Abstract
Objective: To evaluate the long-term effectiveness of lifestyle counselling for low-moderate cardiovascular (CV) risk subjects in primary care. Methods: Design: Prospective comparison of baseline vs post-intervention, and comparison of enrolled patients vs control subjects extracted from a large primary care database. Setting: 94 general practices in Italy. Participants: All the 20-70-year-old hypercholesterolaemic subjects who did not qualify for statin treatment according to the guidelines and who were seen on 12 predetermined working days; 713 patients; 94 general practitioners. Intervention: Short (5-10 min) educational intervention (qualitative dietary advice, encouraging walking or other aerobic physical activities); handing out simple dietetic advice at physician discretion. Main outcome measures: Total cholesterol level and global CV risk calculated according to the Framingham equation. Results: Total cholesterol and global CV risk (10 years) decreased by 0.31 mmol/l (p < 0.0001, 95% CI 0.23-0.40) and 1.35% (p < 0.01, 95% CI -1.73 to -0.97), respectively, after a 54-month follow-up. Enrolled patients showed a greater total cholesterol decrease than control patients: 2.24% (p < 0.05, 95% CI 0.58-3.91%).
Conclusions: A simple, office-based, long-term, lifestyle counselling programme produces a small, but clinically significant reduction of total cholesterol and of global CV risk. This result should encourage GPs to systematically offer simple, unstructured lifestyle counselling to all their patients.
International guidelines (Citation1) recommend non-pharmacological interventions for hypercholesterolaemia in subjects at low or moderate global cardiovascular risk (CVR); almost all these patients are treated by general practitioners (GPs). Physicians face increasing pressure to counsel their hypercholesterolaemic patients. According to the prevalence of hypercholesterolaemia in western countries, a great number of subjects should be involved in lifestyle counselling. On the other hand, as far as we know, data on the effectiveness of lifestyle counselling in primary care is scarce and controversial (Citation2–6), and long-term results are almost completely lacking. Realistic data on effectiveness of “spontaneous” counselling in real practice are of paramount relevance.
We report the results of lifestyle counselling obtained over a 5-year period by a self-established group of Italian GPs. This intervention involved hypercholesterolaemic individuals not eligible for statin treatment according to the European guideline on prevention of coronary heart disease (Citation7).
Methods
In 2000, a small group of GPs, members of the Italian College of General Practitioners working in a central region of Italy (Umbria), decided to improve the primary prevention of cardiovascular diseases, focusing on their patients with high blood cholesterol, according to the 1998 European guideline (Citation7). They proposed their initiative to other GPs. Overall, 94 GPs, working in different regions of Italy, joined the group. They all agreed on the following routine intervention: a) calculation of global CVR, b) short (5-10 min) educational intervention for hypercholesterolaemic subjects (qualitative dietary advice, encouraging walking or other aerobic physical activities), c) handing out simple dietetic advice at physician's discretion, and d) prescription of statins in high-risk patients. Interventions b) and c) could be repeated, if considered useful by the GPs. The participants also decided to verify the results of their efforts. The high number of patients potentially involved and the burden of the paperwork needed to monitor all of them discouraged the GPs from periodically sending individual reports for every single subject who received a preventive intervention. The group thus decided to monitor the results every year in a randomly selected subgroup of patients: all the 20-70-year-old subjects who were seen on 12 predetermined working days (one day for every month from February 2000 to January 2001). The observation period ended on the last day of 2005; the last available lipid values recorded in 2005 were used for the analysis. In this paper, we describe only the results of the non-pharmacological intervention in primary prevention (all patients had no cardiovascular disease at baseline). Since baseline versus end-of-study cholesterol values were considered insufficient to evaluate the effectiveness of the intervention, the authors asked the Italian College of General Practitioners to provide control patients (“usual care patients”) using the Heath Search Database. The characteristics of the database have been described elsewhere (Citation8). The Health Search Database has been used to survey the everyday practice of Italian GPs (www.healthsearch.it) and to provide data to Italian Heath Authorities (Citation9); it contains the clinical records of over 1 million patients. The database was searched to identify one control for every case. The criteria to identify a control were the following: a) age (±2 years ), b) gender, c) no CHD recorded before January 2001, d) recorded total cholesterol both in the first and the last year of the study, e) no lipid-lowering prescription in the study period, and f) baseline total cholesterol (±0.38 mmol/l).
We used Student's t test (two-tailed, for individually paired case-control study) to compare baseline and end-of-study lipid levels and global CVR (Framingham algorithm) (Citation7). Logistic regression analysis was used to identify predictors of drop-out at follow-up. Statistical analyses were made using the statistical software SPSS v. 10.1 (SPSS Inc., Chicago, Ill., USA).
Results
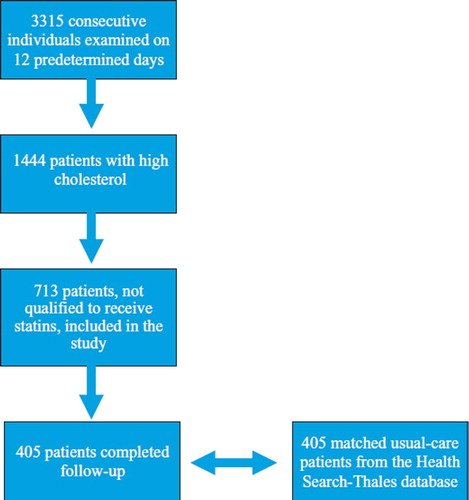
Overall, 3315 patients were included in the monitored group. Of these, 1444 had “high” total cholesterol (> 5.18 mmol/l) at baseline (two determinations at different time points). Seven hundred and thirteen patients with “high” cholesterol did not qualify for statin treatment according to the guidelines (Citation4) and received only lifestyle counselling. Only these subjects are included in this study; their characteristics are summarized in . We examined the differences between the patients lost at follow-up and those who completed the study for the following variables: age, gender, family history of CHD, smoking habits, obesity (body-mass index [BMI] > 30 kg/m2), diabetes mellitus, hypertension (blood pressure ≥ 140/90 mmHg and/or anti-hypertensive drug treatment), and total cholesterol (). The two groups significantly differed for all these variables. The logistic regression analysis identified age and cholesterol level as having a significant inverse association with dropping-out at follow-up.
Table I. Baseline characteristics of the patients with and without completed follow-up.
Follow-up was completed for 405 subjects (56.8%); the mean follow-up was 54,2 months (range 47-60, SD ±3.75). We calculated the global CVR according to the Framingham algorithm (Citation7). shows the study flowchart.
Since high-density lipoprotein (HDL) values were not available in 63 subjects at baseline and 86 at end of study, we calculated the means of the available values (baseline: 1.24 mmol/l and 1.43 mmol/L for men and women, respectively; end of study: 1.37 mmol/l and 1.52 mmol/l for men and women, respectively), and we used those values for the subjects with missing data. The baseline and end-of-study lipid levels, smoking habits, and blood pressure values are reported in . Absolute differences for total cholesterol, HDL cholesterol, triglycerides, and global CVR were –0.31 mmol/l (p < 0.0001, 95% CI -0.40 to -0.23), +0.09 mmol/l (p < 0.0001, 95% CI 0.05-0.13), -0.13 mmol/l (p < 0.01, 95% CI -0.22 to -0.05), and –1.35% (p ≤ 0.01, 95% CI -1.73% to -0.97%), respectively. For every patient who completed the follow-up, a matched control patient was identified in the Health Search Database. We did not correct our analysis for the clustering effect, because the mean number of cases (4.3) and controls (3.8) per single GP were similar and close to the single unit.
Table II. Baseline and end-of-study lipid levels, blood pressure, smoking habits, and global CVR
The mean total cholesterol relative and absolute improvement was greater for the intervention group (-2.24%, p < 0.05, 95% CI -3.91 to -0.58; and –0.16 mmol/l, p < 0.01, 95% CI -0.26 to -0.06, respectively), while no significant changes were observed for HDL cholesterol (-0.16 mmol/l, 95% CI -0.11 to +0.03) and for triglycerides (-0.6 mmol/l, 95% CI -1.29 to +0.09).
Discussion
Hypercholesterolaemia is an important and common CV risk factor in western countries. According to the international guidelines (Citation1), pharmacological therapy should be limited to high-risk subjects, while lifestyle interventions are the sole preventive measures for low- and moderate-risk individuals, who represent not only the largest part of the population, but also the group which pays the highest toll to CV diseases as far as the absolute number of events is concerned. Primary prevention is almost exclusively delivered by primary care on a long-term basis. The efficacy of lifestyle improvement has been well demonstrated by trials (Citation1), while the long-term effectiveness on lipid reduction in “real-world” practice has been scarcely studied, with inconclusive or modest results (Citation2–6). Furthermore, long-term studies on moderate-low CV risk subjects in general practice are almost completely non-existent. This lack of evidence may contribute to the scepticism regarding counselling that can be observed in the GPs’ everyday practice (Citation10). Evaluation of simple, non-expensive interventions that can easily “fit” in everyday practice is of paramount importance if thousands of GPs are supposed to counsel millions of people; over 57% of people aged 35-74 years are hypercholesterolaemic in Italy (Citation11). The effectiveness should also be evaluated in the long-run, according to the characteristics of primary prevention.
Our data show a small, but significant decrease of total cholesterol (0.32 mmol/l) over a 5-year period. We also found that there was no decrease in HDL cholesterol, as reported after dietary advice in general practice in the UK (Citation4). In British practices (Citation12), dietary advice over a 6-month period has been shown to be equally effective when given by a dietician, a practice nurse, or a diet leaflet alone, but resulted in only a small reduction in total and low-density lipoprotein cholesterol: the mean total cholesterol concentration fell by 1.9% (0.13 mmol/l, 95% CI 0.06 to 0.22, p < 0.001). This result is very similar to that reported by the Cochrane collaboration (Citation13): dietary advice reduces total serum cholesterol by 0.13 mmol/l (95% CI 0.03 to 0.23) and low-density lipoprotein (LDL) cholesterol by 0.13 mmol/l (95% CI 0.01 to 0.25) after 3-12 months, but mean HDL cholesterol levels remain unchanged. The authors conclude that dietary advice appears to be effective in bringing about modest beneficial changes in diet and cardiovascular risk factors over approximately 9 months, but longer-term effects are not known. A more recent study, involving moderate-high CV risk patients, showed that a 1-year structured (supervised diet and exercise programme) intervention improved many risk factors, but not total cholesterol levels (Citation14). As far as we know, only one study (Citation15) with adequate long-term follow-up examined this problem in primary care. It examined health check effects on cholesterol levels in the relatively young (30-49 years) patients of a group of GPs in Denmark, showing that, after 5 years of intervention, the health checks had a measurable impact on plasma cholesterol levels, the most pronounced effect (0.5-mmol/l decrease) being seen among individuals at high cardiovascular risk. Another long-term study (Citation16) is a Dutch community-based intervention based on organized activities which promoted and facilitated healthy lifestyles. After five years, there was a small, statistically significant, total cholesterol adjusted decrease in women (0.11 mmol/l), but not in men (0.06 mmol/l). This study did not directly involve GPs in counselling. Our better results may be due to longer exposure to the intervention and to natural selection of the most motivated subjects. Forty-three per cent of the initially involved individuals did not complete the study. Their mean baseline CV risk was lower than that of the patients who completed the follow-up, and it is therefore possible that they perceived little personal benefit, an insufficient motivation to complete the study.
Blood pressure remained unchanged and smoking cessation is very close to that expected by the natural 1-2% yearly quitting rate; the changes in the lipid levels are the main cause of the small (1.33% over a 10-year period), but significant reduction of the total CV risk. Even such a small improvement is of interest, because it may benefit millions of patients.
The comparison with “usual care” also shows a significant lowering of total cholesterol. It must be observed that, even among the usual-care patients, total cholesterol levels slightly decreased during the 5-year observation period. Furthermore, only a minority (data not shown) of Health Search patients had their total cholesterol recorded both in 2001 and 2005. Our control subjects are probably more committed to CV prevention and better cared for than the general population. In our opinion, this bias strengthens our positive results.
The current study has many limitations. The “mother of all limitations” is that this study was not conceived as a randomized trial, but as a “goodwill” initiative of GPs who decided to improve their practice according to the guidelines and to verify the results of their efforts. For this reason, only a sample of all the counselled patients was used to evaluate the effect of the intervention, and the loss at follow-up was high (43.2%). This is not unexpected, since high losses (up to 33%) at follow-up are reported in general practice even in short (1 year), randomized trials with structured lifestyle intervention in high-risk subjects (Citation17). The patients who did not complete the follow-up significantly differed from the group that completed it. Again, this is not unexpected in real life and, in our opinion, does not change the value of the information provided by the current study. Another important problem is that the “strength” of counselling for each individual patient was left to the judgement of each individual GP. For these reasons, our results should be cautiously interpreted. We are fully aware of the methodological weakness of our study, but we considered it important to communicate our findings when thousands of GPs are urged to offer time-consuming counselling to millions of people without adequate evidence about the real effectiveness of such an intervention. We think that our data provide important information on the effectiveness of counselling in real practice, where “tailored” lifestyle counselling and missed control visits are common and where only the most interested patients can be involved in lifestyle improvement.
Our results support the commonsense strategy of offering simple lifestyle counselling to every moderate-low CV risk patient, then focusing re-enforcement efforts on the most interested ones. This intervention is very similar to the recommended “minimal advice” for quitting cigarette smoking (Citation18) and should be recognized as a routine activity in everyday practice; time and economic resources should be also planned accordingly.
Conclusions
In “real life”, only half of moderate-low CV risk patients can be involved in a simple, office-based, long-term, lifestyle counselling programme. In this group, a small, but clinically significant reduction of total cholesterol and of global CV risk is possible. These results are particularly important considering that millions of people could benefit from this low-cost intervention. Our results should encourage GPs to systematically offer simple, unstructured lifestyle counselling to all their patients.
Acknowledgements
We wish to thank all the participant GPs; without their generous help, this study could never have been conceived. This study was supported by an unconditioned educational grant by Bayer Schering Pharma.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- De Backer G, Ambrosioni E, Borch-Johnsen K, Brotons C, Cifkova R, Dallongeville J, . European guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2003; 24:1601–10.
- Ashenden R, Silagy C, Weller D. A systematic review of the effectiveness of promoting lifestyle chance in general practice. Fam Pract. 1997; 14:160–76.
- Van Sluijs EM, van Poppel MN, van Mechelen W. Stage-based lifestyle interventions in primary care: are they effective?. Am J Prev Med. 2004; 26:330–43.
- Price D, Ramachandran S, Knight T, Jones PW, Neary RH. Observed changes in the lipid profile and calculated coronary risk in patients given dietary advice in primary care. Br J Gen Pract. 2000; 50:712–5.
- Ebrahim S, Smith GD. Systematic review of randomised controlled trials of multiple risk factor interventions for preventing coronary heart disease. BMJ. 1997; 314:1666–74.
- Brunner EJ, Thorogood M, Rees K, Hewitt G. Dietary advice for reducing cardiovascular risk. Cochrane Database of Systematic Reviews. 2005; Issue 4.
- Wood D, De Backer G, Faergeman O, Graham I, Mancia G, Pyörälä K. Prevention of coronary heart disease in clinical practice. Summary of recommendations of the Second Joint Task Force of European and other Societies on Coronary Prevention. J Hypertens. 1998; 16:1407–14.
- Cricelli C, Mazzaglia G, Samani F, Marchi M, Sabatini A, Nardi R, . Prevalence estimates of chronic diseases in Italy: exploring the differences between self-report and primary care databases. J Public Health Med. 2003; 25:254–7.
- Osservatorio Nazionale sull'impiego dei farmaci: L'uso dei farmaci in Italia. Annual report. Available from URL: http://www.agenziafarmaco.it
- Brotons C, Ciurana R, Piñeiro R, Kloppe P, Godycki-Cwirko M, Sammut MR. Dietary advice in clinical practice: the views of general practitioners in Europe. Am J Clin Nutr. 2003; 77Suppl 4:1048S–51S.
- . Italian Atlas of Cardiovascular Diseases. Ital Heart J. 2003; 4Suppl 4:9S–121S.
- Neil HAW, Roe L, Godlee RJP, Moore JW, Clark GMG, Brown J, . Randomised trial of lipid lowering dietary advice in general practice: the effects on serum lipids, lipoproteins, and antioxidants. BMJ. 1995; 310:569–73.
- Ebrahim S, Davey Smith G. Multiple risk factor interventions for primary prevention of coronary heart disease (Cochrane Review).In: The Cochrane Library, Issue 1, 2004.
- Eriksson KM, Westborg CJ, Eliasson MC. A randomized trial of lifestyle intervention in primary healthcare for the modification of cardiovascular risk factors. Scand J Public Health. 2006; 34:453–61.
- Kanstrup H, Refsgaard J, Engberg M, Lassen JF, Larsen ML, Lauritzen T. Cholesterol reduction following health screening in general practice. Scand J Prim Health Care. 2002; 20:219–23.
- Schuit AJ, Wendel-Vos GC, Verschuren WM, Ronckers ET, Ament A, Van Assema P, . Effect of 5-year community intervention Hartslag Limburg on cardiovascular risk factors. Am J Prev Med. 2006; 30:237–42.
- Willaing I, Ladelund S, Jørgensen T, Simonsen T, Nielsen LM. Nutritional counselling in primary health care: a randomized comparison of an intervention by general practitioner or dietician. Eur J Cardiovasc Prev Rehabil. 2004; 11:513–20.
- Brief interventions and referral for smoking cessation in primary care and other settings. Available from URL: http://www.nice.org.uk