General Anaesthetic
Discussion
Foetal distress is one of the major indications for caesarean delivery in obstetric practice.Citation25 Our study showed that foetal distress was a major indication for emergency caesarean delivery (69.1%) at CHBAH. This is lower compared to Andisha and Cronje’Citation26 where foetal distress accounted for 81% of indications for emergency caesarean delivery at a tertiary hospital in Kwa-Zulu Natal. Our findings are similar to Guan et alCitation27 in Wuhan China, who found that among 991 mothers who received emergency caesarean delivery, the major direct cause was foetal distress (67.2%). However, our findings are contrary to other sub-Saharan countries where foetal distress contributed only 10% of the indications for caesarean delivery.Citation28 The possible explanation is that foetal distress is diagnosed using CTG at CHBAH and studies have shown that the sensitivity of CTG for foetal hypoxia is high, but the specificity is low.Citation29,Citation30 Also, interobserver interpretation of foetal heart rate for diagnosis of foetal distress has been shown to be only moderateCitation31 and when no specific standard guideline is followed to diagnose foetal distress, studies have shown that the sensitivity and specificity of CTG were also affected.Citation32,Citation33
Our findings show an increase in foetal distress compared to a previous study in 2015 by Adam et alCitation34 at CHBAH, which found that foetal distress (49.7%) was the most common indication for caesarean delivery followed by dystocia and previous caesarean delivery. These findings are consistent with a study by Mittal et al,Citation35 which showed that foetal distress as an indication for emergency delivery was increasing annually. This in keeping with progressive increases in the average annual caesarean delivery rate shown by multiple studiesCitation36–39 or could be due to the practice of defensive medicine, which is driven by litigation in obstetrics and gynaecology.Citation40–42
In our study, no emergency caesarean delivery for foetal distress conformed to the 30-minute DDI recommended by international professional organisations and the mean DDI was 411 minutes. Our study also found a prolonged decision to arrival in theatre time with a mean of 372 minutes and decision to anaesthesia time with a mean of 396 minutes. The prolonged decision to anaesthesia time influenced the DDI, but factors that caused the delay could not be determined as this was a retrospective study.
The prolonged decision to arrival in theatre time implies that delays occur in transferring patients to the theatre. The findings are consistent with Wong et al,Citation43 who found that in Singapore, caesarean delivery that exceeded the recommended timings were due to delays in transferring the patient to the theatre. According to a study by Radhakrishnan et alCitation44 the maximum delay occurred between the decision for caesarean delivery and transporting the patient to the theatre and was due to the non-availability of a theatre in 73.5% of cases. This could be the possible reason at CHBAH, where only two theatres are available for both emergency and elective obstetric cases and at times, are shared with gynaecological emergency cases.
Great variation regarding the percentage of babies delivered within a 30-minute DDI is reported ranging from 5%Citation26,Citation45 to almost 90%.Citation46 In the United Kingdom, multiple studies found that most emergency caesarean deliveries for foetal distress take longer than 30 minutes to commenceCitation47 and that it was not possible for busy obstetric units to reach this target in all emergency caesarean deliveries.Citation48 McKenzie and CookeCitation49 found that the mean DDI for foetal distress was 42.9 minutes. Helmy et alCitation50 showed an improvement in DDI within 30 minutes from 36% to 70% after multiple interventions aimed at improving the DDI and found that the major sources of delay were transporting the women to theatre and starting the anaesthetic. In Germany, Cerbinskaite et alCitation51 presented a shorter mean DDI of 32 minutes, with 45% of deliveries occurring in less than 30 minutes and 93% done within 75 minutes. In the United States of America, 90% of cases met the standard with a mean DDI of 25 minutes after multiple intervention such as open dialogue between nurses and physicians and the implementation of a worksheet.Citation46
In African countries, much longer DDIs have been observed, for instance, Onah et alCitation52 reported a mean DDI of 511 minutes in a Nigerian hospital. However, a cross-sectional study in northern Tanzania found that 12.3% of the women were operated on within 30 minutes, with a median DDI of 60 minutes.Citation24 In South Africa, two studies have evaluated DDI. In Tygerberg Hospital, a mean DDI of 53 minutes with 20% of the women delivered within 30 minutes and 76% within one hour for Category 1 and 2 emergency caesarean delivery was found.Citation53 At King Edward Hospital, a median DDI of 75 minutes with 5.2% of the parturients delivered within 30 minutes for Category 1 emergency caesarean delivery was found.Citation26
At CHBAH, no specific classification is used to categorise the emergency caesarean deliveries, hence all emergencies are prioritised at the discretion of the surgeon. However, Lucas et al,Citation54 in 2000, described a classification system for grading the urgency of caesarean delivery and defined four categories with clinical descriptions. This was later endorsed by the RCOG, NICE and Royal College of Anaesthetists and Obstetric Anaesthetists Association.
Category one (crash caesarean delivery) is defined as a compromise that is an immediate threat to the life of the woman or foetus, for example, foetal distress, and a DDI of equal to or less than 30 minutes is recommended, but for category two (compromise but no immediate threat to the life of the woman or foetus) a DDI of up to 75 minutes is acceptable.Citation17
In our study, 2.3% of the caesarean deliveries were due to an immediate threat to the life of the mother. Two mothers, one with placental abruption and the other with eclampsia, which fall under Category 1 caesarean delivery, were identified. The mother with placental abruption delivered a fresh stillbirth (DDI 75 minutes), while the eclamptic mother delivered a baby with low 5- and 10-minute Apgar scores of 0 and 4 (DDI 40 minutes), respectively. Other mothers who had an immediate threat to life were mothers with HELLP syndrome and antepartum haemorrhage. Both delivered babies with good Apgar scores of 9 and 10 even though their DDIs were prolonged at 375 minutes and 90 minutes, respectively.
A study on urgent caesarean delivery for different causes of foetal distress showed that, when the underlying cause of foetal distress was irreversible, such as placental abruption, cord prolapse, uterine rupture and pre-eclampsia the arterial cord pH deteriorates rapidly from the onset of foetal bradycardia. In such patients, immediate delivery is essential to minimise the risk of foetal brain damage due to hypoxia.Citation55 Kayani et al,Citation56 in a case-control study of pregnancy outcomes in severe placental abruption, showed that a DDI of 20 minutes or less was associated with substantially reduced neonatal morbidity and mortality and a DDI of more than 20 minutes was associated with a poor outcome such as neonatal death or later cerebral palsy. Gabbay-Benziv et alCitation57 found increased short-term morbidity for both mother and foetus in cases of placental abruption with foetal distress. The mean DDI was less than 30 minutes, emphasising that the 30-minute rule does not ensure short-term neonatal well-being.
Overall, studies looking at the relationship between DDI and neonatal outcomes have shown conflicting results. A study by Dunn et al,Citation58 had a mean DDI of 9.4 minutes for Category 1 caesarean delivery, but showed that a shorter DDI was not associated with improved perinatal outcomes. In Germany, a DDI of 20 minutes is recommended for Category 1 caesarean delivery and Hillermanns et alCitation59 found that DDIs below 20 minutes for Category 1 caesarean deliveries were inversely correlated to the foetal outcome, but a longer DDI between 20–28 minutes was associated with an improved foetal outcome such as higher Apgar scores. Heller et alCitation60 in a German perinatal survey of DDI and emergency caesarean delivery found that shorter DDIs of less than 20 minutes were associated with improved neonatal outcome.
The findings in our study showed contrary results since 64.8% of caesarean deliveries had DDIs of more than 240 minutes, but the mean 5-minute and 10-minute Apgar scores were 8.4 and 9.6, respectively. This is consistent with the findings of Roy et alCitation61 who showed that there was no difference in neonatal outcome when DDI was more than 30 minutes, but higher admission to the neonatal intensive unit for suspected birth asphyxia when DDI was less than 30 minutes. Onah et alCitation52 found that longer DDIs, even up to three hours, were not significantly correlated with poor perinatal outcome. However, Weiner et alCitation62 found that shorter DDIs in caesarean delivery for foetal distress resulted in improved neonatal outcome. In our study, 80% of the babies delivered had 10-minute Apgar scores of 10 and only 37% of the babies were admitted to the neonatal nursery for further observation. Our findings suggest that the use of CTG monitoring may result in the over-diagnosis of foetal distress.
Our study was retrospective and relied on the quality of the data recorded. Data were collected from one academic hospital, which limits the ability to generalise the results to other facilities. The neonatal outcome was evaluated using 5-minute and 10-minute Apgar scores, which is subjective and not a good indicator of long-term neurological outcome.Citation63 However, the Apgar score has been extensively used in numerous studies and allows comparisons to be drawn.
Conclusion
This study showed that a DDI of 30-minutes, as recommended by international organisations, was not achieved at CHBAH during the study period. This is concerning and should be addressed at both a clinical and higher management level. The majority of babies diagnosed with foetal distress pre-delivery had 5-minute and 10-minute Apgar scores inconsistent with this diagnosis. This over-diagnosis of foetal distress in some cases could have led to delays in delivery of babies who had actual foetal distress and where a 30-minute DDI could have improved outcome. This also demonstrates the need for further research into more accurate methods to diagnose foetal distress.
Abbreviations
DDI, decision to delivery interval; CHBAH, Chris Hani Baragwanath Academic Hospital; RCOG, Royal College of Obstetricians and Gynaecologists; NICE, National Institute for Clinical Excellence; CTG, cardiotocography.
Disclosure
The authors declare that we have no financial or personal relationships which may have inappropriately influenced us in writing this paper and report no conflicts of interest in relation to this work.
Acknowledgment
This research was done in partial fulfilment of a Master of Medicine degree.
References
- Leveno K, Bloom S, Dashe J, Hoffman B, Casey B, Spong C. William Obstetrics: Study Guide. 24th ed. New York, NY: McGraw-Hill Medical; 2014.
- Thurlow JA, Kinsella SM. Intrauterine resuscitation: active management of fetal distress. Int J Obstet Anesth. 2002;11(2):105–116. doi:10.1054/ijoa.2001.0933
- Eunson P. The long-term health, social, and financial burden of hypoxic-ischaemic encephalopathy. Dev Med Child Neurol. 2015;57(3):48–50. doi:10.1111/dmcn.12727
- Tharmaratnam S. Fetal distress. Baillieres Best Pract Res Clin Obstet Gynaecol. 2000;14(1):155–172. doi:10.1053/beog.1999.0069
- Afolabi BB, Lesi F. Regional versus general anaesthesia for caesarean section. Cochrane Database Syst Rev. 2006;(10):2–65. doi:10.1002/14651858.CD004350.pub3
- Heazell A. Reduced fetal movements. BMC Pregnancy Childbirth. 2012;12(1):2011–2012. doi:10.1186/1471-2393-12-S1-A10
- Ajah LO, Ibekwe PC, Onu FA, Onwe OE, Ezeonu TC, Omeje I. Evaluation of clinical diagnosis of fetal distress and perinatal outcome in a low resource Nigerian setting. J Clin Diagn Res. 2016;10(4):8–11. doi:10.7860/JCDR/2016/17274.7687
- Jenniskens K, Janssen PA. Newborn outcomes in British Columbia after caesarean section for non-reassuring fetal status. J Obstet Gynaecol Can. 2015;37(3):207–213. doi:10.1016/S1701-2163(15)30306-6
- Gravett C, Eckert LO, Gravett MG, et al. Non-reassuring fetal status: case definition and guidelines for data collection, analysis, and presentation of immunization safety data. Vaccine X. 2016;34(49):6084–6092. doi:10.1016/j.vaccine.2016.03.043
- Ayres-de-Campos D. Obstetric Emergencies: A Practical Guide. Porto, Portugal: Springer; 2017.
- Erol SA, Tanacan A, Altinboga O, Ozturk FH, Ozgu BS, Tasci Y. Evaluation of fetal serum thiol/disulfide homeostasis and ischemia-modified albumin levels in fetal distress. Fetal Pediatr Pathol. 2022;41(3):426–435. doi:10.1080/15513815.2020.1831662
- Gaffney G, Sellers S, Flavell V, Squier M, Johnson A. Case-control study of intrapartum care, cerebral palsy, and perinatal death. Br Med J. 1994;308(6931):743–750. doi:10.1136/bmj.308.6931.743
- Edipoglu IS, Celik F, Marangoz EC, Orcan GH, Staffieri F. Effect of anaesthetic technique on neonatal morbidity in emergency caesarean section for foetal distress. PLoS One. 2018;13(11):1–10. doi:10.1371/journal.pone.0207388
- Fernandes NL, Dyer RA. Anesthesia for urgent cesarean section. Clin Perinatol. 2019;46(4):785–799. doi:10.1016/j.clp.2019.08.010
- Afolayan JM, Olajumoke TO, Esangbedo SE, Edomwonyi NP. Spinal anaesthesia for caesarean section in pregnant women with fetal distress: time for reappraisal. Int J Biomed Sci. 2014;10(2):103–110.
- Royal College of Obstetricians and Gynaecologists (RCOG). Classification of urgency of caesarean section: a continuum of risk (Good Practice No 11); 2010. Available from: https://www.rcog.org.uk/globalassets/documents/guidelinesgoodpractice11classificationofurgencpdf. Accessed June 29, 2019.
- National Institute for Health and Care Excellence (NICE). Caesarean section: clinical guideline(CG132); 2011. Available from: www.nice.org.uk/guidance/cg132. Accessed May 24, 2020.
- Royal College of Obstetricians and Gynaecologists and The Royal College of Midwives. Caesarean section: NICE clinical guideline (NG137); 2011. Available from: https://www.nice.org.uk/guidance/ng137. Accessed May 29, 2019.
- Leung TY, Lao TT. Timing of caesarean section according to urgency. Best Pract Res Clin Obstet Gynaecol. 2013;27(2):251–267. doi:10.1016/j.bpobgyn.2012.09.005
- James D. Caesarean section for fetal distress: the 30 minute yardstick is in danger of becoming a rod for our backs. Br Med J. 2001;322(8718):1316–1317. doi:10.1016/0140-6736(90)93291-V
- Gupta S, Naithani U, Madhanmohan C, Singh A, Reddy P, Gupta A. Evaluation of decision-to-delivery interval in emergency cesarean section: a 1-year prospective audit in a tertiary care hospital. J Anaesthesiol Clin Pharmacol. 2017;33(1):64–70. doi:10.4103/0970-9185.202197
- Pearson GA, Kelly B, Russell R, Dutton S, Kurinczuk JJ, MacKenzie IZ. Target decision to delivery intervals for emergency caesarean section based on neonatal outcomes and three year follow-up. Eur J Obstet Gynecol Reprod Biol. 2011;159(2):276–281. doi:10.1016/j.ejogrb.2011.07.044
- Khemworapong K, Sompagdee N, Boriboonhirunsarn D. Decision-to-delivery interval in emergency cesarean delivery in tertiary care hospital in Thailand. Obstet Gynecol Sci. 2018;61(1):48–55. doi:10.5468/ogs.2018.61.1.48
- Hirani BA, Mchome BL, Mazuguni NS, Mahande MJ. The decision delivery interval in emergency caesarean section and its associated maternal and fetal outcomes at a referral hospital in northern Tanzania: a cross-sectional study. BMC Pregnancy Childbirth. 2017;17(1):1–6. doi:10.1186/s12884-017-1608-x
- Chauhan S, Megann E, Scott J, Scardo J, Hendrix N, Martin J. Cesarean delivery for fetal distress: rate and risk factors. Obstet Gynecol Surv. 2003;58(5):337–350. doi:10.1097/01.OGX.0000066802.19138.AE
- Andisha E, Cronje L. Evaluating the decision-to-delivery interval in category 1 emergency caesarean sections at a tertiary referral hospital. S Afr J Obstet Gynaecol. 2020;25(3):95–99. doi:10.7196/sajog.1510
- Guan P, Tang F, Sun G, Ren W. Prediction of emergency cesarean section by measurable maternal and fetal characteristics. J Investig Med. 2020;68(3):799–806. doi:10.1136/jim-2019-001175
- Chu K, Cortier H, Maldonado F, Mashant T, Ford N, Trelles M. Cesarean section rates and indications in sub-Saharan Africa: a multi-country study from Medecins Sans Frontieres. PLoS One. 2012;7(9):5–10. doi:10.1371/journal.pone.0044484
- Steer PJ. Has electronic fetal heart rate monitoring made a difference? Semin Fetal Neonatal Med. 2008;13(1):2–7. doi:10.1016/j.siny.2007.09.005
- Aboulghar W, Ibrahim M, Allam I, Hosny W, Otify M. Validity of cardiotocography in the diagnosis of acute fetal hypoxia in low resources settings. Internet J Gynecol Obstet. 2013;17(1):1–8.
- Blackwell SC, Grobman WA, Antoniewicz L, Hutchinson M, Bannerman CG. Interobserver and intraobserver reliability of the NICHD 3-tier fetal heart rate interpretation system. Am J Obstet Gynecol. 2011;205(4):378.e1–378.e5. doi:10.1016/j.ajog.2011.06.086
- Santo S, Ayres-de-Campos D, Costa-Santos C, et al. Agreement and accuracy using the FIGO, ACOG and NICE cardiotocography interpretation guidelines. Acta Obstet Gynecol Scand. 2017;96(2):166–175. doi:10.1111/aogs.13064
- Olofsson P, Norén H, Carlsson A. New FIGO and Swedish intrapartum cardiotocography classification systems incorporated in the fetal ECG ST analysis (STAN) interpretation algorithm: agreements and discrepancies in cardiotocography classification and evaluation of significant ST events. Acta Obstet Gynecol Scand. 2018;97(2):219–228. doi:10.1111/aogs.13277
- Adam Y, Mwinyoglee J, Masuku B, Nicolaou E. An evaluation of the indications for caesarean sections at Chris Hani Baragwanath Academic Hospital. S Afr J Obstet Gynaecol. 2018;24(1):11–14. doi:10.7196/SAJOG.2018.v24i1.1226
- Mittal S, Pardeshi S, Mayadeo N, Mane J. Trends in cesarean delivery: rate and indications. J Obstet Gynaecol India. 2014;64(4):251–254. doi:10.1007/s13224-013-0491-2
- Barber EL, Lundsberg LS, Belanger K, Pettker CM, Funai EF, Illuzzi JL. Indications contributing to the increasing cesarean delivery rate. Obstet Gynecol. 2011;118(1):29–38. doi:10.1097/AOG.0b013e31821e5f65
- Stavrou EP, Ford JB, Shand AW, Morris JM, Roberts CL. Epidemiology and trends for caesarean section births in New South Wales, Australia: a population-based study. BMC Pregnancy Childbirth. 2011;11(8):1–7. doi:10.1186/1471-2393-11-8
- Chong C, Su LL, Biswas A. Changing trends of cesarean section births by the Robson ten group classification in a tertiary teaching hospital. Acta Obstet Gynecol Scand. 2012;91:1422–1427. doi:10.1111/j.1600-0412.2012.01529.x
- Unnikrishnan B, Rakshith Prasad B, Amarnath A, et al. Trends and indications for caesarean section in a tertiary care obstetric hospital in coastal south India. Australas Med J. 2010;3(12):821–825. doi:10.4066/AMJ.2010.465
- Asher E, Dvir S, Seidman DS, Greenberg-Dotan S, Kedem A, Sheizaf B. Defensive medicine among obstetricians and gynecologists in tertiary hospitals. PLoS One. 2013;8(3):1–5. doi:10.1371/journal.pone.0057108
- Minkoff H. Fear of litigation and cesarean section rates. Semin Perinatol. 2012;36(5):390–394. doi:10.1053/j.semperi.2012.04.025
- Bhatara U. Rising rates of caesarean section: an indicator of defensive medicine practiced by obstetricians. Int J Reprod Contracept Obstet Gynecol. 2018;7(6):2371–2376. doi:10.18203/2320-1770.ijrcog20182352
- Wong TCT, Lau CQH, Tan EL, Kanagalingam D. Decision-to-delivery intervals and total duration of surgery for caesarean sections in a tertiary general hospital. Singapore Med J. 2017;58(6):332–337. doi:10.11622/smedj.2016098
- Radhakrishnan G, Yadav G, Vaid N, Ali H. Factors affecting “decision to delivery interval” in emergency caesarean sections in a tertiary care hospital: a cross sectional observational study. Int J Reprod Contracept Obstet Gynecol. 2013;2(4):651–656. doi:10.5455/2320-1770.ijrcog20131231
- Bruce D, Stone S, Harding K. Evaluation of emergency caesarean sections: completion of the audit cycle in a central London teaching hospital. J Obstet Gynaecol. 2002;22(3):273–278. doi:10.1080/01443610220130553
- Nageotte MP, Van der Wal B. Achievement of the 30-minute standard in obstetrics: can it be done? Am J Obstet Gynecol. 2012;206(2):104–107. doi:10.1016/j.ajog.2011.09.008
- Mackenzie IZ, Cooke I. Prospective 12 month study of 30 minute decision to delivery intervals for “emergency” caesarean section. Br Med J. 2001;322(7298):1334–1335. doi:10.1136/bmj.322.7298.1334
- Livermore LJ, Cochrane RM. Decision to delivery interval: a retrospective study of 1000 emergency caesarean sections. J Obstet Gynaecol. 2006;26(4):307–310. doi:10.1080/01443610600594898
- MacKenzie IZ, Cooke I. What is a reasonable time from decision-to-delivery by caesarean section? Evidence from 415 deliveries. BJOG. 2002;109(5):498–504. doi:10.1111/j.1471-0528.2002.01323.x
- Helmy WH, Jolaoso AS, Ifaturoti OO, Afify SA, Jones MH. The decision-to-delivery interval for emergency caesarean section: is 30 minutes a realistic target? BJOG. 2002;109(5):505–508. doi:10.1111/j.1471-0528.2002.00491.x
- Cerbinskaite A, Malone S, McDermott J, Loughney AD. Emergency caesarean section: influences on the decision-to-delivery interval. J Pregnancy. 2011;2011:1–6. doi:10.1155/2011/640379
- Onah HE, Ibeziako N, Umezulike AC, Effetie ER, Ogbuokiri CM. Decision - delivery interval and perinatal outcome in emergency caesarean sections. J Obstet Gynaecol. 2005;25(4):342–346. doi:10.1080/01443610500119671
- Le Riche H, Hall DR. Non-elective caesarean section: how long do we take to deliver? J Trop Pediatr. 2005;51(2):78–81. doi:10.1093/tropej/fmh082
- Lucas DN, Yentis SM, Kinsella SM, et al. Urgency of caesarean section: a new classification. J R Soc Med. 2000;93(7):346–350. doi:10.1177/014107680009300703
- Leung TY, Chung PW, Rogers MS, Sahota DS, Lao TT-H, Chung TKH. Urgent cesarean delivery for fetal bradycardia. Obstet Gynecol. 2010;115(4):1023–1028. doi:10.1097/AOG.0b013e3181d67ebc.
- Kayani SI, Walkinshaw SA, Preston C. Pregnancy outcome in severe placental abruption. BJOG. 2003;110(7):679–683. doi:10.1016/S1470-0328(03)02988-4
- Gabbay-Benziv R, Ashwal E, Lahav-Ezra H, et al. Decision-to delivery interval in suspected placental abruption: association with pregnancy outcome. J Matern Neonatal Med. 2013;27:1–4. doi:10.3109/14767058.2013.871703
- Dunn CN, Zhang Q, Sia JT, Assam PN, Tagore S, Sng BL. Evaluation of timings and outcomes in category-one caesarean sections: a retrospective cohort study. Indian J Anaesth. 2016;60(8):546–551. doi:10.4103/0019-5049.187782
- Hillemanns P, Strauss A, Hasbargen U, et al. Crash emergency cesarean section: decision-to-delivery interval under 30 min and its effect on apgar and umbilical artery pH. Arch Gynecol Obstet. 2005;273(3):161–165. doi:10.1007/s00404-005-0045-7
- Heller G, Bauer E, Schill S, et al. Decision-to-delivery time and perinatal complications in emergency cesarean section. Dtsch Arztebl Int. 2017;114(35–36):589–596. doi:10.3238/arztebl.2017.0589
- Roy KK, Baruah J, Kumar S, Deorari AK, Sharma JB, Karmakar D. Cesarean section for suspected fetal distress, continuous fetal heart monitoring and decision to delivery time. Indian J Pediatr. 2008;75(12):1249–1252. doi:10.1007/s12098-008-0245-9
- Weiner E, Bar J, Fainstein N, et al. The effect of a program to shorten the decision-to-delivery interval for emergent cesarean section on maternal and neonatal outcome. Am J Obstet Gynecol. 2014;210(3):224.e1–224.e6. doi:10.1016/j.ajog.2014.01.007
- Finster M, Wood M, Raja S. The apgar score has survived the test of time. Anesthesiology. 2005;102(4):855–857. doi:10.1097/00000542-200504000-00022