X-linked retinoschisis (XLRS) is an early-onset hereditary retinal dystrophy. This disease is caused by mutation(s) of the RS1 gene, which encodes for a protein (retinoschisin) that binds to the external membrane of photoreceptor and bipolar cells and plays a role in the structural integrity of the retinal layers.Citation1 In the first few decades of life cystic-appearing (schitic) lesions are found in the macula, and central visual acuity is decreased. Clinically detectable peripheral retinoschisis, most commonly observed bilaterally in the inferior-temporal retina, is often found in XLRS. Subclinical extramacular cystoid spaces were observed on spectral-domain optical coherence tomography (SD-OCT) in 5 of 11 eyes of XLRS patients in one study.Citation2 Carbonic anhydrase inhibitors have been found to reduce the macular intraretinal cystoid spaces in a notable number of XLRS patients.Citation3 In this current report, we present a patient diagnosed with XLRS with intraretinal cystoid spaces in the macula and extending to the mid-peripheral retina. With the use of topical dorzolamide 2%, the intraretinal cystoid spaces resolved from the macula out to the mid-peripheral retina. To our knowledge, the resolution of mid-peripheral retinal cystoid spaces with the use of a carbonic anhydrase inhibitor has not been previously reported.
Case Report
A 34-year-old man presented with a chief complaint of long-standing difficulty with distance and near central vision. He reported only slight difficulty with night driving and no color or peripheral vision complaints. His medical history was remarkable for a cardiac murmur, generalized anxiety, and hypercholesterolemia. There was no known family history of hereditary eye disease. The patient’s best-corrected visual acuity was 20/40−2 in each eye. He read 17/17 Ishihara color plates in each eye. Confrontation visual fields were full. On dilated fundus exam, cystic-appearing lesions in a honeycomb pattern and some central hypopigmentation were seen in the macula of each eye. The optic discs and retinal blood vessels were normal although situs inversus of the retinal vessels was noted in both eyes. No peripheral retinoschisis was observed in either eye.
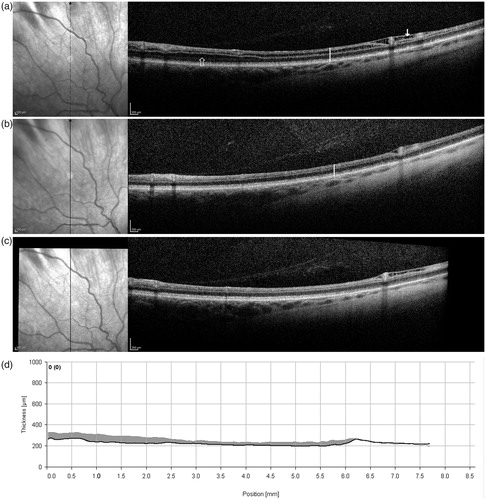
An electroretinogram of the right eye demonstrated selective b-wave reduction to a white single-flash stimulus, under both dark-adapted and light-adapted conditions. SD-OCT (Heidelberg Spectralis HRA + OCT, Heidelberg, Germany) line scans of the macula showed splitting of retinal layers in both eyes, with a large cyst centrally in the right eye. A mid-peripheral SD-OCT line scan of the superior retina demonstrated intraretinal cystoid spaces in both eyes, OD greater than OS. The extramacular cystoid spaces OD involved the outer nuclear layer, inner nuclear layer, and retinal nerve fiber layer ().
FIGURE 1. Right eye vertical SD-OCT line scans of the superior retina (about 10° to 40° from foveal center) at baseline, prior to treatment (a), and after 3 months (b) and 6 months (c) of treatment on topical dorzolamide 2% TID OU. At baseline (a), note splitting of the retina in the outer nuclear layer (open arrow), inner nuclear layer (vertical white line), and retinal nerve fiber layer (closed arrow). At follow-up the splitting is markedly reduced in both the outer and inner nuclear layers, while splitting of the retinal nerve fiber layer remained. No change from baseline to follow-up is seen in the outer segment ellipsoid layer, retinal pigment epithelial layer or posterior vitreous. The retinal thickness (from internal limiting membrane to Bruch’s membrane) at the location marked by the vertical white line in the SD-OCT images is 233 microns at baseline (a) and 207 microns at follow-up (b). The OCT line scan in (c) is aligned with a baseline OCT line scan, and the thickness profile difference is shown in (d) as the shaded gray area.
With a clinical diagnosis of X-linked retinoschisis, diagnostic molecular genetic testing was performed looking for mutations in the RS1 gene, which is known to underlie XLRS. Genomic DNA was extracted, PCR amplified, and sequenced according to standard procedures at the Carver non-profit genetic testing laboratory at the University of Iowa. A hemizygous Pro192Ser mutation was found in the RS1 gene.
The patient was prescribed topical dorzolamide 2% (off-label) in both eyes three times a day as treatment for the macular schisis. He returned for follow-up 3 months later. At that visit, he was uncertain of any definite visual change. Visual acuities were 20/40+2 in each eye. Dilated fundus exam still showed slight mottling in the macula, but no definite macular schisis. SD-OCT showed marked reduction in intraretinal cystoid spaces in the macula and superior retinal mid-periphery () of the right eye. Similar reductions in less extensive intraretinal cystoid spaces were found in the left macula and superior mid-periphery. The effect was maintained at another follow-up visit 6 months from baseline ().
Discussion
To our knowledge, this is the first report of a reduction of extramacular cystoid spaces in XLRS with a pharmacologic treatment. This micro-anatomical improvement likely occurs in other XLRS patients who have been treated with carbonic anhydrase inhibitors, but it remains unappreciated if the extramacular areas are not scanned with SD-OCT. Such extramacular cystoid spaces are a relatively new observation and the longitudinal course of extramacular cystoid spaces is unknown. Macular cystoid spaces persist in XLRS patients, except in cases of pharmacologic treatment,Citation3 outer retinal degeneration,Citation4 or posterior vitrectomy.Citation5 We expect that extramacular cystoid spaces should similarly persist.
Treatment with topical CAIs can both reduce macular cystoid spaces and improve visual acuity in at least some patients with XLRS.Citation3 Some patients with XLRS have reduced retinal sensitivity in the mid-periphery and periphery even in the absence of ophthalmoscopically detectable peripheral retinoschisis.Citation4,Citation6 In this case, we did not test for functional changes (e.g. with formal visual fields) since we did not anticipate the extent of resolution in the extramacular cysts. It remains to be demonstrated whether the resolution of cystoid spaces observed in the mid-peripheral retina in such patients results in a corresponding improvement in retinal function.
Declaration of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper. This research was supported by the Illinois Society for the Prevention of Blindness.
References
- Molday RS, Kellner U, Weber BH. X-linked juvenile retinoschisis: clinical diagnosis, genetic analysis, and molecular mechanisms. Prog Retin Eye Res 2012;31:195–212
- Gregori NZ, Lam BL, Gregori G, et al. Wide-field spectral-domain optical coherence tomography in patients and carriers of X-linked retinoschisis. Ophthalmology 2013;120:169–174
- Genead MA, Fishman GA, Walia S. Efficacy of sustained topical dorzolamide therapy for cystic macular lesions in patients with X-linked retinoschisis. Arch Ophthalmol 2010;128:190–197
- Apushkin MA, Fishman GA, Rajagopalan AS. Fundus findings and longitudinal study of visual acuity loss in patients with X-linked retinoschisis. Retina 2005;25:612–218
- Yu H, Li T, Luo Y, et al. Long-term outcomes of vitrectomy for progressive X-linked retinoschisis. Am J Ophthalmol 2012;154:394–402
- Peachey NS, Fishman GA, Derlaki DJ, Brigell MG. Psychophysical and electroretinographic findings in X-linked juvenile retinoschisis. Arch Ophthalmol 1987;105:513–516

