Abstract
AA-type amyloidosis of the genitourinary tract is a rare phenomenon and few cases are described in the literature. We report a 42-year-old man with ankylosing spondylitis, who developed hematuria, bilateral hydronephrosis, and renal failure caused by AA amyloidosis.
INTRODUCTION
The association of AA-type amyloidosis with collagen vascular diseases such as rheumatoid arthritis (RA) or juvenile RA has been well documented. There have been few published cases of patients with ankylosing spondylitis (AS) complicated with AA-type amyloidosis.Citation1 At the same time, amyloidosis of the genitourinary tract (AGT) seldom causes significant clinical symptoms. Diagnosis is difficult and often has to be differentiated from, amongst others, tumors of the urinary tract. We describe a patient diagnosed with AS with hematuria, bilateral hydronephrosis, and chronic renal failure caused by AA-type AGT.
CASE REPORT
A 42-year-old man with a 20-year history of AS has been reported. He had been treated with low-dose prednisone for 1 year and with nonsteroidal anti-inflammatory drugs (NSAIDs) for many years, with irregular compliance.
He was admitted to our hospital because of microhematuria. Laboratory findings (serum creatinine 2.3 mg/dL and proteinuria 500 mg/24 h) showed renal failure. Hemoglobin, coagulation parameters, immunological study, viral serology, urine cytology, urine culture, and acid-fast bacilli in urine were normal/negative. Ultrasound and abdominal computed tomography (CT) scan were normal and the cystoscopy showed nonspecific inflammation. NSAIDs were stopped and serum creatinine became stable at 1.9 mg/dL; therefore, the patient was discharged to be treated as an outpatient.
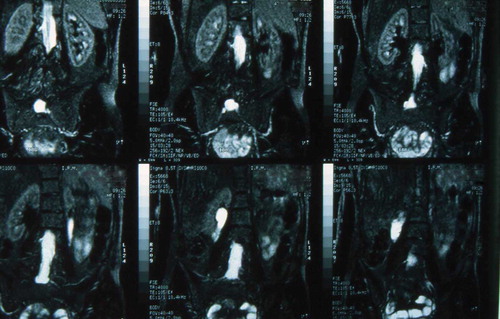
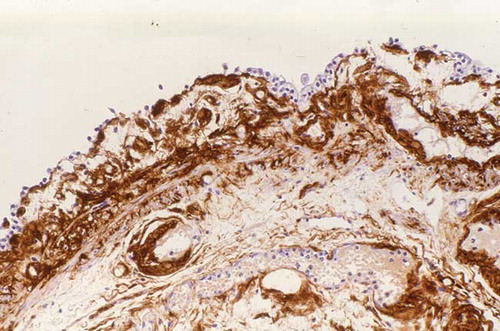
Ten months later, the patient presented with a new episode of hematuria. Clinical examination was normal. Laboratory values included hemoglobin 11.9 g/dL; white cell count, platelet count, coagulation, liver functions tests, and electrolytes were normal; serum electrophoresis showed hypoalbuminemia 2.3 g/dL and serum immunofixation did not identify a monoclonal gammopathy. Serum creatinine was 5 mg/dL, proteinuria (800 mg/day) and urinary analysis demonstrated hematuria. Urinary Bence-Jones protein was not detected. There was no pyuria or bacteriuria. Renal ultrasonography disclosed moderate bilateral hydronephrosis, and magnetic resonance imaging (MRI) confirmed this finding (). Urinary calculi were not seen. A transurethral mucosal biopsy of bladder and prostate were performed. Anatomopathological examination revealed eosinophilic deposits in the muscularis and lamina propria of the bladder and prostate; vascular and interstitial amyloidosis was demonstrated by strong apple-green birefringence under polarized light after Congo red staining. The immunohistochemical study with AA antibody protein was positive (). Bone marrow aspiration was normal and transthoracic echocardiography showed left ventricular hypertrophy with slight diastolic dysfunction. The patient was diagnosed with AA-type amyloidosis of the ATG.
A double-J bilateral catheter was introduced. Over the following days, the patient presented severe hematuria. He required blood transfusions, continuous bladder irrigation, and intravenous administration of epsilon-aminocaproic acid.
A 1-month follow-up revealed a satisfactory evolution with cessation of microhematuria and partial recovery of renal function to a creatinine level of around 3 mg/dL. The patient refused subsequent evaluation to complete the study of systemic amyloidosis, along with other aggressive therapy measures. We are unaware of his subsequent evolution because he was lost from follow-up as he did not attend programmed check-ups.
DISCUSSION
AGT is infrequent; it mostly affects the bladder but can also affect the ureters, prostate, renal pelvis, seminal vesicles, deferential ducts, testicles, urethra, and penis. AGT may be localized or systemic; in contrast, amyloidosis can be classified as type AL or AA by immunohistochemical staining.
It is possible that the incidence of AGT has been underestimated. Indeed, in a series of autopsies of symptom-free patients with RA, vesical amyloid deposits were discovered in every case.Citation2 On the other hand, AGT most often presents with gross hematuria,Citation3–5 local irritative symptoms, and most rarely with obstructive nephropathy.Citation6–11 The cystoscopy findings are variable: diffuse edema, hemorrhages, or pseudotumoral lesions.Citation2,Citation6,Citation9 These findings make the biopsy mandatory for the diagnosis. Once AGT is diagnosed it is necessary to evaluate these patients about a possible systemic disease; for this purpose rectal biopsy or anterior abdominal fat biopsy are both extremely useful.
Patients with AS can develop renal AA amyloidosis manifested by proteinuria, nephrotic syndrome, and renal failure. The prevalence of AA amyloidosis, associated with AS, in some series, is rated at 2.8%.Citation1,Citation12–15 Long-standing RA is the systemic disease most frequently associated with AA-type AGT, but as far as we know there are no previous publications about this complication in AS.
In our case, a systemic amyloidosis cannot be ruled out. On the other hand renal failure was probably multifactorial: obstructive nephropathy by massive amyloid deposits in the urinary tract, renal amyloidosis, and nonsteroidal anti-inflammatory drug treatment.
Therapy is centered on managing hematuria, with conservative measures and in case of persistent or large quantities, transurethral surgical removal, partial cystectomy, and occasionally resorting to the ligature of hypogastric arteries and total cystectomy.Citation16 Treatment has also been applied with colchicine as well as vesical instillations with dimethylsulfoxide following surgery with the purpose of breaking down the residual amyloid deposit.Citation16,Citation17 As often as possible, systemic therapy must be associated by controlling the underlying disease process. New therapeutic approaches, in particular antitumor necrosis factor (anti-TNF) alpha agents are promising in inducing clinical remission by suppressing systemic inflammation in AA amyloidosis.Citation18
In conclusion, this represents an unusual case of AA-type ATG with obstructive nephropathy and renal failure and should be considered in the differential diagnosis in patients with long-standing chronic inflammatory diseases.
Declaration of interest:The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this paper.
REFERENCES
- Lance NJ, Curran JJ. Amyloidosis in a case of ankylosing spondylitis with a review of the literature. J Rheumatol. 1991;18:100–103.
- Hajji K, Martin L, Devevey JM, Rheumatoid arthritis-induced pseudotumoral AA amyloidosis of the bladder with vesico-peritoneal fistula. Clin Nephrol. 2007;67:38–43.
- Duffau P, Imbert Y, De Faucal P, Primary localized amyloidosis of the urinary tract. A case series of five patients. Rev Med Interne. 2005;26:288–293.
- Palmero Martí JL, Budia Alba A, Arlandis Guzmán S, Benedicto Redón A, Hernández Martí M, Jiménez Cruz JF. Secondary vesical amyloidosis. Actas Urol Esp. 2004;28:238–242.
- Tesedo Cubero J, Ristol RM, Fernández Zuazu J, Dinares J, Autanell J. Massive hematuria and bladder perforation, complication of systemic amyloidosis. Arch Esp Urol. 1991;44:862–864.
- Lai AY, Lu SH, Huang CW, Yu HJ, Kuo YC. Renal amyloidosis presenting with obstructive uropathy. Kidney Int. 2007;72:1173–1174.
- Akram CM, Al-Marhoon MS, Mathew J, Grant CS, Rao TV. Primary localized AA type amiloydosis of urinary bladder: Case report of rare cause of episodic painless hematuria. Urology. 2006;68:1343.e15–1343.e17.
- Callaghan P, Asklin B. Ureteral obstruction due to primary localized amyloidosis. Scand J Urol Nephrol. 1993;27:535–536.
- Caballero Giné JM, Borrat Font P, Martí Picas L, Ristol Pont J. Bladder amyloidosis: Report of 2 cases. Actas Urol Esp. 2000;24:413–415.
- García Vivar ML, Galíndez Agirregoikoa E, Arostegui Lavilla J, García Llorente JF, Aramburu Albizuri JM. Secondary amyloidosis: Urologic involvement. An Med Interna. 1998;15:619–620.
- Ehara H, Deguchi T, Yanagihara M, Yokota T, Uchino F, Kawada Y. Primary localized amyloidosis of the bladder: An immunohistochemical study of a case. J Urol. 1992;147:458–460.
- Gandhi RM, Jacob CK, Kirubakaran MG, Shastry JC, Date A. Renal amyloidosis with ankylosing spondylitis. J Assoc Physicians India. 1984;32:1069–1070.
- Lehtinen K. Cause of death in 79 patients with ankylosing spondylitis. Scand J Rheumtol. 1980;9:145–147.
- Bielsa O, Romero JA, Alcaraz A, Secondary bladder amyloidosis. A rare cause of hematuria. Actas Urol Esp. 1990;14:76–77.
- Ben Taarit C, Ajlani H, Ben Moussa F, Ben Abdallah T, Ben Maïz H, Khedher A. Renal involvement in ankylosing spondylitis: Concerning 210 cases. Rev Med Interne. 2005;26:966–969.
- Hayashi T, Kojima S, Sekine H, Mizuguchi K. Primary localized amyloidosis of the ureter. Int J Urol. 1998;5:383–385.
- Nurmi MJ, Ekfors TO, Rajala PO, Puntala PV. Intravesical dimethyl sulfoxide instillations in the treatment of secondary amyloidosis of the bladder. J Urol. 1990;143:808–810.
- Kobak S, Oksel F, Kabasakal Y, Doganavsargil E. Ankylosing spondylitis-related secondary amyloidosis responded well to etarnercept: A report of three patients. Clin Rheumatol. 2007;26:2191–2194.