Abstract
Methotrexate (MTX) is an important component in the therapy used to treat childhood acute lymphoblastic leukemia (ALL). Methylenetetrahydrofolate reductase (MTHFR) is a key enzyme for MTX pharmacokinetics. Two single-nucleotide polymorphisms in MTHFR gene, C677T and A1298C, affecting MTHFR activity, have been widely studied as potential markers of MTX toxicity and/or outcome in pediatric ALL. In this review, we show that the majority of published reports do not find association or present opposite effect. Therefore, MTHFR C677T and A1298C polymorphisms do not seem to be good markers of MTX-related toxicity and/or outcome in pediatric ALL. The efforts should be focused on other genes, such as transporter genes or microRNA-related genes.
Introduction
Acute lymphoblastic leukemia (ALL) is the most common type of cancer in children, representing ~30% of all childhood malignancies.Citation1,Citation2 Survival rates have increased dramatically over the last years because of chemotherapy progress, with expected cure rates higher than 80%.Citation3 Methotrexate (MTX) is an important drug used in the treatment protocols for ALL. However, MTX can cause toxicity, leading to a dose reduction or treatment interruption, which could compromise the survival.
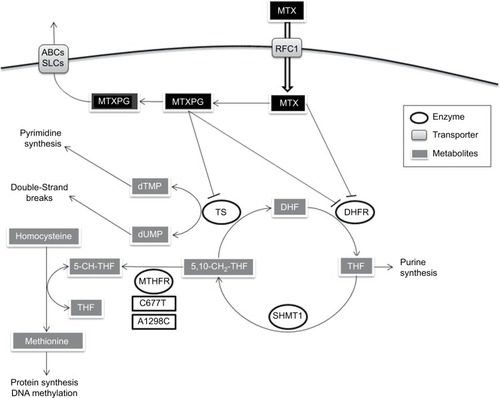
MTX is a folate analog that enters the cell via active transport mediated by the reduced folate carrier (RFC1).Citation4 Then, MTX inhibits dihydrofolate reductase, arresting the folic acid cycle and affecting other important enzymes such as methylenetetrahydrofolate reductase (MTHFR), an enzyme that interferes with nucleic acid synthesis and favors cell death.Citation5 Thus, MTHFR is a key enzyme for intracellular folate homeostasis and metabolism, because it catalyzes the irreversible conversion of 5,10-methylenetetrahydrofolate, required for purine and thymidine synthesis, to 5-methyltetrahydrofolate, required for protein synthesis and nucleic acid methylation. Subsequently, changes in the activity of MTHFR provoking an impaired conversion of 5,10-methylenetetrahydrofolate to 5-methyltetrahydrofolate could modify folate pools and in turn alter the response of malignant and nonmalignant cells to MTX and influence its toxicityCitation6 ().
Figure 1 MTX pathway.
Abbreviations: ABCs, ABC family transporters; DHF, dihydrofolate; DHFR, dihydrofolate reductase; MTHFR, methylenetetrahydrofolate reductase; MTX, methotrexate; MTXPG, methotrexate polyglutamated forms; RFC1, reduced folate carrier; SHMT1, serine hydromethyl transferase; SLCs, SLC family transporters; THF, tetrahydrofolate; TS, thymidilate synthase; 5-CH-THF, 5-methyltetrahydrofolate; 5,10-CH2-THF, 5,10-methylenetetrahydrofolate.
In this context, two of the MTHFR polymorphisms most widely studied in relation to the toxicity of MTX are C677T (causing Ala222Val) and A1298C (causing Glu429Ala). Both polymorphisms have been associated with reduced enzyme activity. In the case of C677T, 677CT and 677TT individuals exhibit 60% and 30% of the normal MTHFR activity, respectively.Citation7,Citation8 In the case of A1298C, 1298CC individuals show 60% of the normal activity.Citation9 Therefore, the patients carrying the variant alleles might have a higher intolerance to MTX or an increased risk of progression.Citation8
MTX intolerance can manifest through adverse reactions of several organ systems such as hematological (anemia, thrombocytopenia, leukopenia, neutropenia), gastrointestinal (mucositis), hepatobiliary, urogenital, or central nervous system.Citation10 Also, MTX plasma levels are used as an objective MTX-related toxicity marker.Citation11 In some patients, the toxic effects are so serious that the dose must be cut down or the treatment paused, which besides the problems related to toxicity, can also have a negative impact on survival.Citation12
As we have mentioned herein, variants that alter MTHFR activity may increase the availability of 5,10-methylenetetrahydrofolate and decrease 5-methyltetrahydrofolate. The reduction of this last would lead to DNA hypomethylation, which could invoke carcinogenesis through three different mechanisms: chromosomal instability, reactivation of elements, and loss of imprinting.Citation13 The loss of methylation might favor mitotic recombination, leading to loss of heterozygosity as well as promoting karyotypically detectable rearrangements. Intragenomic parasitic DNA and other previously silent transposons may then be transcribed and even “jump” to other parts of the genome, leading to disruption of normal genes. Hypomethylation can likewise affect imprinted genes, which have been shown to contribute to carcinogenesis. Finally, genomic DNA hypomethylation can also increase through all the tumorigenic steps,Citation14 from the benign proliferations to the invasive cancers.Citation13 Therefore, decreased MTHFR activity due to 677T or 1298C alleles could induce hypomethylation, and all these modifications can lead to an increase in carcinogenesis.
To date, several groups have investigated the potential role of MTHFR polymorphisms in relation to the toxicity of MTX, as well as outcome in pediatric ALL, but the conclusions remain controversial. Some studies do not find association, whereas others present opposite effect. In consequence, we consider that it would be interesting to clarify these discrepancies.
Toxicity and MTHFR C677T and A1298C polymorphisms
In 2013, our group performed an exhaustive search to identify studies that examined the association between the C677T and A1298C polymorphisms of MTHFR and MTX toxicity in pediatric ALL patients. We used the keywords and subject terms “MTHFR and acute leukemia”, and “MTHFR and polymorphism(s) and toxicity” to search PubMed (www.ncbi.nlm.nih.gov/pubmed) for articles published through November 2011. We also carried out a meta-analysis with those articles supplying enough information on toxicity by genotype. The study was performed in a population composed only of pediatric ALL patients for short-term toxic effects including (MTX plasma levels, mucositis, hepatic toxicity, neutropenia, thrombocytopenia, anemia, and leucopenia).
The meta-analysis included 24 studies for C677T and 16 studies for A1298C. For C677T, none of the analysis revealed a statistically significant association with toxicity. In the case of A1298C, only a slight protective effect of 1298CC genotype for leukopenia was observed.Citation15 Therefore, we concluded that there was no evidence to support the use of either the MTHFR C677T or the A1298C single-nucleotide polymorphisms (SNPs) as MTX toxicity markers in pediatric ALL patients, and consequently the MTX dose should not be adjusted based on these variants.
At the same time, Yang et alCitation16 performed another meta-analysis studying the effect of C677T and A1298C MTHFR polymorphisms on MTX-induced myelosuppression, oral mucositis, liver, hematological, gastrointestinal, and neurological toxicities. They only found a slight association between C677T and gastrointestinal toxicity in pediatric ALL. None of the polymorphisms was associated to any of the other studied toxicities, so again in this study, neither C667T nor A1298C were proved to be good toxicity markers for MTX dose reduction.
In spite of all this evidence, new studies are being published every year analyzing the involvement of MTHFR C677T and A1298C polymorphisms in MTX toxicity in pediatric ALL treatment. Herein, we have performed an exhaustive search to identify new studies that explore the association between the C677T and A1298C polymorphisms of MTHFR and MTX-induced toxicity from November 2011 to November 2016, following the same strategy as before.Citation15 Keywords “MTHFR” and “acute lymphoblastic leukemia” for PubMed database were used.
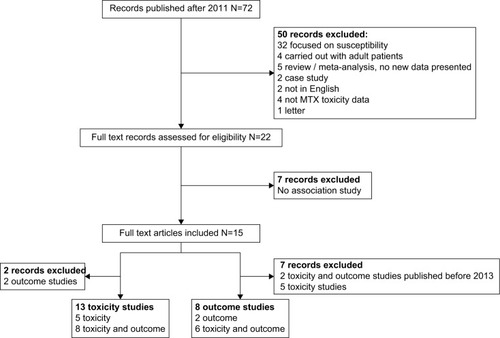
The search provided 186 records, 114 of them were directly discarded because they were published before 2011. From the remaining 72 papers, after abstract screening, 50 were excluded for not analyzing C677T and A1298C polymorphisms in pediatric ALL. For the other 22, full lecture was performed. Seven out of 22 articles were discarded, 4 because they were not focused on the analysis of C677T and A1298C polymorphism and MTX-induced toxicities,Citation17–Citation20 and other 3 because they analyzed the effect of the C677T/A1298C haplotype in MTX-related toxicity and each genotype could not be evaluated separately.Citation21–Citation23 We finally reviewed 15 articles that analyzed the MTHFR polymorphisms in relation to MTX-induced toxicities in pediatric ALL patients. Of the 15 reviewed papers, 2 were discarded for analyzing only outcome, and 13 studies that analyzed the association with MTX induced toxicities remained. The search and study selection process are shown in .
C677T polymorphism analysis
The 13 selected articles analyzed the C677T polymorphism in relation to MTX-induced toxicities. From them, only 5 found significant associations with toxicity, but with contradictory results: 2 studies related the T variant allele to a decrease in toxicity risk,Citation24,Citation25 whereas the other 3 associated it to increased risk ().Citation26–Citation28
Table 1 List of 13 studies that analyzed association between the MTHFR C677T polymorphism and MTX toxicity in pediatric ALL, grouped according to the level of association between the SNP and MTX toxicity
When we analyzed those studies in depth, we again found discordant results (). The association study between MTX pharmacokinetics and C677T polymorphism showed that 7 out of 8 studies did not find significant association. Haase et alCitation25 was the only study in which MTX levels were significantly increased in patients with the MTHFR C677T wild type compared to CT/TT genotype variant carriers. However, the number of patients included in this study was very low (n=35). In our previous meta-analysis, only one study found association, but the result was just the opposite.Citation29 Until now, taking into account our previous meta-analysis and the studies included in this review, a total of 13 studies have been performed about MTX pharmacokinetics, 11 with no association, and 2 with association but with opposite results. Therefore, C677T could not be considered as a good marker for MTX pharmacokinetics.
Table 2 Types of toxicities analyzed and the findings in each study of the association between the MTHFR C677T polymorphism and MTX toxicity
With regard to hematological toxicity, when anemia was analyzed, only 2 out of 5 studies found association. Haase et alCitation25 showed that the variant of C677T was associated with a decreased toxicity, whereas Zgheib et alCitation27 found the opposite effect. The other 3 studies found no association with anemia (). Contradictory results were also seen for leukopenia, for which Haase et alCitation25 showed that the C677T T variant allele was associated with a decreased toxicity, whereas Aráoz et alCitation26 found that this allele increased the risk of severe leukopenia, but only in carriers who received 2 g/m2 of MTX. However, Aráoz et alCitation26 also observed that the 677T allele did not seem to modulate the presence of severe adverse events in patients who received 5 g/m2 of MTX. The analysis of leukopenia in the other 3 studies showed no association with toxicity (). Neutropenia was analyzed in 4 studies. Only the study of Aráoz et alCitation26 found risk 677T allele associated to neutropenia in patients who received low doses of MTX (2 g/m2). None of the other 3 studies found association. Again, these results are in line with the results of our previous meta-analysis in which we proposed that C677T polymorphism does not seem to be a good marker for hematological toxicity.
Hepatotoxicity was analyzed in 7 studies, and only the study of Fukushima et alCitation28 found significant association for 677CT/TT carriers. This study was conducted in a cohort of 103 Japanese patients, that mixed ALL (n=82) and non-Hodgkin lymphoma (NHL) (N=21) patients. In contrast, another study carried out in another Japanese population found no significant association.Citation30 The other 5 studies performed in other populations found no significant association either. Once more, these results are in line with the results found by our group in the previous review, in which 13 studies out of 16 were not significant.
Mucositis was analyzed in 5 studies, and only Ramírez-Pacheco et alCitation24 concluded that CC genotype was associated with a higher risk of developing mucositis in a cohort of 109 children with ALL. The rest of the 4 studies found no association, in line with our meta-analysis results in which 8 out of 10 studies were not significant.
Finally, for thrombocytopenia and renal toxicity with 3 studies and neurotoxicity with 2 studies, none of them found significant association. Once more, these results were in agreement with the previous ones.
In conclusion, after analyzing thoroughly a total of 37 articles and 4,583 patients (24 studies with 3,104 patients from the previous meta-analysis and 13 studies with 1,479 patients from our actual review) and considering that the majority of studies were not significant, the significant results were often contradictory or with low statistical power, we can conclude that C677T is not a good MTX toxicity marker in pediatric ALL.
A1298C polymorphism analysis
Of the 13 articles reviewed, 10 analyzed the association of A1298C polymorphism with MTX-induced toxicity (). From them, only 3 studies found significant association. Moulik et alCitation31 and Haase et alCitation25 showed the C variant allele favoring an increase in toxicity, whereas Fukushima et alCitation28 showed a protective role for the C variant allele. When the different toxicities were considered, almost all the results found no significant associations ().
Table 3 List of 10 studies that analyzed association between the MTHFR A1298C polymorphism and MTX toxicity in pediatric ALL, grouped according to the level of association between the SNP and MTX toxicity
Table 4 Types of toxicities analyzed and the findings in each study of the associations between the MTHFR A1298C polymorphism and MTX toxicity
Regarding anemia, 3 of 5 studies found no significant results, whereas both Moulik et alCitation31 and Haase et alCitation25 found association with an increase in toxicity for patients carrying the CC genotype. These studies included a low number of patients (n=21 and n=35, respectively), whereas the studies that did not result in significance were performed in cohorts of 106,Citation32 161,Citation26 and 127Citation27 patients. Since our previous review found no association in 5 of the 6 studies that analyzed anemia and the one that showed association was performed in a population of 37 patients,Citation33 we can conclude that A1298C variant is not a good marker for anemia.
Hepatotoxicity was analyzed in 7 studies, only Fukushima et alCitation28 showed significant results in their cohort of children, which as previously mentioned, mixed 82 ALL patients and 21 NHL patients. In this study, 1298CC genotype patients presented a lower hepatic toxicity risk comparing to the 1298AA genotype patients. The other 6 studies did not find association between the polymorphism and hepatic toxicity. These results agree with our previous meta-analysis where 8 out of 10 studies neither found significant association. Moreover, the 2 studies that showed association in the previous meta-analysis found the opposite effect for the variant C allele that increased hepatic toxicity.Citation33,Citation34
For MTX pharmacokinetics and A1298C since November 2011, 6 new studies have been performed, but significant results have not been detected in any of them. These results in combination with the results from our previous meta-analysis, where only one study conducted in a population of 37 patients obtained significant results,Citation33 give us a total confirmation of no association between the A1298C polymorphism and MTX pharmacokinetics.
None of the other analyzed toxicities (leukopenia, neutropenia, and mucositis with 4 studies; thrombocytopenia and renal toxicity with 3 studies; and neurotoxicity with 1 study) showed statistically significant results ().
The results from 26 articles and 3,546 patients (16 studies with 2,323 patients from the previous meta-analysis and 10 studies with 1,223 patients from our actual review) makes us reject the MTHFR A1298C polymorphism as a MTX toxicity marker.
To sum up, in these 13 new studies analyzing C677T and A1298C and MTX-induced toxicities, we have confirmed our previous results. Most of the studies concluded that there was no association between MTHFR polymorphisms and MTX toxicity, and in those few studies with positive associations, opposite effects were often observed. Therefore, we consider that MTHFR C677T and A1298C polymorphisms are not good toxicity markers in pediatric ALL, and we think that no further studies are needed in this line.
Outcome and MTHFR C677T and A1298C polymorphisms
In 2014, He et alCitation35 published the results of a meta-analysis that studied the relationship between the MTHFR C677T and A1298C polymorphisms and ALL relapse risk. They conducted a literature search of PubMed (www.ncbi.nlm.nih.gov/pubmed) and Web of Knowledge (http://isiknowledge.com/) using the following keywords and subject terms: “acute lymphoblastic leukemia and relapse and polymorphism (variant)” and “methylenetetrahydrofolate reductase (MTHFR) and acute lymphoblastic leukemia and relapse”, last updated on September 2013. The association between the two SNPs and ALL relapse was evaluated in childhood ALL patients. In He et al’sCitation35 work, the meta-analysis for childhood ALL was performed with 6 studies for C677T (n=1,553) and with 3 studies for A1298C (n=711). Significant association was only found for C677T. According to their results, the relapse risk in pediatric ALL was higher for the 677TT genotype than for the CT/CC genotypes.
Simultaneously, Ojha and GurneyCitation36 published a systematic review on the association between MTHFR C677T and overall survival in pediatric ALL (n=909). The search included literature through March 2013, and the review was based on 6 studies, 3 of them already included on He et al’ s,Citation35 meta-analysis. As expected, they reached a similar conclusion, individuals with MTHFR 677T variant showed a higher relative risk of pediatric ALL mortality, with greater statistical support for the genotype MTHFR 677TT.
Herein, we performed a new review of the literature published after the mentioned two reviews, from September 2013 to November 2016, to assess the relationship between childhood ALL outcome and MTHFR C677T and A1298C polymorphisms. Keywords “MTHFR” and “acute lymphoblastic leukemia” for PubMed database were used.
The study selection process, previously described for toxicity studies, was the same for outcome in the first steps. Out of the 15 articles selected for complete lecture, 7 were discarded, 2 for being published before 2013 and 5 for not studying outcome. Finally, we analyzed 8 articles that studied the MTHFR polymorphisms in relation to pediatric ALL patients outcome ().
C677T polymorphism analysis
From 2013, eight studies that included 1,353 pediatric ALL patients have analyzed the association between the C677T polymorphism and outcome (relapse, death, or secondary malignancy). None of the new eight studies showed significant association between outcome and C677T variant (). These results differ from the previously mentioned reviews that found association between increased relapse/mortality risk and 677TT genotype. Nevertheless, in the He et al’s,Citation35 meta-analysis, the significant result is based only in two studies (D’Angelo et alCitation37 and Tantawy et alCitation38) from the 6 studies included. Taking all these results in consideration, we cannot affirm that MTHFR C677T polymorphism is a good outcome marker for pediatric ALL.
Table 5 List of 8 studies that analyzed association between the MTHFR C677T polymorphism and outcome
A1298C polymorphism analysis
In the case of A1298C, six new studies that included 1,104 pediatric ALL patients analyzed the association with outcome (relapse, death, or secondary malignancy). From them, 2 studies showed significant results but with opposite effect. Fukushima et alCitation28 demonstrated that individuals with AC-CC genotypes presented increased Event Free Survival (EFS) (versus AA genotype), whereas Radtke et al’sCitation39 study found that individuals with AC or CC genotypes showed decreased EFS (versus AA genotype) (). The other 4 studies showed no association between A1298C and outcome, which is in line with the previously published meta-analysis of He et alCitation35 and other 3 studies. All these results together suggest that MTHFR A1298C polymorphism is not a good predictor for outcome in childhood ALL.
Table 6 List of 6 studies that analyzed association between the MTHFR A1298C polymorphism and outcome
In conclusion, our review indicates that MTHFR C677T and A1298C polymorphisms cannot be considered as outcome markers for childhood ALL.
Conclusion
Numerous studies have been performed analyzing the relationship between the C677T and A1298C polymorphisms of MTHFR and MTX toxicity and/or outcome in pediatric ALL. The majority of these studies does not find association or present opposite effect. As a result, MTHFR C677T and A1298C polymorphisms cannot be considered as toxicity or outcome markers for childhood ALL. Therefore, the efforts should be focused on other genes. For instance, interesting and robust results have been obtained in regards to transporter genes and MTX toxicity. In fact, Treviño et alCitation40 performed a genome-wide association study in patients with ALL and found rs4149081 and rs11045879 in SLCO1B1 strongly associated for the first time with MTX clearance, and this association was widely confirmed by subsequent studies.Citation11,Citation39,Citation41 As a result, other works have focused their interest on the analysis of polymorphism in MTX transporters, finding several SNPs in genes such as SLC19A1, ABCC4, or ABCC2 also associated with MTX levels and other toxicities.Citation42–Citation44
Additionally, miRNA-related SNPs interfering with miRNA levels or function may lead to drug resistance/sensitivity. Since miRNA expression can be exogenously controlled by blocking the expression of upregulated miRNAs or by restoring the expression of downregulated miRNAs, this field seems very promising in pharmacogenetics. Indeed, our group has detected 3 SNPs in miR-5189, miR-595, and miR-453 that might affect SLC46A1, SLC19A1, SLCO1A2, and ABCC4 MTX transport genes regulation and could affect MTX levels in patients with pediatric B-ALL.Citation45,Citation46
Disclosure
The authors report no conflicts of interest in this work.
References
- KoppenIHermansFKaspersGFolate related gene polymorphisms and susceptibility to develop childhood acute lymphoblastic leukaemiaBr J Haematol200914831419775302
- JohnstonWTLightfootTJSimpsonJRomanEChildhood cancer survival : a report from the United Kingdom Childhood Cancer StudyCancer Epidemiol201034665966620674536
- PuiCRobisonLLookAAcute lymphoblastic leukaemiaLancet20083711030104318358930
- GorlickRGokerETrippettRWalthamMBanerjeeDBertinoJIntrinsic and acquired resistance to methotrexate in acute leukemiaN Engl J Med1996335104110488793930
- KrajinovicMMoghrabiAPharmacogenetics of methotrexatePharmacogenomics20045781983415469405
- De MattiaEToffoliGC677T and A1298C MTHFR polymorphisms, a challenge for antifolate and fluoropyrimidine-based therapy personalisationEur J Cancer20094581333135119144510
- CheokMEvansWAcute lymphoblastic leukaemia: a model for the pharmacogenomics of cancer therapyNat Rev Cancer20066211713016491071
- FrosstPBlomHMilosRA candidate genetic risk factor for vascular disease: a common mutation in methylenetetrahydrofolate reductaseNat Genet19951011111137647779
- WeisbergIJacquesPSelhubJThe 1298A/C polymorphism in methylenetetrahydrofolate reductase (MTHFR): in vitro expression and association with homocysteineAtherosclerosis2001156240941511395038
- NiedzielskaEWęcławek-TompolJMatkowska-KocjanAChybickaAThe influence of genetic RFC1, MS and MTHFR polymorphisms on the risk of acute lymphoblastic leukemia relapse in children and the adverse effects of methotrexateAdv Clin Exp Med2013224579584 Available from: http://www.ncbi.nlm.nih.gov/pubmed/2398621923986219
- Lopez-LopezEMartin-GuerreroIBallesterosJPolymorphisms of the SLCO1B1 gene predict methotrexate-related toxicity in childhood acute lymphoblastic leukemiaPediatr Blood Cancer201157461261921387541
- Lopez-LopezEGutierrez-CaminoABilbao-AldaiturriagaNPombar-GomezMMartin-GuerreroIGarcia-OradAPharmacogenetics of childhood acute lymphoblastic leukemiaPharmacogenomics201415101383139825155938
- EstellerMAberrant DNA methylation as a cancer-inducing mechanismAnnu Rev Pharmacol Toxicol20054562965615822191
- AbeMOhiraMKanedaACpG island methylator phenotype is a strong determinant of poor prognosis in neuroblastomasCancer Res200565382883415705880
- Lopez-LopezEMartin-GuerreroIBallesterosJGarcia-OradAA systematic review and meta-analysis of MTHFR polymorphisms in methotrexate toxicity prediction in pediatric acute lymphoblastic leukemiaPharmacogenomics J201313649850623089671
- YangLHuXXuLImpact of methylenetetrahydrofolate reductase (MTHFR) polymorphisms on methotrexate-induced toxicities in acute lymphoblastic leukemia: a meta-analysisTumor Biol201267714451454
- YanagimachiMGotoHKanekoTInfluence of pre-hydration and pharmacogenetics on plasma methotrexate concentration and renal dysfunction following high-dose methotrexate therapyInt J Hematol201398670270724241962
- TorunYAPatirogluTOzdemirMAOzkulYEkiciAKarakukcuMInherited prothrombotic risk factors in Turkish children with acute lymphoblastic leukemia: significance of concomitant genetic mutationClin Appl Thromb Hemost201218221822121873357
- SivasliogluSGurselTKocakUKayaZThe risk factors for thrombosis in children with acute lymphoblastic leukemiaClin Appl Thromb Hemost201420665165323364161
- AbdelazizDHElhosseinyNMKhaleelSASabryNAAttiaASEl-SayedMHAssociation between combined presence of Hepatitis C Virus and polymorphisms in different genes with toxicities of methotrexate and 6-mercaptopurine in children with acute lymphoblastic leukemiaPediatr Blood Cancer20166391539154527163515
- TanakaYManabeANakadateHMethylenetetrahydrofolate reductase gene haplotypes affect toxicity during maintenance therapy for childhood acute lymphoblastic leukemia in Japanese patientsLeuk Lymphoma20145551126113123865834
- KaluznaEStraussEZajac-SpychalaOFunctional variants of gene encoding folate metabolizing enzyme and methotrexate-related toxicity in children with acute lymphoblastic leukemiaEur J Pharmacol2015769939926528799
- Karas KuzelickiNMilekMJazbecJMlinaric-RascanI5,10-Methylenetetrahydrofolate reductase (MTHFR) low activity genotypes reduce the risk of relapse-related acute lymphoblastic leukemia (ALL)Leuk Res200933101344134819178944
- Ramírez-PachecoAMoreno-GuerreroSAlamilloIMedina-SansonALopezBMoreno-GalvanMMexican childhood acute lymphoblastic leukemia: a pilot study of the MDR1 and MTHFR gene polymorphisms and their associationsGenet Test Mol biomrkers20162010597602
- HaaseRElsnerKStiefelMMauz-KorholzCKrammCKorholzDHigh dose methotrexate treatment in childhood ALL : pilot study on the impact of the MTHFR 677C > T and 1298A > C polymorphisms on MTX-related toxicityKlin Pädiatrie20122243156159
- AráozHAloiKFoncubertaMPharmacogenetic studies in children with acute lymphoblastic leukemia in Argentina Pharmacogenetic studies in children with acute lymphoblastic leukemia in ArgentinaLeuk Lymphoma20155651370137825110820
- ZgheibNAkra-IsmailMAridiCGenetic polymorphisms in candidate genes predict increased toxicity with methotrexate therapy in Lebanese children with acute lymphoblastic leukemiaPharmacogenet Genomics201424838739625007187
- FukushimaHFukushimaTSakaiAPolymorphisms of MTHFR associated with higher relapse/death ratio and delayed weekly MTX administration in pediatric lymphoid malignanciesLeuk Res Treatment2013201319
- ImanishiHOkamuraNYagiMGenetic polymorphisms associated with adverse events and elimination of methotrexate in childhood acute lymphoblastic leukemia and malignant lymphomaJ Hum Genet200752216617117180579
- SuzukiRFukushimaHNoguchiEInfluence of SLCO1B1 polymorphism on maintenance therapy for childhood leukemiaPediatr Int201557457257725939871
- MoulikNKumarAAgrawalSMahdiAKumarAEffect of folate status and methylenetetrahydrofolate reductase genotypes on the complications and outcome of high dose methotrexate chemotherapy in north Indian children with acute lymphoblastic leukemiaIndian J Med Paediatr Oncol2016372858927168705
- YazicioğluBKayaZErgunSInfluence of folate-related gene polymorphisms on high-dose methotrexate-related toxicity and prognosis in Turkish children with Acute Lymphoblastic LeukemiaTurkish J Hematol2016219
- KantarMKosovaBCetingulNMethylenetetrahydrofolate reductase C677T and A1298C gene polymorphisms and therapy-related toxicity in children treated for acute lymphoblastic leukemia and non-Hodgkin lymphomaLeuk Lymphoma200950691291719391036
- KarathanasisNVStiakakiEGoulielmosGNKalmantiMThe role of the methylenetetrahydrofolate reductase 677 and 1298 polymorphisms in Cretan children with acute lymphoblastic leukemiaGenet Test Mol Biomarkers2011151–251021117954
- HeHChenSYouHAssociation between methylenetetrahydrofolate reductase polymorphisms and the relapse of acute lymphoblastic leukemia: a meta-analysisPharmacogenomics J201414543243824637499
- OjhaRPGurneyJGMethylenetetrahydrofolate reductase C677T and overall survival in pediatric acute lymphoblastic leukemia: a systematic reviewLeuk Lymphoma2014551677323550988
- D´AngeloVRamagliaMIannottaAMethotrexate toxicity and efficacy during the consolidation phase in paediatric acute lymphoblastic leukaemia and MTHFR polymorphisms as pharmacogenetic determinantsCancer Chemother Pharmacol20116851339134621590445
- TantawyAEl-BostanyEAdlyAMethylene tetrahydrofolate reductase gene polymorphism in Egyptian children with acute lymphoblastic leukemiaBlood Coagul Fibrinolysis2010211283419923983
- RadtkeSZolkORennerBGermline genetic variations in methotrexate candidate genes are associated with pharmacokinetics, toxicity, and outcome in childhood acute lymphoblastic leukemiaBlood J20131212651455154
- TreviñoLShimasakiNYangWGermline genetic variation in an organic anion transporter polypeptide associated with methotrexate pharmacokinetics and clinical effectsJ Clin Oncol200927355972597819901119
- RamseyLBPanettaJCSmithCGenome-wide study of methotrexate clearance replicates SLCO1B1Blood2013121689890423233662
- Lopez-LopezEBallesterosJPinanMAPolymorphisms in the methotrexate transport pathway: a new tool for MTX plasma level prediction in pediatric acute lymphoblastic leukemiaPharmacogenet Genomics2013232536123222202
- den HoedMALopez-LopezEte WinkelMLGenetic and metabolic determinants of methotrexate-induced mucositis in pediatric acute lymphoblastic leukemiaPharmacogenomics J201515324825425348617
- Gutierrez-CaminoALopez-LopezEGarcia-OradASLC19A1 hot spot for MTX plasma concentrationMed Oncol2014311020425178938
- IparraguirreLGutierrez-CaminoAUmerezMMiR-pharmacogenetics of methotrexate in childhood B-cell acute lymphoblastic leukemiaPharmacogenet Genomics2016261151752527649261
- Lopez-LopezEGutierrez-CaminoAPinanMAPharmacogenetics of microRNAs and microRNAs biogenesis machinery in pediatric acute lymphoblastic leukemiaPLoS One201493e9126124614921
- TsujimotoSTanakaFYanagimachiMInfluence of ADORA2A gene polymorphism on leukoencephalopathy risk in MTX-treated pediatric patients affected by hematological malignanciesPediatr Blood Cancer2016631983198927399166
- WangSSunLZengWWuWZhangGInfluence of genetic polymorphisms of FPGS, GGH, and MTHFR on serum methotrexate levels in Chinese children with acute lymphoblastic leukemiaCancer Chemother Pharmacol20147428328924908438
- de DeusDde LimaESeabra SilvaRLeiteECartaxo MunizMInfluence of methylenetetrahydrofolate reductase C677T, A1298C, and G80A polymorphisms on the survival of pediatric patients with acute lymphoblastic leukemiaLeuk Res Treatment2012201216
- KimHKangHKimHPharmacogenetic analysis of pediatric patients with acute lymphoblastic leukemia: a possible association between survival rate and ITPA polymorphismPLoS One201279110
- LeonardiDAbbateMRiccheriMImproving risk stratification of patients with childhood acute lymphoblastic leukemia: glutathione-S-transferases polymorphisms are associated with increased risk of relapseOncotarget2016518
- HoangPAmbroiseJDekairelleAComparative pharmacogenetic analysis of risk polymorphisms in Caucasian and Vietnamese children with acute lymphoblastic leukemia: prediction of therapeutic outcome?Br J Clin Pharmacol201579342944025099492