Abstract
Background: In medical education and practice, smartphone apps are increasingly becoming popular. In general practice, apps could play an important future role in supporting medical education and practice.
Objectives: To explore medical students’ perceptions regarding the potential of a general practice app for training and subsequent work as a physician.
Methods: Cross-sectional survey among Leipzig fourth-year medical students who were provided with an app prototype for a mandatory general practice course.
Results: Response rate was 99.3% (n = 305/307); 59.0% were female and mean age was 24.5 years. Students certified that the app had a higher potential than textbooks in both education (57.4% vs. 18.0%) and practice (47.1% vs. 22.8%). Students’ most desired possible app extensions when anticipating its use for subsequent work as a physician were looking up information for diagnostics, therapy and prediction (85.1%), access to electronic patient files (48.1%), communication and networking (44.3%), organization of medical training (42.9%) and online monitoring of patients (38.1%). Students experienced with medical smartphone apps were more interested in app extensions. Consideration to use the app to support the opening of their own practice was significantly associated with higher interest in accessing electronic patient files, networking with colleagues and telemedicine.
Conclusion: Fourth year medical students from Leipzig see a high potential in smartphone apps for education and practice and are interested in further using the technology after undergraduate education.
Key Messages
Fourth year medical students from Leipzig, Germany, were interested in using a general practice app during and after medical education.
The responding students anticipated using a future general practice app mainly for collaboration, access to knowledge and diagnostic purposes when working as physicians.
Introduction
Smartphones and related apps have found their way into the healthcare domain. The variety of available apps targeted at patients, doctors and students – with purposes such as personal health tracking, patient monitoring, decision support, diagnosis and measurement, patient education and communication and access to medical knowledge – reflects the spectrum of purposes for this technology in medicine.[Citation1–3] A key group of users who grew up with the smartphone are medical students and young healthcare professionals, with as many as 90% owning a smartphone and having medical smartphone apps installed on their devices.[Citation4,Citation5] With students believing that mobile technologies contribute to their medical education, it remains no surprise that institutions concerned with medical education and practice are beginning to unlock this potential.[Citation6–9]
Understanding the demands of target users plays an important role in providing content congruent with their needs.[Citation10] With 67.1% of previously surveyed students welcoming a general practice app supporting them during vocational training and 42.2% when opening their own practice, our previous research highlighted the potential of this technology to bridge the gap between medical education and practice.[Citation10] Additionally, our research on the adoption of a prototype of a general practice app showed students’ willingness to use it during education.[Citation11]
In the current study we aimed to explore students’ perceptions regarding the potential of a general practice app for training and subsequent work as a physician. We specifically wanted to understand students’ evaluation of the relative potential compared to textbooks. Particular attention was paid to the students’ interest in content that might be useful in daily practice. We wanted to gain a more refined understanding of students’ interests by employing group comparisons.
Methods
Sampling
In May 2014, we conducted a cross-sectional classroom survey among medical students at the end of their mandatory lecture series on general practice (8th semester of 12) at the Leipzig Medical Faculty. Previously, a web-based prototype of a smartphone app on general practice was provided to the participating students, who were encouraged to use it as an additional learning tool accompanying the lectures. Participation in the survey was voluntary and students were notified about its purpose.
Provided app prototype
A web-based prototype of a general practice app was developed based on a general practice textbook.[Citation12] It provided specialist texts, information on medicines, differential diagnostic algorithms, lecture notes, selected scientific articles available for download, and a multiple-choice mock examination. A screenshot of the prototype’s user interface can be found in the appendix of a previously published study.[Citation11]
Questionnaire
Questionnaire items were developed by an interdisciplinary research team (business, computer science, psychology and general practice background) based on prior experience, a paper on smartphone usage by doctors [Citation13] and interviews with experienced general practitioners (GPs) running medical practices. The original German questionnaire was reviewed by GPs prior to being piloted among a group of students to ensure understandability. Besides socio-demographic variables and career considerations, the data relevant to this publication addressed the perceived potential of the provided app compared to a textbook, its perceived potential for the subsequent work as a physician and students’ interest in several additional features that might be helpful in a physician’s daily practice.
Statistical analysis
The anonymized dataset was analysed with IBM SPSS Statistics 22 and Microsoft Excel for Windows. Frequencies were presented as valid percentages. Continuous variables were presented as mean ± standard deviation (SD). Chi-square tests were used to compare frequencies. To enable exploratory group comparisons based on the variables for perceived potential of an app compared to a textbook for medical education and for the profession of a doctor, respectively, these variables have been dichotomized. To explore differing preferences towards app features depending on the intention to work practice-based, we compared students who considered using a GP app for the support of opening their own practice (e.g. when closing insurances and completing registrations) with those who did not. Statistical significance was assumed for p < 0.05.
Results
Sample characteristics
The response rate was 99.3% (n = 305/307). The majority of the participants (59.0%; n = 180/305) were female and mean age was 24.5 ± 2.7 years (range 21–35, n = 297). When asked about their desired career choice, general practitioner was mentioned by 6.0% (n = 18/302) and specialist in another field by 43.4% (n = 131/302) of the respondents while 50.7% (n = 153/302) replied that they had not decided yet.
Nearly all participants stated that they had used the provided prototype (97.7% (n = 296/303)).[Citation11]
Perceived potential of the provided app
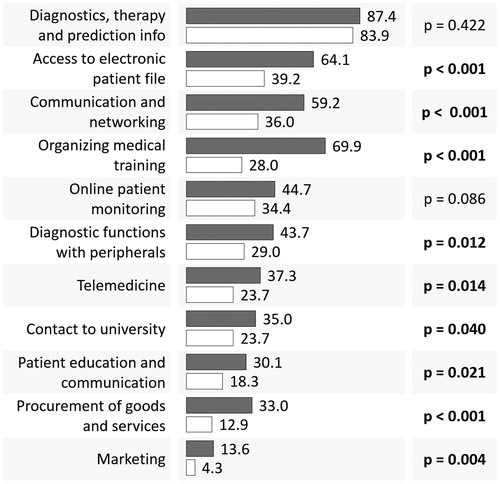
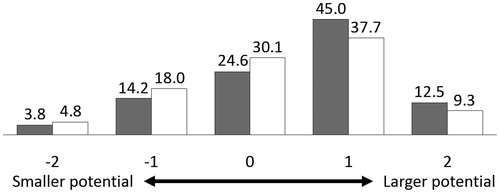
Students’ opinions about the potential of the supplied app compared to a textbook, both for their subsequent work as a doctor as well as for acquiring knowledge during undergraduate, postgraduate and continuing medical education are displayed in .
Figure 1. Students’ judgment of the potential of the supplied app prototype compared to a textbook for the medical profession (white bars) as well as for acquiring knowledge during undergraduate, postgraduate and continuing medical education (grey bars) (Values displayed in valid percent for n = 289).
Furthermore, 79.4% (n = 227/286) of the students mentioned that they were interested or very interested in further development of the provided general practice app. This corresponds to a mean of 4.1 ± 1.0 (n = 286) on a Likert scale extending from 1 (strongly disagree) to 5 (strongly agree).
Preferences regarding possible app extensions
Students’ selection of the purposes for which they would like to use a future app as a physician, given it would provide the necessary functionality, are summarized in .
Figure 2. Purposes for which students would like to use a future app as a doctor given that respective features are provided (displayed as valid %, n = 289).
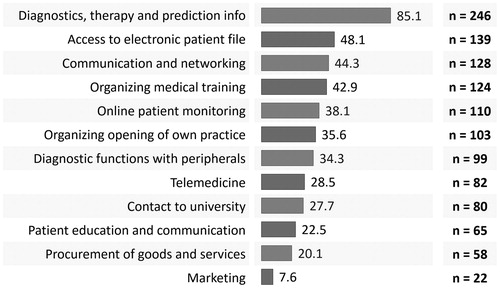
Out of 12 purposes to choose from, a mean of 4.3 ± 2.7 (n = 288) features was selected and 72.9% (n = 210/288) of the students selected three or more items. The results of comparisons for gender and judgment of the potential of the app compared to a book for education and for the job, respectively, are presented in .
Table 1. Group comparisons for possible extensions to future app based on gender (male vs. female) and relative potential of apps (students attributing a higher potential to apps vs. those attributing a higher potential to textbooks) (Chi-square test, items are sorted in order of overall preferences).
Those students aspiring to a GP career were significantly more interested in using the app to stay in contact with the university than those who preferred another specialty and those who had not yet made a decision (52.9% vs. 28.3% vs. 23.9%, p = 0.040). Differences based on the consideration to use the app for the purpose of supporting the opening of one’s own practice are presented in .
Discussion
Main findings
After having tried a prototype of an educational app on general practice, students signalled their interest in further development and highlighted the potential of the app prototype over medical textbooks for both education and medical practice. While using a future app on general practice for diagnostics, therapy and prediction were popular among almost all surveyed students, group comparisons highlighted differentiated preferences for the other, less desired features. Despite the overall moderate interest towards most of the functionalities, the mean number of functionalities selected was over four, which indicates that although students see a general potential for an app, preferences towards specific functionalities may differ.
Strengths and limitations
This study addresses an innovative and relevant topic, namely the future generation of doctors’ perception on employing apps. It provides evidence on this topic from Germany from the field of general practice, where research is scarce. The results are especially relevant to developers, for practitioners as well as for suppliers of healthcare software, as we provide evidence of their target customer’s needs. The high response rate (total estimation) is a further strength of the study.
As a possible limitation it could be argued that although fourth-year medical students typically have completed clerkships, they might have an inexperienced view on the effects of specific app extensions for their work as physicians. Furthermore, the results are based on only one medical faculty, which may limit generalizability. However, since medical students in Germany are not entirely able to choose their university by themselves, it seems unlikely that the medical students in Leipzig differ relevantly from those of other German universities.
Interpretation of the study results in relation to existing literature
Convenience of an app for information access
Using the future app as a physician to look up information was considered highly attractive by surveyed students. We found no differences for the preference of this feature based on the group comparisons, which could be due to the high convenience an app offers in quickly accessing or searching specific content while being portable. Another benefit of mobile resources over traditional methods of accessing information lies within their easy updateability. Reportedly, online resources are more up-to-date than textbooks.[Citation14] An app can simplify the access to relevant state of the art information.[Citation15] These benefits are reflected in the presence of apps for topics that require detailed information, such as disease diagnosis and management or drug references, which have been found to be commonly used among students in Germany and the UK.[Citation10,Citation16] Such benefits may result in time savings and increased quality of clinical decision making.[Citation4,Citation17].
Contact to university
The overall moderate to low interest in using the app for contact with the university if it provides specific services may be explained by the fact that for most graduates in the German healthcare system the university has a very limited role in practical postgraduate medical education. It has, however, been significantly preferred by those students who aspire to a GP career. This may be explained by the anticipation to work in a single-handed practice, which makes the access to mobile up-to-date information delivered through a trustworthy channel valuable, especially since currently no institution regulates medical apps or websites, thereby letting professionals solely rely on their own judgment.[Citation18] Other authors reasoned that with trustworthy and validated apps, health care professionals can be more confident about employing smartphones in a clinical setting.[Citation19]
Students' experience
We found that the surveyed students would like to use the app in areas where students typically use mobile devices already, in areas that are obviously related to medical education and in those that can be expected to be related to clinical work (e.g. during the final year or when starting postgraduate education). In these fields students can easily picture the direct benefits of an app with the respective functionality. For example, although accessing the patient file with an app can improve efficiency and quality of documentation resulting in more time for direct patient care,[Citation20,Citation21] we found that 4th year students do not attribute an extraordinary relevance to such a feature. Similarly, as 4th year students are far away from operating their own practice, the low interest towards other functionalities, such as procurement of goods and services as well as marketing, may be explained (). Existing marketing apps for medical services, however, have demonstrated effectiveness in other fields of medicine.[Citation22]
Gender differences
With regard to gender, previous literature found no differences in technology perceptions and more specifically in the use of mobile apps for medical purposes among the younger generation.[Citation23,Citation24] However, we found that males wanted to use the app for rather more technical tasks than did females. Females may prefer to use the app for supporting organizational tasks more than males. These findings are, in principle, in accordance with those from Kennedy et al., who reported different usage of the Internet among males and females.[Citation25]
Using an app for opening an own medical practice
Students who considered using the app to support the opening of their own practice preferred other purposes significantly more. This could be due to the respective features being perceived as more beneficial in a practice-based than in a hospital-based setting. There might be lower barriers to using a mobile device in this environment. For example, there is no need to explain oneself to colleagues for using a smartphone to avoid making an unprofessional impression.[Citation16,Citation17] Results also suggest that students considering opening their own practice would like to use a future app for collaboration and networking. This is interesting considering that practices in Germany are usually single-handed. Reportedly, social media and Web 2.0 tools improve collaboration in problem solving, sharing of knowledge and networking among medical students.[Citation26,Citation27] Additionally, such a community could help young physicians with organizing their medical training, which also has been significantly more preferred by those who want to use a future app to support the opening of their own practice. The same group was also more interested in using the app with peripheral devices (e.g. portable ultrasound systems and electrocardiographic Bluetooth devices). The combination of smartphones and peripheral devices is able to simplify and improve patient care in general practice settings.[Citation28,Citation29]
Implications
Others stated that students should acquire the skills that enable them to effectively use mobile learning in the workplace.[Citation8] We believe this can be warranted by providing medical students with an app that not only aids them during undergraduate education, but also after graduation. Our results on students’ demands towards practice oriented app extensions suggest that the future generation of doctors is very open to employing medical apps. Thus, healthcare institutions should be prepared to provide useful mobile technologies and encourage their usage.
Conclusion
Medical students attribute a higher potential to an app on general practice than to a textbook. They expressed demand for practice oriented app extensions and are willing to use a future app in subsequent daily practice mainly for access to knowledge on diagnostics, therapy, and prediction as well as for collaboration. Future research should assess priorities of cohorts in later stages of medical education and different countries.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
References
- Bort-Roig J, Gilson ND, Puig-Ribera A, et al. Measuring and influencing physical activity with smartphone technology: a systematic review. Sports Med. 2014;44:671–686.
- Khalifian S, Markman T, Sampognaro P, et al. Medical student appraisal: searching on smartphones. Appl Clin Inform. 2013;4:53–60.
- Ventola CL. Mobile devices and apps for health care professionals: uses and benefits. Pharm Ther. 2014;39:356–364.
- Koh KC, Wan JK, Selvanathan S, et al. Medical students’ perceptions regarding the impact of mobile medical applications on their clinical practice. J Mob Technol Med. 2014;3:46–53.
- O’Connor P, Byrne D, Butt M, et al. Interns and their smartphones: use for clinical practice. Postgrad Med J. 2014;90:75–79.
- Robinson T, Cronin T, Ibrahim H, et al. Smartphone use and acceptability among clinical medical students: a questionnaire-based study. J Med Syst. 2013;37:9936.
- Stanford School of Medicine. App Recommendations. 2014a. Available at: http://med.stanford.edu/estudent/ipads/app-recommendations.html [accessed at 2014-12-09]
- Fuller R, Joynes V. Should mobile learning be compulsory for preparing students for learning in the workplace? Br J Educ Technol. 2015;46:153–158.
- Choi JS, Yi B, Park JH, et al. The uses of the smartphone for doctors: an empirical study from Samsung Medical Center. Healthc Inform Res. 2011;17:131–138.
- Sandholzer M, Rurik I, Deutsch T, et al. Medical students’ expectations towards an implementation of a family medicine textbook as a comprehensive app in Germany. J Med Syst. 2014;38:1–9.
- Sandholzer M, Deutsch T, Frese T, et al. Predictors of students’ self-reported adoption of a smartphone application for medical education in general practice. BMC Med Educ. 2015;15:91.
- Sandholzer H, Frese T. Allgemeinmedizin: Familienmedizin. 3rd edn. Aachen: Shaker Verlag; 2010.
- Ozdalga E, Ozdalga A, Ahuja N. The smartphone in medicine: a review of current and potential use among physicians and students. J Med Internet Res. 2012;14:e128.
- Reavley NJ, Mackinnon AJ, Morgan AJ, et al. Quality of information sources about mental disorders: a comparison of Wikipedia with centrally controlled web and printed sources. Psychol Med. 2012;42:1753–1762.
- Davies K, Harrison J. The information-seeking behaviour of doctors: a review of the evidence. Health Info Libr J. 2007;24:78–94.
- Payne KFB, Wharrad H, Watts K. Smartphone and medical related app use among medical students and junior doctors in the United Kingdom (UK): a regional survey. BMC Med Inform Decis Mak. 2012;12:121.
- Payne KF, Weeks L, Dunning P. A mixed methods pilot study to investigate the impact of a hospital-specific iPhone application (iTreat) within a British junior doctor cohort. Health Informatics J. 2014;20:59–73.
- Visser BJ, Bouman J. Student BMJ: There’s a medical app for that. Student Br Med J. 2012;20:e2162.
- Bierbrier R, Lo V, Wu RC. Evaluation of the accuracy of smartphone medical calculation apps. J Med Internet Res. 2014;16:e32.
- Sampognaro PJ, Mitchell SL, Weeks SR, et al. Medical student appraisal: electronic resources for inpatient pre-rounding. Appl Clin Inform. 2013;4:403–418.
- Mickan S, Tilson JK, Atherton H, et al. Evidence of effectiveness of health care professionals using handheld computers: a scoping review of systematic reviews. J Med Internet Res. 2013;15:e212.
- Workman AD, Gupta SC. A plastic surgeon’s guide to applying smartphone technology in patient care. Aesthet Surg J. 2013;33:275–280.
- Bibault J-E, Leroy T, Blanchard P, et al. Mobile technology and social media in the clinical practice of young radiation oncologists: results of a comprehensive nationwide cross-sectional study. Int J Radiat Oncol Biol Phys. 2014;90:231–237.
- Ward R, Stevens C, Brentnall P, et al. The attitudes of health care staff to information technology: a comprehensive review of the research literature. Health Info Libr J. 2008;25:81–97.
- Kennedy T, Wellman B, Klement K. Gendering the digital divide. IT & Society. 2003;1:72–96.
- Bullock A. Does technology help doctors to access, use and share knowledge? Med Educ. 2014;48:28–33.
- George DR, Dellasega C. Use of social media in graduate-level medical humanities education: two pilot studies from Penn State College of Medicine. Med Teach. 2011;33:e429–434.
- Haddock LJ, Kim DY, Mukai S. Simple, inexpensive technique for high-quality smartphone fundus photography in human and animal eyes. J Ophthalmol. 2013;2013:518479.
- Slaveykov K, Tanev I, Trifonova K, et al. Cost effective screening for diabetic retinopathy in the general practice setting during economic crisis. EGPRN-Meeting, Heraklion, Oct 24th 2014. Available at: http://www.egprn.org/index.php?option=com_jdownloads&Itemid=97&view=finish&cid=911&catid=1 [accessed at 2015-11-01]