Abstract
The Danish Breast Cancer Cooperative Group (DBCG) introduced BCT as a standard treatment in Denmark in 1990. The aim of this study was to investigate late morbidity, cosmetic outcome, and body image after BCT and to associate these outcome variables with patient, tumor, and treatment characteristics. Material and methods. A total of 214 patients treated with BCT from 1989–2002 participated in a long-term follow-up visit comprising an interview, clinical examination, photos of the breast region and completion of a questionnaire on Body Image. Results. Median follow-up time was 12 years (range 7–20). Moderate to severe fibrosis was found in 23% of patients and was associated with chemotherapy [OR 2.6, CI (1.1; 5.9), p = 0.02], large breast size [OR 3.2, CI (1.6; 6.4), p = 0.001], and smoking [OR 2.4, CI (1.1; 4.9), p = 0.02]. Patients with a satisfactory cosmetic outcome, when assessed by a clinician, were characterized by small tumors [OR 3.2, CI (1.5; 6.8), p = 0.003] and small to medium sized breasts [OR 2.0, CI (1.1; 3.5), p = 0.002]. Fifty percent of patients scored good or excellent when assessed by a clinician compared to 88% when reported by the patients themselves. Patients satisfied with their own cosmetic outcome were the younger patients [< 50 years; OR 3.2, CI (1.1; 8.6), p = 0.03] with no postoperative complications [OR 3.3, CI (1.2; 9.2), p = 0.02]. Regarding body image 15% felt less feminine, 25% felt less sexually attractive, and 28% of patients had changed their clothing habits as a result of the disease or treatment. Conclusion. The majority of patients were satisfied with their cosmetic outcome after BCT, whereas only half of the patients were found to have a good or excellent cosmetic outcome when assessed by the clinician. Body image was found to be only minimally disturbed in the majority of patients. The level of moderate to severe fibrosis was acceptable compared to both national and international studies with similar patient compositions.
Large clinical trials have previously shown that breast conserving surgery (BCS) supplemented with radiotherapy (RT) are comparable to mastectomy in terms of recurrence rate and overall survival [Citation1–6]. Protocols and guidelines from the Danish Breast Cancer Cooperative Group (DBCG) have ensured that Danish breast cancer patients receive uniform treatment. In the DBCG 1982TM randomized trial [Citation1], breast conserving therapy (BCT), consisting of BCS and RT, was compared with mastectomy, and in 1990 BCT was implemented as a standard treatment in Denmark. The risk of late adverse reactions to the skin and connective tissue in the operated and irradiated areas in a number of patients can cause discomfort and pain, reduce cosmetic outcome, and disturb the patients’ body image.
Based on the hypothesis that BCT is a beneficial treatment, that leaves the patients with an acceptable degree of late morbidity and a satisfying cosmetic outcome, we launched a retrospective follow-up study of a Danish cohort of women treated with BCT from 1989 to 2002. The study was initiated because of the need for investigations on late morbidity, since the patients receiving BCT has changed from a trial cohort to a group of more unselected patients.
Materials and Method
Patients
Patients were recruited from the DBCG database () based on the following inclusion criteria: BCT in the period 1989–2002, treated with postoperative RT at the Oncological Department at Aarhus University Hospital in accordance to one of three Danish protocols (DBCG 1989, -1999 and -2001). The protocols have been described in detail elsewhere [Citation7,Citation8]. Exclusion criteria were: local, regional or distant breast cancer recurrence, patients treated with immediate or delayed reconstruction of the breast, with a new primary contra-lateral breast cancer, or other malignant diseases treated with adjuvant systemic treatment. From 1989 to 2002, 788 patients received RT at Aarhus University Hospital. A total of 597 patients were invited to participate in a single long-term follow-up visit by letter (see Supplementary Appendix to be found online at http://informahealthcare.com/doi/abs/10.3109/0284186X.2012.744469). Patients were divided into three treatment groups: Group A patients received BCT only, Group B patients received BCT + adjuvant chemotherapy, and Group C patients received BCT + adjuvant anti-hormone therapy. Invited patients were selected randomly from within each treatment group. The visits were conducted by the same clinician (CDL) from March to September 2010 at the Department of Oncology, Aarhus University Hospital. The visit comprised a clinical examination, photos taken of the breast region, and an interview on aspects such as breast sensibility and breast pain. Patients were asked to complete a questionnaire on body image in advance and deliver it at the follow-up visit. At the time of the visit, the clinician was blinded as to which treatment the patients had received, and patients were asked not to disclose this information during the visit. After the follow-up visits had ended, an audit of all patient charts were performed, and detailed data on tumor, treatment and the postoperative period was registered.
Surgery
According to the DBCG criteria in the period 1989–2002, patients suitable for BCS were: 1) the tumor could be removed with a good cosmetic result; 2) 10 mm macroscopic and 5 mm microscopic tumor-free margins were obtainable; and 3) the patient accepted postoperative RT to the residual breast tissue [Citation9]. The BCS procedure was performed as a lumpectomy and an axillary dissection (see Supplementary Appendix to be found online at http://informahealthcare.com/doi/abs/10.3109/0284186X.2012.744469).
Radiation therapy
Detailed information on the radiation therapy given has been described elsewhere [Citation10]. The recommended treatment was megavoltage (6–16 MV) irradiation with tangential fields, with wedges or tissue compensators used to minimize dose inhomogeneity. All patients treated with BCS received the recommended dose of irradiation to the chest wall and the residual breast of 48 Gy in 24 fractions with 5 fractions per week. Boost treatment and irradiation of regional lymph nodes were given according to the treatment guidelines (see Supplementary Appendix to be found online at http://informahealthcare.com/doi/abs/10.3109/0284186X.2012.744469). In our study cohort boost treatment was given to 177 patients, and irradiation of regional lymph nodes was given to 61 patients.
Adjuvant systemic treatment
According to the DBCG protocols, patients were identified as having low or high risk of recurrence based on a number of criteria (). Low-risk patients entered treatment group A with no adjuvant systemic treatment. High-risk patients entered either treatment group B if premenopausal, or postmenopausal and ER-receptor negative, receiving chemotherapy [(cyclophosphamide, methotrexate, and 5-fluouracil (CMF) or cyclophosphamide, epirubicin, and 5-fluouracil (CEF)] administered concomitantly or sequentially to RT, or treatment group C if postmenopausal, receiving antihormone therapy, Tamoxifen, letrozole or both for up to five years (see Supplementary Appendix to be found online at http://informahealthcare.com/doi/abs/10.3109/0284186X.2012.744469). Detailed descriptions of the chemotherapy and antihormone treatment according to the DBCG-protocols have been published previously [Citation8,Citation11].
Endpoints
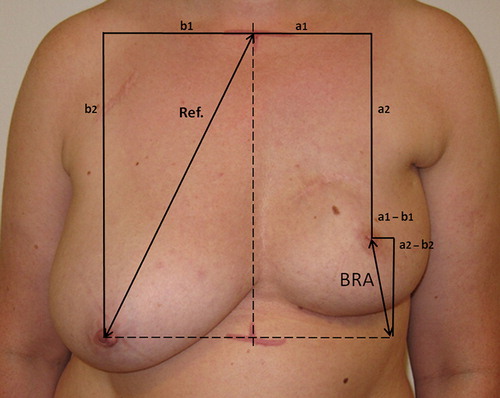
Most endpoint variables were scored using four point grades (), and later dichotomized for the use in logistic regression analysis. Assessment of the primary endpoint fibrosis was performed by palpation using the healthy breast as reference. Since information on whether patients had been treated with boost irradiation was blinded at the time of the clinical examination, fibrosis was scored for the whole breast including the tumor bed/boost area. Secondary endpoints were overall cosmetic outcome assessed by the patient and by the clinician into four grades (excellent, good, fair, poor); patients were only asked to give an overall assessment, whereas the clinician had a set description to follow (). Other secondary endpoints were late morbidity after treatment (telangiectasia and dyspigmentation), scar appearance, Breast Retraction Assessment [BRA – a quantitative measure for the nipple displacement both vertically and horizontally ()] [Citation12] calculated by means of the BCCT.core software program [Citation13], edema of the arm (comparing the circumference of the arms 15 cm above and 10 cm below Olecranon), and impaired shoulder movement (difference in flexion and abduction between the operated and the non-operated side). Breast size was quantified as cup size A, B, C, D, E, or above according to the size stated by the patients and aligned with the clinician's estimate determined by eye. If there were discrepancies between the two, the clinician's estimate was applied. BMI was measured at the follow-up visit. All 214 participants were scored for adverse effects (see supplementary material Appendix to be found online at http://informahealthcare.com/doi/abs/10.3109/0284186X.2012.744469). Nine patients were not evaluated concerning all aspects of the cosmetic outcome because of either contra-lateral or bi-lateral breast reduction years after primary treatment. Patients were asked to answer questions regarding reduced sensibility of the breast, pain in the breast, and consumption of analgesics connected to pain in the breast. Other subjective endpoints were questions on body image from the questionnaire. As a result of the work done by Johansen and colleagues on the DBCG 82 cohort [Citation14], two extra questions were added; whether, as a result of the disease and treatment, the patient had changed her clothing habits or had been considering plastic- or reconstructive surgery to the treated breast. All questions in the questionnaire had four ratings (‘not at all’, ‘a little’, ‘quite a bit’, and ‘very much’) and patients answered the questions taking into account only the last month before the follow-up visit (see Supplementary Appendix to be found online at http://informahealthcare.com/doi/abs/10.3109/0284186X.2012.744469).
Table I. Definitions of chosen endpoints and the grades.
Statistical and ethical considerations
Based on the assumption of a difference in the frequency of fibrosis (the primary endpoint) of at least 20% in the reference group A, compared to group B and C, the sample size of the three groups were calculated to be 71 patients in each, with a significance level of 5% (α) and a test strength of 80% (β) [Citation15]. Univariate logistic regression analyses were performed on dichotomous endpoints. Multivariate logistic regression analyses were performed on significant and borderline significant variables with stepwise backward selection, using a significance level of 0.05 for removal from the model. T-tests and rank sum tests were used for continuous data, which were not normally distributed. Data were analyzed using STATA/IC 11. All p-values were two-sided.
Written informed consent was obtained for all patients. The Central Denmark Regional board under the Danish National Committee on Biomedical Research Ethics approved the study in February 2010 (M-20100013).
Results
A total of 214 patients agreed to participate in the study. Patients were evenly divided into the treatment groups; A: 75 patients, B: 68 patients and C: 71 patients. Mean age at diagnosis was 52 years, varying between the groups because of the selection of pre- and postmenopausal women into group B and C, respectively. Patient, tumor, and treatment characteristics are shown in , outcome, treatment, and patient variables in . See supplementary material for a table of the overall distribution of patients into variable categories and scores.
Table II. Patient-, tumor- and treatment characteristics of 214 patients treated with BCT from 1989–2002, according to treatment groups.
Table III. Outcome, treatment and patient variables.
Fibrosis
After a median follow-up time of 12 years, 23% of the patients in our cohort had developed moderate to severe fibrosis (). The treatment-related variable that significantly increased the risk of fibrosis was a high boost dose (> 10 Gy), [i.e. moderate to severe fibrosis occurred in 6/10 patients (60%) treated with high boost doses, compared to 34/133 patients (20%) treated with the lower boost doses]. Patient-related variables shown to significantly increase the risk of fibrosis were large breasts (≥ cup C), smoking, and chemotherapy. Postoperative complications, axillary dissection, axillary irradiation, age at diagnosis, length of follow-up, body mass index (BMI), and antihormone therapy posed no increased risk of fibrosis.
Table IV. Relationship between patient-, tumor-, and treatment characteristics and endpoints: Fibrosis and cosmetic outcome assessed by patients and by clinician, univariate analysis.
In the multivariate analysis, variables entered were boost dose, smoking status, breast size, treatment group and BMI. In this setting smoking status and BMI had no effect on fibrosis, whereas a boost dose [> 10 Gy; OR 8.1, CI (1.8; 36.7), p = 0.007], breast size [≥ C cup; OR 4.5, CI (1.9; 10.5), p = 0.001] and chemotherapy [CEF; OR 3.2, CI (1.1; 9.2), p = 0.03] were still variables significantly identified as predictors (see Supplementary Tables to be found online at http://informahealthcare.com/doi/abs/10.3109/0284186X.2012.744469).
Shoulder movement and edema of the arm
Twenty-one patients (10%) presented with impaired shoulder movements (flexion and/or abduction); 13 patients had impaired flexion, mean reduction: 42° (range 5 to 90, SD: 33), and 17 patients had impaired abduction, mean reduction: 37° (range 5 to 90, SD: 34). All patients had been treated with axillary dissection, but only 6/21 patients had been treated with axillary irradiation. The number of removed axillary lymph nodes, showed no influence on the presence of impaired shoulder movements [OR 1.01, CI (0.9; 1.1), p = 0.9].
Arm edema was found in 36 patients (17%). Adjuvant systemic treatment was not found to influence the risk of edema; this was also the case for axillary dissection, axillary irradiation and the number of removed axillary lymph nodes.
Scar
The number of patients with an unacceptable scar appearance (Grade 2 + 3, ) was 84/205 (41%). Average length of scar did not differ significantly between the two groups; unacceptable (6.8 cm) versus acceptable (6.3 cm) (Grade 0 + 1) scar appearance (p = 0.11). The scar evaluation was not significantly associated with the size of the tumor [OR 1.0, CI (1.0; 1.1), p = 0.11] or with the placement (quadrant) of the scar [OR 1.0, CI (0.8; 1.3), p = 0.99]. Average BRA ± standard deviation (SD) differed significantly between the unacceptable (4.2 ± 2.0 cm) and the acceptable (2.9 ± 1.6 cm) scar groups. The shape of the scar had a significant influence on scar appearance with 51/101 straight scars rated acceptable, compared to 70/99 semi-circle shaped scars [OR 2.4, CI (1.3; 4.2), p = 0.004].
Cosmetic outcome – descriptive and agreement between patient and clinician
A total of 181/205 patients (88%) scored their own cosmetic outcome as good or excellent. When assessed by the clinician 102/205 patients (50%) were rated good or excellent on cosmetic score (). A weighted Kappa value of 9.4% was calculated, comparing the clinicians and the patients ratings, corresponding to a poor and insignificant (p = 0.0006) agreement.
Cosmetic outcome – patients’ assessment
Treatment-related predictors of a poor cosmetic result were postoperative complications [i.e. 19/116 patients (16%) with complications scored their cosmetic outcome fair or poor, compared to 5/89 patients (6%) without complications] and axillary irradiation, the latter with a four-fold higher risk of a fair or poor result if the patients had received axillary irradiation [14/60 patients (23%)] compared to those not irradiated [10/145 patients (7%)]. Axillary dissection, boost treatment, and boost dose were not able to predict the cosmetic result assessed by the patients. Patient-related predictors of a fair or poor cosmetic result were age at diagnosis, 16% of patients ≥ 50 years scored fair or poor compared to 6% of patients < 50 years. Length of follow-up in the fair or poor group was significantly shorter [10.8 years, CI (9.7; 12.0)] than in the good or excellent group [12.4 years, CI (11.9; 12.8)] (p = 0.03). Smoking status was also found to be an independent predictor; 24% of current smokers scored their own cosmetic result as fair or poor, compared to 9% of non- or ex-smokers. Patient-related variables not associated with the cosmetic result, were BMI, breast size, tumor size, and adjuvant systemic treatment.
In the multivariate analysis variables entered were postoperative complications, axillary irradiation, age at diagnosis, length of follow-up, smoking status, breast size, and treatment group. Variables that could predict an unsatisfying cosmetic outcome were axillary irradiation [OR 3.8, CI (1.5; 9.5), p = 0.004], age [OR 3.9, CI (1.3; 11.8), p = 0.02], and smoking status [OR 3.8, CI (1.4; 10.3), p = 0.01]; patients who had received axillary irradiation, were ≥ 50 years, and were currently smoking, rated the cosmetic outcome as fair or poor four-times more frequently, than their counterparts.
Clinician's assessment
Treatment-related variables significantly associated with the cosmetic outcome assessed by the clinician, was only axillary dissection. More than 50% (100/194) of the patients being scored fair or poor had been treated with axillary dissection, compared to 18% (2/11) in the small group of patients who had not. Of the patient-related variables, BMI ≥ 25, breast size ≥ cup C, and tumor size > 2 cm significantly increased the risk of a fair or poor cosmetic outcome by 2–3. Photographic examples of patients with the four different grades of cosmetic outcome are shown in .
Figure 4. Example of the different grades of cosmetic outcome on patients from the cohort. Cosmetic outcome; top left: Excellent, top right: Good, bottom left: Fair, bottom right: Poor.

Variables entered in the multivariate analysis were axillary dissection, BMI, breast size, tumor size, axillary irradiation and length of follow-up. In this setting patients with BMI ≥ 25 [OR 2.7, CI (1.5; 4.8), p = 0.001] and tumor size > 2 cm [OR 3.2, CI (1.4; 7.3), p = 0.005] were associated with a fair or poor cosmetic outcome.
BRA – the Breast Retraction Assessment
Average BRA ± SD for all 205 patients evaluated on cosmetic issues was 35 (± 19) mm. Fibrosis and BRA was found to be significantly associated, with the average BRA and SD being greater in patients with moderate to severe fibrosis compared to patients with none to mild fibrosis [44 (± 22) mm and 32 (± 17) mm, respectively (p = 0.001)]. Also, patients with a fair or poor cosmetic outcome had a significantly greater average BRA than patients with a satisfying cosmetic outcome (good or excellent), when examined by the patients [43 (± 19) mm vs. 33 (± 19) mm, p = 0.012] as well as by the clinician [43 (± 20) mm vs. 26 (± 13) mm, p < 0.00005].
Entering BRA in the above shown multivariate settings of cosmetic outcome, when assessed by the patients, only shifted one variable (axillary irradiation) to non-significant [OR 2.44, CI (0.7; 6.8), p = 0.09]. The other two variables (age at diagnosis and smoking status) remained almost unchanged, while BRA itself was non-significant (p = 0.125). When assessed by the clinician, entering BRA shifted the two variables that were previously significant (tumor size and BMI) to non-significant, with BRA as the only significant predictor of cosmetic outcome [OR 1.8, CI (1.5; 2.2), p = 0.000].
Patient questionnaire and patient body image
All 214 patients answered the questionnaire on body image (Supplementary to be found online at http://informahealthcare.com/doi/abs/10.3109/0284186X.2012.744469). At the time of follow-up, 23% and 22% of patients felt ‘a little’ less physically or sexually attractive, respectively, while 7% felt this ‘quite a bit’ or ‘very much’. Around one-third of patients answered ‘a little’ to the question on whether they felt the treatment had left their body less whole, while only 3% answered ‘quite a bit’ or ‘very much’. Twenty-one percent had changed their clothing habits ‘a little’, 7% ‘quite a bit’ or ‘very much’. Patients generally did not have difficulties looking at themselves naked; only 7% answered ‘a little’ or ‘quite a bit’. Lastly, 10% of the patients had been considering having a plastic or reconstructive procedure performed to their treated breast. No associations between age (≤ or > 50 years) and the feeling of physically and sexually attractiveness was found, nor with the patients’ feeling feminine or not. Patients with moderate to severe fibrosis were found to have a significantly higher risk of changing their clothing habits [OR 7.2, CI (2.3; 22.7)].
Discussion
A total of 23% of the patients in our study presented with moderate to severe fibrosis and this finding was in line with other studies with comparable patient compositions. The EORTC ‘Boost-No Boost’-trial with 3624 patients treated with BCT, showed a 10-year risk of moderate-severe fibrosis in 26.9% in the ‘boost’ arm compared to 12.6% in the ‘no boost’ arm. In the EORTC study the risk of moderate to severe fibrosis was significantly associated with chemotherapy in premenopausal women and tamoxifen in postmenopausal women. Our study corroborated the correlation between the risk of fibrosis and chemotherapy, but showed no association with antihormone therapy. The EORTC study also showed a significant association between breast fibrosis and boost dose, with a further risk of developing fibrosis, in addition to postoperative complications (hematoma or edema), if the patient received boost treatment [Citation16]. This correlation between moderate to severe fibrosis and boost dose was emphasized with a dose-effect relationship for the development of fibrosis in the treated breast with four levels of boost dose treatment (0, 10, 16 and 26 Gy) [Citation17]. The finding of a significant association between high boost-doses (> 10 Gy) and the development of moderate to severe fibrosis in our study was in agreement with this, although only 10 patients received a boost dose > 10 Gy. In our study cosmetic outcome was rated good or excellent by the patients and by a clinician in 88% and 50% of cases, respectively. These findings were consistent with the findings in the DBCG-1982-study [Citation14,Citation18], in spite of our cohort having a higher mean age at diagnosis, a longer follow-up time, and a higher number of patients in the high-risk groups given adjuvant systemic treatment. Other studies have shown cosmetic outcome to worsen with increasing age and length of follow-up [Citation19,Citation20]. Our study could not establish any association between anti-hormone therapy and an unsatisfactory cosmetic outcome. This was also the case in a large study examining disease recurrence and cosmesis in approximately 500 women treated with BCT and tamoxifen [Citation21,Citation22].
The patients who were satisfied with their own cosmetic outcome in our study, were those with no postoperative complications after BCT, who received no axillary irradiation, were young (< 50 years) and/or were non- or ex-smokers. This could imply that the experience of an uncomplicated course of disease may influence the patient's assessment on cosmetic outcome. The patients found to have a satisfying cosmetic outcome as assessed by the clinician, were characterized by having had no axillary dissection performed, having small to medium sized breasts, being of normal weight, and with small tumors. Some of these variables indicate an uncomplicated course of disease, but in particular they have a direct influence on cosmetic outcome. Overweight is known to increase the risk of asymmetric breasts as larger breasts often need higher RT-doses to reach the tumor cavity, exerting an increased risk of hot-spots and eventually fibrosis [Citation23]. Overweight is also associated with larger tumors and thus more tissue removed [Citation24]. Small tumor size is a surrogate measure for a small excision volume and a small incision line, which reduces the risk of asymmetry and an unsatisfying scar appearance. No axillary dissection means less extent of surgery and a reduced risk of postoperative complications, which together with no spread of disease to the axilla, means less irradiation overall in favor of a better cosmetic outcome.
The poor agreement between the ratings by the patients and the clinician may have several explanations. It could be that patients were unable to clearly separate which parameters were related to physical features as opposed to emotional when evaluating the cosmetic outcome. Another explanation could be that patients themselves could decide which parameters were the most important. Asymmetry must be included by the clinician, whereas patients were asked to score their overall impression comparing the treated and the non-treated breast. Adding BRA to the multivariate analysis of the clinician's assessment shifted the other predicting variables (BMI and tumor size) to being non-significant, and left BRA as the sole predicting variable. Adding BRA to the patients’ assessment only shifted one variable (axillary irradiation) to non-significant, and with BRA being non-significant in itself, it suggests that asymmetry had a crucial influence on the clinician's assessments. Yet another explanation may be that patients actually compared the cosmetic outcome after BCT to mastectomy, because this was the option given at the time of diagnosis. Lastly, it must be remembered that a satisfaction level of 100% is impossible to achieve, as some tissue will always have to be removed, in most cases leading to asymmetry.
Oncoplastic surgery was not integrated on a national scale at the time our patients were treated. However, with the current implementation of Oncoplastic surgery, it is our expectation that both patients and clinicians will ask for even better cosmetic outcome, although the access to, and need for, reconstructive surgery has been shown to have geographical and educational barriers [Citation25]. There were some limitations to this study. Due to the long follow-up time we experienced a recruiting problem in the postmenopausal group. This led us to expand the recruitment to DBCG 1999 and 2001 for all three treatment groups, thus the median length of follow-up differed: 14, 12, and 9 years for groups A, B, and C, respectively. The types of chemotherapy and antihormone therapy given were the same in all three treatment protocols, but in the 1999 and 2001 protocols a higher percentage of patients received CEF, while tamoxifen was given for a longer time period (2.5 or 5 years). The RT was in general unchanged until the end of 2002.
Cup size varies among different brands, and many women actually use a wrong size. Although quantifying breast size by asking the patients about their cup size is quick and easy, it is only a crude measure. Therefore the clinician determined the individual cup size by sight, to catch the misclassified cases. Still the results including breast size in this study should be interpreted with precaution. Several studies have tried to categorize breast size [Citation26,Citation27], and it would have benefitted this study if we had measured ribcage circumference since this is closely related to cup size; both cup size and rib cage circumference give a better correlation with actual breast volume [Citation28].
When assessing cosmetic outcome, baseline evaluations with photographs would have been of great value, making it possible to compare the surgical outcome with the effect of irradiation. This has now been implemented in the ongoing DBCG protocols.
In conclusion, long-term evaluation of BCT, with or without adjuvant systemic treatment, showed satisfying levels of cosmetic outcome from the patients view point, associated with an uncomplicated course of disease. Cosmetic outcome from the clinician's view point was at a less satisfying level, associated with variables representing less treatment, and dominated by asymmetry. Moderate to severe fibrosis was at an acceptable level, but enhanced by adjuvant chemotherapy in terms of CEF, and by high boost doses. However the morbidity seen in patients may also be associated with genetic variations. As shown in previous studies [Citation29–32] there is a known individual genetic variation, predisposing some patients to develop morbidity (especially fibrosis) after BCT. Thus further studies are needed to be able to identify patients that may have an enhanced risk of developing radiation-related morbidity.
http://informahealthcare.com/doi/abs/10.3109/0284186X.2012.744469
Download PDF (384 KB)Acknowledgements
The author wishes to thank M. J. Cardoso, J. S. Cardoso and INESC Porto Breast Research Group for generously lending the software program BCCT.core for the use in our study.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper. This work was supported by CIRRO – the Lundbeck Foundation Center for Interventional Research in Radiation Oncology, Aarhus University, the Danish Cancer Society, the Danish Agency for Science, Technology and Innovation, and Breast Friends.
References
- Blichert-Toft M, Rose C, Andersen JA, Overgaard M, Axelsson CK, Andersen KW, . Danish randomized trial comparing breast conservation therapy with mastectomy: Six years of life-table analysis. Danish Breast Cancer Cooperative Group. J Natl Cancer Inst Monogr 1992;19–25.
- Jacobson JA, Danforth DN, Cowan KH, d’Angelo T, Steinberg SM, Pierce L, . Ten-year results of a comparison of conservation with mastectomy in the treatment of stage I and II breast cancer. N Engl J Med 1995;332: 907–11.
- van TG, Voogd AC, Peterse JL, Nielsen M, Andersen KW, Mignolet F, . Prognosis after treatment for loco-regional recurrence after mastectomy or breast conserving therapy in two randomised trials (EORTC 10801 and DBCG-82TM). EORTC Breast Cancer Cooperative Group and the Danish Breast Cancer Cooperative Group. Eur J Cancer 1999; 35:32–8.
- Fisher B, Jeong JH, Anderson S, Bryant J, Fisher ER, Wolmark N. Twenty-five-year follow-up of a randomized trial comparing radical mastectomy, total mastectomy, and total mastectomy followed by irradiation. N Engl J Med 2002;347:567–75.
- Blichert-Toft M, Nielsen M, During M, Moller S, Rank F, Overgaard M, . Long-term results of breast conserving surgery vs. mastectomy for early stage invasive breast cancer: 20-year follow-up of the Danish randomized DBCG-82TM protocol. Acta Oncol 2008;47:672–81.
- Clarke M, Collins R, Darby S, Davies C, Elphinstone P, Evans E, . Effects of radiotherapy and of differences in the extent of surgery for early breast cancer on local recurrence and 15-year survival: An overview of the randomised trials. Lancet 2005;366:2087–106.
- Ewertz M, Kempel MM, During M, Jensen MB, Andersson M, Christiansen P, . Breast conserving treatment in Denmark, 1989–1998. A nationwide population-based study of the Danish Breast Cancer Co-operative Group. Acta Oncol 2008;47:682–90.
- Moller S, Jensen MB, Ejlertsen B, Bjerre KD, Larsen M, Hansen HB, . The clinical database and the treatment guidelines of the Danish Breast Cancer Cooperative Group (DBCG); its 30-years experience and future promise. Acta Oncol 2008;47:506–24.
- DBCG - 89 protocol [Danish Breast Cancer Cooperative Group], 2012. [cited 2012 June 25]. Available from: http://dbcg.dk/PDF%20Filer/DBCG%2089%20protokol.pdf
- Overgaard M, Christensen JJ. Postoperative radiotherapy in DBCG during 30 years. Techniques, indications and clinical radiobiological experience. Acta Oncol 2008;47:639–53.
- Ejlertsen B, Mouridsen HT, Jensen MB. Adjuvant cyclophosphamide, methotrexate, and fluorouracil in premonopausal patients with node-positive breast cancer: Indirect comparison of dose and schedule in DBCG trials 77, 82, and 89. Acta Oncol 2008;47:662–71.
- Pezner RD, Patterson MP, Hill LR, Vora N, Desai KR, Archambeau JO, . Breast retraction assessment: An objective evaluation of cosmetic results of patients treated conservatively for breast cancer. Int J Radiat Oncol Biol Phys 1985;11:575–8.
- Cardoso JS, Cardoso MJ. Towards an intelligent medical system for the aesthetic evaluation of breast cancer conservative treatment. Artif Intell Med 2007;40:115–26.
- Johansen J, Overgaard J, Rose C, Engelholm SA, Gadeberg CC, Kjaer M, . Cosmetic outcome and breast morbidity in breast-conserving treatment – results from the Danish DBCG-82TM national randomized trial in breast cancer. Acta Oncol 2002;41:369–80.
- Whitley E, Ball J. Statistics review 4: Sample size calculations. Crit Care 2002;6:335–41.
- Collette S, Collette L, Budiharto T, Horiot JC, Poortmans PM, Struikmans H, . Predictors of the risk of fibrosis at 10 years after breast conserving therapy for early breast cancer: A study based on the EORTC Trial 22881-10882 ‘boost versus no boost’. Eur J Cancer 2008;44:2587–99.
- Poortmans PM, Collette L, Bartelink H, Struikmans H, Van den Bogaert WF, Fourquet A, . The addition of a boost dose on the primary tumour bed after lumpectomy in breast conserving treatment for breast cancer. A summary of the results of EORTC 22881-10882 “boost versus no boost” trial. Cancer Radiother 2008;12:565–70.
- Johansen J, Overgaard J, Overgaard M. Effect of adjuvant systemic treatment on cosmetic outcome and late normal-tissue reactions after breast conservation. Acta Oncol 2007;46:525–33.
- Curran D, van Dongen JP, Aaronson NK, Kiebert G, Fentiman IS, Mignolet F, . Quality of life of early-stage breast cancer patients treated with radical mastectomy or breast-conserving procedures: Results of EORTC Trial 10801. The European Organization for Research and Treatment of Cancer (EORTC), Breast Cancer Co-operative Group (BCCG). Eur J Cancer 1998;34:307–14.
- Whelan TJ, Pignol JP, Levine MN, Julian JA, MacKenzie R, Parpia S, . Long-term results of hypofractionated radiation therapy for breast cancer. N Engl J Med 2010;362: 513–20.
- Wazer DE, Kaufman S, Cuttino L, DiPetrillo T, Arthur DW. Accelerated partial breast irradiation: An analysis of variables associated with late toxicity and long-term cosmetic outcome after high-dose-rate interstitial brachytherapy. Int J Radiat Oncol Biol Phys 2006;64:489–95.
- Wazer DE, Morr J, Erban JK, Schmid CH, Ruthazer R, Schmidt-Ullrich RK. The effects of postradiation treatment with tamoxifen on local control and cosmetic outcome in the conservatively treated breast. Cancer 1997;80:732–40.
- Clarke D, Martinez A, Cox RS. Analysis of cosmetic results and complications in patients with stage I and II breast cancer treated by biopsy and irradiation. Int J Radiat Oncol Biol Phys 1983;9:1807–13.
- Ewertz M, Jensen AB. Late effects of breast cancer treatment and potentials for rehabilitation. Acta Oncol 2011;50:187–93.
- Hvilsom GB, Holmich LR, Frederiksen K, Steding-Jessen M, Friis S, Dalton SO. Socioeconomic position and breast reconstruction in Danish women. Acta Oncol 2011;50: 265–73.
- Dundas KL, Atyeo J, Cox J. What is a large breast? Measuring and categorizing breast size for tangential breast radiation therapy. Australas Radiol 2007;51:589–93.
- Strombeck JO, Malm M. Priority grouping in a waiting list of patients for reduction mammaplasty. Ann Plast Surg 1986;17:498–502.
- Ringberg A, Bageman E, Rose C, Ingvar C, Jernstrom H. Of cup and bra size: Reply to a prospective study of breast size and premenopausal breast cancer incidence. Int J Cancer 2006;119:2242–3.
- Andreassen CN, Alsner J, Overgaard M, Overgaard J. Prediction of normal tissue radiosensitivity from polymorphisms in candidate genes. Radiother Oncol 2003;69:127–35.
- Andreassen CN. Can risk of radiotherapy-induced normal tissue complications be predicted from genetic profiles?Acta Oncol 2005;44:801–15.
- Andreassen CN, Alsner J, Overgaard M, Sorensen FB, Overgaard J. Risk of radiation-induced subcutaneous fibrosis in relation to single nucleotide polymorphisms in TGFB1, SOD2, XRCC1, XRCC3, APEX and ATM – a study based on DNA from formalin fixed paraffin embedded tissue samples. Int J Radiat Biol 2006;82:577–86.
- Alsner J, Rodningen OK, Overgaard J. Differential gene expression before and after ionizing radiation of subcutaneous fibroblasts identifies breast cancer patients resistant to radiation-induced fibrosis. Radiother Oncol 2007;83: 261–6.