Abstract
Increased plasma catecholamine levels are associated with a high risk of perioperative cardiac events in aged individuals undergoing non-cardiac surgical interventions. Given the different effects of β1-adrenoreceptor (β1AR) and β2-adrenoreceptor (β2AR) stimulation by catecholamine in cardiomyocytes, this study evaluated whether simultaneous inhibition of β1AR and activation of β2AR is better than separate application in reducing the risk of perioperative cardiac events in aged rats undergoing non-cardiac surgery. Male aged Sprague–Dawley (SD) rats were divided into five groups. Normal group received no treatment. Surgery group received an abdominal surgery with hypoxia. group,
group and
group received surgery and hypoxia with metoprolol (100 mg/kg·d), fenoterol (250 μg/kg·d) or both, respectively. The drugs were given three days before surgery with treatment continued through post-surgical day 7. The results showed that simultaneous activation of β2AR with a β2AR agonist and inhibition of β1AR with a selective β1AR blocker normalized myocardial oxygen consumption, decreased myocardial damage, augmented cardiomyocyte survival, improved cardiac function, reduced the incidence of arrhythmia, thus decreasing the occurrence of cardiac events in perioperative aged rats undergoing non-cardiac surgery. The results demonstrated that combined use of β2AR agonist and β1AR blocker achieved better general effects than use of either one alone. Our results provide a new insight into preventing perioperative cardiac events for elderly patients undergoing surgical stress.
Introduction
Increased life expectancy, safer anesthesia and less invasive surgical techniques have led to more aged patients to consider surgical intervention. It has been pointed out that aging increases the likelihood of perioperative cardiac events in non-cardiac surgery, and that age is an independent predictor of perioperative events (Poldermans et al., Citation2008). Aging itself is associated with elevated myocardial and serum norepinephrine levels (Ahmed, Citation2003; Kaye & Esler, Citation2008). Surgical stress causes elevated catecholamine release leading to changes in myocardial energetics, reflecting the process of oxygen metabolism, aerobic/oxygenic supply balance and the relationship with cardiac work. These are the major causes of perioperative cardiac events.
Age-related cardiac changes include decrease in contractility, beta-adrenoceptor expression, beta-adrenoceptor mediated modulation of inotropy and chronotropy, and increases in stiffness, ventricular filling pressures, left atrial pressure/size as well as cardiac action potential time (Deneer & van Hemel, Citation2011; Maruyama, Citation2012). All of the changes are possible candidates for explaining increased perioperative cardiac risk in the elderly. Moreover, these factors interact with each other, which may cause additional complications. Appropriate perioperative management of the elderly patients may reduce perioperative cardiovascular morbidity and mortality.
Initial approaches to balance post-surgical myocardial energetics included the use of β-blocking drugs. Drugs originally used were non-selective β1 adrenoceptor receptor (β1AR) and β2 adrenoceptor receptor (β2AR) agents, such as propranolol. Blockade of both the β1AR and β2AR results in a state of predominant α receptor stimulation that results in hypertension and increased myocardial stress (Rehsia & Dhalla, Citation2010). β1AR selective agents (such as bisoprolol) are more effective. But the adverse effects of β1AR blocker, as in the case of bradycardia, increased airway resistance, and negative inotropic effect of cardiomyocytes, have become a stumbling block to large scale application (VanDenKerkhof et al., Citation2003), especially in the elderly (Zaugg et al., Citation2002). Some studies have shown that patients treated with β1AR blocker therapy developed myocardial ischemia at a lower heart rate than those receiving placebo (Suttner et al., Citation2009).
It is well known that β2AR activation has a protective effect on myocardial contraction, reducing cardiac afterload by dilating peripheral vasculature, and decreasing airway resistance, antagonizing the side effects of β1AR blocker. In addition, it was also reported that β2AR stimulation could protect cardiomyocytes (Zhang et al., Citation2010). Animal experiments also showed that the combined use of selective β1AR blocker and β2AR agonist was better than use of β1AR blocker alone in the treatment of heart failure (Ahmet et al., Citation2008). Finally, it was also found that the physiological function of β2AR could significantly strengthen the aged heart during heart failure (Brodde, Citation2007).
Based on these preliminary findings, we postulated that simultaneous activation of β2AR and inhibition of β1AR would be particularly beneficial in preventing cardiac events during perioperative period in aged individuals. The study investigated whether combination of β1AR blocker and β2AR agonist had better heart protection than use of either alone in the aged rats undergoing surgical stress.
Materials and methods
Animals
Approval for the experiments was obtained in advance from the Animal Ethics Committee of Xuzhou Medical College (permit number: xz10-12379) and all studies conformed to the Guide for the Care and Use of Laboratory Animals published by the US National Institutes of health (NIH publication No. 85-23, revised 1996). Male adult and aged Sprague–Dawley (SD) rats (180–200 g, 3–4 months old; 540–600 g, 20–22 months old, clean grade, Xuzhou Medical College) were used in these experiments.
Aged rats were randomly assigned to five groups. Normal aged group (normal group) received no treatment. Surgery aged group (surgery group) received a surgical procedure only. group were treated with metoprolol (Shanghai-AstraZeneca plc, China; Intragastric administration, 100 mg/kg·d) and a surgical procedure.
group were treated with fenoterol (Sigma-Aldrich, St. Louis, MO; Intragastric administration, 250 μg/kg·d) and a surgical procedure.
group were treated with both metoprolol (100 mg/kg·d) and fenoterol (250 μg/kg·d) and a surgical procedure. Each group was further divided into five subgroups: preoperation group (Pre), intraoperation group (Ope), and day 1, 3, 7 post-operative groups (Day 1; Day 3; Day 7). Metoprolol and/or fenoterol were dissolved in water and given from three days before the surgical procedure until the rats were euthanatized at the end of the experiment. ECG, hemodynamics, rate-pressure product (systolic blood pressure × heart rate/100, RPP), the release of lactate dehydrogenase (LDH), amplitude of cardiomyocytes contractions were recorded at different time points for analyses.
Surgical procedure
The surgical procedure was performed as follows: rats were given pentobarbital (150 mg/kg, i.p) with ketamine (20 mg/kg) and xylazine (8 mg/kg) for anesthesia and analgesia. Then, an abdominal incision was made extending from the lower most point of the xiphoid to the upper most point of the pubis (about 4 cm in length). The abdominal right and left flaps were stabilized by means of sutures (5-0) to expose the peritoneum. A part of the intestines (5 to 8 cm in length) were exteriorized. Then, the operated rats were put into a low oxygen equipment (oxygen concentration: 12–13%) for 90 min to increase the stress levels, and hence increase the incidence of cardiac events. Finally, the exteriorized intestines were put back and the abdomen was sutured.
Rats were nursed round-the-clock during the first 48 h after surgery. Assessments for post-operative pain were run systematically to determine whether animals require analgesics. They were then assessed every 8 h. If the following signs occurred, buprenorphine 0.05 mg/kg (subcutaneous injection) was administered for relieving pain: decreased water and food intake; decreased locomotor activity; cat-like stretching or horizontal stretching (i.e. rat horizontal on the ground); or withering or twitching. There was no evidence of (1) anorexia, (2) dehydration, (3) respiratory distress or (4) porphyrin staining at the eyes and/or nostrils during this study.
There was 6 and 2% mortality in the surgery and the group, respectively. All these rats died from sudden cardiac arrest during surgical procedure. According to the design which was approved in advance of the experiments from the Animal Ethics Committee of the Medical College of Xuzhou (permit number: xz10-12379), we compared whether simultaneous inhibition of β1AR and activation of β2AR is better than separate application in reducing the risk of perioperative cardiac events in aged rats undergoing non-cardiac surgery. Therefore, in the experiments, if cardiac events occurred, the animals were allowed to progress to death as a direct result of the experimental procedures.
Hemodynamic and electrocardiographic measurements
The heart rate (HR), left ventricle end-diastolic pressure (LVEDP) and the maximal rate of change in left ventricle pressure (±dp/dtmax) were measured by means of a 2-French Millar catheter (Millar Instruments, Houston, TX) inserted into the left ventricle through the right carotid artery. Another catheter flushed with heparinized saline was inserted into a femoral artery for blood sampling and mean arterial blood pressure (MAP) measurement. The ECG was obtained by the second lead (following a normal ECG procedure). Catheters and the lead were connected to Powerlab system (PowerLab, Sydney, Australia) and the data were displayed and monitored in real time.
Measurement of epinephrine, norepinephrine and LDH
A sample of about 2 ml blood, taken from tail vein, was centrifuged at 2000 rpm for 15 min. The ensuing supernatant was collected and stored in the refrigerator (−80 °C). Plasma epinephrine and norepinephrine were measured by high-pressure liquid chromatography (SRL, Tokyo, Japan). All samples were assayed in triplicate.
The LDH concentration was assayed spectrophotometrically as described previously (Wu et al., Citation2008). Supernatant were used for the determination of LDH. Spectrophotometric enzyme activity assay (Beckman DU-650, Beckman Coulter, Inc., Brea, CA) was performed with a UV kinetic assay kit (Sigma-Aldrich). This test relies on the reduction of pyruvate to lactate catalyzed by LDH, which results in an equimolar amount of NADH oxidized to NAD. The oxidation of NADH results in a decrease in the absorbance at 340 nm. The rate of decrease in absorbance at 340 nm is directly proportional to LDH activity in the sample.
Ventricular myocytes isolation
Ventricular myocytes were isolated using methods described previously (Hao et al., Citation2009; Xu et al., Citation2010). Isolated hearts were perfused for 5 min with Ca2+-free buffer, then, switched to the same perfusion buffer containing 0.04% collagenase, 0.1% bovine serum albumin, and 50 μM CaCl2. The perfusate was recirculated for 25 min. Next, the hearts were removed from the perfusion cannula and the left ventricles were cut into small pieces in Krebs–bicarbonate (KB) solution (pH 7.2). Myocytes were harvested and filtered through a 200 μm nylon mesh, then resuspended in KB solution and stabilized for at least 30 min before measurement of ventricular myocyte contraction. After isolation, 83–87% of the viable myocytes were quiescent.
Survival rates of isolated cardiomyocytes
Rod-shaped cells are the viable cells, and round-shaped cells are non-viable cells. The cells were counted under an inverted microscope. Five micrographs were taken randomly per sample, and all rod-shaped and round-shaped myocytes in these fields were measured. A total of 300–400 cells were counted for one condition of one preparation. The percentage of rod cells in total cells was calculated. The analysis of the cells was done under blind conditions.
Indexes of cardiac complications
Cardiac complications were defined as myocardial ischemia, cardiac arrhythmia, cardiac arrest or cardiac death by ECG changes during the perioperative period. The arrhythmia assessment is based on the ECG recorded from extremities in standard lead II. Ventricular bigeminy, ventricular trigeminy and frequent premature ventricular contractions were counted as arrhythmia.
Data analysis
Data were presented as mean ± standard deviation and one-way analysis of variance (ANOVA) followed by the Bonferroni post-hoc test, which was used for multiple comparisons of means among groups. Chi-square test with a Bonferroni-correction was conducted to test differences of probability of occurring arrhythmia. Fisher’s exact test was used for comparing the differences of probability of occurring myocardial ischemia and mortality. Statistical significance was set at p < 0.05, except for when the Bonferroni correction was used for multiple comparisons, in which case statistical significance was set at p < 0.05/6 = 0.0083.
Results
Operation with hypoxia elevated plasma catecholamine level, especially in aged rats
We assessed circulating catecholamine levels to determine whether operation and hypoxia created a stress state. In adult rats, operation with hypoxia caused 11.6-fold and 4.2-fold increases in plasma epinephrine and norepinephrine, respectively. In aged rats, operation with hypoxia caused 17.9-fold and 7.7-fold increases in plasma epinephrine and norepinephrine, respectively (; ). Surgery with hypoxia increased plasma epinephrine and norepinephrine levels much higher in aged rats than in adult rats [; for epinephrine: F (7, 24) = 4.334; p < 0.01; for norepinephrine: F (7, 24) = 3.852; p < 0.01].
Figure 1. Fold increase of plasma epinephrine and norepinephrine induced by operation and hypoxia. The results were expressed as the fold increase of plasma epinephrine or norepinephrine level in operated rats relative to normal rats. Mean ± SD. n = 7 rats in each group. **p < 0.01 versus corresponding normal adult or aged rats; ##p < 0.01 versus operated adult.
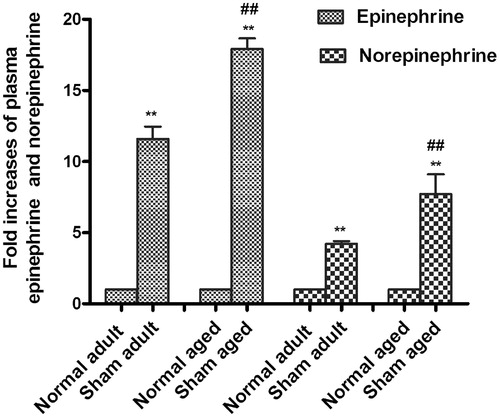
Table 1. Operation and hypoxia elevated plasma epinephrine and norepinephrine.
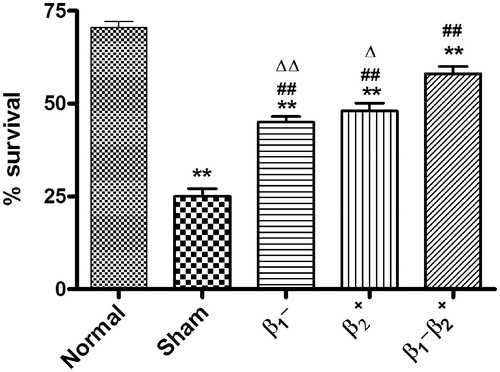
Combined use of selective β1AR blocker and β2AR agonist increased the survival rates of cardiomyocytes
Operation with hypoxia decreased the survival rate of isolated cardiac myocytes [; F (4, 30) = 6.81; p < 0.01]. Selective β1AR blocker metoprolol or selective β2AR agonist fenoterol augmented the survival rate [; for metoprolol: F (4, 30) = 2.984; p < 0.05; for fenoterol: F (4, 30) = 3.495; p < 0.05]. Combined use of both further improved the survival rate [; F (4, 30) = 4.802; p < 0.01; group versus
group. F (4, 30) = 3.694; p < 0.05;
group versus
group, respectively].
The effects of combined use of selective β1AR blocker and β2AR agonist on the MAP and HR
There was no significant difference of MAP between normal and any other groups before operation. The MAP in all groups decreased during the operation [; F (4, 45) = 8.333; p < 0.05], then slowly returned towards normal. The MAP of group remained at a lower level. The maximum fluctuations of MAP appeared in the surgery group.
Figure 3. Combined use of selective β1AR blocker and β2AR agonist smoothed the fluctuations of MAP and HR in the perioperative period. a: Changes in MAP in the perioperative period. b: Changes in HR in the perioperative period. Each value represents the mean ± SD. n = 10 rats in each group. *p < 0.05 versus normal group at corresponding time point; #p < 0.05 versus surgery group at corresponding time point; $p < 0.05 versus group at corresponding time point; Δp < 0.05 versus
group at corresponding time point. Pre: day 3 after administration (pre-operation); Ope: intra-operation; Day 1: day 1 after surgery; Day 3: day 3 after surgery; Day 7: day 7 after surgery.
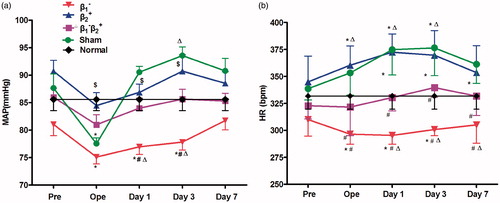
The HR of group was decreased relative to controls, while the HR in surgery group and
group were elevated [; F (4, 45) = 10.41; p < 0.05]. The MAP and HR in the
group presented no significant differences, compared with normal controls.
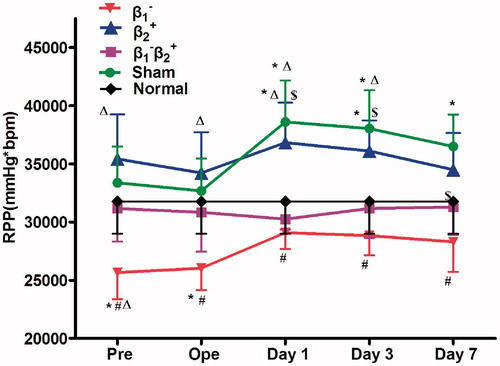
The effects of combined use of selective β1AR blocker and β2AR agonist on the RPP
During the perioperative period, RPP in the surgery group and group increased markedly at day 1 and day 3 after surgery. RPP in
group was significantly lower than controls [; F (4, 45) = 7.263; p < 0.05]. Combined use of selective β1AR blocker and β2AR agonist adjusted RPP to normal level.
Figure 4. Combined use of selective β1AR blocker and β2AR agonist normalized RPP in the perioperative period. Each value represents the mean ± SD. n = 10 rats in each group. *p < 0.05 versus normal group at corresponding time point; #p < 0.05 versus surgery group at corresponding time point; $p < 0.05 versus group at corresponding time point; Δp < 0.05 versus
group at corresponding time point. Pre: day 3 after administration (pre-operation); Ope: intra-operation; Day 1: day 1 after surgery; Day 3: day 3 after surgery; Day 7: day 7 after surgery.
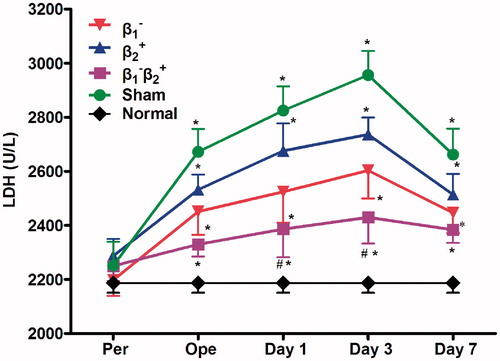
Combined use of selective β1AR blocker and β2AR agonist decreased the release of LDH
Compared with the normal group, the release of LDH in the surgery group began to increase during intra-operative period, and reached the highest level at day 3 after surgery, then gradually returned to normal level. Either selective β1AR blocker or β2AR agonist decreased the release. The strongest effect was obtained following combined use of both [; F (4, 45) = 15.19; p < 0.05].
Figure 5. Combined use of selective β1AR blocker and β2AR agonist decreased the release of LDH in the perioperative period. Each value represents the mean ± SD. n = 10 rats in each group. *p < 0.05 versus normal group at corresponding time point; #p < 0.05 versus surgery group at corresponding time point; Pre: day 3 after administration (pre-operation); Ope: intra-operation; Day 1: day 1 after surgery; Day 3: day 3 after surgery; Day 7: day 7 after surgery.
Combined use of selective β1AR blocker and β2AR agonist improved the cardiac function
The LVEDP was increased gradually after operation in surgery group and group or
group. Combined use of selective β1AR blocker and β2AR agonist completely recovered the LVEDP to normal level [; F (4, 45) = 10.33; p < 0.05].
Figure 6. Combined use of selective β1AR blocker and β2AR agonist improved LVEDP and ±dP/dtmax in the perioperative period. a: Changes in LVEDP in each group. b: Changes in +dp/dtmax in each group. c: Changes in −dp/dtmax in each group. Each value represents the mean ± SD. n = 10 rats in each group.*p < 0.05 versus normal group at corresponding time point; #p < 0.05 versus surgery group at corresponding time point; $p < 0.05 versus at corresponding time point; Pre: day 3 after administration (pre-operation); Ope: intra-operation; Day 1: day 1 after surgery; Day 3: day 3 after surgery; Day 7: day 7 after surgery.
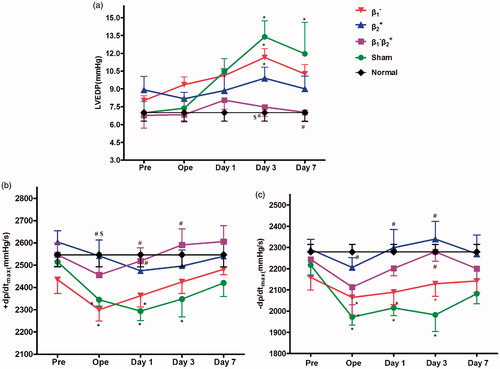
Rats in surgery group and group showed significant decreases in ±dP/dtmax, compared to normal rats. β2AR agonist alone or combined use of β1AR blocker and β2AR agonist improved the recovery of ±dP/dtmax [; F (4, 45) = 9.872; p < 0.05. ; F (4, 45) = 14.76; p < 0.05].
The effects of combined use of selective β1AR blocker and β2AR agonist on contraction of single cardiomyocytes
Compared with the normal group, there were no significant differences in shortening amplitudes among ,
and
group before surgery. But the shortening amplitudes of
group were lower than those of
group or
groups. During the perioperative period, the shortening amplitudes of surgery group and
group decreased significantly [; F (4, 30) = 17.25; p < 0.05]. The shortening amplitudes did not change in the
and
groups.
Figure 7. Selective β1AR blocker or/and β2AR agonist changed myocytes shortening amplitudes in the perioperative period. Each value represents the mean ± SD. n = 7 rats in each group. *p < 0.05 versus normal group at corresponding time point; #p < 0.05 versus surgery group at corresponding time point; $p < 0.05 versus group at corresponding time point; Pre: day 3 after administration (pre-operation); Day 1: day 1 after surgery; Day 3: day 3 after surgery; Day 7: day 7 after surgery.
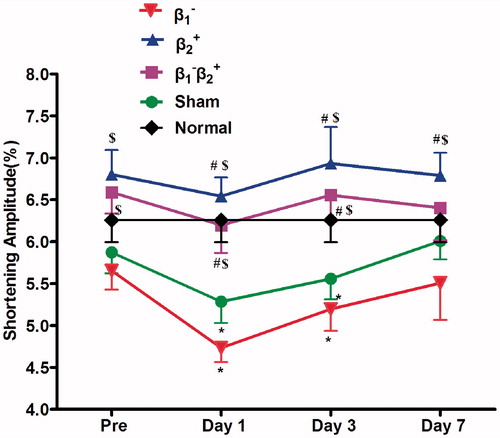
At day 1 after surgery, TTP in the and
groups was shorter than that of the surgery group [; F (4, 30) = 5.351; p < 0.05].
Table 2. The time to peak contraction (TTP, ms) of cardiomyocytes.
The R90 was longer in the and
groups compared with those in the normal group after a 3-day administration. The R90 maintained at normal level and was longer in the
group than that in the surgery group at day 1 after surgery [; F (4, 30) = 7.158; p < 0.05].
Table 3. The time to 90% relaxation (R90, ms) of cardiomyocytes.
Combined use of selective β1AR blocker and β2AR agonist reduced cardiac complications
ECG showed that the incidence of arrhythmia, including ventricular bigeminy, ventricular trigeminy, premature ventricular contractions, ventricular tachycardia, was 28% in the surgery group (; ). Cardiac changes were significantly inhibited by combined use of β1AR blocker and β2AR agonist. Paroxysmal ventricular tachycardia occurred more readily in group. The occurrence of myocardial ischemia was 8, 3, 3% in the surgery group,
group,
group, respectively. However, myocardial ischemia did not occur in the
group. The mortality was 6 and 2% in surgery group and
group, respectively. All the rats in the
and
groups survived.
Figure 8. ECG recorded from extremities in standard lead II. a: Normal ECG; b: Ventricular bigeminy occurred in surgery group; c: Ventricular trigenimy occurred in surgery group; d: Frequent premature ventricular contractions occurred in surgery group; e: Myocardial ischemia occurred in surgery group; f: Paroxysmal ventricular tachycardia occurred in group.
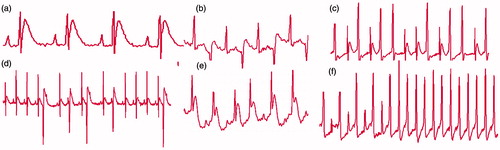
Table 4. The rate of cardiac complications.
Discussion
Our results demonstrated that combined use of a β1AR blocker, metoprolol and a β2AR agonist, fenoterol, was more effective than using single one alone in normalizing MAP and HR, improving hemodynamic changes, lowering myocardial oxygen consumption and reducing the incidence of cardiac complications during the perioperative period in aged non-cardiac surgery rats. These data provide new evidence for perioperative cardiac protection afforded by simultaneously stimulating β2AR and inhibiting β1AR in the aged animals undergoing non-cardiac surgery.
Aging increases perioperative cardiac events for two major causes: (a) anesthesia and surgical trauma as well as a hyperadrenergic state related to perioperative stress, hypoxia and hypovolemia leading to an increased myocardial oxygen demand (Stoschitzky, Citation2001); and (b) aging itself is associated with an increased activation of the sympathetic nervous system (Kaye & Esler, Citation2005). The overall cardiovascular response to high concentration of catecholamine increased myocardial oxygen demand and systemic vascular resistance (Engebretsen et al., Citation2011), which promotes the damage of cardiac muscle.
To mimic this situation, we generated a non-cardiac surgery with a hypoxia model to test cardiac function in aged rats. We found that the operation and hypoxia increased plasma norepinephrine and epinephrine levels in aged rats relative to younger adults, indicating that aged rats have more sympathetic activation in response to these stimuli. Our non-cardiac surgery and hypoxia aged rat model met the conditions of age increasing perioperative cardiac events.
Combined use of selective β1AR blocker and β2AR agonist normalized myocardial oxygen consumption, decreased myocardial damage
RPP is a sensitive index of myocardial oxygen consumption. Measurements of the RPP were obtained from HR and MAP. RPP increased significantly during perioperative period. The β1AR blocker decreased RPP and maintained it at lower level. This was to a large extent due to the decrease of BP and HR, which might lead to impairment of coronary perfusion and results in myocardial ischemia. Activation of β2AR can increase the perfusion by dilating coronary arteries, decrease peripheral resistance by activating the β2ARs of the peripheral vasculature (Ahmet et al., Citation2004). β2AR agonist can increase myocardial contractility and cardiac output (Xiao et al., Citation2003). Pharmacological experiments revealed that β2AR activation specifically regulates intracellular oxygen availability in cardiomyocytes. The β2AR-Gi-eNOS pathway is involved in this regulation (Li et al., Citation2010). β2AR activation increased the AMP/ATP ratio, AMPK activity, ROS production and prolyl hydroxylase activity. Our results indicate that combined use of a selective β1AR blocker with a β2AR agonist kept the RPP at the normal level during perioperative period.
A small amount of cardiomyocyte injury or necrosis is known to be sufficient to cause the increasing activity of LDH, which is an enzyme localized to cardiomyocyte (Metzler et al., Citation2001). Our results indicated that the release of LDH began to increase during the operation, and reached the highest level on day 3 after surgery, then gradually returned to the normal level. Combined use of selective β1AR blocker and selective β2AR agonist reduced LDH more than the use of either one alone.
Our previous studies found that inhibition of β1AR with CGP20712A increased the survival of myocytes injured by isoprenaline, whereas inhibition of β2AR with ICI 118551 decreased the survival in vitro (Sun et al., Citation2006). These results suggested that inhibition of β1AR or activation of β2AR provided protection to cardiomyocytes. However, it does not appear that simultaneous treatment of myocytes with both drugs resulted in a greater improvement.
This studies clearly indicated that in vivo inhibition of β1AR with metoprolol and excitation of β2AR with fenoterol increased the survival rate of cardiac myocytes following operation and hypoxia better than either alone. The results can be explained by different roles of β1AR and β2AR in response to adrenergic stimulation. Bristow et al. (Citation1986) demonstrated that in the normal heart, myocardial contractility in response to an adrenergic stimulation is mediated via both β1AR and β2AR, with most of the inotropic response of the normal heart mediated via β1AR. Stimulation of β1AR, which activates the Gs-protein pathway, can promote apoptosis of cardiomyocytes. Stimulation of β2AR results in coupling with both Gs proteins which mediated positive inotropic effect and Gi proteins, which has antiapoptotic and cardioprotective effects.
Both β1AR and β2AR stimulation can activate Gs and increase cAMP/PKA signaling, increasing cardiac myocytes contraction. Xiao et al. (Citation2003) reported that there may be some advantages of using fenoterol rather than β1AR agonists to provide contractile support in the failing heart. Ahmet et al. (Citation2008) found that, unlike β1AR stimulation, β2AR stimulation by fenoterol does not induce cardiac myocyte apoptosis. Perhaps this is because of distinct compartmentalization of cAMP signal in response to different βAR subtype activation (Rybin et al., Citation2000). The β1 and β2AR are located in different regions of the cardiomyocytes. In cardiomyocytes from healthy adult rats and mice, it was spatially confined that β2AR-induced cAMP signals are localized exclusively to the deep transverse tubules, whereas functional β1ARs are distributed across the entire cell surface (Nikolaev et al., Citation2010).
Combined use of selective β1AR blocker and β2AR agonist improved cardiac function
Regarding cardiac function, the present study confirmed that combined use of β1AR blocker and β2AR agonist improved the cardiac functions by restraining the decrease of ±dp/dt, inhibiting the increase of LVEDP of aged rats in the perioperative period. These were consistent with the results obtained from the contraction amplitude of the single myocyte. The amplitude of single myocyte shortening was increased, the R90 was lengthened, and the RTT was shortened in and
groups, compared with those in the surgery group. These indices reflecting cardiac function are closer to normal levels in the
group than in any other group.
Combined use of selective β1AR blocker and β2AR agonist improves cardiac function on at least two aspects. First, stimulation of β2AR improved myocyte contraction and increased myocyte survival. Second, inhibition of β1AR counteracted the cardiotoxicity of chronic adrenergic signaling. Under certain pathological conditions or stress, stimulation of high concentration of catecholamines causes β1AR desensitization and down-regulation. The resulting partial loss of β1AR function is believed to be an adaptive mechanism to counteract the cardiotoxicity of chronic adrenergic signaling. This hypothesis is supported by the fact that β1-adrenergic blockade has proved to be effective in the treatment of chronic heart failure (Hossain et al., Citation2009). Ahmet et al. (Citation2008) found that in the rat experimental model of dilated cardiomyopathy post-myocardial infarction, combined therapy with the β1AR blocker and the β2AR agonist is effective and exceeds either single therapy alone. Addition of β1AR blocker (i.e. combination of ) prevented the reduction in β2AR density. β1AR blockade alone or in combination with the β2AR agonist rescued the reduction of β1AR number. The same group also found that the better therapeutic effects of chronic β1AR blockade, supplemented with β2AR stimulation, on cardiac remodeling following heart failure (Ahmet et al., Citation2005).
Combined use of selective β1AR blocker and β2AR agonist reduced the incidence of arrhythmia
In the present study, β1AR blocker decreased the occurrences of arrhythmic, myocardial ischemia and mortality, but the benefit was not statistically significant, compared with the surgery group or the group. However, combination of the use of selective β1AR blocker and β2AR agonist had the lower morbidity, in terms of arrhythmias.
It is well known that enhanced sympathetic activation can provoke large increases in intracellular calcium by evoking increases in ICa-L through β1- or β2-adrenoceptors. The resulting elevations in intracellular Ca2+ concentration could trigger oscillations in membrane potential and reduce the electrical stability of the heart that could culminate in the induction of malignant arrhythmias (Billman et al., Citation2006). Selective β1AR blockers are commonly used in the treatment of cardiac arrhythmia, which produce less inhibition of the β2AR that mediate bronchodilation or peripheral vasodilatation (Ahmet et al., Citation2008; Brodde, Citation2008). On the other hand, coupling of rat β2AR to pertussis toxin (PTX)-sensitive Gi protein was reported to prevent Gs protein-mediated increases in Ca2+ transients and myocyte contractions and relaxations through these receptors (Christ et al., Citation2009). Maybe through these mechanisms, β1AR blockade in combination with the β2AR agonist reduced the cardiac arrhythmias. Suppression of fatal ventricular arrhythmias resulted in the reduction of mortality.
Implications and limitations
Over 200 million people receive major non-cardiac surgical procedures every year. At least 2% of elective non-cardiac procedures result in perioperative cardiac complications, which account for up to a third of postoperative deaths. Elderly patients undergoing major surgery are at higher risk for serious perioperative cardiac complications (Wijeysundera et al., Citation2011). Our results provide a new insight for preventing cardiac events during perioperation in aged patients. However, we only selected a single β1 adrenergic receptor blocker and single β2 agonists, and only one dose was used.
Both β1AR blocker and β2AR agonist are used clinically. Further studies are needed to collect clinical information and estimate the correlation between cardiac events and administration of β1AR blocker or β2AR agonist either or both during perioperative period from the patients with non-cardiac surgery.
Conclusions
The present study proved that simultaneous activation of β2AR with β2AR agonist and inhibition of β1AR with selective β1AR blocker normalized myocardial oxygen consumption decreased myocardial damage, augmented cardiomyocytes survival, improved cardiac function, reduced the incidence of arrhythmia, therefore, decreased the occurrence of cardiac events during the perioperative period in aged rats undergoing non-cardiac surgery. The general effects of the combined use of β2AR agonist and β1AR blocker appear to be superior to either treatment alone.
Declaration of interest
There are no financial or other interests with regard to the paper that represent a conflict of interest.
This study was supported by the National Natural Science Foundation of China (No. 81370329).
Acknowledgements
We thank Youjian Qi, Xuzhou Medical College, for the technical assistance, and Medical Statistics analysis Center of Xuzhou Medical College, for their kind help in data analysis.
References
- Ahmed A. (2003). Myocardial beta-1 adrenoceptor down-regulation in aging and heart failure: implications for beta-blocker use in older adults with heart failure. Eur J Heart Fail 5:709–15
- Ahmet I, Krawczyk M, Heller P, Moon C, Lakatta EG, Talan MI. (2004). Beneficial effects of chronic pharmacological manipulation of beta-adrenoreceptor subtype signaling in rodent dilated ischemic cardiomyopathy. Circulation 110:1083–90
- Ahmet I, Krawczyk M, Zhu W, Woo AY, Morrell C, Poosala S, Xiao RP, et al. (2008). Beta(2)-adrenoceptor agonist clenbuterol reduces infarct size and myocardial apoptosis after myocardial ischaemia/reperfusion in anaesthetized rats. J Pharmacol Exp Ther 325:491–9
- Ahmet I, Lakatta EG, Talan MI. (2005). Pharmacological stimulation of beta2-adrenergic receptors (beta2AR) enhances therapeutic effectiveness of beta1AR blockade in rodent dilated ischemic cardiomyopathy. Heart Fail Rev 10:289–96
- Billman GE, Kukielka M, Kelley R, Moustafa-Bayoumi M, Altschuld RA. (2006). Endurance exercise training attenuates cardiac beta2-adrenoceptor responsiveness and prevents ventricular fibrillation in animals susceptible to sudden death. Am J Physiol Heart Circ Physiol 290:H2590–9
- Bristow MR, Ginsburg R, Umans V, Fowler M, Minobe W, Rasmussen R, Zera P, et al. (1986). Beta 1- and beta2-adrenergic-receptor subpopulations in nonfailing and failing human ventricular myocardium: coupling of both receptor subtypes to muscle contraction and selective beta1-receptor down-regulation in heart failure. Circ Res 59:297–309
- Brodde OE. (2007). Beta-adrenoceptor blocker treatment and the cardiac beta-adrenoceptor-G-protein(s)-adenylyl cyclase system in chronic heart failure. Naunyn Schmiedebergs Arch Pharmacol 374:361–72
- Brodde OE. (2008). Beta-1 and beta-2 adrenoceptor polymorphisms: functional importance, impact on cardiovascular diseases and drug responses. Pharmacol Ther 117:1–129
- Christ T, Galindo-Tovar A, Thoms M, Ravens U, Kaumann AJ. (2009). Inotropy and L-type Ca2+ current, activated by beta1- and beta2-adrenoceptors, are differently controlled by phosphodiesterases 3 and 4 in rat heart. Br J Pharmacol 156:62–83
- Deneer VH, van Hemel NM. (2011). Antiarrhythmic treatment in the elderly different? A review of the specific changes. Drugs Aging 28:617–33
- Engebretsen KM, Kaczmarek KM, Morgan J, Holger JS. (2011). High-dose insulin therapy in beta-blocker and calcium channel-blocker poisoning. Clin Toxicol (Phila) 49:277–83
- Hao Y, Sun Y, Xu C, Jiang X, Sun H, Wu Q, Yan C, Gu S. (2009). Improvement of contractile function in isolated cardiomyocytes from ischemia-reperfusion rats by ginkgolide B pretreatment. J Cardiovasc Pharmacol 54:3–9
- Hossain M, Rashid M, Bhuiyan MA, Nakamura T, Ozaki M, Nagatomo T. (2009). Mutagenesis of important amino acid reveals unconventional homologous internalization of beta(1)-adrenergic receptor. Life Sci 85:339–44
- Kaye D, Esler M. (2005). Sympathetic neuronal regulation of the heart in aging and heart failure. Cardiovasc Res 66:256–64
- Kaye DM, Esler MD. (2008). Autonomic control of the aging heart. Neuromolecular Med 10:179–86
- Li J, Yan B, Huo Z, Liu Y, Xu J, Sun Y, Liu Y, et al. (2010). β2- but not β1-adrenoceptor activation modulates intracellular oxygen availability. J Physiol 588:2987–98
- Maruyama Y. (2012). Aging and arterial-cardiac interactions in the elderly. Int J Cardiol 155:14–19
- Metzler B, Mair J, Lercher A, Schaber C, Hintringer F, Pachinger O, Xu Q. (2001). Mouse model of myocardial remodelling after ischemia: role of intercellular adhesion molecule-1. Cardiovasc Res 49:399–407
- Nikolaev VO, Moshkov A, Lyon AR, Miragoli M, Novak P, Paur H, Lohse MJ, et al. (2010). β2-adrenergic receptor redistribution in heart failure changes cAMP compartmentation. Science 327(5973):1653–7
- Poldermans D, Hoeks SE, Feringa HH. (2008). Preoperative risk assessment and risk reduction before surgery. J Am Coll Cardiol 51:1913–24
- Rehsia NS, Dhalla NS. (2010). Mechanisms of the beneficial effects of beta-adrenoceptor antagonists in congestive heart failure. Exp Clin Cardiol 15:e86–95
- Rybin VO, Xu X, Lisanti MP, Steinberg SF. (2000). Differential targeting of β-adrenergic receptor subtypes and adenylyl cyclase to cardiomyocyte caveolae: amechanism to functionally regulate the cAMP signaling pathway. J Biol Chem 275:41447–57
- Stoschitzky K. (2001). Beta-blockers and non-cardiac surgery. J Clin Basic Cardiol 4:21–3
- Sun H, Zhou F, Wang Y, Zhang Y, Chang A, Chen Q. (2006). Effects of beta-adrenoceptors overexpression on cell survival are mediated by Bax/Bcl-2 pathway in rat cardiac myocytes. Pharmacology 78:98–104
- Suttner S, Boldt J, Mengistu A, Lang K, Mayer J. (2009). Influence of continuous perioperative beta-blockade in combination with phosphodiesterase inhibition on haemodynamics and myocardial ischaemia in high-risk vascular surgery patients. Br J Anaesth 102:597–607
- VanDenKerkhof EG, Milne B, Parlow JL. (2003). Knowledge and practice regarding prophylactic perioperative beta blockade in patients undergoing noncardiac surgery: a survey of Canadian anesthesiologists. Anesth Analg 96:1558–65
- Wijeysundera DN, Beattie WS, Karkouti K, Neuman MD, Austin PC, Laupacis A. (2011). Association of echocardiography before major elective non-cardiac surgery with postoperative survival and length of hospital stay: population based cohort study. Brit Med J 342:d3695
- Wu Q, Zhao Z, Sun H, Hao YL, Yan CD, Gu SL. (2008). Oestrogen changed cardiomyocyte contraction and beta-adrenoceptor expression in rat hearts subjected to ischaemia-reperfusion. Exp Physiol 93:1034–43
- Xiao RP, Zhang SJ, Chakir K, Avdonin P, Zhu W, Bond RA, Balke CW, et al. (2003). Enhanced G(i) signaling selectively negates beta2-adrenergic receptor (AR) – but not beta1-AR-mediated positive inotropic effect in myocytes from failing rat hearts. Circulation 108:1633–9
- Xu C, Liu A, Sun H, Wang G, Gao L, Hao Y, Yan C. (2010). beta2- Adrenoceptor confers cardioprotection against hypoxia in isolated ventricular myocytes and the effects depend on estrogenic environment. J Recept Signal Transduct Res 30:255–61
- Zaugg M, Schaub MC, Pasch T, Spahn DR. (2002). Modulation of beta-adrenergic receptor subtype activities in perioperative medicine: mechanisms and sites of action. Br J Anaesth 88:101–23 (Review)
- Zhang Q, Xiang J, Wang X, Liu H, Hu B, Feng M, Fu Q. (2010). Beta(2)-adrenoceptor agonist clenbuterol reduces infarct size and myocardial apoptosis after myocardial ischaemia/reperfusion in anaesthetized rats. Br J Pharmacol 160:1561–72