Abstract
Objective. To describe the prevalence, awareness, and control of hypertension in a Swedish population during the early 2000s to address implications for care and prevention. Design. A cross-sectional population survey. Setting. Primary health care in Skaraborg, a rural part of western Sweden. Subjects. Participants (n =2816) in a population survey of a random sample of men and women between 30 and 75 years of age in the municipalities of Vara (81% participation rate) and Skövde (70%), in western Sweden during 2001–2005. Main outcome measures. Anthropometric measures, blood pressure, leisure-time physical activity, current smoking, fasting glucose, and cholesterol. Hypertension was defined as ongoing treatment for hypertension, or three consecutive blood pressure readings ≥140 systolic and/or ≥90 mmHg diastolic. Hypertension was considered controlled when the blood pressure was <140/90 mm Hg (both). Results. The prevalence of hypertension was 20% in both men and women with a steep increase by age. Among hypertensive subjects, 33% were unaware, 36% aware but uncontrolled, and 31% aware and controlled, with no statistically significant differences between men and women. Patients with diabetes had a higher awareness (87% vs. 64%, p <0.001), but the same control rate (56% vs. 44%, p =0.133), when compared with those without diabetes. Conclusion. A large proportion of subjects with hypertension are still unaware of their condition, or aware but not controlled. It is important to emphasize population-based prevention to reduce the prevalence of hypertension, to perform screening to increase awareness, and to improve implementation of expert guidelines in clinical practice to improve control.
Using strict measures of blood pressure we found the prevalence of hypertension in the ages 30–75 years in Sweden to be 20%.
A rule of thirds evolved as 1/3 was not previously known, 1/3 was treated but not controlled, and only 1/3 was treated and controlled.
It is important to emphasize population-based prevention to reduce the prevalence of hypertension, to perform screening to increase awareness, and to improve implementation of expert guidelines in clinical practice to improve control.
Introduction
Hypertension is a common condition strongly associated with cardiovascular morbidity and mortality [Citation1,Citation2]. As lowering high blood pressure significantly reduces the mortality rate and risk of CVD events [Citation1], it is vital to identify people with hypertension and control their blood pressure in order to avoid complications and thereby prevent increasing societal costs as well as personal suffering. This is even more important for individuals with diabetes as they run a higher risk of cardiovascular complications [Citation2].
In some older studies, only half of the hypertensive subjects were aware of their high blood pressure, half of the patients who were aware were treated, and only half of those treated were adequately controlled, coining the phrase “the rule of halves” [Citation3–5]. Though recent studies have shown an improvement in other countries [Citation6,Citation7], we aimed to find out whether the “half rule” still applied in Sweden by describing the prevalence, awareness, and control rates of hypertension among the participants of the Skaraborg Project during 2001–2005. By applying strict and systematic methodological procedures, including repeated blood pressure measurements, our results should be more reliable than previous population-based, one-visit studies in similar populations. Thus, our aim was to provide more up-to-date knowledge for clinicians and providers of primary health care.
Material and methods
Subjects
This study was based on a survey conducted in 2001–2005 of the populations in Vara and Skövde, two small municipalities in south-western Sweden. Men and women aged 30–75 years were randomly sampled, and 2816 of those invited participated (81% and 70% in Vara and Skövde, respectively) [Citation8]. All participants gave signed informed consent before being enrolled in the study, and the Ethical Committee at the University of Gothenburg, Sweden, approved the study.
Methods
Two specially trained nurses collected the information as previously described in detail [Citation8]. Participants completed forms on medical history and lifestyles, including smoking habits and physical activity. Blood samples were collected and an oral glucose tolerance test (OGTT) was conducted on all subjects without known diabetes [Citation8]. All ongoing medications were documented, and physical examinations included waist circumference, body weight (nearest 0.1 kg on a calibrated scale), height (nearest cm), and heart rate. Blood pressure was measured in a supine position with the arm (supported by a pillow) at heart level after a five-minute rest, using Tricuff™ for automatic adjustment of cuff size to arm circumference [Citation9]. The mean value from two measurements with a one-minute interval was used.
Hypertension was diagnosed in accordance with national and international guidelines [Citation1,Citation2]. For definite hypertension, three consecutive high readings with four-week intervals were requested (≥140 systolic and/or ≥90 mmHg diastolic), or the participant had a known diagnosis with ongoing treatment. Hypertension was considered controlled when the systolic blood pressure was <140 mm Hg, and the diastolic blood pressure was ≤90 mm Hg. Self-reported leisure-time physical activity (LTPA) was measured using the validated question, “How much physical activity do you engage in during your leisure time?” [Citation10]. The question referred to the past year and had four alternative answers: (1) sedentary, (2) some, (3) moderate, or (4) heavy activity, respectively. LTPA was dichotomized into low LTPA (1+2) and active LTPA (3+4). Educational level was examined by a question with 10 alternatives ranging from primary school to PhD exams. Current smoking was defined as daily smoking (yes/no). General obesity was characterized by body mass index (BMI). BMI was estimated using the formula body weight (kg) divided by the square of body height in meters (m2). Participants were defined as obese when BMI ≥30 kg m−2, and overweight if BMI ≥25 kg m−2 but <30 kg m−2.
Statistics
All statistical analyses were done using the SPSS software package for Mac, version 19.0. Direct standardization was used for prevalences to account for the age distribution in the background population. All tests were two-sided and statistical significance was assumed at p <0.05. Standard methods were used for descriptive statistics. For comparison between groups in categorical variables, either a chi-squared test for bivariate analyses, or multiple binary logistic regression with associations expressed as odds ratios (OR) with 95% confidence intervals (CI) was used. General linear models (GLM) were used to estimate differences in means of continuous variables and were presented with 95% CI. To adjust for possible contextual differences between the municipalities of Vara and Skövde, and for differences in lifestyle between residents in these municipalities, we included study site as a covariate in all analyses for and .
Table I. Study characteristics of men and women participating in the Vara-Skövde population survey 2001–2005.
Table II. Comparison of common cardiovascular disease risk factors between categories of hypertension in men and women using aware controlled hypertension as reference: The Vara-Skövde Cohort 2001–2005 within the Skaraborg Project.
Results
In sum, 415 participants (209 males and 206 females) were defined as hypertensive. Characteristics of the study population are shown in . The overall age-standardized prevalence was 20.1% (women 20.4%, men 19.9%). If only the blood pressure measured at the study visit was considered for new cases of hypertension, the total prevalence would have increased to 26.1%. Of all those diagnosed with hypertension, 137 subjects (33%) were unaware of their high blood pressure, whereas 278 subjects (67%) had been diagnosed earlier. Among patients aware of their hypertension, less than half (46%) had adequately controlled blood pressure at the study visit (31% of all subjects with hypertension).
Among those aware of their condition, the proportion of controlled hypertension was 49% in men and 44% in women (p =0.358). Patients with known type 2 diabetes had significantly higher awareness (87% vs. 64%, p <0.001), but similar control rate (56% vs. 44%, p =0.133), when compared with those without diabetes.
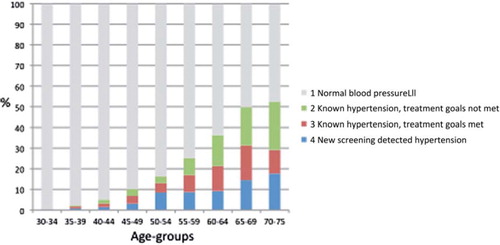
As seen in the prevalence of hypertension increased sharply with age, ranging from under 2% in the youngest subjects (30–34 years) to over 50% in those older than 65 years (p <0.001 in both sexes). While the distribution between aware/controlled, aware/uncontrolled, and new hypertension did not vary significantly by five-year age groups, both awareness and new hypertension increased with age, while control in subjects aware of their hypertension declined (all p <0.001). In the oldest five-year age group, 23% of the hypertensive men were adequately controlled versus 21% among the women.
Figure 1. Proportions of normal blood pressure (1), known hypertension, treatment goals not met (2), known hypertension, treatment goals met (3), and new screening detected hypertension (4), respectively: Distribution by five-year age groups in men and women combined in the Vara-Skövde cohort 2001–2005.
Blood pressure levels in aware men with controlled hypertension did not differ significantly from normotensive men, while they were still significantly higher in corresponding women (). In both genders, general and abdominal obesity were more common, and fasting plasma glucose was higher, in all categories with hypertension compared with those with normal blood pressure (data not shown). As seen in , traditional determinants for hypertension were significantly associated with known hypertension independent of age and sex. However, none of these factors discriminated between those with controlled and uncontrolled hypertension.
Figure 2. Factors related to known hypertension in the Vara-Skövde cohort 2001–2005: Associations estimated by logistic regression entering age and study site as covariates and expressed as odds ratios (OR) with 95% confidence intervals.
In men, current smoking was less common among those aware of their hypertension (7% vs. 16%), and more had quit smoking (56% vs. 33%), p <0.001. Corresponding proportions in women were 16% vs. 21%, and 31% vs. 27%, respectively, p =0.315.
Discussion
As many as 20% of both men and women were found to have manifest hypertension, and this is therefore a major public health issue. In general, one-third were not previously identified, and of those aware and treated only about one-half fulfilled recommended blood pressure targets consistent with the “rule of halves”. Overall, however, this pattern would most likely be described today as a rule of thirds rather than a rule of halves. This pattern was consistent throughout the age distribution.
A major strength of this study was the high participation rates, which give the results a high reliability. It is still likely that individuals with chronic diseases or health problems prior to the study would be more reluctant to participate than healthy people, as often seen in other surveys. Nevertheless, this is not likely to have had a considerable impact on the observed prevalence. Another strength of the study was the accurate blood pressure measurements. For all new cases of hypertension three consecutive high measurements were required for diagnosis, thus limiting the risk of overestimating unaware hypertension due to randomly high blood pressure levels. Furthermore, at the outset of the survey, two study nurses who were well educated and experienced in the care of both hypertension and diabetes reviewed the participants’ background and medical history. We used a device for automatic adjustment of cuff size for the individual arm that should reduce the overestimation of hypertension in overweight/obese patients seen when they are exposed to a normal-sized cuff [Citation11]. Accordingly, the prevalence might be lower in our study than in other epidemiological studies often based on only one screening blood pressure, but still more accurate. While we measured blood pressure in a supine position, it has internationally long been recommended to have the patient in a sitting position. Though it is well known that both body and arm position influence blood pressure measurements, studies to compare these methods have in fact given contradictory and inconsistent results as reviewed by Netea et al. [Citation12]. Furthermore, in their expert recommendations the European Society of Hypertension state that despite a general tendency for the blood pressure to be lower in a sitting compared with a supine position, posture is unlikely to lead to a significant error in blood pressure measurements in most people, provided that the arm is supported at heart level [Citation13]. We considered these points; accordingly, our results should be comparable to studies measuring blood pressure in a sitting position.
Similar to the Intergene study, we confirmed the association between traditional risk factors for high blood pressure and prevalent hypertension. In contrast, we did not find duration of education to be significantly associated with hypertension. However, their study population was collected in urban Gothenburg with a higher proportion of people with higher education and with a wider range in the duration of education. Consequently, the power to find an association may have been lower in rural Skaraborg; therefore, the possibility of a type 2 error cannot be excluded here. All patients with a blood pressure less than 140/90 were considered well treated in this study, despite the fact that some patients may have lower treatment goals because of diabetes, kidney disease, or ischaemic heart disease [Citation1,Citation2]. In a national sample within the Swedish Diabetes Registry, 33.3% reached a blood pressure goal of ≤140/85 mm Hg, while only 9.4% achieved a blood pressure <130/85 mm Hg, which is the goal set for hypertension in diabetes [Citation14]. Considering the prevalence of diabetes among patients with hypertension, the control rate of hypertension would have been even worse than what we found had we considered accurate blood pressure goals in hypertensive patients with diabetes.
Many studies on the prevalence, treatment, and control of hypertension are based on cross-sectional one-visit surveys. The considerable intra-individual variation in blood pressure, rather than a white coat effect, is known to cause an overestimation in the prevalence of hypertension, and a corresponding underestimation of treatment of hypertension [Citation15,Citation16]. Accordingly, most comparable studies reported higher prevalence of hypertension and lower rate of treatment than in our cohort as seen in the Västerbotten Intervention Program (VIP) study on a study population of 59 735 participants in northern Sweden in 2002 [Citation17]. A smaller study restricted to 60-year-old men and women in Stockholm showed a similar pattern but yet a higher prevalence and lower control than in the VIP study, probably explained by higher age [Citation18]. Also in other European countries the prevalence of hypertension was relatively high (Czech Republic 39% [Citation19], Greece 31% [Citation20]), compared with the Vara and Skövde Cohort (VSC). Similarities were found in comparison with the Netherlands where the prevalence of hypertension was 23% [Citation21]. In the USA, the NHANES 1999–2004 reported a prevalence of 29% in the population older than 18 years based on two study visits for verification of diagnosis and control of hypertension [Citation22], thus similar to Skaraborg. Though this is a higher rate than in Skaraborg, prevalence and control rates were similar in corresponding age levels. This is inconsistent with many other studies where European countries had a higher prevalence of hypertension compared with the USA [Citation23]. This might be explained by differences in design and age bands between studies.
It has been argued that the global risk score should be accounted for when treatment and control of hypertension are discussed, as mild hypertension at low risk should be treated non-pharmacologically [Citation2,Citation21,Citation24,Citation25]. The control rate of hypertension may then be better than commonly appreciated; however, even with the more strict definition of hypertension as used in Skaraborg, the control rate is far from acceptable. Our observation of similar control rates in hypertensive subjects with and without diabetes may be an effect of the physician's recognition of recommendations on more intense treatment in diabetes and other risk categories [Citation2]. This is consistent with the significantly higher awareness in those with diabetes.
Our findings show that today's primary health care does not successfully manage to identify, treat, and control individuals with hypertension despite repeatedly updated expert guidelines [Citation26]. For better control, barriers defined with the patients, the doctors, and within the health care service have to be identified and solved. Though patients’ compliance is discussed as a significant issue [Citation27,Citation28], major responsibility has to be put on the health care and educational systems. In general, the low control rates cannot be blamed on the patients; it is a more systematic problem. As hypertension, in general, comes without symptoms health care providers may easily neglect it in a busy clinic [Citation29]. Structured care programmes for hypertension have previously and recently been found effective [Citation30–32], but are not often used in primary care today. Pay for performance has been suggested to improve quality of health care [Citation33]; however, a recent publication on the effect of a change in the funding of primary care in the UK did not support that [Citation34]. This may, however, be better studied in controlled interventions. However, according to Rose, the optimal effect will be achieved by combining primary prevention in a population strategy with identification of individuals at high risk for individual care [Citation35].
We found strong associations between traditional risk factors for hypertension and current hypertension in Skaraborg; however, all these factors, including type 2 diabetes, failed to distinguish between controlled and uncontrolled hypertension. This might partly be explained by an increasing consideration of global risk in the management of hypertension. There is a strong need for future studies on the mechanisms of uncontrolled hypertension.
Acknowledgements
The Skaraborg Project received financial support from: the National Research Foundation Council (VR), Sweden; Sahlgrenska Academy; University of Gothenburg; the Skaraborg Institute in Skövde, Sweden; Skaraborg Primary Care, Sweden; the Health & Medical Care Committee of the Regional Executive Board of the Region Västra Götaland, Sweden; Malmö University Hospital, Sweden; Region Skåne, Sweden; and Faculty of Medicine, Lund University, Sweden.
Declaration of interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the paper.
References
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, . The seventh report of the joint national committee on prevention, detection, evaluation and treatment of high blood pressure. JAMA 2003;289: 2560–72.
- Guidelines Sub-Committee. 1999 World Health Organization: International Society of Hypertension guidelines for the management of hypertension. J Hypertens 1999;17: 151–83.
- Wilber JA, Barrow JG. Hypertension: A community problem. Am J Med 1972;52:653–63.
- Hart JT. Semicontinuous screening of a whole community for hypertension. Lancet 1970;2:223–6.
- Smith WC, Lee AJ, Crombie IK, Tunstall-Pedoe H. Control of blood pressure in Scotland: The rule of halves. BMJ 1990;300:981–3.
- Marques-Vidal P, Tuomilehto J. Hypertension awareness, treatment and control in the community: Is the “rule of halves” still valid? J Hum Hypertens 1997;11:213–20.
- Antikainen RL, Moltchanov VA, Chukwuma C Sr, Kuulasmaa KA, Marques-Vidal PM, Sans S, . Trends in the prevalence, awareness, treatment and control of hypertension: The WHO MONICA Project. Eur J Cardiovasc Prev Rehabil 2006;13:13–29.
- Larsson CA, Gullberg B, Rastam L, Lindblad U. Salivary cortisol differs with age and sex and shows inverse associations with WHR in Swedish women: A cross-sectional study. BMC Endocrine Disorders 2009;9:16. PMID: 19545400.
- Råstam L, Sjönell G. A new device for measuring blood pressure in adults. Lancet 1991;337:249–50.
- Løchen ML, Rasmussen K. The Tromsø study: Physical fitness, self reported physical activity, and their relationship to other coronary risk factors. J Epidemiol Community Health 1992;46:103–7.
- Stolt M, Sjönell G, Aström H, Hansson L. The reliability of auscultatory measurement of arterial blood pressure: A comparison of the standard and a new methodology. Am J Hypertens 1990;3:697–703.
- Netea RT, Lenders JW, Smits P, Thien T. Influence of body and arm position on blood pressure readings: An overview. J Hypertens 2003;21:237–41.
- European Society of Hypertension working group on blood pressure monitoring. European Society of Hypertension recommendations for conventional, ambulatory and home blood pressure measurement. J Hypertension 2003;21: 821–48.
- Nilsson PM, Gudbjörnsdottir S, Eliasson B, Cederholm J. Steering Committee of the National Diabetes Register, Sweden. Hypertension in diabetes: Trends in clinical control in repeated large-scale national surveys from Sweden. J Hum Hypertens 2003;17:37–44.
- Klungel OH. Quality of hypertension treatment and risk of stroke in the general population. J Hypertens 2002;20: 1949–50.
- Mancia G, Sega R, Milesi C, Cesana G, Zanchetti A. Blood-pressure control in the hypertensive population. Lancet 1997;349:454–7.
- Weinehall L, Öhgren B, Persson M, Stegmayr B, Boman K, Hallmans G, . High remaining risk in poorly treated hypertension: The “rule of halves” still exists. J Hypertens 2002;20:2081–8.
- Carlsson AC, Wändell PE, Journath G, de Faire U, Hellénius ML. Factors associated with uncontrolled hypertension and cardiovascular risk in hypertensive 60-year-old men and women: A population-based study. Hypertens Res 2009; 32:780–5.
- Cífková R, Skodová Z, Lánská V, Adámková V, Novozámská E, Petrzílková Z, . Trends in blood pressure levels, prevalence, awareness, treatment, and control of hypertension in the Czech population from 1985 to 2000/01. J Hypertens 2004;22:1479–85.
- Efstratopoulos AD, Voyaki SM, Baltas AA, Vratsistas FA, Kirlas DE, Kontoyannis JT, . Prevalence, awareness, treatment and control of hypertension in Hellas, Greece: The Hypertension Study in General Practice in hellas (HYPERTENSHELL) national study. Am J Hypertens 2006;19:53–60.
- Scheltens T, Bots ML, Numans ME, Grobbee DE, Hoes AW. Awareness, treatment and control of hypertension: The “rule of halves” in an era of risk-based treatment of hypertension. J Hum Hypertens 2007;21:99–106.
- Cutler JA, Sorlie PD, Wolz M, Thom T, Fields LE, Roccella EJ. Trends in hypertension prevalence, awareness, treatment and control rates in United States adults between 1988–1994 and 1999–2004. Hypertension 2008;52:818–27.
- Wolf-Maier K, Cooper RS, Kramer H, Banegas JR, Giampaoli S, Joffres MR, . Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension 2004;43:10–7.
- Barroso LC, Muro EC, Herrera ND, Ochoa GF, Hueros JI, Buitrago F. Performance of the Framingham and SCORE cardiovascular risk prediction functions in a non-diabetic population of a Spanish health care centre: A validation study. Scand J Prim Health Care 2010;28:242–8. Epub 2010 Sep 27.
- Conroy RM, Pyörälä K, Fitzgerald AP, Sans S, Menotti A, De Backer G, . SCORE project group. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur Heart J 2003;24:987–1003.
- Van der Wel M, Bakx C, de Grauw W, van Gerwen W, Mulder J, van Weel C. The influence of guideline revisions on the process and outcome of hypertension management in general practice: A descriptive study. Eur J Gen Pract 2008;14(Suppl 1):47–52.
- Corrao G, Parodi A, Nicotra F, Zambon A, Merlino L, Cesana G, . Better compliance to antihypertensive medications reduces cardiovascular risk. J Hypertens 2011; 29:610–8.
- Mazzaglia G, Ambrosioni E, Alacqua M, Filippi A, Sessa E, Immordino V, . Adherence to antihypertensive medications and cardiovascular morbidity among newly diagnosed hypertensive patients. Circulation 2009;120:1598–605.
- Midlöv P, Ekesbo R, Johansson L, Gerward S, Persson K, Nerbrand C, Hedblad B. Barriers to adherence to hypertension guidelines among GPs in southern Sweden: A survey. Scand J Prim Health Care 2008;26:154–9.
- Råstam L, Berglund G, Isacsson SO, Rydén L. The Skaraborg hypertension project, III: Influence on blood pressure of a medical care program for hypertension. Acta Med Scand 1986;219:261–9.
- Eckerlund I, Jonsson E, Rydén L, Råstam L, Berglund G, Isacsson SO. Economic evaluation of a Swedish medical care program for hypertension. Health Policy 1985;5:299–306.
- Voogdt-Pruis HR, Beusmans GH, Gorgels AP, Kester AD, Van Ree JW. Br J Gen Pract. Effectiveness of nurse-delivered cardiovascular risk management in primary care: A randomised trial. 2010;60:40–6.
- Petersen L, Woodard L, Urech T, Daw C, Sookanan S. Does pay for performance improve the quality of health care? Ann Intern Med 2006;145:265–72.
- Serumaga B, Ross-Degnan D, Avery AJ, Elliott RA, Majumdar SR, Zhang F, . Effect of pay for performance on the management and outcomes of hypertension in the United Kingdom: Interrupted time series study. BMJ 2011;342:d108. doi: 10.1136/bmj.d10.
- Rose G. The strategy of preventive medicine. Oxford: Oxford University Press; 1992.
