Abstract
The ‘Research Agenda for General Practice/Family Medicine and Primary Health Care in Europe’ summarizes the evidence relating to the core competencies and characteristics of the Wonca Europe definition of GP/FM, and its implications for general practitioners/family doctors, researchers and policy makers. The European Journal of General Practice publishes a series of articles based on this document. The previous articles presented background, objectives, and methodology, as well results on ‘primary care management’ and ‘community orientation’ and the person-related core competencies of GP/FM. This article reflects on the general practitioner's ‘specific problem solving skills’. These include decision making on diagnosis and therapy of specific diseases, accounting for the properties of primary care, but also research questions related to quality management and resource use, shared decision making, or professional education and development. Clinical research covers most specific diseases, but often lacks pragmatism and primary care relevance. Quality management is a stronghold of GP/FM research. Educational interventions can be effective when well designed for a specific setting and situation. However, their message that ‘usual care’ by general practitioners is insufficient may be problematic. GP and their patients need more research into diagnostic reasoning with a step-wise approach to increase predictive values in a setting characterized by uncertainty and low prevalence of specific diseases. Pragmatic comparative effectiveness studies of new and established drugs or non-pharmaceutical therapy are needed. Multi-morbidity and complexity should be addressed. Studies on therapy, communication strategies and educational interventions should consider impact on health and sustainability of effects.
Background
The ‘Research Agenda for General Practice/Family Medicine and Primary Healthcare in Europe’ was published in September 2009 by the European General Practice Research Network (EGPRN) (Citation1). It summarizes the evidence relating to the core competencies and characteristics of the Wonca Europe definition of General Practice/Family Medicine (GP/FM) (Citation2), and indicates evidence gaps and research needs. The European Journal of General Practice presents this document as a series of articles. Background, objectives and methodology were presented in part 1 (Citation3); results on the two core competencies, which deal with organizational aspects of GP/FM, i.e. ‘primary care management’ and ‘community orientation’ were presented in part 2 (Citation4), and part 3 reflected on results on the three core competencies featuring person related aspects of GP/FM, i.e. ‘person centred care’, ‘comprehensive approach’ and ‘holistic approach’(Citation5) This article presents results related to ‘specific problem solving skills’.
Definition of the research domain
According to the Wonca Europe definition of GP/FM (Citation2) ‘specific problem solving skills’ include the ability to
relate decision making processes to the prevalence and incidence of illness in the community;
selectively gather, interpret and apply information from history-taking, physical examination and investigations, in collaboration with the patient;
adopt incremental investigation, using time as a tool and to cope with uncertainty;
manage conditions which present early or in an undifferentiated way;
make effective and efficient use of diagnostic and therapeutic interventions, both in acute or chronic conditions.
Solving specific medical problems is one of the foremost tasks of the general practitioner/family physician (GP), but effective problem solving and decision making are also related to management, resource use, or professional development. Therefore, this research domain includes substantial parts of clinical research on diagnosis and therapy performed by other medical and scientific disciplines. To be relevant to primary care, clinical and health services research studies must meet specific requirements in research questions, setting, patient selection, and methodology. Finally, epidemiological research in primary care provides the necessary background to develop and apply problem solving competencies. The specific fields and topics to be treated within this large research domain were consented by the research agenda authors as shown in .
Table I. Research topics related to ‘specific problem solving skills’.
Methodology
A general description of the methodology applied when constructing the Research Agenda—key informant surveys, a comprehensive literature review, and expert consensus—was presented in the first part of this series (Citation3). For this part, to identify both well-covered research topics and blank spots, all papers presented at EGPRN conferences from 2001 to 2007 had been classified for their main topic and methodology (Citation6). Additionally, a semi-quantitative overview of research topics was obtained by searching PubMed (2003–2008) for RCTs or clinical trials labelled with the Medical Subject Heading (MeSH) terms ‘family practice’ or ‘general practice’. Papers were classified for their predominant theme, and whether their main outcomes were on a patient level, or doctor or system related.
The research domain of ‘specific problem solving skills’ is particularly vast. Therefore, it was impossible to cover all fields in detail, and choices had to be made. It was not our aim to give an overview of the state of knowledge on individual clinical issues; that is the domain of the Cochrane Collaboration (Citation7) and the many organizations and scientific societies working on meta-analyses and guidelines for primary care. Instead, the Research Agenda aims to highlight general, systematic characteristics or weaknesses of studies in this field. Therefore, we selected exemplary conditions to retrieve and evaluate the evidence on diagnosis and therapy, and to estimate the contribution of general practice research to the field. ‘Sore throat’, linked to ‘pharyngitis’ in MeSH, was chosen as an acute complaint, and ‘heart failure’ as a serious chronic disease to be used as specific disease terms in exemplary searches on diagnosis and therapy. ‘Dysuria/urinary tract infection’ and ‘diabetes’ were other conditions used for exemplary searches. As for conclusions, authors also drew on their general expertise as researchers and reviewers.
Literature on the various fields of was sought using the MeSH terms and combinations as shown in .
Table II. Search strategies: Specific problem solving skills.
Results
Challenges in retrieval and appreciation of literature
Using MeSH, most symptom terms are linked to a disease or diagnosis, which hampers retrieval of studies evaluating symptoms. Many studies from GP/FM, or relevant to primary care, are not labelled with the MeSH terms ‘family practice’ or ‘primary health care’. Frequently, in clinical trials, the exact setting and degree of sample selection are not well described, and thus the external validity or relevance for general practice is not easy to verify. This can also be problematic when interpreting meta-analyses and systematic reviews. There is no consensus on how to judge an RCT's quality and relevance for general practice, though there have been useful attempts to establish a system to rate the quality of research articles, i.e. by the SIGN network, or the GRADE collaboration (Citation8,Citation9). Nevertheless, authors of systematic reviews may come to contradictory conclusions based on the same RCTs, depending on their evaluation of quality, external validity and relevance.
Predominant research themes
The review of the research presented in EGPRN conferences revealed that the largest group of presentations dealt with health services research, including organisation and delivery of care and undergraduate, vocational and continuous professional training, followed by research on therapy and, less common, diagnosis or prevention of specific diseases, most often cardiovascular disorders. As to methodology, practice based prevalence studies, attitude surveys or description of current care were common, mostly with a cross-sectional approach. Longitudinal studies or instrumental research were very rare (Citation4,Citation6).
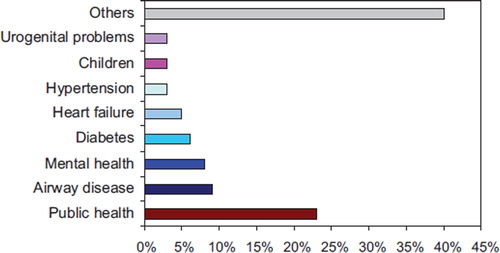
Our MeSH based search for RCTs and clinical trials labelled with the MeSH term ‘family practice’ yielded approximately 500 articles for 2003–2008. This relatively low number is possibly due to the fact that many relevant papers are not labelled with ‘family practice’ or ‘general practice’. Seventy per cent of the retrieved papers had patient-related outcomes, the remainder focussed on doctors or system related outcomes. The most frequent research topics are shown in .
Research on diagnostic reasoning and diagnostic tests
In general, GPs’ symptom- or reason-for-encounter based diagnostic approaches were very poorly reflected in the literature we retrieved. Relatively few papers on symptom assessment could be identified, and these were either on very specific themes or about (unspecific) syndromes. For acute disorders (i.e. sore throat, urinary tract infection), there was some research on symptom scores or utility and predictive values of near-patient tests. However, these were rarely assessed for their added value (increase in positive or negative likelihood of a disease) to history, signs and symptoms. We found a lack of studies addressing diagnostic strategies, step-wise reasoning or diagnostic tests relevant to GPs decision-making and subsequent management.
Most studies on diagnosis focussed on specific, usually sophisticated technical or laboratory tests in selected settings. Evidence on predictive values of diagnostic findings, screening instruments, or tests in unselected or primary care populations was scarce. Many instruments or tests have not been formally evaluated in primary care settings. Nevertheless, in many studies, they are used to screen unselected populations, often yielding unrealistically high prevalence estimates for chronic diseases or concluding that GPs are not good at detecting disease. Quite commonly, these articles then recommend tests for screening of unselected populations, or for identification of patients to be treated. This approach tends to mistake point prevalence of screening results or individual symptoms (not complaints) for an indication to treat (10–31).
Research on therapy
Research evidence can be found related to the treatment of almost any specific disease. However, there is an obvious lack of investigator-initiated trials assessing or comparing established, frequently prescribed drugs or non-pharmaceutical therapies. One reason may be the lack of significant marketing potential and funding. There are few studies comparing several standard treatments, or a standard treatment versus placebo, or different doses of the same drug, or optimal duration of treatment, or safety issues. Many RCTs featured new or expensive drugs and study their efficacy in selected patient samples. Numerous clinical RCTs were relatively small; sometimes they failed to be sufficiently powered for the main outcome and more frequently for secondary effects. Particularly in older studies, comparators were often less than ideal: sometimes, the control treatment is appeared deliberately sub-optimal, being either under-dosed or second-choice. Outcomes are often surrogate markers of questionable value. Often there was selection bias at recruitment (i.e. patients were recruited from walk-in clinics or secondary care, or were either privileged or disadvantaged regarding access to care), and randomisation problems were quite frequent. However, more recent studies tend to be better designed. Relatively few clinical RCTs have been performed in primary care settings (19,32–44).
Many clinical trials suffer from limited external validity, particularly those focussing on chronic diseases (45). Most patients recruited into trials are younger and healthier than the average general practice patients, and those with multiple chronic diseases or women are frequently underrepresented. Pragmatic, large trials of therapies, which are relevant in GP and look at the effectiveness of treatments in everyday settings and typical populations is scarce (46). Although there is some research on alternative/complementary therapy, it is often of relatively poor quality. Non-pharmacological treatment is a rare research topic. We found little research on or accounting for co- or multi-morbidity (47–50).
Research on chronic care
It is estimated that in developed countries the major portion of a GP's working time (up to 80%) is devoted to chronic care (51). So far, most research on problem solving in chronic diseases focussed on single diagnostic or therapeutic strategies or single outcomes. Recently, there has been a growing consensus that chronic care requires integrated, comprehensive and structured models (52,53). However, many studies describe structured models of chronic care that bypass the general practitioner or take ‘usual care’ as a presumably poor comparator. Many intervention studies are designed by specialists, in many cases the (mostly disease specific) intervention is administered by nurses (54). Most of these studies show no or marginal effects; follow-up is usually short.
One challenge for research in general practice may be proving that most of these managed or structured care models add to fragmentation of the healthcare system if they neglect the coordinating role of GP/FM. Several reviews provide evidence for the value of GP-led primary care for chronic diseases (55–57).
Research on (shared) decision making
Many studies refer to particular clinical situations and identified patients’ or doctors’ characteristics associated with particular decisions, usually with a cross-sectional design. Qualitative research explored doctors’ decision making processes or preferences, or the issue of decision making in a situation of uncertainty (58,59). Qualitative methods or specific measurement tools for satisfaction, patient preferences, compliance and involvement were used to explore patients’ experience with consultations in general or shared decision making in particular. Results of these studies were quite variable. A substantial proportion of patients studied were less satisfied with shared decision making than with a classical, more paternalistic consultation style. Patients who prefer shared decision making were usually younger and more educated, or had chronic disorders. A few studies showed that patients who were more involved in their own care fared better. There are multiple studies on decision making tools or aids, mostly related to specific disease related situations, for either doctors (i.e. synthesised evidence, electronic decision support) or patients (i.e. information materials). Some of these studies featured development or implementation with an observational design, whereas others applied a specific tool as an intervention and compared with control groups (see also the paragraph on Educational Research) (60–64).
Research on quality of care
Quality of care and quality management was an early stronghold of general practice researchers (65–69), and is now under the umbrella of the European network organisation EQuIP (70). Major research fields and methods of quality improvement were peer review or quality circle work (71), medical audit (72–74), guideline development and dissemination (75,76), research on implementation strategies (77,78), patient participation (79,80), and quality indicators/quality frameworks (81). A vast body of literature deals with solving specific quality problems, e.g. improving guideline adherence, improving the use of laboratory test results (82) or optimizing prescribing by different methods such as continuing medical education, benchmarking, academic detailing, structured feedback etc. (83). Quite often, and particularly when performed in managed care settings, ‘cost-effectiveness’ featured as a primary outcome in studies on referral, treatment/prescribing, or screening. Doctor related quality of care research included studies on knowledge, but also clinical competence and performance. Guidelines or recommendations were often used as reference standard in studies with a benchmarking approach, though they were originally intended to be decision aids. Several reports targeted patients, often attempting to encourage them to adopt a healthier lifestyle. Multidisciplinary or collaborative care was studies fairly often, as was the issue of frequent attendees. Most ‘quality of care’ studies attempted to show the superiority of a specific intervention as compared to the default ‘usual care’. This approach tends to shed an unfavourable light on general practice, as ‘usual care’ is presumed to be deficient. However, most empirical studies showed only minor (or even no) effect. Despite some important reviews (68,75), a consistent theoretical framework on the rationale and effects of strategies in quality improvement is still lacking.
Research on genetics/genomics in GP/FM
Research papers on genetics/genomics in GP/FM or primary health care generally dealt with either GPs’ or sometimes patients’ views on genetic tests or counselling services, or interventions undertaken to increase their implementation. GPs and patients revealed mostly ambivalent feelings towards the importance and possibilities of genetic medicine, but simultaneously expressed concern about its complex implications on patient management and impact on families. Intervention studies looked at the uptake of services or at attitudes, but not at patients’ health outcomes; results were inconclusive (84–89).
Educational research
We retrieved a large body of literature, including many meta-analyses and RCTs, so only a rough overview can be given. While most studies were not done within the context of primary care/family medicine; they are relevant to this theme as they addressed teaching methods and educational interventions to enhance clinical competence. Early experience in primary care helps medical students to acquire professional attitudes and skills and it can influence career choices (90).
Educational interventions in the context of continuous professional development mostly had small to medium effect on physician knowledge. However, the effect size was generally small with respect to behavioural change, which seems to be a central obstacle to quality improvement (91,92), and even more so for performance and (much more rarely studied) patient outcomes, across many individual educational methods. Dissemination of materials, didactic lectures, but also feedback (when insufficiently specific), seemed to be largely ineffective (93,94). Interventions were somewhat more successful when they were interactive, used multiple methods and were designed for a small group of physicians from a single discipline. Multifaceted interventions aimed at physicians, patients and other stakeholders simultaneously were also shown to be effective, if they were well tailored to local factors such as physicians’ current performance and barriers to change (95). However, even thoughtfully designed interventions could be unsuccessful. Bias was probably introduced by the fact that most quality of care studies relied on volunteer participants. These self-selected practices probably performed better at baseline and tended to implement experimental strategies better than average practices. There is very little research on the sustainability of teaching/learning effects, in particular on interventions targeting practising physicians. Instrumental research on assessment methods for educational studies is needed (96–101).
Implications for research and research methodology
Descriptive, cross-sectional surveys and attitude studies are unlikely to add much knowledge in most countries and settings. Nevertheless, large primary care registries on a sound data basis (e.g. QRESEARCH) (102) will increasingly be used for non-experimental studies, for example, primary care epidemiology, longitudinal observational studies of the prognosis of symptoms and diseases, or association studies of socioeconomical, environmental and health risk factors and co morbidity with health outcomes, research on rare events, or the health impact of care interventions, i.e. desired or undesired effects of medication.
Given the results of our review, future research should focus on:
high quality studies on primary care epidemiology, and on reasons for encounter, using data referring to episodes of care, and with a longitudinal perspective.
clinical studies, dealing with common, everyday complaints and illnesses.
observational and interventional research on diagnostic reasoning in (low-prevalence) primary care settings. This would start from complaints and symptoms and deal with uncertainly and complexity, using step-wise strategies, including watchful waiting, assumptive symptomatic treatment, and focussing on low technology strategies.
pragmatic RCTs using non-selected general practice patients on treatments, which are relevant for primary care, including comparative effectiveness studies on established treatments, on dosages, or studies on when to stop treatment.
research on primary care patients with multi-morbidity, or simultaneously experiencing acute and chronic diseases. This includes research into the attitudes of patients and physicians on how to set, rank and agree on priorities or specific wishes, and to revise this ranking over time.
large observational and interventional studies, which focus on relevant health outcomes, less common health problems, or safety issues, i.e. unwanted effects of treatment.
longitudinal research, both observational and interventional, with extended follow-up periods.
instrumental research on measurement tools and outcomes specific for general practice.
mixed method studies exploring and subsequently measuring patient perspectives and preferences, and changes in health over time.
observational and interventional research on the impact and sustainability of educational interventions.
Final comments
The research domain related to problem solving skills specific for GP/FM contains many different research topics, including ‘classical’ clinical research. The authors’ consensus included the decision to treat quality management and guidelines as part of this core competency: quality management was perceived as a skill and guidelines as a tool to deal with the diversity of problems and uncertainty specific to general practice. However, quality management and its tools are also part of primary care management, resulting in some overlap with the respective part (Citation4). Similarly, shared decision making was considered a specific skill, though it is also an essential part of person-centred care (Citation5).
Identifying the specific contribution of GP/FM to clinical research on specific diseases, but also identifying studies relevant to primary care performed by other disciplines, is difficult due to labelling problems. Currently, though research can be retrieved on almost any disease, it is often restricted to selected patient populations, narrowly defined strategies, technical approaches or new drugs, and characterised by a lack of studies of questions relevant to general practitioners, comparative trials in particular. Nevertheless, major successes of GP/FM research concern care for acute and chronic disorders, and issues of quality management in GP/FM.
GPs and their patients need the results of pragmatic studies in primary care settings, accounting for the specific properties named above. Research on these issues needs specific methods (e.g. management of a large number of trial sites and research networks, definition of adequate control groups, and specific statistical methods), and sufficient follow-up to inform on the sustainability of treatment or intervention effects.
Full text versions of the research agenda
Electronic versions (pdf) in English, Spanish or Portuguese are available from: http://www.egprn.org. Paper versions can be requested from the Coordinating Centre of EGPRN, Mrs Hanny Prick. E-mail: [email protected]
Supplementary Material
Download PDF (49.2 KB)Acknowledgments
The authors acknowledge the support and contribution of many organizations and persons. The full text can be read in the first article of this series (Citation3).
Declaration of interest: The authors report having no conflict of interest. The authors alone are responsible for the content and writing of the paper. All authors are members of EGPRN and active in its committees. Additionally, EHP was member of the Wonca Europe Executive Board from 2007–2010, and Mehmet Ungan since 2010. The Research Agenda was supported solely by EGPRN and grants from Wonca Europe.
References
- Hummers Pradier E, Beyer M, Chevallier P, Eilat-Tsanani S, Lionis C, Peremans L, . Research agenda for general practice/family medicine and primary health care in Europe. Maastricht: European General Practice Research Network EGPRN; 2009.
- Wonca. Europe definition of Family Medicine. 2005. http://www.woncaeurope.org/Web%20documents/European%20Definition%20of%20family%20medicine/Definition%202nd%20ed%202005.pdf (accessed 21 June 2010).
- Hummers-Pradier E, Beyer M, Chevallier P, Eilat-Tsanani S, Lionis C, Peremans L, . The research agenda for general practice/family medicine and primary health care in Europe. Part 1. Background and methodology. Eur J Gen Pract. 2009; 15:243–50.
- Hummers-Pradier E, Beyer M, Chevallier P, Eilat-Tsanani S, Lionis C, Peremans L, . Series: The research agenda for general practice/family medicine and primary health care in Europe. Part 2. Results: Primary care management and community orientation. Eur J Gen Pract. 2010;16:42–50.
- Van Royen P, Beyer M, Chevallier P, Eilat-Tsanani S, Lionis C, Peremans L, . Series. The research agenda for general practice/family medicine and primary health care in Europe. Part 3. Results: Person centred care, comprehensive and holistic approach. Eur J Gen Pract. 2010;16:113–9.
- Kruschinski C, Lange M, Lionis C, van Weel C, Hummers-Pradier E; EGPRN. Themes and methods of research presented at European General Practice Research Network conferences. Fam Pract. 2010;27:459–67.
- Cochrane Library. http://www.thecochranelibrary.com (accessed 21 June 2010).
- Scottish Intercollegiate Guidelines Network. SIGN 50: A guideline developer's handbook. Edinburgh 2008. http://www.sign.ac.uk/guidelines/fulltext/50/index.html (accessed 21 June 2010).
- Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Allonso-Coello P, . GRADE working group. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. Br Med J. 2008;336:924–6.