Abstract
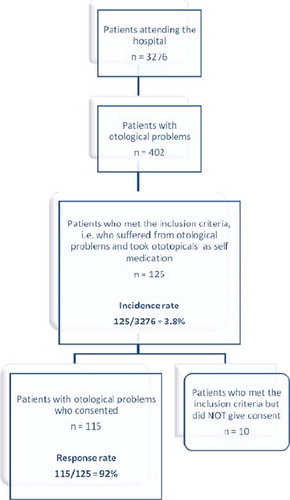
Background: Ototopical self-medication is a common practice in Nigeria. Objective: The aim of the study was to establish the proportion of patients with otological problems that practice ototopical self-medication. Methods: A 12-week cross-sectional study of all the new patients attending the general outpatient (also called family medicine (FM)) and ear, nose and throat (ENT) departments of a Nigerian specialist hospital was carried out. A semi-structured questionnaire was used to obtain information on bio data, practice of ototopical self medication among new patients with otological problems, the drugs used and the reasons for engaging in the practice. The results were analysed using SPSS version 11 and presented in Tables. Results: Out of 3276 patients that visited the hospital during the study period, 402 had otological problems. Of these, 125 (31%) used ototopical self-medication, giving a hospital incidence of 3.8%. 115 (92%) patients consented to fill in the questionnaire on the self-use of ototopical agents. Otalgia was the most common indication (27%) for ototopical self-medication. Gentamycin and Chloramphenicol topical agents were the most commonly used by the study participants. A total of 39 participants (34%) reported to have used non-prescribed self-medication because it was time saving. In 69 of the participants (60%), the drugs were self recommended while chemists and nurses recommended their use in 23 (20%) and 22 (19%) participants, respectively.
Conclusion: In Nigeria, there is a need for public enlightenment and health education about the possible drawbacks of this practice.
Background
In most societies, a person suffering from physical discomfort or emotional distress has several ways of helping himself or seeking help from others (Citation1). In developing countries, most illnesses are treated by self-medication (Citation2). Self-medication is a common practice, which is defined as ‘the use of drugs by oneself without clinical evaluation by a trained medical professional’ (Citation3). This could result in a missed diagnosis and a delay in getting the appropriate treatment.
In Nigeria, it is a common practice and it not surprising that ototopical drugs are also being abused. The reasons for this practice include the belief that visiting hospitals is a time-wasting venture; drugs are being taken on advice of friends and previous experience with the medications. Indeed, in developing countries like Nigeria access to health care is not uniformly distributed and mainly concentrated in the urban centres. Hence, some patients might have to travel for hundreds of kilometres to access care. Most ototopical agents are widely available for purchase without doctor's prescription over the counter. The erroneous belief that ear ailments are minor contributes to this problem (Citation4). Self-medication has also been found to contribute to increased health care costs, untold adverse drug effects, possible antimicrobial resistance and some increased morbidity among the population (Citation5,Citation6). Apart from the problem of poor outcomes and possible worsening morbidity, there are also economic and safety issues associated with self-medication. A debate on the issue of ototoxicity of eardrops is started and still ongoing (Citation7–10).
The aim of this study was to estimate the incidence of ototopical self-medication, conditions and reason for its use, patient's information sources, and type of drugs used.
Methods
Design and setting
This was a twelve-week descriptive study of all new patients attending the general outpatient (also called family medicine, FM) and ear, nose and throat (ENT) departments of the State Specialist Hospital, located in Lokoja, North-central Nigeria. It is an 80-bed tertiary-care health facility, which also offers primary and secondary care to about four million people both within and outside the state. The centre's involvement in primary and secondary care is because the institutions responsible for both levels of health care in the state in question do not have the required training, personnel and equipments to care for these patients.
The family medicine (FM) department is responsible for the initial screening of patients attending the hospital for the first time apart from emergency cases. Patients are then referred to other specialists when needed.
Study population
All new patients with otological problems attending the ENT and family medicine clinics, who have practiced self-medication with ototopical agents, were asked to participate in the study. Informed consent was obtained from each participant before being enrolled into the study. Patients that did not consent to the study and old patients of the ENT clinic on follow-up visits were excluded from the study.
Measurements
The total number of patients seen in the hospital during the study period was noted to enable the calculation of the hospital incidence rate. One of the authors and two trained assistants interviewed all consenting patients, using a semi-structured questionnaire developed for this study (Appendix A). It was based on modification of a questionnaire used for another local self-medication study (Citation11). Information obtained included: bio-data, practice of otological self-medication among, drugs used, and reasons for engaging in the practice.
Analysis
Data obtained was entered using SPSS version 11.0 statistical software and analysed descriptively.
Study ethics
The research ethics committee of the Kogi State Specialist Hospital, Lokoja, Nigeria, approved the study.
Results
Patient characteristics
Out of 3276 patients, that visited the hospital during the study period, 402 patients had otological complaints, and 125 used ototopical self-medication. The age ranged from 16–78 years. There were 72 males (57.4%) and 53 females (42.6%). Sixty-two (49.6%) had secondary school (post elementary) education, 32 (25.2%) had at least primary or elementary education, 30 (24.3%) had tertiary level (polytechnic/university) education and only 1 (0.9%) had no formal education. Forty-seven (37.5%) of the participants were civil servants, 31 (25.1%) were students, 25 (20.2%) were traders, 12 (10%) were artisans and 9 (7.2%) were pensioners.
Incidence of ototopical self medication
The hospital incidence of ototopical self-medication was 3.8% (125/3276) over a period of 12 weeks. Thirty-one% of all patients who consulted with otological problems (125/402) used self-medicated ototopical medication.
Results of the questionnaire
In , the ototopicals that were commonly used are given, as well as conditions and motives for their use. Furthermore, patients’ sources of information about ototopical drugs are presented.
Table I. Results of the questionnaire on ototopical self-medication (n = 115).
In 85 cases (73.9%), the ototopical medications contained antibiotics. Otalgia was the major reason for taking these medications (61.7%). Most mentioned motives for taking ototopical self-medication were ‘time saving’ (33.9%) and ‘costs’ (31.3%).
Most participants (60.9%), who admitted to using ototopical drugs, did not know it was an act of drug misuse or self-medication, while others went ahead despite being aware. In answering the question whether self-medication with these drugs was beneficial to them, 53 (46.1%) of the participants did not think so, while only 25 (21.7%) believed the use had a positive impact. The remaining 37 (32.2%) were not actually sure of the benefits of self-medication with these agents.
Discussion
Incidence
The incidence of ototopical drug use among visitors of our hospital was 3.8%. This finding is in contrast with results from self-medication studies in ophthalmology and other fields of medicine with documented higher rate of self-medication, both from Nigeria and other parts of the world (Citation11–13). The authors are not aware of any local self-medication study on ototopical drugs. Most studies are related to antibiotic self-medication, especially with oral antibiotic preparations in ENT practice (Citation14,Citation15). In our study ototopic self medication is more common among males than females; however, previous studies on self-medication in general do not follow any particular trend as per gender (Citation16,Citation17).
Indications for self-use
Otalgia was the most common indication for the use of ototopical agents among the respondents. This result is not strange as people usually respond quickly to pain trying to find ways to relieve it. Neither was it surprising that the use of ototopicals was not beneficial in most participants; this is because application of ear drops either steroid or antibiotic based over pus is usually ineffective. The recommendation for treatment of suppurative otitis media is aural toileting with application of topical eardrops (Citation18). Awareness about inappropriate self-medication was low among the participants as more than half of them did not consider the use of these non-prescribed eardrops an act of drug misuse, hence the need for further health education of the populace.
Motives for self-use of ototopical drugs
The main motive for using ototopical self-medication among our participants was the time saving factor. This result confirms findings from other studies on self-medication (Citation5,Citation17). Most ototopical drugs are widely available as over the counter drugs (OTC), cheap and affordable, hence its propensity to misuse. This is a source of concern, and a clarion call for action by the government, and its regulatory authorities. Furthermore, most patients in our setting belief that waiting to consult a specialist is time consuming and an expensive venture. The minimum costs in Nigeria to access a specialist is about N 2000.00–N 2500.00 ($13–$17 US dollar) where over 60% of the people have less than $1 US dollar per day to spend (Citation19). One other reason why patients choose for self-medication is due to the lack of access to ENT specialists (Citation5). This can be understood from two angles: the few available specialists are usually concentrated in the urban centres where most of the tertiary health care facilities are sited. In view of the limited availability of ENT specialists, training of more medical doctors in family medicine will go a long way in solving the problem of manpower.
Strengths and limitations of the present study
The study explored a significant public health problem to which adequate attention is not being paid in Nigeria. The study gives baseline information upon which interventions to address this problem can be directed. One of the major limitations of the study is that being a self-reporting one, there is always a problem of recall accuracy, bias and unverifiable information.
Implications for clinical practice, education or research
This study shows that self-medication with ototopical agents is an important problem in the ENT and family medicine practice. It also shows the need to educate patients about the potential negative effects of self-medication. For policy makers and government agencies, it highlights the need for concerted efforts towards uncontrolled access to drugs in Nigeria.
Conclusion
The practice of ototopical self-medication is common among patients with otological complaints attending the ENT and family medicine clinics of our specialist hospital in Nigeria. There is a need for public enlightenment and health education of the populace about the possible drawbacks of this practice.
Supplementary material available online, at http://www.informahealthcare.com/doi/abs/10.3109/13814788.2011.565323.
Supplementary Material
Download PDF (31.7 KB)Acknowledgement
The authors are grateful to Dr Mohammed K, Dr Attah K, Dr Ibrahim E and other staffs of the Family Medicine and ENT Department of the Kogi State Specialist Hospital who also assisted in the data collection and interpretation. The authors are also grateful to Dr TO Odi for his constructive criticism.
Declaration of interest: The authors report no conflicts of interest. The authors alone are responsible for the writing and content of the paper.
References
- Helman C. Culture health and illness. An introduction for health professional 1st. Bristol B545 NUU.: John Writing and sons (Printing) Ltd, at the stone bridge press, Berkeley, California, USA; 1985. 42–53.
- Geissler PW, Nokes K, Prince RJ, Odhiambo RA, Aagaard-Hansen J, Ouma JH. Children and medicines: Self-treatment of common illnesses among Luo schoolchildren in western Kenya. Soc Sci Med. 2000;50:1771–83.
- Hamel MJ, Odhacha A, Roberts JM, Deming MS. Malarial control in Bungoma district Kenya: A survey of home treatment of children with fever, bed net use and attendance of antenatal clinics. Bulletin of World health organization 2001;79:1014–23.
- Ibrahim MI. Treating one's own ailment. World Health Forum 1996;17:409–10.
- Al-Bakri AG, Bustanji Y, Yousef AM. Community consumption of antibacterial drugs within the Jordanian population: Sources, patterns and appropriateness. Int J Antimicrob Agents 2005;26:389–95.
- Abasaeed A, Vlcek J, Abuelkhair M, Kubena A. Self-medication with antibiotics by the community of Abu Dhabi Emirate, United Arab Emirates. J Infect Dev Ctries. 2009;30;491–7.
- Coates H, Ear drops and ototoxicity Aust Prescr. 2008;31: 40–1.
- Natsch S, Mylanus EAM, Mulder JJS, Hekster YA. The use of ear drops in ENT department, Pharm World Sci. 1999; 21:266–9.
- Jackman A, Ward R, April M, Bent J. Topical antibiotic induced otomycosis. Int J Pediatr Otorhinolaryngol. 2005; 69:857–60.
- Raz R, Edelstein H, Grigoryan L, Haaijer-Ruskamp FM. Self-medication with antibiotics by a population in northern Israel. Isr Med Assoc J. 2005;7:722–5.
- Afolabi AO. Factors influencing the pattern of self-medication in an adult Nigerian population. Ann Afr Med. 2008;7: 120–7.
- Onajole AT, Bamgbala AO. Socio demographic characteristic of drug misuse in a polytechnic in Lagos, Nigeria. Nig J Health and Biomed Sciences 2004;31:40–3.
- Awad AI, Eltayeb IB and Capps PA. Self medication practices in Khartoum state, Sudan. Eur J Clin Pharmacol. 2006;62;317–24.
- Das BP, Sethi A, Rauniar GP, Sharma SK. Antimicrobial utilization pattern in out patient services of ENT department of tertiary care hospital of Eastern Nepal. Kathmandu Univ Med J. 2005;3:370–5.
- Raza SA, Denholm SW, Wong JC. An audit of the management of acute otitis externa in an ENT casualty clinic. J Laryngol Otol. 1995;109:130–3.
- Al-Azzam SI, Al-Husein BA, Alzoubi F, Masadeh MM, Al-Horani MS. Self-Medication with antibiotics in Jordanian population. Int J Occup Med Environ Health 2007;20: 373–80.
- Grigoryan L, Burgerhof JG, Degener JE, Deschepper R, Lundborg CS, Monnet DL, . Determinants of self-medication with antibiotics in Europe: The impact of beliefs, country wealth and the healthcare system. J Antimicrob Chemother. 2008;61:1172–9.
- Verhoeff M, Van der Veen EL, Rovers MM, Sanders EAM, Schilder AGM. Chronic suppurative otitis media: A review. Int J Pediatr Otorhinolaryngol. 2006;70:1–12.
- World Development Report 2010. Available at http://www.siteresouces.worldbank.org/INTWDR2010 (accessed 21 September 2010).