To the Editor,
Standard of care treatment for pediatric patients with stage III Hodgkin lymphoma (HL) is chemotherapy with involved-field radiotherapy (IFRT) reserved for patients receiving less-intensive chemotherapy regimens or with incomplete or slow responses to chemotherapy [Citation1]. Unfortunately, HL survivors are at a very high risk of long-term side effects from their definitive treatment [Citation2–9]. As these sequelae are a function of exposure to both chemotherapy and radiotherapy, investigators seek ways to reduce damage to normal tissue [Citation1,Citation9,Citation10].
Although researchers have demonstrated the dosimetric advantages of using intensity-modulated radiation therapy (IMRT) and proton therapy (PT) in patients with stage I/II HL [Citation6], to our knowledge, no study has evaluated their use in patients with advanced-stage HL. The present presentation investigates dose reduction to the organs at risk (OAR) with IMRT and PT in a pediatric patient with stage III HL treated at the University of Florida Proton Therapy Institute (UFPTI).
Case
A 16-year-old female with stage IIIAS Nodular Sclerosing HL with initial involvement of the bilateral cervical neck and supraclavicular region, left axilla, spleen, and bulky mediastinum presented to UFPTI following a complete response to four cycles of doxorubicin, bleomycin, vincristine, etoposide, prednisone, cyclophosphamide (ABVE-PC) chemotherapy.
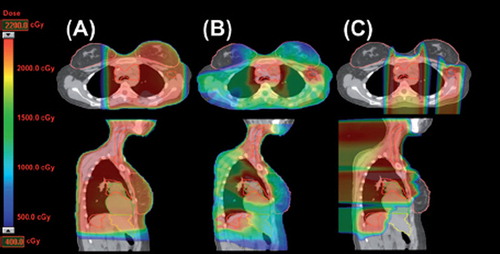
A four-dimensional (4D)-computed tomography (CT) simulation was performed followed by a 3D-CT scan with intravenous (IV) contrast (Philips Brilliance, Philips Medical Systems, Madison, WI, USA). After reviewing the patient's pretreatment PET- CT scan, the clinical target volume (CTV) was defined as the prechemotherapy involved node field (including the spleen) with a 1 cm margin created for the PTV. The patient underwent comparative treatment planning with PT, 3D conformal radiotherapy (CRT), and IMRT plan, which were normalized and optimized for both target coverage requirements [CTV D99% 100% and planning target volume (PTV) D95% 95%] and OAR protection. depicts the three plans. demonstrates the mean doses to the OARs among the three plans as well as the relative reduction and absolute reduction. PT substantially reduced the dose to the breasts, heart, lungs, stomach, bowel, and the integral body dose compared with 3DCRT and IMRT. There was no benefit to IMRT compared with 3DCRT. The patient, therefore, was treated with proton therapy and received 21 Gy (RBE) in 1.5-Gy daily fractionations for a total course of 14 days. With approximately 15 months of follow-up, she is still in remission with no toxicities secondary to treatment.
Table I. Mean dose to organs at risk.
Figure 1. Comparison of the dose distribution of (A) three-dimensional conformal radiotherapy (3DCRT), (B) intensity-modulated radiotherapy (IMRT), and (C) proton therapy (PT) plans. The clinical target volume (CTV), breasts, heart, and liver are outlined in red, pink, green and yellow, respectively.
Discussion
Although the risk of secondary cancers and cardiovascular disease in HL survivors will likely improve in the coming years, due to reductions in chemotherapy, radiation dose, and radiation field size, they still represent a major concern. This case illustrates how PT can further reduce the risk compared with IMRT or 3DCRT.
From a standpoint of overall second cancer risk, PT reduced the integral body dose by 40% compared with the other plans. In a cohort of 4230 patients, those exposed to integral doses of radiation greater than 150 J had a statistically significant adjusted relative risk of 5.2 for development of carcinomas and 12.6 for sarcomas [Citation4]. Only the PT plan was able to deliver a dose lower than 150 J. In terms of limiting dose to specific sites of interest, breast and lung cancer reduction have become a cornerstone for progress [Citation2,Citation5,Citation8,Citation9]. Although advances in using smaller radiotherapy fields in female HL patients that omit the uninvolved axilla, such as IFRT, have already shown a reduction in breast cancer development, it remains a problem in patients with axillary involvement, that was of particular concern in this patient. While IMRT performed better than PT at reducing the high-dose radiation profile (V20 0% for IMRT and 3% for PT), it did so at the expense of subjecting larger amounts of tissue to a lower but still harmful dose (V5 78% for IMRT and 11% for PT). This advantage was also seen in lung tissue where PT performed better than either 3DCRT or IMRT at reducing low and moderate doses (V5 52% for PT, 99% for IMRT, and 63% for 3DCRT). Travis et al. observed an increased risk of secondary malignancies (SMN) at both of the aforementioned sites with radiation doses even as low as 4 Gy [Citation8,Citation9]. As the only modality that met these stringent guidelines, PT may provide an increased margin of safety against development of future malignancy over 3DCRT or IMRT.
PT also reduced the radiation dose to the GI tract, which is expected to reduce her risk of secondary GI cancers. In a cohort of over 5100 patients with testicular cancer or Hodgkin lymphoma, van den Belt-Dusebout et al. found that mean stomach doses of more than 20 Gy were associated with a relative risk of 9.9 for SMN compared with doses below 11 Gy [Citation3]. PT reduced the dose to the stomach by 7.7 Gy and 9.5 Gy and her bowel dose by 6.5Gy and 5.5 Gy compared with IMRT and 3DCRT, respectively.
Cardiac disease also significantly impacts survival rate of HL patients [Citation5,Citation7]. Radiation doses above 15 Gy are associated with over a two-fold increase in the hazard ratio of cardiac sequelae [Citation7]. In this patient, only PT allowed us to meet that dose constraint, while 3DCRT and IMRT treated the heart to doses of 16 Gy or higher.
This investigation demonstrated that PT reduced radiation to non-targeted tissues in a pediatric patient with stage III HL without compromising target coverage. This improvement in OAR and integral dose suggests an increased margin of safety against the long-term side effects of radiotherapy, and establishes the foundation for clinical utilization and further research in pediatric patients with stage III HL.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Wolden SL, Chen L, Kelly KM, Herzog P, Gilchrist GS, Thomson J, . Long-term results of CCG 5942: A randomized comparison of chemotherapy with and without radiotherapy for children with Hodgkin’s lymphoma – A report from the Children’s Oncology Group. J Clin Oncol 2012;30:3174–80.
- Oeffinger KC, Mertens AC, Sklar CA, Kawashima T, Hudson MM, Meadows AT, . Chronic health conditions in adult survivors of childhood cancer. N Engl J Med 2006;355:1572–82.
- van den Belt-Dusebout AW, Aleman BM, Besseling G, de Bruin ML, Hauptmann M, van ‘t Veer MB, . Roles of radiation dose and chemotherapy in the etiology of stomach cancer as a second malignancy. Int J Radiat Oncol Biol Phys 2009;75:1420–9.
- Tukenova M, Guibout C, Hawkins M, Quiniou E, Mousannif A, Pacquement H, . Radiation therapy and late mortality from second sarcoma, carcinoma, and hematological malignancies after a solid cancer in childhood. Int J Radiat Oncol Biol Phys 2011;80:339–46.
- Mertens AC, Yasui Y, Neglia JP, Potter JD, Nesbit ME, Jr., Ruccione K, . Late mortality experience in five-year survivors of childhood and adolescent cancer: The Childhood Cancer Survivor Study. J Clin Oncol 2001;19:3163–72.
- Hoppe BS, Flampouri S, Su Z, Latif N, Dang NH, Lynch J, . Effective dose reduction to cardiac structures using protons compared with 3DCRT and IMRT in mediastinal Hodgkin lymphoma. Int J Radiat Oncol Biol Phys 2012;84: 449–55.
- Mulrooney DA, Yeazel MW, Kawashima T, Mertens AC, Mitby P, Stovall M, . Cardiac outcomes in a cohort of adult survivors of childhood and adolescent cancer: Retrospective analysis of the Childhood Cancer Survivor Study cohort. BMJ 2009;339:b4606.
- Travis LB, Gospodarowicz M, Curtis RE, Clarke EA, Andersson M, Glimelius B, . Lung cancer following chemotherapy and radiotherapy for Hodgkin’s disease. J Natl Cancer Inst 2002;94:182–92.
- Travis LB, Hill DA, Dores GM, Gospodarowicz M, van Leeuwen FE, Holowaty E, . Breast cancer following radiotherapy and chemotherapy among young women with Hodgkin disease. JAMA 2003;290:465–75.
- Dorffel W, Luders H, Ruhl U, Albrecht M, Marciniak H, Parwaresch R, . Preliminary results of the multicenter trial GPOH-HD 95 for the treatment of Hodgkin’s disease in children and adolescents: Analysis and outlook. Klin Padiatr 2003;215:139–45.
