Abstract
Objective
This study aims to explore the nexus between students’ psychological well-being and the manifestation of gastrointestinal symptoms (GISs) amid the health lockdown enforced in Xi’an, focusing on the student populace of Xi’an Medical College and Shaanxi University of Traditional Chinese Medicine.
Materials and methods
A survey encompassing psychological parameters and GISs was administered to a randomized cohort of 1327 college students drawn from Xi’an Medical College and Shaanxi University of Traditional Chinese Medicine. The survey instrument was developed utilizing the Questionnaire Star platform. Subsequent to data collection, analysis was performed using GraphPad Prism 9 and SPSS 22.0.
Results
Comparative analysis revealed statistically significant disparities (P < 0.05) in various GISs between the periods during and preceding the health lockdown, encompassing symptoms such as nausea/vomiting, acid reflux, postprandial fullness/early satiety, anorexia, decreased appetite, bloating, abdominal discomfort, abdominal pain, diarrhea, and constipation. Notably, the mean score for Generalized Anxiety Disorder 7 (GAD-7) was 3.31±3.92, indicating mild anxiety, while the mean score for Patient Health Questionnaire-2 (PHQ-2) was 1.15±1.28, suggesting mild depression. Detailed evaluation of anxiety revealed prevalence rates of 34% among respondents, with 34.2% of these individuals reporting concurrent GISs, while among those evaluated for depression (38.8% of the sample), 44.2% reported concurrent GISs. Furthermore, multiple linear regression analysis unveiled a negative correlation between GISs during the health lockdown and lifestyle scores, while positive correlations were observed with GISs preceding the lockdown, anxiety, and depression. The formulated multiple linear regression equation for GISs during the health lockdown is delineated as follows: 14.693–0.342 life style + 0.725GISs before health lockdown + 0.218anxiety + 0.564 depression.
Conclusion
This investigation underscores the substantial impact of anxiety and depression on the student body, accentuating their role in precipitating GISs during health lockdown situations. The psychological well-being of medical students during exigent circumstances such as natural disasters warrants heightened attention, necessitating proactive measures aimed at emotional regulation to mitigate the onset of GISs.
Introduction
Since December 31, 2019, when Wuhan, Hubei Province, reported the initial case of Coronavirus Disease 2019 (COVID-19), the contagion swiftly disseminated across the globe. This phenomenon has led to profound alterations in societal routines and has significantly impacted individuals’ physical and mental well-being. Within the context of this global pandemic, an increasing number of individuals are grappling with psychological distress.Citation1–3 Research from China, Italy, Iran, Saudi Arabia, and Vietnam have revealed that anxiety, depression, and sleep difficulties were more prevalent during the COVID-19 pandemic.Citation4–10 These findings align with the notion that anxiety and depression constitute principal factors impacting individuals’ mental well-being in response to the COVID-19 pandemic.Citation4–7 Whether it was the outbreak of SARS in 2002, the Middle East respiratory syndrome, or the ongoing COVID-19 pandemic since 2019, numerous nations have resorted to implementing quarantines as a preventive measure against the spread of the virus. However, such quarantine measures can detrimentally affect individuals’ psychological well-being, contributing to negative mental health outcomes such as anxiety and depression.Citation11,Citation12 Because the “brain-gut axis” is bidirectionally regulated, negative emotions like anxiety and depression can impact how the gastrointestinal system functions, leading to a range of GISs.Citation13 Given the bidirectional regulation of the “brain-gut axis”, negative emotions such as anxiety and depression have the potential to influence the functioning of the gastrointestinal system, thereby precipitating a spectrum of GISs.Citation13 Similar findings have been corroborated by other studies wherein health restrictions exacerbated feelings of depression and anxiety, consequently precipitating a diverse array of GISs.Citation14,Citation15 During health lockdowns, GISs encompass a spectrum of manifestations including nausea/vomiting, heartburn, acid reflux, early satiety, anorexia, loss of appetite, bloating, abdominal discomfort, abdominal pain, diarrhea, constipation, as well as vomiting of blood and black stools. Psychological status, comprising anxiety and depression, is assessed using the GAD-7 Anxiety Scale and the PHQ-2 depression scale, respectively. It is noteworthy that medical personnel, confronting heightened stress levels amidst an epidemic, are more prone to experiencing GISs associated with negative emotions compared to the general population.Citation16,Citation17 Research suggests that worry can significantly affect a substantial proportion of college students, particularly those affiliated with medical institutions.Citation18 Medical students, constrained by their academic and professional commitments, may possess limited expertise in disease pathology. Consequently, they are susceptible to heightened levels of anxiety and depression, attributed to the prolonged duration of study, heightened academic pressure, and workload overload, in contrast to their counterparts in non-medical fields.Citation19,Citation20
A city-wide health lockdown was enforced in Xi’an, Shaanxi Province, on December 23, 2021, in response to the epidemic outbreak. The objective of our study was to examine the association between psychological well-being and GISs among students of Xi’an Medical College and Shaanxi University of Traditional Chinese Medicine (located in Xianyang, albeit subject to the health lockdown in Xi’an) during the period of health lockdown in Xi’an.
Participants and Methods
Participants
During the health lockdown in Xi’an, spanning from December 5th, 2022, to January 15th, 2023, a random sampling approach was employed to select 1089 students from a total of 5000 students enrolled at Shaanxi University of Traditional Chinese Medicine, alongside 238 students from a pool of 1200 enrolled at Xi’an Medical College. Subsequently, the questionnaire was administered utilizing the Questionnaire Star software. The inclusion criteria were as follows: (1) Enrollment at either Xi’an Medical College or Shaanxi University of Traditional Chinese Medicine as a medical student; (2)Residence under sealed and controlled management conditions during the health lockdown period; exclusion criteria: (1)Individuals testing positive for the novel coronavirus nucleic acid test; (2) Students residing in areas unaffected by health lockdown measures; (3) Survey respondents not affiliated with either of the two aforementioned universities.
Methods
Survey content (Supplementary Tables 1 and 2): ①Background characteristics of the participants (gender, ethnicity, age, single situation, school, household registration, education level, serving as a volunteer, infecting new crowns in the sealing and control area, etc.) 9 questions. ②Good life style (fruits, vegetables, meat, eggs and milk, irregular diet, exercise, a Likert 5-point scale score was used, with 1=never, 2=rarely, 3=sometimes, 4=often, and 5=always). Bad life style(alcohol consumption, smoking, staying up late, irregular diet, Multiple-choice a Likert 5-point scale score was used, with 5=never, 4=rarely, 3=sometimes, 2=often, and 1=always), calculate the total score.③The 12 questions were asked whether there were GISs (nausea/vomiting, heartburn, acid reflux, early satiety, anorexia, loss of appetite, bloating, abdominal discomfort, abdominal pain, diarrhea, constipation, vomiting of blood and black stools, etc.) during and before health lockdown. The same Likert 5-point scale was used to score the questions, 1=never, 2=rarely, 3=sometimes, 4=often, and 5=always. We divided the results into two categories: No and Yes GISs, or calculate the total score. ④GAD-7 Anxiety Scale:The GAD-7 was developed to screen and assess the severity of GAD-7 symptoms in clinical and research settings.Citation21 There were seven self-assessment items total. The items used a 4-point rating system, with 0 representing not at all, 1 representing 1–7 days, 2 representing 2–7 days, and 3 representing virtually every day. The frequency of symptoms was primarily graded based on the previous two weeks. The overall score was 21, where 0–4 represented no anxiety symptoms, 5–9 represented moderate anxiety, 10–14 represented medium anxiety, and 15–plus represented severe anxiety. You can also calculate the entire score. We divided the results into four categories: no anxiety, light anxiety, medium anxiety, and heavy anxiety, or divided into categories: no or yes anxiety, or the total score. ⑤PHQ-2 depression scale: The PHQ-2 scale, which is extremely simple and has a high sensitivity and specificity, was chosen for depression screening.Citation22 Two self-assessment items were included, using a 4-point scale of 0–3, with the frequency of symptoms rated mainly on the basis of the last 2 weeks, with the following criteria: 0=not at all, 1≤7 days, 2>7 days; 3=almost every day. The total score was 6, with 0–1 indicating no depression,1–2 indicating light depressive tendency, 3–4 indicating medium tendency, and 4–6 indicating heavy depressive tendency. We divided the results into four categories: no depression, light depression, medium depression, and heavy depression, or divided into categories: no or yes depression, or calculate the total score
Data Collection
During the health lockdown, a random sampling approach was employed to select 1327 students from Xi’an Medical College and Shaanxi University of Traditional Chinese Medicine. Among these, 1089 students from Shaanxi University of Traditional Chinese Medicine, constituting 5000 students in total, and 238 students from Xi’an Medical College, amounting to 1200 students overall, were included in the study sample.
Confidence Validity Analysis and Sample Size Estimation
The reliability and validity of the scale were demonstrated by the Kaiser-Meyer-Olkin (KMO) measure of sampling adequacy, which yielded a value of 0.901, indicating good reliability. Additionally, the internal consistency of the scale was confirmed by the Cronbach’s alpha coefficient, which was calculated as 0.942. The scale comprised 41 questions, and the estimated sample size required for analysis was 410. However, the actual sample size utilized in this survey was 1327, which substantially exceeded the estimated sample size, thereby enhancing the statistical robustness of the study.
Statistical Analysis
Initially, Excel 2019 was employed for organizing the raw data, while SPSS 26.0 statistical software served as the primary tool for data processing and analysis. Discontinuous rank data between groups were compared using either the chi-square test or Fisher’s exact test, while the independent samples t-test was applied to compare continuously variable measures across groups. To assess the normality of measurement data, the Shapiro–Wilk test was initially conducted. In cases where the data followed a normal distribution, results were presented as mean ± standard deviation (x ± s). Conversely, for skewed distributions, results were expressed as median (IQR). Statistical significance was determined at a threshold of p < 0.05.
Results
GISs During and Before Health Lockdown
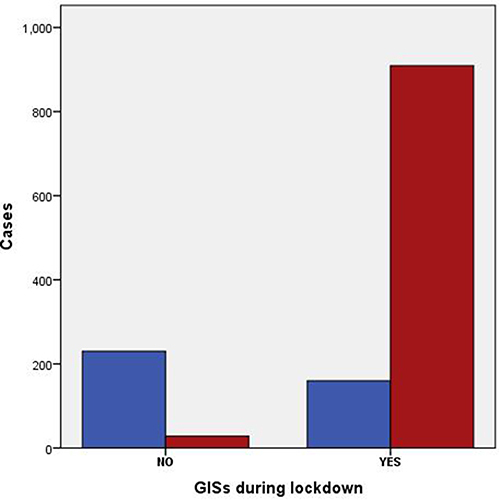
The demographic profiles of the subjects selected for this investigation are summarized in Supplementary Materials. Statistical analysis revealed that 80.6% of the respondents reported experiencing gastrointestinal symptoms (GISs) during the health lockdown, while 70.6% reported GISs prior to the implementation of the health lockdown (). illustrates a clustered bar chart presenting the contingency table depicting the relationship between GISs before and during the lockdown period. Among the 1327 participants, the distribution of GISs can be categorized as follows: 68.5% exhibited GISs both during and prior to the health lockdown; 12.1% manifested GISs solely during the lockdown; 2.1% did not experience GISs either during or prior to the health lockdown; and 17.3% were devoid of GISs both during and prior to the health lockdown. Furthermore, the association between GISs before and during the health lockdown was evaluated using a nonparametric correlation analysis based on the Spearman approach, revealing a highly significant statistical relationship between these variables in our dataset.
Table 1 GIS State: Frequency Analysis
Figure 1 Clustered bar chart based on the contingency table related to the interactions between GISs during lockdown and GISs before lockdown. The blue bar graph represents No GISs before lockdown, the red bar graph indicates yes GISs before lockdown, the horizontal axis NO represents No GISs during lockdown, the horizontal axis Yes represents yes GISs during lockdown. Crosstabs Person Chi-Square, p-value:0.000(<0.001).
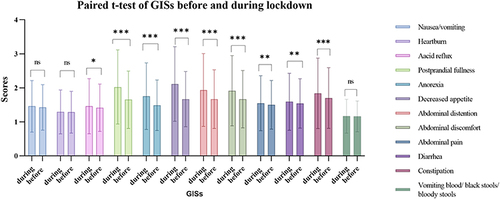
The paired t-test results indicate varying impacts of the epidemic on gastrointestinal symptoms (GISs) (refer to ). Specifically, the occurrence rates of nausea/vomiting, acid reflux, postprandial fullness/early satiety, anorexia, decreased appetite, abdominal distention, abdominal discomfort, abdominal pain, diarrhea, and constipation exhibited statistically significant differences between the periods during and prior to the health lockdown (P < 0.05).
Figure 2 Clustered bar chart based on paired t-test of GISs before and during lockdown. In academic statistical analysis, NS typically denotes a P-value greater than 0.05, indicating a lack of statistical significance in the results. The symbol * is used to denote a P-value less than or equal to 0.05, signifying statistical significance. Similarly, ** represents a P-value less than or equal to 0.01, while ***indicates a P-value less than or equal to 0.001, highlighting varying degrees of significance in the findings.
Anxiety and Depression State During Health Lockdown
The mean GAD-7 score was calculated to be 3.31±4.00, indicative of minimal anxiety, with scores ranging from 0 to 21. As illustrated in , the PHQ-2 score ranged from 0 to 6, suggesting a tendency towards depression, with a mean score of 1.15±1.28. Upon thorough examination, it was revealed that 34% of the surveyed individuals reported symptoms of anxiety, while 38.8% exhibited signs of depression ().
Table 2 Psychological Status Scores
Table 3 Anxiety and Depression State During Health Lockdown: Frequency Analysis
The Relationship Between GISs with Anxiety and Depression State
In order to elucidate the potential relationship between anxiety and depression and GISs during health lockdown, depression and anxiety states were dichotomized as “no” and “yes”. Subsequent analyses were conducted to explore the associations between the presence of GISs and the states of anxiety and depression, as well as the interplay between anxiety and depression themselves. Spearman’s rank correlation coefficient revealed a positive correlation between the presence of GISs during the health lockdown and both anxiety and depression states, with correlation coefficients of 0.22 (P < 0.001) for anxiety state and 0.23 (P < 0.001) for depression state.
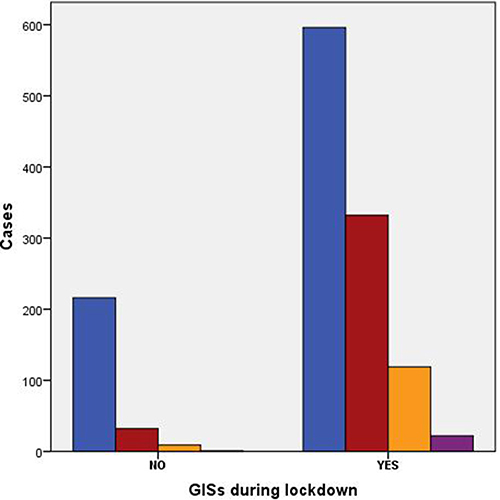
Further investigation is warranted to ascertain the potential causal relationship between GISs during a health lockdown and anxiety and depression. Anxiety and depression were stratified into categories of heavy, medium, and absent. A comprehensive analysis revealed that 34% of the surveyed individuals reported experiencing anxiety, with 34.2% of them also reporting GISs (). Additionally, anxiety was observed in 38.8% of the participants, among whom 44.2% also reported GISs (). To explore the association between GISs during health lockdown and the states of anxiety and depression, a nonparametric correlation analysis employing the Spearman approach was conducted. Our findings demonstrated a high level of statistical significance between these variables in our dataset.
Figure 3 Clustered bar chart based on the contingency table related to the interactions between GISs and anxiety state during the lockdown period.The blue bar graph represents No anxiety, the red bar graph indicates light anxiety, the yellow bar graph indicates medium anxiety, the purple bar graph indicates heavy anxiety, the horizontal axis NO represents No GISs during lockdown, the horizontal axis Yes represents yes GISs during lockdown. Crosstabs Person Chi-Square, p-value:0.000(<0.001).
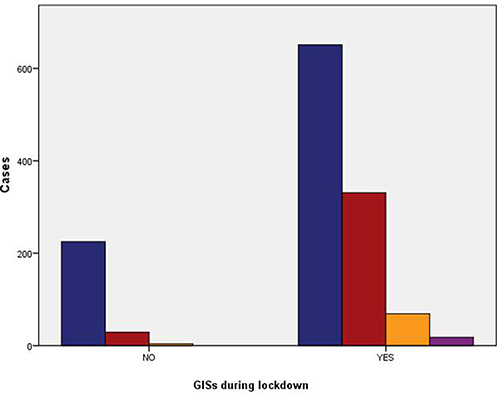
Figure 4 Clustered bar chart based on the contingency table related to the interactions between GISs and depression state during the lockdown period.The blue bar graph represents No depression, the red bar graph indicates light depression, the yellow bar graph indicates medium depression, the purple bar graph indicates heavy depression, the horizontal axis NO represents No GISs during lockdown, the horizontal axis Yes represents yes GISs during lockdown. Crosstabs Person Chi-Square, p-value:0.000(<0.001).
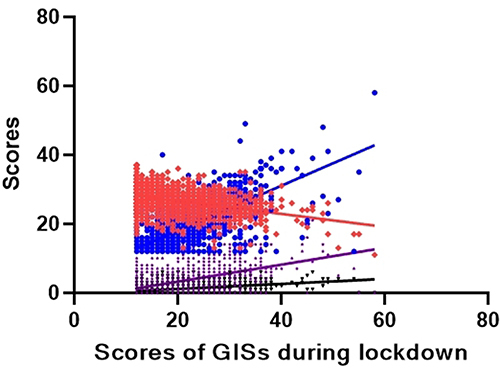
The preceding analysis established an association between gastrointestinal symptoms (GISs) and the states of anxiety and depression. However, the specific factors influencing GISs during the epidemic remained unidentified. Consequently, a multiple linear regression analysis was conducted to address this gap. The results indicated that GISs during the health lockdown exhibited a negative correlation with lifestyle scores, while demonstrating positive correlations with GISs before the health lockdown, anxiety, and depression (). The multiple linear regression equation describing GISs during the health lockdown is expressed as 14.693–0.342* lifestyle + 0.725* GISs before health lockdown + 0.218* anxiety + 0.564* depression ().
Table 4 Multiple Linear Regression of GISs During Health Lockdown
Figure 5 Multiple linear regression of GISs during lockdown. The red represents scores of life style, the blue represents scores of GISs before lockdown, the purple represents scores of anxiety, the black represents scores of depression. The multiple linear regression equation of GISs during health lockdown is 14.693–0.342*life style + 0.725*GISs before health lockdown + 0.218*anxiety + 0.564*depression.
Discussion
In the context of the global pandemic, an increasing number of individuals are grappling with psychological challenges. COVID-19 has emerged as the most formidable public health crisis of our era, profoundly reshaping the fabric of human existence.Citation1 Simultaneously, enforced isolation not only precipitates psychological issues but also gives rise to a spectrum of GISs.Citation13,Citation23,Citation24 Medical students constitute a distinctive cohort, possessing a deeper understanding of medicine compared to the general college populace, yet lacking the extensive clinical exposure characteristic of practicing physicians. A study documented a spectrum of psychological distress and GISs experienced by medical students during the enforced city closure in Italy.Citation25 With the objective of investigating the correlation between students’ psychological well-being and GISs, we conducted a survey among students enrolled in two medical schools situated in the epicenter of the outbreak in Xi’an during the health lockdown period.
Our study revealed that 34% and 38.8% of students encountered adverse psychological issues, namely anxiety and depression, while nearly 80.6% experienced gastrointestinal symptoms (GISs) during the health lockdown period. These findings align with a global investigation into anxiety and depression among medical students, which reported a prevalence rate of 33.8%.Citation18 Paired t-tests the results suggested that nausea/vomiting, acid reflux, postprandial fullness/early satiety, anorexia, decreased appetite, bloating, abdominal discomfort, abdominal pain, diarrhea, and constipation were significantly different (p < 0.05) during and before health lockdown. It has been shown that a range of GISs can occur or exacerbate existing GISs during the outbreak.Citation26,Citation27 Paired t-tests revealed significant differences (p < 0.05) between the occurrences of nausea/vomiting, acid reflux, postprandial fullness/early satiety, anorexia, decreased appetite, bloating, abdominal discomfort, abdominal pain, diarrhea, and constipation during and before the health lockdown period. These results indicate that various GISs may either manifest or worsen during the outbreak.Citation4–7,Citation10 Furthermore, studies have indicated that medical professionals are particularly prone to experiencing negative psychological phenomena such as anxiety and depression, attributed to the heightened stress they encounter amidst the pandemic.Citation7,Citation28,Citation29 Given their distinctive circumstances, medical students are predisposed to a heightened susceptibility to negative psychological manifestations, notably anxiety and depression.Citation18,Citation19 According to research findings, a minimum of 20% of individuals routinely present with “functional” GISs, meeting the diagnostic criteria for conditions characterized by the interplay between the brain and the stomach, such as irritable bowel syndrome (IBS) and/or functional dyspepsia (FD).Citation30 Aberrant gastrointestinal function and perturbed visceral sensory processing within the brain constitute integral components of the pathogenesis of these disorders. Mental states and various forms of stress have the potential to modulate the central processing of visceral sensations.Citation31
In conclusion, our study revealed a negative correlation between GISs during the health lockdown and lifestyle scores, while positive associations were observed with GISs preceding the health lockdown, as well as anxiety and depression. Multiple linear regression analysis confirmed these findings. Moreover, a 12-year follow-up investigation demonstrated a heightened likelihood of GISs among individuals with anxiety, underscoring the bidirectional influence of the brain-gut axis.Citation32 A separate investigation involving medical school students in Italy during the epidemic yielded congruent findings to our study, affirming the presence of GISs among students during the Italian health lockdown. However, unlike our study, they did not conduct linear regression analysis to elucidate the association with anxiety and depressive states.Citation25 These findings substantiate the notion that detrimental psychological manifestations, such as anxiety and depression, may precipitate GISs. While health lockdown serves as a primary catalyst for anxiety and depression, these outcomes are notably pronounced within the distinct cohort of medical students.
Hence, clinicians should remain cognizant of the impact of psychological conditions on GISs during lockdown scenarios, and proactively offer psychological counseling and lifestyle guidance to patients. Given the magnitude of a major catastrophic event, heightened attention should be directed towards individuals’ negative emotions, with timely counseling interventions being imperative. However, this study also bears certain limitations: (1) The survey encompassed only two institutions, which may not adequately represent the entirety of the medical student population; (2) Sole reliance on online questionnaires raises concerns regarding response bias and necessitates validation of respondents’ attitudes towards questionnaire completion; (3) The study solely delineates the association between GISs and negative mood without delving into further depth, leaving room for subsequent researchers to explore this relationship comprehensively.
Conclusion
Our research underscores the pivotal role of the gut-brain axis in human health, particularly in how stress-inducing life events interact with it to precipitate gastrointestinal symptoms (GISs). Specifically, we shed light on the stressors associated with health lockdowns and unveil a direct correlation between escalating health-related anxiety among medical students and a deterioration in GISs. Our findings accentuate the ramifications of prolonged stress conditions on psychological well-being and elucidate the indirect repercussions of the COVID-19 pandemic on the gastrointestinal system. Furthermore, our study reveals a noteworthy prevalence of anxiety symptoms among medical students. In circumstances of adversity, such as earthquakes and fires, heightened attention to the psychological well-being of both medical students and individuals experiencing GISs is imperative. Increasing awareness regarding the necessity to mitigate negative emotions and implementing proactive measures to prevent the onset of GISs is paramount.
Abbreviations
Corona Virus Disease 2019(COVID-19); gastrointestinal symptoms(GIS); Inflammatory bowel disease(IBD); Irritable bowel syndrome(IBS).
Data Sharing Statement
Both the article and its online supplementary material contain the data that support it (see Supplementary Tables S1 and S2).
Ethical Considerations
All participants were duly apprised of the voluntary nature of their participation and assured that they could withdraw from the study at any juncture without facing repercussions. The study protocol received approval from the Ethics Committee of the First Affiliated Hospital of Xi’an Medical College on January 18, 2022, and informed consent was diligently obtained from all participants. The approval number assigned to the study is NO.XYYFY2022LSK-003.Our study complies with the Declaration of Helsinki.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
We thus declare that there was no financial or commercial tie that might be interpreted as posing a conflict of interest during the research.
Acknowledgments
This is a short text to acknowledge the contributions of Yubei District People’s Hospital of Chongqing and The First Affiliated Hospital of Xi’an Medical University.
Additional information
Funding
References
- Pfefferbaum B, North CS. Mental Health and the Covid-19 Pandemic. New Engl J Med. 2020;383(6):510–512. doi:10.1056/NEJMp2008017
- Gencer S, Lacy M, Atzler D, van der Vorst EPC, Döring Y, Weber C. Immunoinflammatory, Thrombohaemostatic, and Cardiovascular Mechanisms in COVID-19. Thrombosis Haemostasis. 2020;120(12):1629–1641. doi:10.1055/s-0040-1718735
- Nicola M, Alsafi Z, Sohrabi C. The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int J Surgery. 2020;78:185–193. doi:10.1016/j.ijsu.2020.04.018
- Ornell F, Schuch JB, Sordi AO, Kessler FHP. “Pandemic fear” and COVID-19: mental health burden and strategies. Rev Bras Psiquiatr. 2020;42(3):232–235. doi:10.1590/1516-4446-2020-0008
- Wang C, Pan R, Wan X, et al. Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int J Environ Res Public Health. 2020;17(5).
- Parvar SY, Ghamari N, Pezeshkian F, Shahriarirad R. Prevalence of anxiety, depression, stress, and perceived stress and their relation with resilience during the COVID −19 pandemic, a cross-sectional study. Health Sci Rep. 2022;5(1):e460. doi:10.1002/hsr2.460
- Hassannia L, Taghizadeh F, Moosazadeh M. Anxiety and Depression in Health Workers and General Population During COVID-19 in Iran: a Cross-Sectional Study. Neuropsychopharmacology Rep. 2021;41(1):40–49. doi:10.1002/npr2.12153
- Lenzo V, Quattropani MC, Musetti A. Resilience Contributes to Low Emotional Impact of the COVID-19 Outbreak Among the General Population in Italy. Front Psychol. 2020;11:576485. doi:10.3389/fpsyg.2020.576485
- Ngoc Cong Duong K, Nguyen Le Bao T, Thi Lan Nguyen P. Correction: psychological Impacts of COVID-19 During the First Nationwide Lockdown in Vietnam: web-Based, Cross-Sectional Survey Study. JMIR Format Res. 2021;5(3):e28357. doi:10.2196/28357
- Alkhamees AA, Alrashed SA, Alzunaydi AA, Almohimeed AS, Aljohani MS. The psychological impact of COVID-19 pandemic on the general population of Saudi Arabia. Comprehensive Psychiatry. 2020;102:152192. doi:10.1016/j.comppsych.2020.152192
- Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Em Infect Dis. 2004;10(7):1206–1212. doi:10.3201/eid1007.030703
- Salazar A, Palomo-osuna J, De Sola H, et al. Psychological Impact of the Lockdown Due to the COVID-19 Pandemic in University Workers: factors Related to Stress, Anxiety, and Depression. Int J Environ Res Public Health. 2021;18(8).
- Nakov R, Dimitrova‐Yurukova D, Snegarova V, Nakov V, Fox M, Heinrich H. Increased prevalence of gastrointestinal symptoms and disorders of gut-brain interaction during the COVID-19 pandemic: an internet-based survey. Neurogastroenterol Motility. 2022;34(2):e14197. doi:10.1111/nmo.14197
- Oliviero G, Ruggiero L, D’Antonio E. Publication: “Impact of COVID-19 lockdown on symptoms in patients with functional gastrointestinal disorders: relationship with anxiety and perceived stress”. Neurogastroenterol Motil. 2021;33(11):e14263. doi:10.1111/nmo.14263
- Wang XJ, Murphy B, Breen‐Lyles M, Fox J. Publication: “Impact of COVID-19 lockdown on symptoms in patients with functional gastrointestinal disorders: relationship with anxiety and perceived stress”. Neurogastroenterol Motil. 2021;33(11):e14207. doi:10.1111/nmo.14207
- Chew NWS, Lee GKH, Tan BYQ. A multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav Immun. 2020;88:559–565. doi:10.1016/j.bbi.2020.04.049
- Liang Y, Wu K, Zhou Y, et al. Mental Health in Frontline Medical Workers during the 2019 Novel Coronavirus Disease Epidemic in China: a Comparison with the General Population. Int J Environ Res Public Health. 2020;17(18).
- Quek TT, Tam WW, Tran BX, et al. The Global Prevalence of Anxiety Among Medical Students: a Meta-Analysis. Int J Environ Res Public Health. 2019;16(15).
- Almazan AN, Chun AS, Perez-Urbano I. The Medical Student Response to the Mental Health Consequences of COVID-19. Acad Psychiatry. 2020;44(6):689–690. doi:10.1007/s40596-020-01313-x
- Sun S, Goldberg SB, Lin D, Qiao S, Operario D. Psychiatric symptoms, risk, and protective factors among university students in quarantine during the COVID-19 pandemic in China. Globalization Health. 2021;17(1):15. doi:10.1186/s12992-021-00663-x
- Spitzer RL, Kroenke K, Williams JBW, Löwe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Internal Med. 2006;166(10):1092–1097. doi:10.1001/archinte.166.10.1092
- Levis B, Sun Y, He C. Accuracy of the PHQ-2 Alone and in Combination With the PHQ-9 for Screening to Detect Major Depression: systematic Review and Meta-analysis. JAMA. 2020;323(22):2290–2300. doi:10.1001/jama.2020.6504
- Debock EFilipe MD, Meij V, et al. Quality of life in patients with IBD during the COVID-19 pandemic in the Netherlands. BMJ Open Gastroenterol. 2021;8(1):e000670.
- Larussa T, Flauti D, Abenavoli L, et al. The Reality of Patient-Reported Outcomes of Health-Related Quality of Life in an Italian Cohort of Patients with Inflammatory Bowel Disease: results from a Cross-Sectional Study. J Clin Med. 2020;9(8):2416.
- Abenavoli L, Cinaglia P, Lombardo G, et al. Anxiety and Gastrointestinal Symptoms Related to COVID-19 during Italian Lockdown. J Clin Med. 2021;10(6):1221.
- Yuan S, Liao Z, Huang H. Comparison of the Indicators of Psychological Stress in the Population of Hubei Province and Non-Endemic Provinces in China During Two Weeks During the Coronavirus Disease 2019 (COVID-19) Outbreak in February 2020. Med Sci Monitor. 2020;26:e923767. doi:10.12659/MSM.923767
- Haug TT, Mykletun A, Dahl AA. The association between anxiety, depression, and somatic symptoms in a large population: the HUNT-II study. Psychosomatic Med. 2004;66(6):845–851. doi:10.1097/01.psy.0000145823.85658.0c
- Saragih ID, Tonapa SI, Saragih IS, et al. Global prevalence of mental health problems among healthcare workers during the Covid-19 pandemic: a systematic review and meta-analysis. Int J Nursing Studies. 2021;121:104002.
- Chutiyami M, Bello UM, Salihu D, et al. COVID-19 pandemic-related mortality, infection, symptoms, complications, comorbidities, and other aspects of physical health among healthcare workers globally: an umbrella review. Int J Nursing Studies. 2022;129:104211.
- Ford AC, Mahadeva S, Carbone MF, Lacy BE, Talley NJ. Functional dyspepsia. Lancet. 2020;396(10263):1689–1702. doi:10.1016/S0140-6736(20)30469-4
- Ford AC, Sperber AD, Corsetti M, Camilleri M. Irritable bowel syndrome. Lancet. 2020;396(10263):1675–1688. doi:10.1016/S0140-6736(20)31548-8
- Koloski NA, Jones M, Kalantar J, Weltman M, Zaguirre J, Talley NJ. The brain--gut pathway in functional gastrointestinal disorders is bidirectional: a 12-year prospective population-based study. Gut. 2012;61(9):1284–1290. doi:10.1136/gutjnl-2011-300474

