Abstract
Objective: Resistive index (RI) is an indirect measurement of blood flow resistance that can be used to evaluate vascular damage in ophthalmologic diseases. The purpose of this study was to evaluate the association between RI values of orbital arteries by using the color Doppler imaging (CDI) in type II diabetes mellitus (DM) patients with microalbuminuria. Patients and methods: We evaluated 91 type II DM patients with microalbuminuria and 27 healthy subjects. The DM patients with microalbuminuria were grouped into two: group 1 consisted of patients with retinopathy (n = 51) and group 2 consisted of patients without retinopathy (n = 40). Healthy subjects constituted group 3 (n = 27). The mean RI values of ophthalmic artery (OA), central retinal artery (CRA), and posterior ciliary artery (PCA) were measured using CDI. Results: Compared to diabetic group 2, group 1 had significantly higher mean RIs of OA, CRA, PCA, and HbA1c levels (p < 0.001 for all). Besides, there were no statistical differences in mean RIs of OA, CRA, and PCA between the control group and group 2 (p = 1.0; p = 0.44; p = 0.67, respectively). Mean RIs of OA and PCA were significantly correlated with age in group 1 (r = 0.549, p < 0.001; r = 0.407, p = 0.003, respectively). Mean RI of CRA was significantly correlated with the duration of diabetes and age in group 1 (r = 0.296, p = 0.035; r = 0.486, p < 0.001, respectively). Conclusion: Our study indicates that RI might be a useful marker for early diagnosis and follow-up of diabetic retinopathy, and orbital RI assessment would be beneficial for diabetic patients with retinopathy.
INTRODUCTION
The resistive index (RI) is a widely used measure of resistance to arterial flow and is calculated from the color Doppler imaging (CDI).Citation1,2 CDI is a noninvasive, safe, and useful method that provides morphologic and vascular information in various diseases. Circulatory parameters in the retrobulbar blood vessels are one of them.Citation3,4 Diabetes mellitus (DM) alters vascular resistance in eyes and is a major risk factor for arteriosclerosis, and advanced arteriosclerosis occurs with increasing age, which indicates long duration of diabetes.Citation5–9 However, there have been many difficulties for earlier diagnosis of diabetic retinopathy. Several studies have been performed to clarify this issue, and RI of orbital arteries has been found to be increased in patients with diabetic retinopathy compared to healthy subjects.Citation10–15 Beyond these studies, we aimed in this study to evaluate the association between RI values of orbital arteries with or without diabetic retinopathy by using the CDI in type II DM patients with microalbuminuria.
MATERIALS AND METHODS
Study Design and Patients
This cross-sectional study was conducted at the Unit of Nephrology of Bagcılar Education and Research Hospital, Istanbul, Turkey. Prior to subject recruitment, the study protocol was reviewed and approved by the local ethics committee, in accordance with the ethical principles for human investigations, as outlined by the Second Declaration of Helsinki and written informed consents were obtained from all the patients. Between June 2009 and September 2010 consecutively 91 age–gender-matched type II DM patients with microalbuminuria and 27 healthy controls were recruited to the study.
Diabetic patients were divided into two groups according to the presence (group 1) or absence (group 2) of retinopathy. Healthy subjects constituted the control group (group 3). Fundus examination was performed in all patients by a trained ophthalmologist using direct and indirect ophthalmoscopy. The RIs of the ophthalmic artery (OA), central retinal artery (CRA), and posterior ciliary artery (PCA) were measured in all patients. The exclusion criteria were as follows: eyes that had an ophthalmic condition that could interfere with the OAs, such as glaucoma, age-related macular degeneration, and high myopia, as well as those with laser photocoagulation or previous ophthalmic surgery.
Baseline Definitions and Measurements
The diagnosis of DM was based on the American Diabetes Association 2010 criteria and on a previous history of diabetes (antidiabetic medications usage).Citation16 Height and weight were measured according to standardized protocols. Body mass index was calculated as the weight in kilograms divided by the height in meters squared (kg/m2). Blood pressure was measured using a mechanical sphygmomanometer in the medical office setting. In each subject, after 15 minutes of comfortably sitting, the average of three BP measurements was calculated.
Measurement of RI by Orbital Color Doppler Imaging
The left and right eyes were examined in all patients to assess RIs of the OA, CRA, and PCA. After resting patients for 10 minutes, all CDI examinations were performed by the same experienced sonographer using a Hitachi EUB 515 (Hitachi Medical Corp., Tokyo, Japan) analyzer with a 7.5-MHz linear transducer. Before the examination, room temperature was brought to optimal level and CDI was performed with the gain adjusted to avoid artifactual color noise, thus allowing detection of low velocities. Scans of the eye were performed in the supine position with a 30° head extension, with eyes closed. Angle of the transducer was taken as 30°–60° during the examination. The transducer was applied to the closed upper eyelid using an ophthalmic sterile gel, with the examiner’s hand resting on the orbital margin to minimize the pressure on the globe. After the exclusion of orbital pathologies by B-mod, CDI was performed. The patients were asked to be at the same position for assessing the RIs of CRA and PCA and were asked to look the other side during evaluating right or left eye for assessing the RI of OA. Optic nerve was taken as reference for all of the measurements. The RI of OA was measured near the nasal side of the optic nerve where it crosses OA, behind the 3–5 cm of globe. CRA was visualized on the localization of the optic nerve head and measurements were taken 5–10 mm behind the optic disc. The RI of PCA was measured on both sides of the optic nerve shadow, just behind the globe and slightly posterior of the CRA. Peak systolic velocity (PSV; the highest velocity achieved during a systole), end diastolic velocity (EDV; the lowest velocity achieved during a diastole), and RI = (PSV − EDV)/PSV) of assessed vessels were measured for every patient. All ultrasonographic assessments were performed by the same experienced radiologist to prevent interobserver variabilities. Intraobserver variability for CDI measurements was <5%.
Biochemical Analysis
All blood samples were collected from antecubital vein while the patient was fasting for 12 h overnight and in supine position. HbA1c was measured by high-performance liquid chromatography. Urinary albumin was measured in 24-h urine collections by immunoturbidimetry. In all study subjects, 24-h urine collections were performed to determine the level of urinary albumin excretion (UAE). Estimated glomerular filtration rate (eGFR) was calculated by using the modification of diet in renal disease formula.Citation17 The patient was considered to have microalbuminuria, if UAE was 30–300 mg/24 h, or normoalbuminuria, if UAE was <30 mg/24 h.
Statistical Analysis
All statistical analyses were performed using SPSS for Windows version 17.0 (SPSS, Chicago, IL, USA). Mean RI values (mean of the right and left eyes) of the OA, CRA, and PCA were calculated. Kolmogorov–Smirnov tests were used to test the normality of data distribution. The data were expressed as arithmetic means and standard deviations. The chi-square test was used to compare the categorical variables between groups. One-way ANOVA with a post hoc Bonferroni and Kruskall–Wallis tests were used in normally and nonnormally distributed continuous data, respectively. Independent sample T-test was used for comparison of continuous variables between the two diabetic groups. Pearson’s correlation analysis was used to examine the association of demographic and biochemical variables with orbital Doppler indices in diabetic patients with retinopathy. Binary logistic regression analysis was performed to determine independent predictors of diabetic retinopathy. Receiver operating curve (ROC) analysis was also performed to investigate the predictive indicators of diabetic retinopathy. Two-sided p-value <0.05 was considered statistically significant.
RESULTS
Clinical, laboratory, and demographic characteristics of control and diabetic subjects are presented in . There were no statistical differences in gender, age, body mass index, and eGFR between the control and diabetic subjects (p > 0.05 for all). Compared with group 2, group 1 had significantly higher mean RIs of OA, CRA, PCA, and HbA1c levels (p < 0.001 for all), whereas there were no statistical differences in mean RIs of OA, CRA, and PCA between the control group and group 2 (p = 1.0; p = 0.44; p = 0.67, respectively).
Table 1. Comparison of the demographic, laboratory, and clinical characteristics of diabetic and control patients.
In bivariate analysis mean RIs of OA and PCA were significantly correlated with age (r = 0.549, p < 0.001; r = 0.407, p = 0.003, respectively) (A and B). Mean RI of CRA was significantly correlated with the duration of diabetes and age (r = 0.296, p = 0.035; r = 0.486, p < 0.001, respectively) (C and D). The binary logistic regression analysis revealed that mean RIs of OA (chi-square: 41.43, beta: −27.28, p < 0.001) and HbA1c (chi-square: 6.72, beta: −0.43, p = 0.040) were independent risk factors for retinopathy.
Figure 1. (A) Relationship between mean resistive index (RI) of ophthalmic artery and age (r = 0.549, p < 0.001). (B) Relationship between mean RI of posterior ciliary artery and age (r = 0.407, p = 0.003). (C) Relationship between mean RI of central retinal artery and age (r = 0.486, p < 0.001). (D) Relationship between mean RI of central retinal artery and diabetes duration (r = 0.296, p = 0.035).
Figure 2. Graph demonstrating receiver operating curve (ROC) analysis of RI of OA and diabetic retinopathy with area under the curve of 0.849.
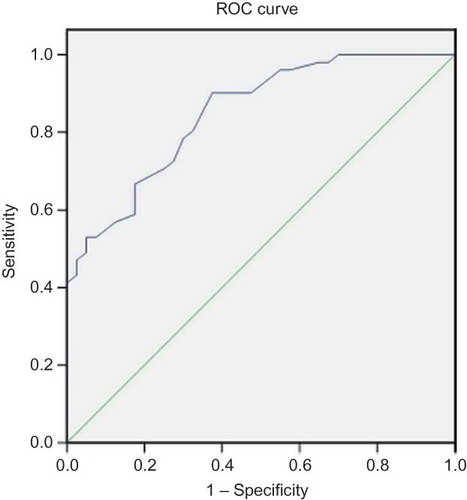
ROC analysis revealed that RIs of OA, CRA, PCA and HbA1c were found 0.849, 0.668, 0.736, 0.621 with area under the curve, respectively. ROC analysis revealed that RI of OA ≥ 0.72 indicated the presence of diabetic retinopathy with sensitivity of 78.4% and specificity of 70% [area under the curve of 0.849 (95% confidence interval: 0.774–0.925)] ().
DISCUSSION
To the best of our knowledge, this is the first report to evaluate the RI of orbital arteries in type II DM patients with microalbuminuria. The main findings of this study were as follows: (Citation1) orbital vascular resistance in diabetic patients with retinopathy is higher than in diabetic patients without retinopathy and healthy individuals, (Citation2) RIs of all arteries were significantly correlated with age, (Citation3) RIs of OA and HbA1c were the independent predictors for diabetic retinopathy, and (Citation4) analysis of ROC for sensitivity and specificity revealed that the RI of OA ≥ 0.72 predicts the presence of diabetic retinopathy with sensitivity of 78.4% and specificity of 70% with area under the curve of 0.849.
CDI may be a method for the evaluation of vascular hemodynamics of retinal vessels and provides morphologic and vascular information in various diseases such as in diabetic retinopathy.Citation4 Several studies reported that the RI of CRA increased in patients with diabetic retinopathy than that in patients without retinopathy and normal subjects.Citation10–13 Dimitrova et al. reported that RIs of OA, CRA, and PCA are significantly increased in patients with diabetic retinopathy than in control subjects.Citation14 Tamaki et al. also suggested that RI of OA is significantly increased in patients either with or without diabetic retinopathy than in normal subjects.Citation15 All of these reports suggest that disturbances in the retrobulbar ocular circulation take place before the clinical manifestation of diabetic retinopathy. In our study, all orbital RI values of patients with diabetic retinopathy were shown to be significantly increased when compared with patients without retinopathy and control subjects. Besides this, on logistic regression analysis, only the mean RIs of OA and HbA1c levels were the independent predictors of diabetic retinopathy.
Several studies have investigated the effects of glycemic control on retrobulbar circulatory parameters in diabetic patients.Citation6,13,18 Goebel et al. reported that no significant correlation existed between the measurements of orbital artery blood velocities obtained by CDI and blood glucose levels in patients at various stages of diabetic retinopathy.Citation6 However, Kawagishi et al. reported that, in type I diabetic patients without retinopathy, plasma glucose levels had a significant effect on the RI of the CRA.Citation13 Also Lieb et al. showed that a significant positive correlation was reported between the velocity parameters in the CRA and fasting blood sugar in patients with early diabetic retinopathy.Citation18 In our study, HbA1c levels were significantly increased in patients with diabetic retinopathy than in patients without retinopathy. However, no significant correlations were found between RI values of all orbital arteries and HbA1c levels.
Type of diabetes, age of the patient, duration of diabetes, and metabolic control may influence ocular circulation.Citation4 The duration of diabetes is the main determining factor in the development of diabetic retinopathy.Citation19–22 Hernandez et al. reported that, as the duration of diabetes increased, there was a decrease in the blood flow in CRA and an increase in resistance in the OA.Citation23 Our study showed that there was a positive correlation between the duration of diabetes and RI values of CRA, but not of OA and PCA. Significant correlations were found between age and RI values of all orbital arteries in diabetic patients with retinopathy, as well.
Certain limitations of this study should be considered. First, sample size was relatively small and design of the study was cross-sectional. Another potential limitation was the operator-dependent nature of ultrasonography although it is noninvasive, easily performed, and a confidential method for evaluating CDI.
CONCLUSIONS
CDI allows rapid, noninvasive evaluation of the orbital hemodynamic abnormalities. RI may be useful as one of the markers for early diagnosis and follow-up of diabetic retinopathy. Therefore when DM is diagnosed, orbital RI values should be measured by CDI for prior prediction of orbital complications. Large-scale prospective studies on ocular circulation are needed to clarify this issue in future.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
REFERENCES
- Halpern EJ, Merton DA, Forsberg F. Effect of distal resistance on Doppler US flow patterns. Radiology. 1998;206:761–766.
- Angeid-Backman E, Coleman BG, Arger PH, Jacobs JE, Langer JE, Horii S. Comparison of resistive index versus pulsatility index in assessing the benign etiology of adnexal masses. Clin Imaging. 1998;22:284–291.
- Conkbayir I, Yücesoy C, Edgüer T, Yanik B, Yaşar Ayaz U, Hekimoğlu B. Doppler sonography in renal artery stenosis. An evaluation of intrarenal and extrarenal imaging parameters. Clin Imaging. 2003;27:256–260.
- Dimitrova G, Kato S. Color Doppler imaging of retinal diseases. Surv Ophthalmol. 2010;55:193–214.
- MacIsaac RJ, Panagiotopoulos S, McNeil KJ, . Is nonalbuminuric renal insufficiency in type 2 diabetes related to an increase in intrarenal vascular disease? Diabetes Care. 2006; 29:1560–1566.
- Goebel W, Lieb WE, Ho A, Sergott RC, Farhoumand R, Grehn F. Color Doppler imaging: A new technique to assess orbital blood flow in patients with diabetic retinopathy. Invest Ophthalmol Vis Sci. 1995;36:864–870.
- Yamasaki Y, Kawamori R, Matsushima H, . Atherosclerosis in carotid artery of young IDDM patients monitored by ultrasound high-resolution B-mode imaging. Diabetes. 1994; 43:634–639.
- Heptinstall RH, ed. Hypertension II essential hypertension. In: Pathology of the Kidney. 3rd ed., Chap. 5. Boston, MA: Little Brown and Company; 1983:181–246.
- Garcia MJ, McNamara PM, Gordon T, Kannel WB. Morbidity and mortality in diabetics in the Framingham population. Sixteen year follow-up study. Diabetes. 1974;23:105–111.
- Arai T, Numata K, Tanaka K, . Ocular arterial flow hemodynamics in patients with diabetes mellitus. J Ultrasound Med. 1998;17:675–681.
- MacKinnon JR, O’Brien C, Swa K, Aspinall P, Butt Z, Cameron D. Pulsatile ocular blood flow in untreated diabetic retinopathy. Acta Ophthalmol Scand. 1997;75:661–664.
- Dimitrova G, Kato S, Yamashita H, . Relation between retrobulbar circulation and progression of diabetic retinopathy. Br J Ophthalmol. 2003;87:622–625.
- Kawagishi T, Nishizawa Y, Emoto M, . Impaired retinal artery blood flow in IDDM patients before clinical manifestations of diabetic retinopathy. Diabetes Care. 1995;18:1544–1549.
- Dimitrova G, Kato S, Tamaki Y, . Choroidal circulation in diabetic patients. Eye (Lond). 2001;15:602–607.
- Tamaki Y, Nagahara M, Yamashita H, Kikuchi M. Blood velocity in the ophthalmic artery determined by color Doppler imaging in normal subjects and diabetics. Jpn J Ophthalmol. 1993;37:385–392.
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33:62–69.
- Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: A new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130:461–470.
- Lieb WE, Flaharty PM, Sergott RC, . Color Doppler imaging provides accurate assessment of orbital blood flow in occlusive carotid artery disease. Ophthalmology. 1991;98:548–552.
- Nathan DM, Singer DE, Godine JE, Harrington CH, Perlmuter LC. Retinopathy in older type II diabetics. Association with glucose control. Diabetes. 1986;35:797–801.
- Aliello LM, Cavallerrano JD. Ocular complications of diabetes mellitus. In: Kahn CR, Weir GC, eds. Joslin’s Diabetes Mellitus. 13th ed. Philadelphia, PA: Lea & Febiger; 1994:771–793.
- Krolewski AS, Warram JH, Freire MB. Epidemiology of late diabetic complications. A basis for the development and evaluation of preventive programs. Endocrinol Metab Clin North Am. 1996;25:217–242.
- Chen MS, Kao CS, Chang CJ, . Prevalence and risk factors of diabetic retinopathy among noninsulin-dependent diabetic subjects. Am J Ophthalmol. 1992;114:723–730.
- Gil Hernández MA, Abreu Reyes P, Quintero M, Ayala E. Doppler ultrasound in type I diabetes: Preliminary results. Arch Soc Esp Oftalmol. 2001;76:175–180.
