Abstract
Objective: Vitamin D deficiency is often unidentified, although treatment is simple and inexpensive. Our objective was to estimate the influence of concealing clothes and other risk factors for vitamin D deficiency in women aged 20 to 50 years consulting general practitioners. Methods: 13 GPs in the Rhone Alps area planned to recruit 300 women (100 veiled and 200 non-veiled) from January to March 2008. Serum 25(OH)D and PTH were measured in one single laboratory (Biomnis®) by a radio-immunoassay method. A survey was administered about dietary habits, sun exposure, and quality of life. Results: Among 247 women enrolled, 196 were analysed: 61 wearing concealing clothes (31.2%) and 135 without (68.8%). As expected, 25(OH)D serum level was significantly lower in covered women (20.1 versus 38.9 nmol/l P < 0.001). Of women who did not wear concealing clothing, 39.3% had severe hypovitaminosis D (25(OH)D concentration < 30 nmol/l). Women wearing concealing clothes had more often other known risk factors such as dark skin (P < 0.001), less sunlight exposure, or a higher Body Mass Index (P = 0.009). Besides concealing clothing (OR 6.37, 95% CI: 1.35–30.09), multivariate analyses revealed two independent risk factors for vitamin D deficiency: no full-body sun exposure (OR: 3.06, 95% CI: 1.18–7.94) and no outdoor sports (OR: 2.81, 95% CI: 1.11–7.12) for threshold 52 nmol/l.
Conclusion: Young women consulting their GP had hypovitaminosis D more often than expected. Besides concealing clothing, absence of full body sun exposure during summer and of outdoor sports practice could suggest a possible vitamin D deficiency.
Introduction
As 80% to 100% of vitamin D is synthesized by the skin under sunlight exposure, insufficient exposure is expected to increase the risk of hypovitaminosis D. This condition is frequent in countries where concealing clothing is typically worn (Citation1–6). Several studies have found higher than expected rates of vitamin D deficiency and other risk factors for hypovitaminosis D in the general population of Western countries (Citation7–10). Actually, the ideal healthy blood level of 25-hydroxyvitamin D—25(OH)D— widely accepted, is above 75 nmol/l (30 ng/ml). These international recommendations enable a maximum result on bone tissue and contribute to the prevention of diseases like cancer (Citation11,Citation12).
In France, supplementation is recommended for babies, pregnant women, and elderly people. Other groups are not concerned (Citation13). Chapuy and colleagues found that 14% of French women aged 30–60 years, had vitamin D concentrations below 30 nmol/l, whereas in the Rhone Alps area only 9% of women had such low concentrations (Citation14). In 2006, in the same area, 82.5% of a cohort of 96 veiled women, who probably were not or under represented in Chapuy's study, were found with a vitamin D deep deficiency (25(OH)D < 30 nmol/l) and 72.6% were symptomatic (pain and asthenia) (Citation15). In 2006, a large sample of people has been questioned about their eating habits; in this sample only 4.4% had a vitamin D deficiency (Citation16). This large discrepancy in vitamin D status depending on the population studied, led us to explore in more details vitamin D status in patients consulting GP whatever reason.
The objective of this study was to identify the effects of concealing clothing and other risk factors for vitamin D deficiency in women aged 20–50 years who consulted general practitioners (GPs) and its consequences.
Methods
Study design and participants
This cross-sectional study was carried out by 13 GPs working in the Rhone Alps area at 45°N latitude. Eligible subjects were women (19–49 years old) who consulted their GP for any reason. The GPs invited all women who wore concealing clothing and the first woman without such clothing from each day's consultations during January through March 2008. Clothing covering the arms, legs, and head was considered to be concealing. The exclusion criteria were pregnancy, breast-feeding, malabsorption syndrome, hepatic, renal, or cutaneous diseases, and medication known to affect vitamin D metabolism.
Potential participants were informed of the study's goals and methods, which included free vitamin D and parathyroid hormone (PTH) tests. The women, who verbally agreed to participate in the study, provided a blood sample. After an interview and physical examination, the GPs collected data with a questionnaire. The study was conducted in accordance with the CNIL guidelines for medical research, the MR001 norm.
Measurements
The subjects were examined for body mass index (BMI), phototype, and clinical symptoms of hypovitaminosis D. Socio-demographic status and risk factors such as number of pregnancies, breast-feeding, use of concealing clothing, sports activities, dietary intake of vitamin D, and amount of sunlight exposure were recorded. Asthenia and musculoskeletal pain were measured with a visual analogue scale. Sunlight exposure was measured with a previously validated questionnaire (Citation17,Citation18). Quality of life was measured with the Short Form health survey (SF12) (Citation19). Mean scores for each scale were determined. The population was divided into age groups.
All blood samples were analysed in the same laboratory (Biomnis, Lyon, France) using DiaSorin® kits. Serum 25(OH)D and PTH concentrations were measured by radio-immunoassay, which detects 25(OH)D2 and 25(OH)D3, to assess potential skeletal consequences. Calcium, phosphorus, and alkaline phosphatase (PAL) were not measured because studies have shown no correlation between these levels and low 25(OH)D or high PTH levels (Citation20).
Vitamin D deficiency was defined as a 25(OH)D concentration <75 nmol/l, with the following thresholds: mild (<50 nmol/l), medium (<30 nmol/l), and severe (<10 nmol/l) deficiency. PTH concentrations of 17–73 ng/l were considered normal.
Statistical analysis
All data were analysed using SPSS software (version 12.0; SPSS Inc., Chicago, IL, USA). Statistical significance was set at a 95% level. Group comparisons were performed with Student's t-test for independent samples (interval variables) and χ² tests (categorical variables). The Gaussian distribution of the variables was verified. We first tested the relationship between the potential risk factors and the existence of hypovitaminosis D with univariate analyses. Variables exhibiting significant contributions in the univariate model (P < 0.05) were retained in the multiple logistic regression models, where hypovitaminosis D was the dependant variable. Two regression models were performed with 25(OH)D thresholds <52 nmol/l and <30 nmol/l.
Results
Socio-demographic characteristics
A total of 247 women completed the questionnaire, while 51 did not supply a blood sample and thus were excluded. The final study sample included 196 women, of whom 61 (31.2%) wore concealing clothing and 135 (68.8%) did not. The women who wore concealing clothing on average were younger (33.4 ± 7.7 years versus 36.9 ± 8.6 years; P = 0.008), more frequently unemployed (36.1% versus 17.3%; P < 0.001), and more economically disadvantaged (42.6% versus 14.9%; P < 0.001) ().
Table I. Characteristics of the women included in this study.
Serum 25(OH)D
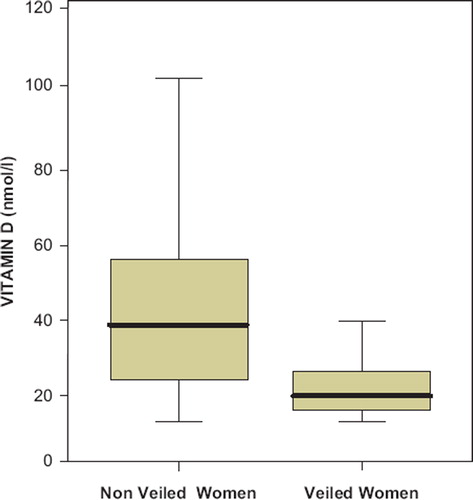
The study population had very low 25(OH)D serum levels (mean = 33.0 nmol/l). Women who wore concealing clothing differed statistically significant from those who did not, for 25(OH)D serum level (mean = 20.1 nmol/l ± 13.2 versus 38.9 nmol/l ± 21.6; P < 0.001; , ).
Table II. Prevalence of vitamin D deficiency based at different thresholds.
Risk factors
shows the risk factors for vitamin D deficiency among women who did or did not wear concealing clothing, respectively. Women who dressed in concealing clothing more frequently had dark skin (Fitzpatrick's phototypes IIIB, IV, or V; P < 0.001), higher mean BMI (BMI > 25; P = 0.009), and less sunlight exposure for each body component. Women who did not wear concealing clothing exposed large parts of their bodies more often, for longer periods (>1 week) in summer, and more frequently in the middle of the day (12:00–16:00). More than 50% of women without concealing clothing were exposed to sunlight at the seaside or in the mountains.
Table III. Risk factors for vitamin D deficiency in women with and without concealing clothing.
We found no difference between groups in vitamin D intake, which was lower than recommended for all women. Few women (10.7% n = 20) in either group used dietary supplements.
Determinants of vitamin D deficiency
shows the results of the univariate regression analyses.
Table IV. Odds ratios of risk factors for two thresholds of vitamin D deficiency (univariable logistic regression).
A multivariate analysis including all significant risk factors was performed. Independent risk factors for the 25(OH)D threshold of 30 nmol/l were ‘concealing clothing’ (odds ratio (OR): 5.6, 95% CI: 2.3–13.6) and ‘no full-body sun exposure’ (OR: 4.5, 95% CI: 2.0–10.2).
Independent risk factors for the threshold 52nmol/l were ‘concealing clothing’ (OR: 6.37, 95% CI: 1.35–30.09), ‘no full-body sun exposure’ (OR: 3.06, 95% CI 1.18–7.94) and ‘no outdoor sports’ (OR: 2.81, 95% CI: 1.11–7.12).
Parathyroid hormone
The mean PTH concentration was higher in vitamin D–deficient women (25(OH)D < 30 nmol/l, 67.2 ± 28.8 versus 25(OH)D > 30 nmol/l, 46.1 ± 18.1; P < 0.001). 40% of vitamin D-deficient women presented biological signs of hyperparathyroidism (P < 0.001).
Clinical consequences
Of all women studied, 53% (n = 103) had asthenia and 45% (n = 88) had musculoskeletal pain. Women wearing concealing clothing complained more frequently of fatigue than those who did not (65% versus 47%; P = 0.023), but this was not significantly associated with the severity of vitamin D deficiency. Fatigue affected 58% of women below the 30 nmol/l threshold and 47% of women above the threshold (P = 0.145). More women wearing concealing clothing reported pain (59% versus 38.5%; P = 0.008), which differed significantly with the severity of deficiency (25(OH)D < 30 nmol/l, 53% versus 25(OH)D > 30 nmol/l, 35%; P = 0.011).
Quality of life
The SF12 results were not entirely interpretable because the number of patients in each subgroup was too small. Thus, we only interpreted the mean physical and mental component scores (PCS, MCS) and the combined average. The PCS was significantly higher for women who did not wear concealing clothing, indicating better physical health (49.7, 95% CI: 48.2–51.4, versus 44.9, 95% CI: 42.5–47.3; P = 0.001), and was associated with the severity of vitamin D deficiency. Women with 25(OH)D < 30 nmol/l had lower PCS than women with 25(OH)D > 30 nmol/l (46.5, 95% CI: 44.6–48.3 versus 50.2, 95% CI: 48.2–52.3; P = 0.006). The mean MCS did not differ significantly between groups (43.0, 95% CI: 40.5–45.5 versus 42.9, 95% CI: 41.1–44.8; P = 0.9).
None of the SF12 scales differed significantly between groups (i.e. women with vs. without concealing clothing, and vitamin D-deficient vs. non-deficient women), except physical functioning (PF). PF scores were lower among women wearing concealing clothing as compared with those who did not (45.7 versus 50.4; P = 0.002), and among vitamin D-deficient women as compared to non-deficient women (47.5 versus 50.6; P = 0.025).
Discussion
In this study among 196 women, 61 (31.2%) were wearing concealing clothing. Women dressed in concealing clothing on average were younger, more frequently unemployed, and more economically disadvantaged. Serum levels of vitamin D—25(OH)D—were low (mean 33.0 nmol/l); for women wearing concealing clothing this was 20.1 nmol/l. For all women, vitamin D intake was lower than recommended. Women who dressed in concealing clothing more frequently had dark skin, higher mean BMI and less sunlight exposure for each body component. A multivariate analysis including all significant risk factors identified ‘concealing clothing’ (OR: 5.6) and ‘no full-body sun exposure’ (OR: 4.5) as independent risk factors for the 25(OH)D threshold of 30 nmol/l. For the 25(OH)D threshold of 52nmol/l these were ‘concealing clothing’ (OR: 6.37), ‘no full-body sun exposure’ (OR: 3.06) and ‘no outdoor sports’ (OR: 2.81). 40% of the vitamin D-deficient women presented biological signs of hyperparathyroidism. Women wearing concealing clothing complained more frequently of fatigue and more frequently reported pain, which was associated with vitamin D deficiency. As for the SF12, the physical components score (PCS) was significantly higher for women who did not wear concealing clothing, indicating better physical health and was inversely associated with the severity of vitamin D deficiency. The mean mental components score (MCS) did not differ significantly between groups.
Strengths and limitations
These results were obtained from a non-randomized sample of family physicians; selection bias may thus be present. In spite of regular phone calls to remind them, it is possible that GPs did not include every day, because they are busy working in winter.
Women who did not have a blood sample taken were interviewed on their reasons for refusal, which primarily was lack of time or interest. They did not significantly differ in age, number of children, or professional occupation from the study participants, but had significantly higher BMI.
Low Vitamin D status
Our multivariate analysis showed that wearing concealing clothing is an independent risk factor for vitamin D deficiency. Meddeb et al. found that 70.5% of women wearing concealing clothing in Tunisia had hypovitaminosis D, in contrast to 48.9% of women without such clothing, but did not establish concealing clothing as an independent risk factor (Citation21). Gannage-Yared et al. found pronounced vitamin D deficiency in Lebanon, 62% of women wearing concealing clothing had 25(OH)D concentrations <12.5 nmol/l (versus 23.5% of women without concealing clothing), and concealing clothing was an independent risk factor (Citation2). Mishal et al. found that 83.3% of women wearing concealing clothing in winter had 25(OH)D concentrations <30 nmol/l in Jordan (Citation3). El-Sonbaty and Guzel obtained similar results in Kuwait and Turkey (Citation4,Citation5).
We found that 39.3% of women without concealing clothing had 25(OH)D concentrations <30 nmol/l, which differs markedly from the 9% obtained in the same region by Chapuy et al. (Citation14). Our results are similar to those of other studies. In the United States, the third National Health and Nutrition Examination Survey (NHANES III; 1988–1994) found that 28.8% of 2418 women aged 19 to 59 years had serum 25(OH)D concentrations <37.5 nmol/l in winter at 32°N latitude. Furthermore, Looker et al. found that 25(OH)D concentrations were 5 to 20 nmol/lower in NHANES 2000–2004 than in NHANES III. Overweight, sun protection and lower milk intake appeared as possible explanations (Citation22,Citation23). Likewise these reasons could explain a part of the difference with the results of Chapuy. In the UK, Hyppönen et al. found a high prevalence of vitamin D deficiency in winter among 45-year-olds (serum 25(OH)D concentration <25 nmol/l, 15.5%; <40 nmol/l, 46.6%)(Citation7). Carnevale et al. found that 27.6% of women in southern Italy were vitamin D deficient (<30 nmol/l) (Citation24).
Known risk factors
Despite our small sample size, we demonstrated that overweight or obesity and not participating in outdoor sports were risk factors for hypovitaminosis D. These findings are consistent with those of other studies (Citation7,Citation23,Citation25).
Sun exposure was the second most important risk factor in this study. Women who never exposed their full body (e.g. at the beach or outdoor swimming pool) during the previous summer were at higher risk of hypovitaminosis D. Gilchrest et al. showed that only 2–8 min of exposure were sufficient for vitamin D photosynthesis in mountain or seaside contexts from June to September between 12:00 and 16:00, if a large area of skin was exposed (Citation26). Holick et al. recommended 5–15 min of exposure between 10:00 and 15:00 during spring, summer, and autumn, followed by the application of sunscreen with an SPF below 15, to achieve a slight pinkness of the skin (Citation27).
Physical and psychological well-being
Women wearing concealing clothing were significantly more tired and reported pain more frequently. Previous European studies have found that most young people with non-specific musculoskeletal pain are not screened for hypovitaminosis D, and that 30 to 59 months may elapse before the deficiency is diagnosed (Citation28–30). Women wearing concealing clothing may have a long-term deficiency that does not improve in summer and consequently worsens over time. Another possible explanation is the erroneous diagnosis of anxiety or depression to explain the functional complaints (Citation29). The SF12 questionnaire used in this study distinguishes complaints linked to somatic pathology from those linked to depression. Our study found no difference in depression scores (MCS) between groups divided by clothing or by serum 25(OH)D concentration thresholds. In contrast, women wearing concealing clothing and vitamin D-deficient women had worse physical health (PCS) and physical functioning (PF) scores. Therefore, vitamin D deficiency is associated with lower physical quality of life, but not with depression. This finding is similar to that of a retrospective study conducted in a chronic pain centre (Citation31).
Women wearing concealing clothing and vitamin D-deficient women had significantly higher mean PTH serum values than women without concealing clothing or deficiency, as found in other studies (Citation2–3,Citation10,Citation21). These results justify treatment of the deficiency before complications arise (Citation12,Citation32).
Conclusion
This cross-sectional study showed that many women in our region in France had hypovitaminosis D in winter. Concealing clothing was a strong risk factor for vitamin D deficiency, as were the lack of full-body sun exposure and non-participation in outdoor sports. We also found physical quality of life and physical functioning to be significantly lower in vitamin D-deficient women. In France, like in other countries, vitamin D deficiency is under-recognised. Our results provide information on easily assessed risk factors that may help GPs identifying women at high risk of hypovitaminosis D. They could be particularly attentive to women who wear concealing clothing, never expose their full body or only do so in the city, with a dark phototype, do not practise outdoor sports, and possibly do not have a job, or are socially disadvantaged.
Acknowledgments
The authors are grateful to our general practitioner colleagues who recruited patients and facilitated this study, DiaSorin® and Biomnis® laboratories for providing all the testing kit free of charge, and Mrs Dujet Isabelle for reading over the manuscript.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Allali F, El Aichaoui S, Khazani H, Benyahia B, Saoud B, El Kabbaj S, . High prevalence of hypovitaminosis D in Morocco: relationship to lifestyle, physical performance, bone markers, and bone mineral density. Semin Arthritis Rheum. 2009;38:444–51.
- Gannage-Yared MH, Chemali R, Yaacoub N, Halaby G. Hypovitaminosis D in a sunny country: Relation to lifestyle and bone markers. J Bone Miner Res. 2000;15: 1856–62.
- Mishal AA. Effects of different dress styles on vitamin D levels in healthy young Jordanian women. Osteoporos Int. 2001;12:931–5.
- el-Sonbaty MR, Abdul-Ghaffar NU. Vitamin D deficiency in veiled Kuwaiti women. Eur J Clin Nutr. 1996;50:315–8.
- Guzel R, Kozanoglu E, Guler-Uysal F, Soyupak S, Sarpel T. Vitamin D status and bone mineral density of veiled and unveiled Turkish women. J Womens Health Gend Based Med. 2001;10:765–70.
- Hatun S, Islam O, Cizmecioglu F, Kara B, Babaoglu K, Berk F, . Subclinical vitamin D deficiency is increased in adolescent girls who wear concealing clothing. J Nutr. 2005;135:218–22.
- Hypponen E, Power C. Hypovitaminosis D in British adults at age 45 y: Nationwide cohort study of dietary and lifestyle predictors. Am J Clin Nutr. 2007;85:860–8.
- MacFarlane GD, Sackrison JL, Jr, Body JJ, Ersfeld DL, Fenske JS, Miller AB. Hypovitaminosis D in a normal, apparently healthy urban European population. J Steroid Biochem Mol Biol. 2004;89-90:621–2.
- Gonzalez Solanellas M, Romagosa Perez-Portabella A, Zabaleta del Olmo E, Gudina Escudero N, Pozo Diaz C, Moreno Feliu R, . Vitamin D deficiency in women of reproductive age. Aten Primaria. 2008;40:393–9.
- Lamberg-Allardt CJ, Outila TA, Karkkainen MU, Rita HJ, Valsta LM. Vitamin D deficiency and bone health in healthy adults in Finland: Could this be a concern in other parts of Europe? J Bone Miner Res. 2001;16:2066–73.
- Holick MF, Chen TC. Vitamin D deficiency: A worldwide problem with health consequences. Am J Clin Nutr. 2008;87: 1080S–6S.
- Souberbielle JC, Body JJ, Lappe JM, Plebani M, Shoenfeld Y, Wang TJ, . Vitamin D and musculoskeletal health, cardiovascular disease, autoimmunity and cancer: Recommendations for clinical practice. Autoimmun Rev. 2010;9:709–15.
- INPES. PNNS 3. Available at: http://www.mangerbouger.fr (accessed 2010).
- Chapuy MC, Preziosi P, Maamer M, Arnaud S, Galan P, Hercberg S, . Prevalence of vitamin D insufficiency in an adult normal population. Osteoporos Int. 1997;7:439–43.
- Belaid S, Martin A, Schott AM, Laville M, Le Goaziou MF. Hypovitaminosis D among 18-to-49-years-old women wearing concealing clothes, an ignored reality in general practice. Presse Med. 2008;37:201–6.
- Étude nationale nutrition santé (ENNS, 2006). Situation nutritionnelle en France en 2006 selon les indicateurs d'objectif et les repères du Programme national nutrition santé (PNNS). Institut de veille sanitaire, Université de Paris 13, Conservatoire national des arts et métiers; 2007 74.
- Garabedian M, Menn S, Nguyen TM, Ruiz JC, Callens A, Uhlrich J. Prevention of vitamin D deficiency in the child and adolescent. I. Proposal and arguments for use of a decision tree. Arch Pediatr. 1999;6:990–1000.
- Garabedian M, Menn S, Walrant-Debray O, Teinturier C, Delaveyne R, Roden A. Prevention of child and adolescent vitamin D deficiency. II. Validation of a decision-making abacus based on sun exposure and vitamin D intakes. Arch Pediatr. 2005;12:410–9.
- Gandek B, Ware JE, Aaronson NK, Apolone G, Bjorner JB, Brazier JE, . Cross-validation of item selection and scoring for the SF-12 Health Survey in nine countries: results from the IQOLA Project. International Quality of Life Assessment. J Clin Epidemiol. 1998;51:1171–8.
- Smith GR, Collinson PO, Kiely PD. Diagnosing hypovitaminosis D: Serum measurements of calcium, phosphate, and alkaline phosphatase are unreliable, even in the presence of secondary hyperparathyroidism. J Rheumatol. 2005;32:684–9.
- Meddeb N, Sahli H, Chahed M, Abdelmoula J, Feki M, Salah H, . Vitamin D deficiency in Tunisia. Osteoporos Int. 2005;16:180–3.
- Looker AC, Dawson-Hughes B, Calvo MS, Gunter EW, Sahyoun NR. Serum 25-hydroxyvitamin D status of adolescents and adults in two seasonal subpopulations from NHANES III. Bone 2002;30:771–7.
- Looker AC, Pfeiffer CM, Lacher DA, Schleicher RL, Picciano MF, Yetley EA. Serum 25-hydroxyvitamin D status of the US population: 1988–1994 compared with 2000–2004. Am J Clin Nutr. 2008;88:1519–27.
- Carnevale V, Modoni S, Pileri M, Di Giorgio A, Chiodini I, Minisola S, . Longitudinal evaluation of vitamin D status in healthy subjects from southern Italy: seasonal and gender differences. Osteoporos Int. 2001;12:1026–30.
- Florez H, Martinez R, Chacra W, Strickman-Stein N, Levis S. Outdoor exercise reduces the risk of hypovitaminosis D in the obese. J Steroid Biochem Mol Biol. 2007;103:679–81.
- Gilchrest BA. Sun exposure and vitamin D sufficiency. Am J Clin Nutr. 2008;88:570S–7S.
- Holick MF. Sunlight and vitamin D for bone health and prevention of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr. 2004;80:1678S–88S.
- Plotnikoff GA, Quigley JM. Prevalence of severe hypovitaminosis D in patients with persistent, nonspecific musculoskeletal pain. Mayo Clin Proc. 2003;78:1463–70.
- de Torrente de la Jara G, Pecoud A, Favrat B. Female asylum seekers with musculoskeletal pain: The importance of diagnosis and treatment of hypovitaminosis D. BMC Fam Pract. 2006;7:4.
- Nellen JF, Smulders YM, Jos Frissen PH, Slaats EH, Silberbusch J. Hypovitaminosis D in immigrant women: Slow to be diagnosed. Br Med J. 1996;312:570–2.
- Turner MK, Hooten WM, Schmidt JE, Kerkvliet JL, Townsend CO, Bruce BK. Prevalence and clinical correlates of vitamin D inadequacy among patients with chronic pain. Pain Med. 2008;9:979–84.
- Bischoff-Ferrari H. Vitamin D: What is an adequate vitamin D level and how much supplementation is necessary? Best Pract Res Clin Rheumatol. 2009;23:789–95.