Abstract
Purpose. We have tested a procedure of focal injection of the contrast medium Lipiodol as a fiducial marker for image-guided boost of the tumor in bladder cancer radiotherapy (RT). In this study, we have evaluated the feasibility and the safety of the method as well as the inter- and intra-fraction shift of the bladder tumor. Materials and methods. Five patients with muscle invasive urinary bladder cancer were included in the study. Lipiodol was injected during flexible cystoscopy into the submucosa of the bladder wall at the periphery of the tumor or the post resection tumor-bed. Cone-beam CT (CBCT) scans were acquired daily throughout the course of RT. Results. Lipiodol demarcation of the bladder tumor was feasible and safe with only a minimum of side effects related to the procedure. The Lipiodol spots were visible on CT and CBCT scans for the duration of the RT course. More than half of all the treatment fractions required a geometric shift of 5 mm or more to match on the Lipiodol spots. The mean intra-fraction shift (3D) of the tumor was 3 mm, largest in the anterior-posterior and cranial-caudal directions. Conclusion. This study demonstrates that Lipiodol can be injected into the bladder mucosa and subsequently visualized on CT and CBCT as a fiducial marker. The relatively large inter-fraction shifts in the positions of Lipiodol spots compared to the intra-fraction movement indicates that image-guided RT based on radio-opaque markers is important for RT of the bladder cancer tumor.
The balance between local tumor control and risk of normal tissue morbidity is the key challenge in curative radiotherapy (RT) of bladder cancer. Local tumor control after RT remains poor while the risk of treatment related side effects is relatively high [Citation1,Citation2].
The shape and position of the bladder changes considerably during the course of RT due to variation in the filling of the bladder and rectum [Citation3]. This reduces the precision with which the radiation dose can be delivered to the tumor. There is a high risk of geographic miss which may impair local tumor control. Consequently, large margins are added to compensate for internal organ movements and positioning errors [Citation4]. Unfortunately, this leads to irradiation of large volumes of normal tissue to a high dose level which increases the risk of radiation induced normal tissue reactions.
Efforts to reduce the margins without compromising target coverage have lead to increased focus on image-guided radiotherapy (IGRT). IGRT involves frequent imaging/localization of the target and treatment verification during the course of RT. Imaging typically involves the acquisition of two orthogonal 2D-kV images or 3D volumetric cone-beam CT (CBCT) image sets. Using IGRT techniques the target position can be adjusted online according to bone or soft-tissue anatomy, or according to implanted fiducial markers. The potential benefit of IGRT is to reduce margins and the treatment related side effects which may allow subsequent dose escalation and thereby improvement of local tumor control. In prostate cancer, the use of IGRT based on implanted fiducial markers has allowed an escalation of the radiation dose which has improved the outcome [Citation5,Citation6]. In RT for bladder cancer, daily IGRT based on bony structures is used in many institutions. However, IGRT based on bony structures does not take inter-fraction motion of the bladder and tumor into account.
To implement tumor-directed IGRT boost of bladder cancer, we have investigated the potential of Lipiodol as a liquid radio-opaque fiducial marker when injected into the bladder mucosa adjacent to the tumor. Lipiodol has been used for decades in diagnostic imaging, and there are reports on its use for visualization in RT for prostate cancer and lung cancer [Citation7,Citation8]. Injection of Lipiodol into the bladder mucosa has recently been presented by Pos et al. [Citation9].
In this study, we have tested the feasibility and safety of iodized oil contrast (Lipiodol) demarcation of the bladder tumor. Visibility of the Lipiodol was evaluated on both the planning CT as well as the subsequent 2D-kV and CBCT images during the course of RT. Additionally, we have estimated the inter- and intra-fractional movements of the Lipiodol-labelled bladder tumor during treatment.
Materials and methods
Patients
From May 2008 to January 2009, five patients with T2-3bN0M0 transitiocellular carcinoma of the urinary bladder were included in the study. All patients were considered medical unfit for cystectomy by a multidisciplinary uro-oncological team and were scheduled for radical RT. Protocol exclusion criteria were thyroid disease and a history of adverse reactions to contrast media. The study protocol was approved by The Central Denmark Region Committees on Biomedical Research Ethics and the Danish Medicines Agency and conducted according to Good Clinical Practice.
Lipiodol demarcation of the bladder tumor
The Lipiodol (Lipiodol-ultra fluid®, Laboratoire Guerbet, France) tumor demarcation was performed without anaesthesia in a median of six days (range five to eight days) before the planning CT in an outpatient setting at a urology department. The patients underwent flexible cystoscopy by an experienced urologist after local gel analgesia. After an overview of the tumor site, an injection therapy needle (InterjectTM, Boston Scientific Corporation, One Boston Scientific Place, Natick, MA 01760-1537, USA) was inserted through the working canal to the tip of the cystoscope. Lipiodol was injected into the mucosa at the periphery of the visible bladder tumor or the scar tissue/tumor bed resulting from the initial TUR-B. It was intended to inject four to six Lipiodol spots in the submucosa at the periphery of the tumor, using 0.25–0.50 ml of Lipiodol at each site.
Adverse effect of demarcation technique and RT treatment
Common Terminology Criteria for Adverse Events version 3.0 (CTCAE) was used for prospective scoring of gastrointestinal and genitourinary toxicity.
Treatment planning
All patients had CT-based IMRT plans created in the Eclipse treatment planning system (Varian Medical Systems, Palo Alto (CA)). The treatment planning CT scan was performed using a helical scanner (Philips MX8000 IDT16 or Philips Brilliance Big Bore) with 3 mm slice thickness and reconstructed with 512×512 pixels in the axial plan. Prior to the planning CT and before each treatment fraction the patients were instructed to empty their bladder. Delineation of the clinical target volume (CTV) of the bladder (CTV-B), lymph nodes (CTV-LN) and the rectum was performed in collaboration between a radiation oncologist and a diagnostic radiologist. To account for geometrical and set-up uncertainties, planning target volumes (PTVs) were created from both the CTV-B by adding an an-isotropic margin to the bladder (superior 25 mm, inferior 15 mm, lateral 15 mm, anterior 25 mm and posterior 20 mm) [Citation4] and an isotropic 10–15 mm margin to the CTV-LN. A six-field simultaneous integrated boost IMRT technique was used to deliver 60 Gy (to PTV-B) and 48 Gy (to PTV-LN) in 30 fractions, 5 fraction per week [Citation10].
Online CBCT match on the bony anatomy
The patients were positioned prior to treatment with aid of in-room lasers and skin-marks. Daily kV-CBCT scans were acquired using the Varian On-board Imager (OBI software version 1.3 and 1.4, Varian Medical System, Palo Alto (CA)) system in half-fan mode and reconstructed to 3 mm slice thickness. The CBCT was then on-line matched according to the reference planning CT image. In the match procedure we used a region of interest (ROI) and the Hounsfield unit (HU) intensity range of bone (200–3000 HU) to perform an automated match followed by the corresponding appropriate translational corrections of the treatment couch. A visual check of the automated match was performed by an experienced physicists or physician. For the purpose of this study, the patients also had post-treatment CBCT the first five fractions and post-treatment orthogonal 2D-kV images for all 30 fractions. The post-treatment CBCT scans were used to calculate the changes in intra-fractional bladder volume and changes in Lipiodol marker position.
Offline CBCT match on the Lipiodol
The Lipiodol tumor match was performed on a stand-alone version of the OBI software (OBI v.1.4, Varian Medical System, Palo Alto (CA)). By the off-line match procedure, a Lipiodol volume of interest (L-VOI) was generated in the Eclipse software. The L-VOI consisted of the Lipiodol volume defined by an intensity range of 200–2500 HU and expanded by a 5 mm margin confined inside the bladder. The offline match was then performed as an automated procedure on the L-VOI plus a 1 cm margin. No intensity range was specified in the automated Lipiodol tumor match procedure. Inter-and intra-fractional translational shifts of the Lipiodol tumor were calculated based on match on the pelvic bony anatomy.
Additionally, the volume of the Lipiodol spots (LV) were defined on each CBCT in order to evaluate the change in LV as a function of time. The bladder contour was delineated by the same observer (JS) on all pre and post-treatment CBCT scans. Data were expressed in mean, range and standard deviation (SD) of the measured parameters.
Results
Lipiodol demarcation and imaging
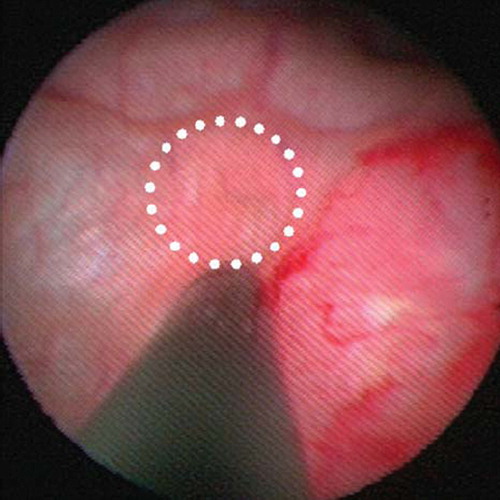
Lipiodol was successfully injected in the periphery of the post TUR-B tumor-bed in four of five patients (). The median time between tumor resection (TUR-B) and Lipiodol injection was 46 days (range 25–98 days). A learning curve for injection of Lipiodol was observed. For patient 1, 0.5 ml Lipiodol was injected at each injection site which resulted in very intense spots on CT and even resulted in artefacts on the CBCT scans. Therefore, it was decided to use a smaller Lipiodol volume (0.25 ml) at each injection site for the remaining patients. In patient 2, part of the Lipiodol was injected into the bladder cavity resulting in dim spots and only one (out of five) spots were visible on the treatment planning CT and CBCT-scans. With this experience in mind we adjusted the injection technique to focus on formation of a small papule at the site of injection (). With the formation of a papule, we had a visual conformation of Lipiodol injection into the mucosa. For the following three patients, the Lipiodol demarcations were clearly visible on CT and CBCT for the full course of RT. On 2D-kV images, only the anterior-posterior projections showed Lipiodol clearly. On the lateral projections the bony structures of the pelvis made visualization of Lipiodol very difficult.
Table I. Lipiodol and bladder measures.
Figure 1. Cystoscopy image of a Lipiodol injection in the bladder mucosa. The tip of the injection needle is in the centre of the picture with the tumor to the right and a formation of an injection papule to the left (white circle).
Although the absolute LVs were different between the patients, the relative loss of Lipiodol from the tissue was quite similar and constant over time. A relative loss of 24% in the LV was observed during the six weeks course of RT ().
Figure 2. The washout of the relative Lipiodol volume during the full radiotherapy course for patients 1 (closed circle), 3 (open circle), 4 (closed triangle) and 5 (open triangle). The Lipiodol volumes were defined on the daily CBCT scans by a fixed HU of 200–2500 confined to the bladder structure.
Adverse effects of Lipiodol demarcation and the RT
The Lipiodol injections and flexible cystoscopy resulted in only mild discomfort during the procedure. Patient 1 experienced a small increase in urinary frequency and patient 2 dysuria grade 1, with all symptoms lasting less than 24 hours. The remaining three patients did not experience any procedure-related side effects.
At baseline, all patients had urinary frequency grade 2 (increase larger than two times normal, but less than hourly), and no bowel symptoms. During the course of RT, patients 2 and 3 experienced diarrhoea grade 2 (increase of 4–6 stools per day over baseline). Patient 5 developed urinary frequency/spasms grade 3 (needed a catheter). One serious adverse event was observed in patient 5 who was hospitalized due to transitory cerebral ischemia grade 3 (expressive dysphasia) lasting less than 5 minutes. This was considered unrelated to the Lipiodol injection and the RT.
Inter- and intra-fraction bladder volume variations
The individual mean bladder volumes as defined by the CBCT scans acquired immediately before the daily treatment session ranged from 82 to 167 cm3. The individual mean increase in bladder volumes based on five measurements per patient ranged from 13 to 34 cm3. The standard deviations were large and varied between patients (). When accounting for time between pre- and post-RT CBCT (mean 16 min, range 15–20 min), this translates into a mean bladder filling rate of 1.3 ml/min. (SD 0.74 ml/min, range 0.4–2.8 ml/min).
Inter- and intra-fraction change in Lipiodol position
Of the 114 pre-treatment CBCT scans, an automated match on the Lipiodol spots was possible in 96% of the situations (). Only when large rotations or changes in bladder volume were present, we had to assist the match procedure manually. After online match on the bony anatomy, inter-fractional shifts of the Lipiodol-spots lead to a 3D geometric mismatch of 5 mm or more in 86%, 63%, 21% and 47% of the fractions for patients 1, 3, 4 and 5, respectively. The average 3D shift for all patients and all fractions was 5 mm (range 0–18 mm). Residual errors of more than 5 mm were present in 6% (left-right, LR), 32% (cranial-caudal, CC), 18% (anterior-posterior, AP) and 54% (3D) of the total number of fractions for all patients. The systematic errors in the LR, CC and AP directions were small. However, large inter-patient and inter-fraction variations were present as illustrated by the standard deviations (). As an example, the couch shifts in the AP direction could vary from −17 mm to +11 mm between fractions in patient 3 ().
Figure 3. Difference between match on bony anatomy and the Lipiodol spots for patient 3. Left-right (closed circle), Cranial-caudal (open circle) and Anterior-posterior (open triangle). A: Inter-fractional shifts for the full course of RT. B: Intra-fractional shifts the first five fractions.
Table II. Inter-fractional translational shifts after offline CBCT match on the Lipiodol spots.
The intra-fractional tumor shifts were considerably smaller than the inter-fractional shifts. The average geometric shift in 3D for all patients ranged from 1 to 6 mm (mean 3 mm). The mean couch shifts needed to correct for tumor-match were −0.3 mm (SD 1), −1 mm (SD 2) and −1 mm (SD 3) for the LR, CC and AP directions, respectively ().
Table III. Intra-fractional translational shifts after offline post-RT CBCT match on the Lipiodol spots.
Discussion
As large margins are needed for adequate tumor coverage, the acute and late side effects complicate the addition of chemotherapy or dose escalation. We aimed to develop a bladder tumor focused IGRT treatment approach with reduced margins to allow for a dose-escalated boost to the bladder tumor. Therefore, imaging of the bladder tumor before and during RT becomes essential.
In preparation for a future Danish dose escalation study which includes a tumor boost, we have conducted the present feasibility study of Lipiodol as a liquid fiducial marker for IGRT in urinary bladder cancer. We found that Lipiodol could simply and safely be injected into the mucosa peripheral to the post TUR-B tumor-bed. Adverse effects were only mild and transient and do not differ from those seen during routine flexible cystoscopy [Citation11].
Previous studies have explored solid fiducial markers in the bladder [Citation12,Citation13]. These techniques required dedicated applicator systems to place a solid fiducial marker during rigid cystoscopy. Because of the pain and discomfort for the patient, these procedures require either general anaesthesia or intravesical installation of Lidocain. With the technique presented in the present study, general anaesthesia can be avoided as flexibly cystoscopy is less painful and patients could be discharged from the hospital almost immediately after the procedure.
Our study has shown that the injected Lipiodol is visible on the anterior-posterior 2D-kV images, CT and CBCT during the full course of RT, although it is slowly absorbed over time. In one patient (patient 2) only one of five injections was visible on the subsequent CT and CBCT scans. All the Lipiodol used in the study was from the same batch. The failure in terms of lack of radio-oblique spots in this patient was most likely due to intravesical spillage of the Lipiodol as indicated by the lack of papules during the injections and not related to the quality of injected Lipiodol. A general experience is that neighbouring Lipiodol spots could, in particular on CBCT, be visualized as one joint demarcation, and therefore the injections should be small and placed as far apart as possible.
A major problem using solid fiducial markers in the bladder wall is the drop-out of markers into the abdomen or with the urine. This is demonstrated in the study by Hulshof et al. were half of the fiducial markers were lost after a median of 11.5 days after implantation [Citation12]. In the study by Mangar et al., the drop-out rate of the seeds could be reduced by a cystodiathermy procedure performed after insertion of the gold markers. However, 73% of the drop-out seeds were from the tumor area, and no seeds could be placed if the tumor was located in the dome of the bladder [Citation13].
Pos et al. recently published a study describing Lipiodol demarcation of the bladder tumor. In 40 bladder cancer patients the tumor was successfully demarcated by Lipiodol in 38 patients with only minimal side effects. They found the technique to be feasible, simple, visible on CT and CBCT and therefore useful for IGRT of bladder cancer. The number of Lipiodol spots per tumor, washout, inter- and intra-fraction tumor shifts are not reported in the Pos study [Citation9].
Voiding and drinking protocols are often used in RT of bladder cancer to minimize the inter-fraction variation in bladder volume and as a result the bladder shape and positions of the bladder wall. In the present study, patients were instructed to empty the bladder before CT scan for dose planning and before each treatment session. However, even after emptying the bladder, the bladder volume ranged from 82 to 155 cm3 with a relatively large variation between the fractions. Therefore, we consider voiding or drinking protocols insufficient for precise localization of the bladder and the tumor in RT of bladder cancer.
By use of IGRT with online match on the bony anatomy, the necessary shifts according to the Lipiodol spots were at least 5 mm in more than half of all treatment fractions. For one patient, as much as 86% of all treatment fractions required a shift of 5 mm or more to match on the Lipiodol spots following an on-line bony anatomy set-up. In a study by Pos et al., 65% of patients had part of the bladder tumor located outside the PTV a least once, even by the use of wide margins [Citation14]. Clearly, IGRT using fiducial markers will improve the dose coverage of the tumor even with small margins in tumor directed-treatment of bladder cancer. The intra-fractional shifts of the bladder tumor (residual error) are considerably smaller than the interfraction shifts. We found that the mean geometric shift needed was 3 mm (range 1–6 mm) between pre- and post-treatment CBCT (average time 16 min, range 15–20 min). Intra-fractional shifts were most pronounced in the CC and AP directions. In contrary to the present study, a study based on cine-MRI revealed large and asymmetric intra-fraction shifts of the urinary bladder wall [Citation15].
In conclusion, Lipiodol injection into the bladder submucosa in the periphery of the bladder tumor is technically and clinically feasible. Because the Lipiodol demarcations are visible on the treatment planning CT, on 2D kV images and CBCT scans during the full course of RT, they are valuable in IGRT and adaptive RT of bladder cancer. The demonstrated inter- and intra- fractional shifts of the Lipiodol underlines the need for online fiducial tumor match to safely apply a tumor directed boost in the treatment of bladder cancer. IGRT-directed dose escalation based on Lipiodol fiducial markers may improve tumor control in RT for urinary bladder cancer and the strategy will be further investigated in a future study.
Acknowledgements
Supported by CIRRO – The Lundbeck Foundation Center for Interventional Research in Radiation Oncology, the Danish Council for Strategic Research, the Danish Graduate School for Clinical Oncology, The Danish Cancer Society, Helga and Peter Kornings Foundation and Varian Medical Systems (Palo Alto, CA, USA). The authors also acknowledge the support from the Department of Medical Physics, Aarhus University Hospital. EudraCT number: 2007-007256-34. ClinicalTrials Identifier: NCT00609843.
Declaration of interest: This work was partly funded with a research grant from Varian Medical Systems (Palo Alto, CA, USA)
References
- Tonoli S, Bertoni F, de Stefani A, Vitali E, de Tomasi D, Caraffini B, . Radical radiotherapy for bladder cancer: Retrospective analysis of a series of 459 patients treated in an Italian institution. Clin Oncol 2006;18:52–9.
- Sengelov L, von der Maase H. Radiotherapy in bladder cancer. Radiother Oncol 1999;52:1–14.
- Fokdal L, Honore H, Hoyer M, Meldgaard P, Fode K, von der Maase H. Impact of changes in bladder and rectal filling volume on organ motion and dose distribution of the bladder in radiotherapy for urinary bladder cancer. Int J Radiat Oncol Biol Phys 2004;59:436–44.
- Muren LP, Smaaland R, Dahl O. Organ motion, set-up variation and treatment margins in radical radiotherapy of urinary bladder cancer. Radiother Oncol 2003;69:291–304.
- Peeters STH, Heemsbergen WD, Koper PCM, Van Putten WLJ, Slot A, Dielwart MFH, . Dose-response in radiotherapy for localized prostate cancer: Results of the Dutch multicenter randomized phase III trial comparing 68 Gy of radiotherapy with 78 Gy. J Clin Oncol 2006;24: 1990–96.
- Zhang M, Moiseenko V, Liu M, Craig T. Internal fiducial markers can assist dose escalation in treatment of prostate cancer: Result of organ motion simulations. Phys Med Biol 2006;51:269–85.
- Watanabe Ki, Nomori H, Ohtsuka T, Kaji M, Naruke T, Suemasu K. Usefulness and complications of computed tomography-guided lipiodol marking for fluoroscopy-assisted thoracoscopic resection of small pulmonary nodules: Experience with 174 nodules. J Thorac Cardiovasc Surg 2006; 132:320–24.
- Dudouet P, Portalez D, Lhez JM, Elman B, Larroque JM, Bachaud JM, . Trans-rectal ultrasonography (TRUS) with lipiodol injection for localization of the prostatic apex before radiotherapy planning. Radiother Oncol 2001;61:135–41.
- Pos F, Bex A, Dees-Ribbers HM, Betgen A, van Herk M, Remeijer P, . Lipiodol injection for target volume delineation and image guidance during radiotherapy for bladder cancer. Radiother Oncol 2009;93:364–67.
- Søndergaard J, Høyer M, Petersen JB, Wright P, Grau C, Muren LP. The normal tissue sparing obtained with simultaneous treatment of pelvic lymph nodes and bladder using intensity-modulated radiotherapy. Acta Oncol 2009;48:238–44.
- Burke DM, Shackley DC, O'Reilly PH. The community-based morbidity of flexible cystoscopy. BJU Int 2002;89:347–49.
- Hulshof MCM, vanAndel G, Bel A, Gangel P, vandeKamer J. Intravesical markers for delineation of target volume during external focal irradiation of bladder carcinomas. Radiother Oncol 2007;84:49–51.
- Mangar S, Thompson A, Miles E, Huddart R, Horwich A, Khoo V. A feasibility study of using gold seeds as fiducial markers for bladder localization during radical radiotheraphy. Br J Radiol 2007;80:279–83.
- Pos FJ, Koedooder K, Hulshof MCCM, van Tienhoven G, González González D. Influence of bladder and rectal volume on spatial variability of a bladder tumor during radical radiotherapy. Int J Radiat Oncol Biol Phys 2003;55:835–41.
- McBain CA, Khoo VS, Buckley DL, Sykes JS, Green MM, Cowan RA . Assessment of bladder motion for clinical radiotherapy practice using cine-magnetic resonance imaging. Int J Radiat Oncol Biol Phys 2009;75:664–71.
