Abstract
Background and purpose — While highly crosslinked polyethylene has shown reduced in vivo wear and lower rates of revision for total hip arthroplasty, there have been few long-term studies on its use in total knee arthroplasty (TKA). We compared the rate of revision of non-crosslinked polyethylene to that of crosslinked polyethylene in patients who underwent TKA for osteoarthritis.
Patients and methods — We examined data from the Australian Orthopaedic Association National Joint Replacement Registry on 302,214 primary TKA procedures with non-crosslinked polyethylene and 83,890 procedures with crosslinked polyethylene, all of which were performed for osteoarthritis. The survivorship of the different polyethylenes was estimated using the Kaplan-Meier method and was compared using proportional hazard models.
Results — The 10-year cumulative revision rate for non-crosslinked polyethylene was 5.8% (95% CI: 5.7–6.0) and for crosslinked polyethylene it was 3.5% (95% CI: 3.2–3.8) (> 6.5-year HR = 2.2 (1.5–3.1); p < 0.001). There was no effect of surgical volume or method of prosthesis fixation on outcome. There were 4 different TKA designs that had a minimum of 2,500 procedures in at least 1 of the polyethylene groups and a follow-up of ≥ 5 years. 2 of these, the NexGen and the Natural Knee II, had a lower rate of revision for crosslinked polyethylene. The Scorpio NRG/Series 7000 and the Triathlon Knee did not show a lower rate of revision for crosslinked polyethylene.
Interpretation — There is a lower rate of revision for crosslinked polyethylene in TKA, and this appears to be prosthesis-specific and when it occurs is most evident in patients < 65 years of age. The difference in revision rates was mainly due to revisions because of lysis and loosening.
Crosslinked polyethylene has shown reduced in vivo wear rates and lower revision rates in clinical studies when used for conventional primary total hip arthroplasty (CitationThomas et al. 2011, CitationLee et al. 2011, CitationBabovic and Trousdale 2013, CitationSnir et al. 2014, CitationAustralian Orthopaedic Association National Joint Replacement Registry (AOANJRR) Annual Report 2014). However, it is uncertain whether the same benefit occurs with total knee arthroplasty (TKA). Polyethylene wear is multifactoral and can be influenced by prosthesis design, technical issues such as alignment, and patient-related factors. The biomechanical environment differs in the knee, with polyethylene being subject to deformation, delamination, and potential crack propagation. This has led to concerns with the use of crosslinked polyethylene in TKA because of reduced strength and fatigue resistance. In vitro studies have shown a decrease in wear with increasing radiation dose from 50 to 100k Gy, but toughness decreased with the higher radiation dose (CitationAkagi et al. 2006, CitationAsano et al. 2007). Knee simulator models of wear have shown less wear for crosslinked polyethylene than for standard compression-molded polyethylene in both aged and unaged forms of the material. Reduced wear was also found in crosslinked polyethylene when subjected to diverse wear models with a scratched femoral component or an unbalanced knee (CitationMuratoglu et al. 2002, Citation2004, CitationHermida et al. 2008). There have, however, only been a few reports of the clinical results of highly crosslinked polyethylene in TKA (CitationHodrick et al. 2008, CitationMinoda et al. 2009, CitationLong et al. 2012). While these studies have shown no difference in clinical or radiographic outcomes when comparing crosslinked polyethylene with non-crosslinked polyethylene, the longest follow-up was 7 years. Longer-term information is lacking.
We compared the rates of revision of non-crosslinked polyethylene and crosslinked polyethylene for all patients who underwent TKA for osteoarthritis as reported to the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR).
Methods
The AOANJRR began data collection on September 1, 1999, and it includes data on over 98% of the arthroplasty procedures performed in Australia since 2002. Registry data are validated against patient-level data provided by each of the state and territory health departments in Australia using a sequential, multilevel matching process. A matching program is run on a monthly basis to search for all primary and revision arthroplasty procedures recorded in the registry that involve the same side and joint of the same patient, thus enabling each revision to be linked to the primary procedure. Data are also matched biannually with the National Death Index of the Department of Health and Ageing to obtain information on the date of death. The registry records the reasons for revision and the type of revision of TKA, and categorizes revision surgery as major or minor. A major revision involves revision of either the tibial or the femoral component, or both. Minor revisions are all other revisions usually including patellar resurfacing and tibial insert changes.
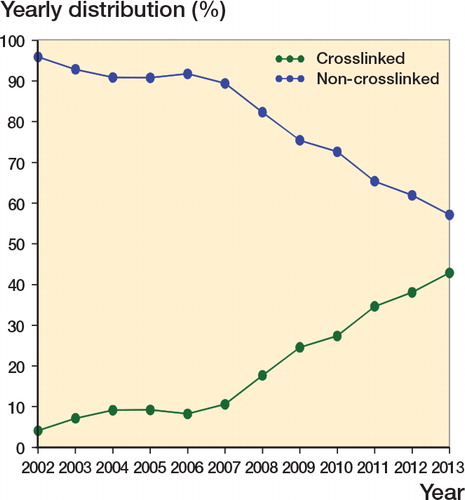
Crosslinked polyethylene was defined in the registry database as ultra-high-molecular-weight polyethylene that has been irradiated with high-dose (≥ 50 kGy) gamma or electron beam radiation, regardless of remelting or annealing. The definition of polyethylene was confirmed with industry and cross-checked with the Australian Prosthesis Advisory List, which records crosslinked polyethylene separately from conventional polyethylene. Vit E crosslinked polyethylene has been recorded separately but included in the crosslinked polyethylene in this study, due to short-term follow-up and its use with 1 type of prosthesis. The study population was all patients with primary TKAs undergone for osteoarthritis (OA). The registry first recorded the use of crosslinked polyethylene in 2001. During the study period, there were 302,214 primary TKA procedures performed for OA reported to the registry that used non-crosslinked polyethylene and there were 83,890 that used crosslinked polyethylene. There was an increase in the use of crosslinked polyethylene, with over 40% of all primary TKA procedures performed in 2013 using crosslinked polyethylene (). Outcomes were determined for all procedures, comparing TKA performed with non-crosslinked polyethylene and crosslinked polyethylene and including the effect of age, sex, and reason for revision. The types of revision were also analyzed.
Figure 1. Relative proportions of primary total knee replacements according to type of polyethylene bearing surface (all diagnoses).
In order to account for possible confounders, we also performed a number of subanalyses. These included method of fixation, type of tibial bearing, the impact of surgical volume, and brand of prosthesis. The effect of the method of fixation (cemented, hybrid, and cementless) and tibial bearing surface (fixed-bearing, mobile, and rotating) with crosslinked and non-crosslinked polyethylene in TKA was examined. Data on the number of TKAs performed were analyzed. Surgeons were divided into 4 groups based on the average number of procedures per year: ≤ 10, 11–25, 26–70, and > 70 TKAs per year.
A separate analysis was performed on specific prostheses that have both crosslinked and non-crosslinked polyethylene options. The criteria for inclusion were a minimum of 2,500 procedures in at least 1 of the polyethylene groups and a follow-up time of 5 or more years.
Statistics
The registry uses Kaplan-Meier estimates of survivorship to describe the time to the first revision of an arthroplasty, with censoring at th
e time of death or closure of the database at the time of analysis. The unadjusted cumulative percentage revision (CPR) after the primary arthroplasty, with an accompanying 95% confidence interval (CI), was calculated using unadjusted pointwise Greenwood estimates. Hazard ratios were calculated using Cox proportional-hazards models, adjusting for age and sex, and were used to make statistical comparisons of the revision rates between groups. The assumption of proportional hazards was checked analytically for each model; if the interaction between the predictor and the log of the postoperative time was significant in the standard Cox model, then a time-varying model was used. Time points were iteratively chosen until the assumption of proportionality was met, and the hazard ratios were calculated for each selected time period. All tests were 2-tailed at the 5% level of significance. Statistical analysis was performed using SAS software version 9.3.
Ethics
The study was approved by the Commonwealth of Australia as a Declaration of Quality Assurance Activity under section 124X of the Health Insurance Act, 1973. All investigations were conducted in accordance with ethical principles of research (the Helsinki Declaration II).
Results
The 10-year CPR for non-crosslinked polyethylene was 5.8% (CI: 5.7–6.0) and for crosslinked polyethylene it was 3.5% (CI: 3.2–3.8) (HR after 6.5 years = 2.2 (1.5–3.1); p < 0.001) (). The main reason for the difference in revision rate was a reduction in the rate of revision for the wear-related problems of loosening and lysis. The 10-year CPR for loosening/lysis for non-crosslinked polyethylene was 1.9% (CI: 1.9–2.0) and for crosslinked polyethylene it was 0.9% (CI: 0.7–1.0) (HR = 1.8 (1.6–2.0); p < 0.001) (). The reasons for revision of TKA for both crosslinked polyethylene and non-crosslinked polyethylene are listed in .
Figure 2. Cumulative percentage revision of primary total knee replacements according to type of polyethylene bearing surface (with OA as primary diagnosis).
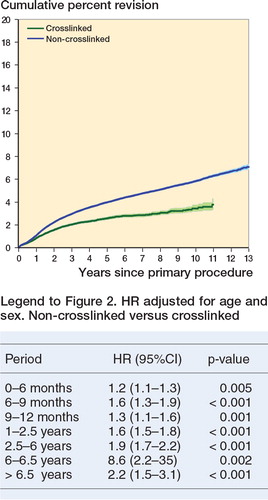
Figure 3. Cumulative percentage revision of primary total knee replacements according to type of polyethylene bearing surface (revision for loosening/lysis, with OA as primary diagnosis). Non crosslinked vs crosslinked (entire period): HR = 1.80 (1.61–2.02), p < 0.001 (HR adjusted for age and sex).
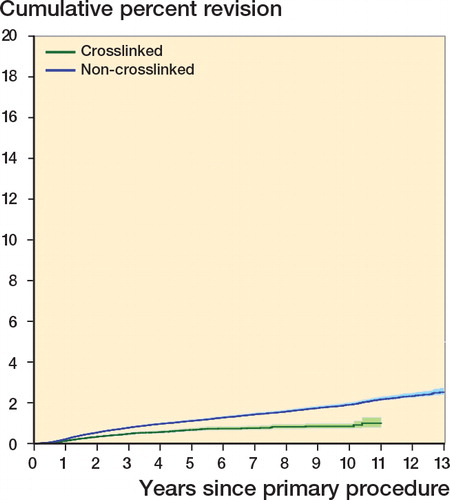
Table 1. Revision diagnosis of primary total knee replacement according to type of polyethylene bearing surface (with OA as primary diagnosis)
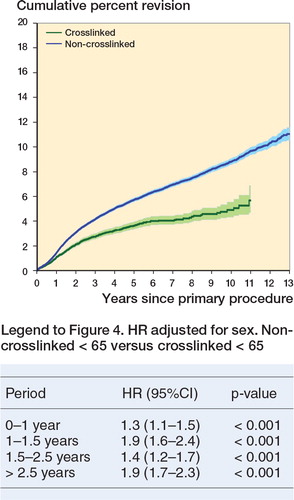
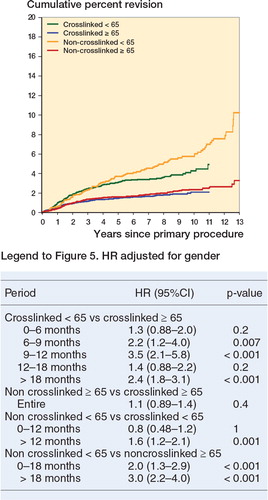
The effect of crosslinked polyethylene was more pronounced in the younger age groups. For patients less than 65 years of age, the 10-year CPR for non-crosslinked polyethylene was 8.8% (CI: 8.5–9.1) and it was 4.9% (CI 4.3–5.5) for crosslinked polyethylene (HR after 2.5 years = 1.95 (1.7–2.3); p < 0.001) ().
Figure 4. Cumulative percentage revision of primary total knee replacements in patients aged < 65 years, according to type of polyethylene bearing surface (with OA as primary diagnosis).
The type of fixation had no effect on the outcomes when comparing non-crosslinked polyethylene and crosslinked polyethylene. For all cemented TKAs, cementless TKAs, and hybrid TKAs, the rate of revision was always lower for crosslinked polyethylene. The type of tibial bearing was examined, but there was only 1 type of knee prosthesis that had sufficient numbers of fixed and mobile bearing surfaces with the 2 types of polyethylene for analysis. This was the NexGen Posterior Stabilized TKA, and at 5 years there was no significant difference in the rate of revision between the fixed-bearing knee and the rotating mobile knee regarding the type of polyethylene. The use of crosslinked polyethylene and non-crosslinked polyethylene was evenly spread over all 4 surgical volume groups. For the surgical volume groups 11–25, 26–70, and > 70, there was a significant reduction in the rate of revision for crosslinked polyethylene (p < 0.001). There was no difference in the rate of revision in the low-volume (≤ 10) group, although this was probably due to the smaller numbers of procedures available for analysis.
Prosthesis-specific analysis
4 different TKA designs fulfilled the criteria of a minimum of 2,500 procedures in at least 1 of the polyethylene groups and a follow-up of 5 or more years. These were the Natural Knee II, the Triathlon, the NexGen, and the Scorpio ().
Table 2. Cumulative percentage revision (95% confidence intervals) of primary total knee replacements according to type of polyethylene bearing surface and age, for specific prostheses (with OA as primary diagnosis)
The Natural Knee II only includes minimally stabilized prostheses, as the posterior-stabilized option has seldom been used. The registry has 10-year follow-up for both types of polyethylene. Crosslinked polyethylene was used in 54% of the procedures, and had a lower rate of revision after 3.5 years. The 10-year CPR for non-crosslinked polyethylene was 7.4% (CI: 6.3–8.5) as compared to 3.8% (CI: 3.0–4.7) for crosslinked (HR after 3.5 years = 3.2 (2.1–5.0); p < 0.001). This difference was evident regardless of age; however, the difference was greater for those who were less than 65 years old.
The Triathlon knee had a minimum 5-year follow-up for both types of polyethylene, and crosslinked polyethylene was used in 72% of the procedures. There was no difference in the rates of revision for both minimally and posterior-stabilized Triathlon prostheses when comparing non-crosslinked and crosslinked polyethylene (HR = 1.0 (0.9–1.2); p = 0.9; and HR = 1.3 (0.95–1.7); p = 0.1).
The NexGen knee had 10-year follow-up for both crosslinked and non-crosslinked polyethylene for the minimally stabilized prosthesis, and 7-year follow-up for the posterior-stabilized prosthesis. Crosslinked polyethylene was used in 76% of minimally stabilized NexGen CR and CR Flex knees, and had a lower rate of revision after 2.5 years. This difference, however, was only evident in those aged less than 65 years. The 10-year CPR for patients aged < 65 with non-crosslinked polyethylene was 5.8% (4.6–7.1), as compared to 4.3% (3.6–5.1) for crosslinked polyethylene (HR after 1 year = 1.6 (1.2–2.1); p = 0.001) (). Crosslinked polyethylene was used in 30% of posterior-stabilized NexGen LPS and LPS Flex knees. The rates of revision were similar when comparing non-crosslinked and crosslinked polyethylene in the posterior-stabilized group.
Figure 5. Cumulative percentage revision of minimally stabilized Nexgen primary total knee replacements according to type of polyethylene bearing surface and age (with OA as primary diagnosis).
The Scorpio NRG/Series 7000 knee had 5-year follow-up for non-crosslinked and crosslinked polyethylene, and the latter was used in 86% of procedures. There was no difference in the rates of revision with minimally and posterior-stabilized Scorpio NRG/Series 7000 prostheses when comparing non-crosslinked and crosslinked polyethylene (HR = 1.3 (0.7–2.6); p = 0.4; and HR = 0.61 (0.34–1.1); p = 0.08).
Discussion
This is the first study to demonstrate a reduced rate of revision for crosslinked polyethylene in TKA in a population-based registry. When a new device or material has been introduced, post-market surveillance is important and registries are ideally suited to determine outcomes—and especially to show whether there are any early problems associated with new prostheses. Concerns regarding the mechanical properties of crosslinked polyethylene in TKA have not been identified in the results reported from the registry. Polyethylene fracture as a reason for revision has only been recorded in 2 cases, suggesting that concerns regarding crosslinked polyethylene toughness are presently unfounded.
While there is a lower rate of revision for crosslinked polyethylene than for non-crosslinked polyethylene, this reduction is not evident for all prostheses. While crosslinked polyethylene is used frequently in hip arthroplasty, the uptake of crosslinked polyethylene for TKA has not been as great, although it accounts for 43% of all tibial polyethylene in 2013. At 10 years, there was a reduction in loosening/lysis as a reason for revision in the crosslinked polyethylene TKA group.
While TKA has a low rate of revision, there is considerable variation with age—with patients younger than 65 having a higher rate of revision (AOANJRR Annual Report 2014). It therefore becomes important to examine factors that may reduce this higher rate of revision. This study has demonstrated that while there is an overall reduction in the rate of revision for all ages when crosslinked polyethylene is used, this is more apparent in the younger age group (< 65). This may become more pronounced as revision for wear-related issues, such as loosening and lysis, increases over time.
In primary TKA, crosslinked polyethylene was used less frequently than non-crosslinked polyethylene and there was considerable prostheses difference in its use. While the registry has shown a lower rate of revision overall for crosslinked polyethylene, the analysis of crosslinked polyethylene may be confounded by well-performing prostheses with a higher use of crosslinked polyethylene. Consequently, any observed difference in revision rate may be confounded by prosthesis type. This study has demonstrated prosthesis variation in the effect that crosslinked polyethylene has on the rate of revision following TKA. A lower rate of revision was identified when crosslinked polyethylene was used in conjunction with the 2 minimally stabilized TKAs with 10-year follow-up (the Natural Knee II and NexGen) in comparison to the use of non-crosslinked polyethylene. This difference was most evident in younger patients. No significant difference in revision rate was identified for either the minimally stabilized or posterior-stabilized Triathlon and Scorpio NRG/Series 7000 TKAs.
One possible explanation for the variation in CPR differential between non-crosslinked and crosslinked polyethylene with different designs may be related to the type of crosslinked polyethylene used. The crosslinked polyethylene used in Natural Knee II is manufactured by electron beam irradiation of the polyethylene at an elevated temperature, to 95 kGy, followed by melting. In NexGen knees, the crosslinked polyethylene is made by electron beam irradiation at elevated temperature, to 65 kGy, followed by melting. In Triathlon and Scorpio knees, the crosslinked polyethylene is made by irradiating the polyethylene to 33 kGy in 3 consecutive steps, with annealing (heating to below the melting point) after each irradiation cycle. All 3 types of crosslinked polyethylene knees are packaged in air-permeable pouches and are gas-sterilized. Thus, during shelf storage they are exposed to air until implantation. Radiation generates trapped free radicals, which are known to cause oxidation; thus, either melting or annealing is used after irradiation to eliminate or reduce the trapped free radicals. Independent reports have shown that the annealing results in detectable trapping of free radicals, increasing the potential for oxidation during shelf storage and use in vivo. There have also been reports showing increased rates of failure due to damage to the polyethylene component, mainly caused by oxidation. It is therefore possible that radiation-crosslinked and annealed polyethylene components may not necessarily perform as well as radiation-crosslinked and melted polyethylene components in patients, in comparison to their non-crosslinked polyethylene counterparts, as found in the current study.
The first clinical study of crosslinked polyethylene was published by CitationHodrick et al. (2008), and they reported a consecutive series of 200 Natural Knee II systems (Zimmer), comparing the first 100 cases to receive crosslinked polyethylene with the previous 100 cases using non-crosslinked polyethylene. The crosslinked polyethylene group had an average age of 67, and was followed for a minimum of 69 months, as compared to an average age of 70 and a minimum follow-up of 82 months for the non-crosslinked group. In the crosslinked polyethylene group, there were no revisions for tibial wear but 2 patients had evidence of radiolucencies. In the non-crosslinked group, there were 20 patients who showed radiolucencies and 3 patients had revisions for tibial loosening and wear. The authors commented on some limitations of their study, which included 35 patients who had been lost to follow-up and lack of retrieval analysis. Our study reports on over 3,000 Natural Knee II TKA using crosslinked polyethylene with a 10-year CPR of 3.8%.
2 other clinical studies have reported on the outcomes of crosslinked polyethylene using the NexGen TKA (Zimmer) with Prolong crosslinked polyethylene, which is electron beam-irradiated to 65 kGy at an elevated temperature and subsequently melted. CitationMinoda et al. (2009) reported on a consecutive series of 113 CR TKAs with non-crosslinked polyethylene, and compared them to 89 CR TKAs using Prolong. At 2 years of follow-up, the clinical outcome was similar between the 2 groups—with no revisions and no evidence of osteolysis or polyethylene failure. CitationLong et al. (2012) reported on a consecutive series of 120 TKAs using the NexGen high flex posterior-stabilized knee. There were 97 patients who had a full clinical and radiographic evaluation at an average of 52 months. There were no cases of radiographic loosening or progressive radiolucent lines. Our study involved 35,557 NexGen TKAs with crosslinked polyethylene, and at 10 years the CPR was 2.8% for the NexGen CR TKA with crosslinked polyethylene. With a shorter follow-up of 7 years, we found no difference in the rates of revision of the NexGen PS knee for the 2 types of polyethylene.
This study has a number of strengths, including the large number of procedures, the use of population-based data, and the longer-term follow-up. Over 83,000 TKAs performed for osteoarthritis with the use of crosslinked polyethylene have been analyzed, making this the largest study to report on the outcomes of crosslinked polyethylene use in TKA. Crosslinked polyethylene is more expensive than conventional polyethylene, so it is important to demonstrate some benefit. The reduction in the rate of revision was seen in both low-volume and high-volume surgeons, and is therefore probably due to the crosslinked polyethylene and less likely to be due to surgeon-related factors.
A potential weakness of this study is that when crosslinked polyethylene was introduced, for each implant studied the tibial trays were new. This may have led to bias, as non-crosslinked polyethylene tibial trays may have been kept for a longer time period, leading to an extended shelf life before implantation. This could lead to a higher rate of revision. We therefore examined the rate of revision of non-crosslinked polyethylene before and after the introduction of crosslinked polyethylene for the NexGen and Triathlon TKA systems. There was no difference in the rates of revision for non-crosslinked polyethylene before and after the introduction of crosslinked polyethylene for these 2 knee systems.
Conclusion
A lower rate of revision has been shown for crosslinked polyethylene in TKA, and this appears to be prosthesis-specific and confined to minimally stabilized options. When it occurs, the lower rate of revision is most evident in patients who are less than 65 years of age and there is a reduction in revision for loosening/lysis.
RdS designed the research question and wrote the manuscript. AC and ML performed the statistical analyses. SG and OM performed critical revision of the manuscript. All the authors were responsible for the interpretation of data and for editing and final approval of the paper.
We thank the AOA National Joint Replacement Registry and the hospitals, orthopedic surgeons, and patients whose data made this work possible. The Australian Government funds the AOA NJRR through the Department of Health and Ageing.
No competing interests declared.
- Akagi M, Asano T, Clarke IC, Niiyama N, Kyomoto M, Nakamura T, Hamanishi C. Wear and toughness of crosslinked polyethylene for total knee replacements: A study using a simulator and small-punch testing. J Orthop Res 2006; 24(10): 2021–7.
- Asano T, Akagi M, Clarke IC, Masuda S, Ishii T, Nakamura T. Dose effects of cross-linking polyethylene for total knee arthroplasty on wear performance and mechanical properties. J Biomed Mater Res B Appl Biomater 2007; 83(2): 615–22
- Australian Orthopaedic Association National Joint Replacement Registry. Annual Report. Adelaide: AOA, 2014
- Babovic N, Trousdale RT. Total hip arthroplasty using highly cross-linked polyethylene in patients younger than 50 years with minimum 10-year follow-up. J Arthroplasty 2013; 28 (5): 815–7.
- Hermida JC, Fischler A, Colwell C WJr, D’Lima DD. The effect of oxidative aging on the wear performance of highly cross-linked polyethylene knee inserts under conditions of severe malalignment. J Orthop Res 2008; 26(12):1585–90.
- Hodrick JT, Severson EP, McAlister DS, Dahl B, Hofmann AA. Highly crosslinked polyethylene is safe for use in total knee arthroplasty. Clin Orthop Relat Res 2008; 466 (11): 2806–12.
- Lee JH, Lee BW, Lee BJ, Kim SY. Midterm results of primary total hip arthroplasty using highly cross-linked polyethylene: minimum 7-year follow-up study. J Arthroplasty 2011; 26 (7): 1014–9.
- Long WJ, Levi GS, Scuderi GR. Highly cross-linked polyethylene in posterior stabilized total knee arthroplasty: early results. Orthop Clin N Am 2012; 43: 35–38.
- Minoda Y, Aihara M, Sakawa A, Fukuoka S, Hayakawa K, Tomita M, Umeda N, Ohzono K. Comparison between highly cross-linked and conventional polyethylene in total knee arthroplasty. The Knee 2009; 16: 348–51.
- Muratoglu OK, Bragdon CR, O’Connor DO, Perinchief RS, Jasty M, Harris WH. Aggressive wear testing of a cross-linked polyethylene in total knee arthroplasty. Clin Orthop Relat Res 2002; 404: 89–95.
- Muratoglu OK, Burroughs BR, Bragdon CR, Christensen SC, Lozynsky A, Harris WH. Knee simulator wear of polyethylene tibias articulating against explanted rough femoral components. Clin Orthop Relat Res 2004; 428: 108–13.
- Snir N, Kaye ID, Klifto CS, Hamula MJ, Wolfson TS, Schwarzkopf R, Jaffe FF. 10-year follow-up wear analysis of first-generation highly cross linked polyethylene in primary total hip arthroplasty. J Arthroplasty 2014; 29 (3): 630–3.
- Thomas GE, Simpson DJ, Mehmood S, Taylor A, McLardy-Smith P, Gill HS, Murray DW, Glyn-Jones S. The seven-year wear of highly cross-linked polyethylene in total hip arthroplasty: a double-blind, randomized controlled trial using radiostereometric analysis. J Bone Joint Surg Am 2011; 93 (8): 716–22.

