Abstract
Despite common perceptions to the contrary, pandemic diseases do not affect populations indiscriminately. In this paper, we review literature produced by demographers, historians, epidemiologists, and other researchers on disparities during the 1918–20 influenza pandemic and the Covid-19 pandemic. Evidence from these studies demonstrates that lower socio-economic status and minority/stigmatized race or ethnicity are associated with higher morbidity and mortality. However, such research often lacks theoretical frameworks or appropriate data to explain the mechanisms underlying these disparities fully. We suggest using a framework that considers proximal and distal factors contributing to differential exposure, susceptibility, and consequences as one way to move this research forward. Further, current pandemic preparedness plans emphasize medically defined risk groups and epidemiological approaches. Therefore, we conclude by arguing in favour of a transdisciplinary paradigm that recognizes socially defined risk groups, includes input from the social sciences and humanities and other diverse perspectives, and contributes to the reduction of health disparities before a pandemic hits.
Introduction
Both Covid-19 and the 1918–20 influenza pandemic struck the rich and famous—including United Kingdom (UK) Prime Minister Boris Johnson and actor Tom Hanks in 2020, and King of Spain Alfonso XIII and the famous Norwegian painter Edvard Munch in 1918—but these diseases did not kill the rich and poor alike. In both 2020–21 and 1918–20, particularly in high-income countries, severe disease and mortality were concentrated among the poor, immigrants, Black people, and Indigenous people (Mamelund Citation2006, Citation2011; Grantz et al. Citation2016; Bengtsson et al. Citation2018; Arrazola et al. Citation2020; Dahal et al. Citation2020; Drefahl et al. Citation2020; Han et al. Citation2020; Hatcher et al. Citation2020; Mamelund et al. Citation2020; Steyn et al. Citation2020; Williamson et al. Citation2020). Beach et al. (Citation2020) reviewed the consequences of Covid-19 and the 1918–20 influenza pandemic for demographic indicators including mortality, fertility, migration, later-life health, and economic inequalities. They also identified available historical data and further research needs, but touched only briefly on the role of socio-economic factors in pandemic mortality disparities. In this paper, we add to the literature by reviewing the association between social factors (socio-economic status (SES); race and ethnicity) and pandemic outcomes during the Covid-19 and 1918–20 influenza pandemics.
The comparison of these two major pandemics is particularly relevant, not only because of the recent interest in the 1918–20 influenza during its centenary in 2018–20, but also because 1918 (as we refer to this pandemic from now on) has frequently been used as a ‘worst-case scenario’ in discussions of pandemic preparedness. The Covid-19 pandemic is the most significant one since 1918, so a broader understanding of demographic and socio-economic impacts during and after a major pandemic is key. Nonetheless, epidemics and pandemics have not traditionally been a major focus in demography, and most studies have been historical (van Raalte, this issue), as indicated by the relatively few related publications in Population Studies (see e.g. Chandra (Citation2013) on the 1918 influenza and Alfani and Bonetti (Citation2019) on seventeenth-century plague).
Demography is a relatively small field in academia, with a broad remit covering not only a variety of patterns in, and influences on, mortality in general, but also patterns in, and influences on, fertility, households and families, and migration. Historical demography is a subfield with a similarly broad remit, and where the feasibility of research is often dictated by the availability of suitable data. It is perhaps not surprising, therefore, that relatively little existing research into historical epidemics and pandemics is found in the field of demography. Far more comes from the discipline of history, and this has affected the approaches taken towards the study of epidemics and particularly the use (or not) of quantitative methods. From the mid-1980s, the ‘narrative turn’ and critique of positivism led to a sharp decline in quantitative studies in history, sociology, geography, and allied disciplines (Ruggles and Magnuson Citation2020; Ruggles Citation2021). Demography was largely unaffected by this, although the quantity of work by other social scientists on demographic topics, such as epidemics, may have declined. However, in the last decade, there has been a slight revival of quantitative studies in major history journals in the United States (US) and also a ‘historical turn’ in sociology, economics, political science, and allied subjects (Ruggles Citation2021).
Because pandemics have not traditionally been a major focus in the field of demography, we discuss the historiography of how, since the 1970s, contemporary epidemiologists and historians, as well as demographers, have studied the socio-economic risk factors for 1918 influenza pandemic outcomes and ways in which demographers can contribute to the field in the future. Namely, while literature published after 2005 on the 1918 influenza and most of the literature on Covid-19 document social disparities, most studies lack the data and/or a theoretical framework to explain the mechanisms for these disparities. We present a framework developed by Crouse and Supriya (Citation2014) as one example of how future research can structure and analyse possible causes of disparities according to differential exposure, susceptibility, and healthcare consequences.
Although the two pandemics clearly demonstrate that such public health crises are not socially neutral and do not function as ‘great equalizer[s]’, as the singer Madonna infamously called Covid-19 in a heavily criticized and promptly deleted Instagram video, social inequalities are not yet taken into account in pandemic preparedness plans for influenza (Mamelund Citation2017), and social inequalities were often not explicitly taken into consideration in real-time public health work during Covid-19 in 2020–21. For example, information on public health interventions was initially published only in the majority languages in Norway, which may be one of several reasons for disproportional cases among some immigrant groups (Folkehelseinstituttet Citation2020a, Citation2020b, Citation2020c; Indseth et al. Citation2020, Citation2021), and it remains to be seen in 2021 and later whether countries are actually prioritizing vaccines for socially vulnerable groups in addition to older people and those medically at risk, as suggested by the Strategic Advisory Group of Experts on Immunization (SAGE) to the World Health Organization (WHO) and by the National Academies of Science, Engineering, and Medicine in the US (Schmidt et al. Citation2020). We therefore conclude this paper with suggestions for a paradigm shift in preparedness and public health work during pandemics. A robust preparedness for the twenty-first century would include reducing social inequalities in health and wealth before the next pandemic, as well as developing explicit plans for targeting not only the medically but also the socio-economically at risk during and after a new pandemic. Such a policy change would acknowledge that: (1) infectious diseases with pandemic potential have always been more than just a medical problem and that their epidemiology and impact are profoundly shaped by socio-economic factors; and (2) large-scale infectious disease pandemics are not confined only to history or low-income countries.
Epidemiology of the 1918 influenza and Covid-19 pandemics
Beginning in 1918, the so-called ‘Spanish flu’ spread around the world in three global waves. The earliest identified cases appeared in Kansas in the US, although other origins such as China and Europe have been proposed (Oxford et al. Citation1999; Shortridge Citation1999; Crosby Citation2003; Barry Citation2005; Oxford and Gill Citation2018). The cause of influenza was unknown at the time, and the pandemic-causing virus itself was not isolated and described until research beginning in the mid-1990s (Taubenberger et al. Citation2001; Taubenberger Citation2003; Barry Citation2005). The total mortality toll might have been as high as 50–100 million people, and a key characteristic of the pandemic was the disproportionately high mortality among young adults (Johnson and Mueller Citation2002; Olson et al. Citation2005). Nonetheless, some areas escaped significant impacts while other areas lost 90 per cent of their populations (Mamelund et al. Citation2013).
Approximately a century later, in late December 2019, an outbreak of pneumonia of an unknown aetiology was identified in Wuhan, Hubei Province, China. Out of 59 suspected cases, 27 individuals had a history of exposure to the Huanan Seafood Wholesale Market, which traded fish and live animals, including poultry and bats. The market was shut down on 1 January 2020, and the causative pathogen—a coronavirus ultimately named SARS-CoV-2—was identified on 7 January (Guarner Citation2020; Sohrabi et al. Citation2020; Wu et al. Citation2020). Likely zoonotic in origin, the natural reservoir remains undetermined, although bats are the most likely possibility (Wu et al. Citation2020). The first exported case was reported in Thailand on 13 January (Wu et al. Citation2020), and at the time of finalizing this paper (14 June 2021), 176,870,304 confirmed cases and 3.8 million deaths had been reported globally (Worldometer Citation2021). The WHO declared the disease a Public Health Emergency of International Concern on 30 January 2020, and characterized it as a pandemic on 11 March (Sohrabi et al. Citation2020; Williamson et al. Citation2020).
compares estimated infection and mortality statistics for seasonal influenza, the 1918 pandemic, and Covid-19. These estimates can vary in different sources or contexts, and as the Covid-19 pandemic is ongoing at the time of writing, total numbers of cases and deaths are still to be determined. For both pandemics, it is difficult to estimate infection fatality rates as exactly how many people were infected is unknown. However, data from surveys carried out in both the US and Norway suggest that case fatality rates for influenza in 1918 were 1 per cent in the summer and 2 per cent in the autumn (Mamelund et al. Citation2016). Case fatality rates for lab-confirmed cases of Covid-19 have been estimated at 2–3 per cent (Guarner Citation2020; Wu et al. Citation2020). However, lab-confirmed cases are capturing just the tip of the iceberg, and the large number of unreported cases is artificially pushing case fatality rates upwards. Estimates of fatalities among the infected (the infection fatality rate) based on serological studies range from under 0.1 per cent in India and some African countries (Ethiopia and Nigeria) to 0.2–2.0 per cent in the US and Europe (Levin et al. Citation2020; Meyerowitz-Katz and Merone Citation2020).
Table 1 Global disease outcomes during seasonal influenza, 1918 influenza, and Covid-19 (Covid-19 data up to 14 June 2021)
However, as mentioned, severe cases and deaths are not distributed equally across populations. Comparisons highlight many potential risk factors but, to date, most research on disparities in 1918 influenza pandemic or Covid-19 outcomes has focused on medically defined risk groups (e.g. high-risk age groups; those with pre-existing or comorbid health conditions). Some has focused on socially defined risk groups (low SES; immigrants; minority race or ethnicity), whereas little to no research has focused on both medical and social risk groups. Some of this may be due to the need for access to both types of data, often requiring linkage of hospital data, administrative data, and survey data, which may not always be at hand, especially in low-income countries. Consideration of both medical and social risk is nevertheless important, especially as these factors are likely to intersect as well as be important independently. summarizes the factors shown to be associated with higher risk during seasonal influenza, the 1918 influenza pandemic, and Covid-19. However, in the interest of space and due to the relative lack of emphasis in previous work and current pandemic preparedness, our subsequent discussion focuses on social risk groups.
Table 2 Summary of medical and social risk factors during seasonal influenza, 1918 influenza, and Covid-19
Evidence of disparities among socially defined risk groups
Socio-economic status
1918 influenza pandemic
A house-to-house survey of four cities in England found no clear relationship between social status and either the incidence of the disease or case fatality rates (Great Britain Ministry of Health Citation1920). However, a similar study published eleven years later by an influential epidemiologist at the time documented a clear association between four economic status categories (‘well to do’, ‘moderate’, ‘poor’, and ‘very poor’) and the incidence of symptomatic influenza illness and case fatality rates for White people in nine cities in the US (Sydenstricker Citation1931): going from the ‘well to do’ to the ‘very poor’ categories in turn, the self-reported morbidity percentages were, respectively, 23.2, 26.0, 33.0, and 37.3 per cent, while case fatalities for the same four groups were 1.5, 1.5, 1.7, and 2.8 per cent. After 1931, research on the 1918 influenza was ‘forgotten’ for the next 45 years, but experienced a renaissance when environmental and social historians started to study it in the late 1970s (Crosby Citation1976). The first wave of this historiography of the 1918 influenza with a focus on social factors continued into the 1980s before tapering off (Phillips Citation1984; Rice Citation1988; Tomkins Citation1992; Van Hartesveldt Citation1992). These 1918 influenza studies shared the idea that the disease, at least in terms of exposure and morbidity, but also mortality, was socially neutral. However, although almost all included aggregate-level, cross-table analysis, few studies had good data to analyse the mechanisms for social disparities at the individual level, and some relied mainly on anecdotal data from 1918 without empirically testing associations between social factors and pandemic outcomes.
Since the beginning of the 2000s, however, a number of studies by demographers, historians, geographers, epidemiologists, sociologists, and other researchers using better individual- and contextual-level data and more sophisticated methods have questioned the ‘socially neutral’ hypothesis, arguing that mortality at least must have had a clear social profile. Again, this is partly due to the fading of the cultural/narrative turn and revival of quantitative analysis in history but also to the historical turn in other disciplines (Ruggles and Magnuson Citation2020; Ruggles Citation2021). Some studies have included various attempts to examine socio-economic aspects but were inconclusive (Johnson Citation2006). Other studies have found strong links between SES and pandemic outcomes. A study of 27 countries, 24 US states, and nine Indian provinces, for example, found large differences in mortality between high- and low-income countries (Murray et al. Citation2007). India’s mortality was 40 times higher than Denmark’s. Using ordinary least squares (OLS) regressions the authors found that when controlling for latitude, a 10 per cent increase in income per head was associated with a 9–10 per cent decrease in mortality. In another ecological study, using 351 medical districts of Norway as units and OLS regressions, Mamelund (Citation2003) found that average wealth per person was significantly related to reduced mortality when controlling for age, sex, share of the population receiving public support due to poverty, crowding (number of persons per room), ethnicity, summer wave exposure, economic sectors, and coastal vs inland areas. A percentage point increase in wealth was associated with a 1.19 per cent reduction in influenza and pneumonia mortality. Further, a recent study of individual-level occupation-based social class and mortality in Sweden found a clear but not perfect class gradient in mortality (Bengtsson et al. Citation2018).
Cities with large pre-pandemic inequalities in health and wealth also showed large disparities in mortality in 1918. In the first and hitherto only individual-level survival analysis in the 1918 influenza literature, data from two parishes in the capital city of Norway (Kristiania, renamed Oslo in 1924) showed a clear but non-significant gradient in mortality by class (measured as occupation-based social class), while apartment size was significantly associated with a reduction in mortality (Mamelund Citation2006). This study also found that living in an impoverished area increased mortality when controlling for occupation-based social class, apartment size, age, sex, and marital status (Mamelund Citation2006). Survey data from the waves of the pandemic in Bergen, Norway, also suggest potential differences in exposure and subsequent outcomes based on SES, as measured by apartment size. The poor were affected first and experienced the highest morbidity in the first wave, whereas in the second wave morbidity was higher among the rich, probably due to a lack of exposure to the first wave and thus lower immunity (Mamelund Citation2018). Further, in a study using both individual- and contextual-level SES measures for Chicago in the US, illiteracy was found to be a significant predictor of higher mortality in 1918 when controlling for age and all other SES variables. There were also statistically significant positive associations between the basic reproduction number (R0, the average number of people infected by one infected person in a population with no immunity) and population density, illiteracy, and unemployment but not homeownership (Grantz et al. Citation2016).
It was long assumed that New Zealand, a country with small pre-pandemic baseline inequalities, saw small social disparities in influenza and pneumonia mortality from the 1918 influenza pandemic. Three studies using data on male soldiers found no associations between mortality and pre-enlistment occupation-based social class (Summers et al. Citation2010, Citation2013, Citation2014), while another early study likewise did not find any role for SES in mortality (Rice Citation1988). However, analysis using data for the civilian population of both sexes in the city of Auckland found clear indications of social disparities in mortality (Wilson et al. Citation2018). Those living in five ‘well to do’ suburbs experienced a crude mortality rate per 1,000 people of 6.4 (95 per cent confidence interval (CI) 5.5–7.4) compared with three ‘working class’ suburbs with mortality of 9.1 (95 per cent CI 7.4–11.1); similarly, ‘professionals’ experienced lower mortality (6.3; 95 per cent CI 5.5–7.3) than all other occupational groups (7.2; 95 per cent CI 7.0–7.5).
A systematic review and meta-analysis of the association between various SES measures (income; education; economic status; occupation-based social class; size of apartments; poor housing or crowding measures; having health insurance) and pandemic outcomes (infection/morbidity; hospitalization; mortality) considered nine studies of the 1918 influenza pandemic and 35 on the 2009–10 pandemic that was referred to early on as ‘swine flu’ (Mamelund et al. Citation2020). A random effects analysis of 46 estimates from 35 studies found a pooled mean odds ratio (OR) of 1.4 (95 per cent CI 1.2–1.7) when comparing the lowest with the highest SES. There was no evidence suggesting differences by pandemic period (1918 or 2009) or level of SES measure (individual or ecological). Of 14 studies on the 2009 pandemic including data on both medical and social risk factors, eight demonstrated an independent impact of SES after controlling for medical risk factors. These results show how persistent individual- and ecological-level social risk factors are, even though the mechanisms and types of social vulnerabilities leading to social disparities in pandemic outcomes may differ over time.
Covid-19 pandemic
Research conducted on socio-economic disparities in Covid-19 outcomes has focused on measures such as level of deprivation and/or economic development in residential or geographic areas, income or income inequality, education level, immigrant status, living situation (e.g. rural or urban; homelessness), and occupation. In some regions during early stages of the pandemic, higher numbers of lab-confirmed cases were seen in more affluent populations, likely due to travel history. For example, the introduction of the disease to Germany corresponded with travel, such as skiing in the Alps (Plümper and Neumayer Citation2020); a similar pattern was observed in Norway and may also be suggested by outbreaks on cruise ships. With the onset of community spread within new regions, however, infections, and/or severe outcomes became more concentrated within lower-SES populations (Plümper and Neumayer Citation2020). Comparisons of age-standardized incidence rates for cases between 26 February and 19 April 2020 among districts in Barcelona showed a positive relationship with mean income; incidence was 2.5 times greater in the district with the lowest mean income than the district with the highest income (Baena-Diez et al. Citation2020). Abedi et al. (Citation2021) looked at the seven states in the US with the highest lab-confirmed infection rates as of 9 April 2020 and found that counties with higher income and education levels experienced higher risks of infection, but counties with higher poverty rates had higher death rates, potentially due to lower levels of mobility or issues with comorbidities or access to care. However, analyses of the five boroughs of New York City have suggested that ‘hospital beds per capita’ is not sufficient for explaining socio-economic-related disparities in pandemic outcomes. Wadhera et al. (Citation2020) noted that Manhattan was the most affluent and the Bronx contained the highest proportions of minorities and people living in poverty and the lowest levels of education. Hospitalizations and deaths per 100,000 population were highest in the Bronx and lowest in Manhattan despite both boroughs ranking most highly for number of hospital beds per capita (Wadhera et al. Citation2020).
Higher risks of death are associated with higher deprivation or poverty, a higher income inequality ratio, and lower incomes (e.g. Hendryx and Luo Citation2020; Lauvrak and Juvet Citation2020; Martins-Filho et al. Citation2020; Public Health England Citation2020; Williamson et al. Citation2020). Lower-SES areas in England also showed a faster rise in the number of lab-confirmed cases and higher peak levels (Liu et al. Citation2020). In Sweden, lower income, lower education level, and being an immigrant from a low- or middle-income country all independently predicted a higher risk of death from Covid-19 (Drefahl et al. Citation2020). Gradients were observed for both men and women when analysing education levels, but only for men when analysing income levels. Among immigrants in the sample, mortality was approximately 2.5 times higher for men and 1.5 times higher for women vs Swedish-born cases. Although immigrants from high-income countries also showed higher mortality, it was much lower than for other immigrants, at only 10 per cent and 20 per cent higher for women and men, respectively, than for Swedish-born cases (Drefahl et al. Citation2020). Similarly, Calderón-Larrañaga et al. (Citation2020) compared excess mortality for subdivisions of the Stockholm region and found that the highest levels were recorded in areas with the lowest levels of income and education and lowest shares of Swedish-born and gainfully employed residents. Also in Stockholm, Rostila et al. (Citation2020) reported large disparities in mortality by country of birth, which were only partially explained by socio-economic and living conditions. Further, in a summary of seven studies, Lauvrak and Juvet (Citation2020) noted evidence suggesting higher risk of infection or disease for people in prison and those who were homeless and living in shelters.
Race and ethnicity
1918 influenza pandemic
Due to long-term systemic factors including racism, SES tends to correlate with racial and ethnic identification, and health disparities among social categories of race likely reflect these factors, although not always in straightforward ways. Although the poorest parts of populations tended to suffer the most from 1918 pandemic morbidity and mortality, Crosby (Citation1976, Citation2003) noted that this norm changed during the 1918 influenza pandemic in the US. The Black population (with expected worse pandemic outcomes) experienced lower morbidity and mortality than the White population during the autumn of 1918. Crosby proposed that Black people might have been more exposed to a mild spring/summer wave of influenza earlier that same year, thus gaining immunity. Økland and Mamelund (Citation2019) reviewed the literature from the 1918 pandemic to better understand this observed crossover in the role of race on mortality in the US. Results from this review showed that the Black population experienced lower morbidity and mortality per 1,000 population but higher case fatality than the White population. The results also showed that influenza morbidity in the Black population was lower than for the White population prior to 1918. The reasons for this lower morbidity both prior to 1918 and during the herald and later waves in 1918 remain unclear. These results may imply that Black people’s risk of developing the disease given exposure was lower, but when they did get sick, their risk of dying was higher.
Indigenous populations in North America and Oceania were uniquely at risk for severe disease and death in the 1918 pandemic (as well as during the 2009 H1N1 pandemic) (Herda Citation2000; Crosby Citation2003; Castrodale et al. Citation2009; Kelly et al. Citation2009; La Ruche et al. Citation2009; Flint et al. Citation2010; Mamelund Citation2011; Trauer et al. Citation2011; Wilson et al. Citation2012; Mamelund et al. Citation2013; Groom et al. Citation2014). For example, in the 1918 pandemic the mortality risks of the Indigenous Māori of New Zealand and the Sami population in Norway were four to six times and seven times higher, respectively, than those of their non-Indigenous counterparts (Mamelund Citation2003; Rice Citation2018). The reasons for these ethnic disparities are complex and poorly understood, and they represent an area of limited research. Existing genetic, epidemiological, historical, and social science research is also rarely integrated, while research on both influenza in Indigenous populations and influenza preparedness planning for Indigenous people as at-risk groups often focuses on either North America (Groom et al. Citation2009) or Oceania (Horwood et al. Citation2019) independently, adding to the fragmented understanding.
Covid-19 pandemic
Studies have found that testing positive, illness, hospitalization, and death from Covid-19 tend to be higher among Asian, Indigenous, and (in particular) Black people relative to White people in the UK and US (e.g. de Lusignan et al. Citation2020; Gu et al. Citation2020; Price-Haywood et al. Citation2020; Public Health England Citation2020). The observed racial and ethnic differences are not always fully explained by controlling for variables such as income, age, and sex (e.g. Gu et al. Citation2020; Patel et al. Citation2020; Williamson et al. Citation2020). On the other hand, Price-Haywood et al. (Citation2020) found that although 70.6 per cent of the 326 patients who died from Covid-19 in a retrospective cohort from the state of Louisiana (US) were Black, when socio-demographic and clinical characteristics were considered Black race was not independently associated with higher mortality in hospitals. In an analysis of US counties, Figueroa et al. (Citation2021) found that a 10 per cent increase in the Black population resulted in approximately 325 additional cases and 14.5 additional deaths per 100,000 population. The same measures for the Latino population were approximately 294 additional cases and 7.6 additional deaths per 100,000 population. Controlling for SES variables (e.g. average household size; share of the population with less than high school education) attenuated these variables for the Latino population, while the disparities for the Black population persisted.
Nonetheless, most results to date consistently show disproportionate burdens among non-White populations. In the UK for example, workers in essential fields, such as healthcare and social care, experienced higher risks of severe outcomes compared with non-essential workers. Yet, the risk was more than eight times higher for non-White essential workers vs White non-essential workers, whereas the risks for White essential workers were similar to those for non-White non-essential workers (Mutambudzi et al. Citation2020). In a sample from Michigan, Gu et al. (Citation2020) found that non-Hispanic Black patients were more likely to be hospitalized than non-Hispanic White patients (OR 1.72; 95 per cent CI 1.15–2.58). In an analysis of 46 lab-confirmed and six suspected cases in Wales, members of Black, Asian, and Minority Ethnic (BAME) populations represented 35 per cent of intensive care unit admissions and 35 per cent of deaths, although these groups accounted for less than 5 per cent of the population covered by the hospital. The BAME group also lived disproportionately in areas of socio-economic deprivation (72 per cent vs 27 per cent of White cases in the sample) (Baumer et al. Citation2020).
Counties in selected US states with higher percentages of Hispanic, Asian, and Black residents reported higher rates of infection (Abedi et al. Citation2021). Disparities are also associated with segregation, where historical patterns of SES, household composition, and other factors may facilitate transmission (Bertocchi and Dimico Citation2020; Hendryx and Luo Citation2020). For example, Kim and Bostwick (Citation2020) found that 62.8 per cent of the 269 deaths recorded as of 20 April 2020 by the medical examiner’s office in Cook County, Illinois (US) were among African Americans and appeared to be clustered in segregated areas, while Bertocchi and Dimico (Citation2020) found that with 35 per cent of Covid-19 deaths as of 16 June 2020, Black people in Cook County were dying at a rate 1.3 times higher than their share of the population. Similarly, Black people represented 27 per cent of the population in Milwaukee County, Wisconsin, while making up 45 per cent of the confirmed cases as of 8 April 2020. Of the 67 deaths reported for the county, 46 (69 per cent) were Black. Milwaukee is one of the most segregated metropolitan areas in the US, and analyses have indicated that there was twice the percentage of cases in census tracts that are predominantly African American than would be expected with an even distribution across the county (Rast et al. Citation2020). As Yang et al. (Citation2021) have noted, although the relative proportion of racial or ethnic groups within a population is related to residential segregation, the two might be only modestly related and are both empirically and conceptually distinguishable. At the US county level, analyses showed that both of these measures were associated with the number of infections, but the relationship between them enhanced or aggravated disparities for some populations. For example, counties with higher proportions of Black residents consistently showed more cases, regardless of segregation levels. The relationship between segregation and confirmed cases is positive for Asian populations, and the relationship does not vary by the proportion of Asians in the county. In contrast, the difference in the number of cases among counties with different proportions of Hispanic residents grows as residential segregation increases (Yang et al. Citation2021). Similarly, Hendryx and Luo (Citation2020) found that prevalence and death rates were highest for counties with both a high proportion of Black residents and high segregation levels, and the disparities between these and other counties widened over the study period in early April 2020.
Although much work has focused on US and UK contexts, racial or ethnic disparities have also been seen in Brazil, where after age, Pardo (mixed ethnicity) status was the second most important risk factor for mortality among hospitalized patients. Further, particularly in the central-south region, White Brazilians were more likely to be admitted to intensive care units (ICUs), and there were similar proportions of survivors between these two groups when comparing total hospitalizations with deaths after ICU admission. These outcomes potentially reflect inequalities in the level of access to private healthcare resources (Baqui et al. Citation2020).
Finally, Indigenous people have once again seemingly been hard hit, at least as reported by the media. Examples are the Navajo Nation in the US and various Indigenous groups in Brazil and the Amazon (Miller Citation2020; Nagle Citation2020). At the time of writing this paper, few peer-reviewed studies addressing these disparities had been identified. However, a study from New Zealand showed that Covid-19 infection fatality rates were at least 50 per cent higher for Māori and Pacific people than for New Zealanders from European backgrounds. Suggested explanations included poorer baseline health and lower life expectancy, crowded housing, being more likely to work in occupations with higher exposure, and unmet health needs (Steyn et al. Citation2020). Studies for the US also have shown that relative to White people, American Indians and Alaska Natives experience 3.5- and 1.8-times higher risks, respectively, of a lab-confirmed case or a Covid-19 death (Arrazola et al. Citation2020; Hatcher et al. Citation2020). In an analysis of data from the Mexican Ministry of Health, Argoty-Pantoja et al. (Citation2021) found that the case fatality rate was nearly 65 per cent higher among Indigenous than non-Indigenous people, with particularly high rates when considering those treated as outpatients. A systematic review of racial and ethnic disparities highlighted the lag in research on Indigenous populations relative to other groups. Mackey et al. (Citation2021) drew conclusions on infection, hospitalization, mortality, and case fatality rates with moderate to high confidence for Black and Hispanic populations (whose risks are generally higher, except for case fatality rates, than those of non-Hispanic Whites) and low confidence for Asian groups (whose outcomes are typically similar to those of non-Hispanic Whites). However, the lack of research or data for American Indian/Alaska Natives, Pacific Islanders, and other ethnic groups resulted in a low-confidence conclusion of higher mortality and were insufficient to draw any conclusions for the other outcomes.
Discussion
The literature on both pandemics has focused mostly on calculating rates and documenting disparities but less on possible mechanisms for the social disparities in pandemic outcomes. One reason for the descriptive approaches in the early studies on the 1918 influenza may be that these studies were mainly carried out by social and oral historians who had not collected individual-level data and had no tradition of explanatory statistical modelling (Crosby Citation1976; Phillips Citation1984; Rice Citation1988; Tomkins Citation1992; Van Hartesveldt Citation1992; Crosby Citation2003; Zylberman Citation2003; Beiner Citation2006). But why did these early studies insist that influenza was a socially neutral disease? Common arguments included: (1) ‘it attacked both rich and poor … ’ (Beiner Citation2006, p. 4), as it spread fast to large parts of the population because few had gained immunity; (2) young adults, many without known risk factors, were hardest hit in terms of both morbidity and mortality; and (3) the King of Spain, the Spanish prime minister, and several Spanish members of parliament were laid low; the famous painter Edvard Munch was infected and barely survived; and, in Sweden, Prince Erik even died at only 29 years old.
Studies published after 2005 using more sophisticated data and regression models showed that morbidity and mortality were not socially neutral (Mamelund Citation2006, Citation2018; Murray et al. Citation2007; Grantz et al. Citation2016; Bengtsson et al. Citation2018), but even these studies did not have data that sufficiently explain the mechanisms for the estimated social disparities, and they did not control for medical risk factors. Many of the studies on Covid-19 also lack a conceptual or theoretical approach to explain the social disparities. One reason might be that the studies on Covid-19 have been published mainly in medical journals, where there is less emphasis given to theoretical reasoning and conceptual frameworks explaining the racial or socio-economic differences. Another reason may lie in the urgency of the situation, with Covid-19 resulting in research being done more quickly than normal in 2020 and 2021, and many working papers and preprint papers being disseminated with the aim of quickly guiding policies during the outbreak. Our review of the literature on Covid-19 represents the current knowledge at the time of writing regarding an ongoing pandemic, so it is not exhaustive and is subject to change as more information becomes available. Further, findings and discussions of results in preprint manuscripts may change as they are finalized into peer-reviewed versions. Nonetheless, the literature reviewed in this paper for both pandemics underlines the value of applying conceptual frameworks for understanding disparities. In the following sections, we briefly discuss several frameworks that would help guide the shift in paradigm we then propose.
Frameworks for understanding disparities in pandemic outcomes
The ‘social determinants of health’ framework is one of the most commonly used to study disparities in both chronic and acute health conditions. Taking a policy-oriented and typically a structural- or institutional-level approach, this body of research explores how the conditions in which people work and live influence socio-economic gradients in health, with particular emphasis on, for example, education, employment, the physical and built environment, and healthcare (e.g. Marmot Citation2005; Raphael Citation2006; Marmot and Bell Citation2009; Bambra et al. Citation2010). Consideration of these determinants provides context as well as potential guidance for data collection. However, some authors have noted, specifically in discussion regarding Covid-19, that the relationships between different variables and poor health are not always clear and that mechanisms or pathways need to be understood better in order to translate policy goals successfully into practices that can address immediate needs (Abrams and Szefler Citation2020; Alberti et al. Citation2020; Burstrom and Tao Citation2020; Okoi and Bwawa Citation2020). Separating distal (social and policy) and proximal (behavioural and biological) risk factors could help to uncover and explain unequal levels of morbidity and mortality during pandemics. A framework which may be useful for future research is the one developed by Crouse and Supriya (Citation2014); this analyses possible causes of inequalities, related to healthcare and treatment, that lead to differential exposure, susceptibility, and consequences after the disease has developed, all of which subsequently result in disparities in pandemic outcomes ().
Figure 1 Framework for risk factors leading to unequal pandemic outcomes
Note: The circled numbers indicate pathways 1–3.
Source: Adapted from Crouse and Supriya (Citation2014).
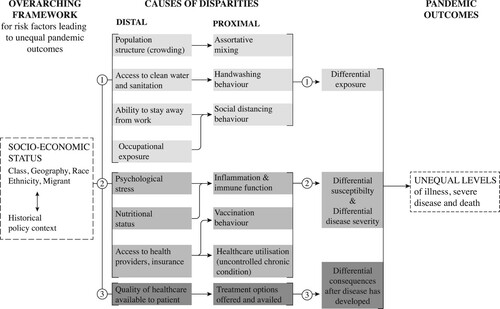
Let us explain the framework by applying it to some of the prior literature. First, SES differences in crowding and assortative mixing, occupational exposure, ability to engage in social distancing behaviour, access to water (distal), and hand hygiene behaviour (proximal) are plausible mechanisms for differential exposure (pathway 1) leading to higher morbidity for the poor during the 1918 pandemic (Mamelund Citation2018). Multigenerational living increases exposure risks, and older people living with people active in the labour market experienced higher risks of dying in Sweden during the first wave of Covid-19 (Brandén et al. Citation2020). Occupational exposure matters too. A study for England showed that the risk of severe Covid-19 was higher among healthcare workers, social and education workers, transport workers, and other essential workers relative to non-essential workers (Mutambudzi et al. Citation2020). Another study found that inability to work from home, lack of paid sick leave, and income were associated with working adults’ ability to comply with influenza mitigation measures during a potentially serious influenza outbreak (Blake et al. Citation2010). In Norway, survey data collected in March and April 2020 showed that SES, as measured by income, was a significant predictor of more handwashing, keeping a 1-metre distance from others, more use of home office facilities, and less use of public transportation in a private and work context during the early spread of the Covid-19 pandemic (Mamelund et al. Citation2021). Similarly, Zelner et al. (Citation2021) concluded that most of the disparity in Covid-19 mortality between Black and White members of a sample from Michigan was likely driven by greater infection rates from household, community, and work exposure than by variation in age-specific case fatality rates.
Second, studies of various pathogens have found greater infection rates among those of low SES compared with those of high SES (Steptoe et al. Citation2007; Semenza Citation2010; Stone et al. Citation2010), although it is difficult to determine the extent to which this is due to differential exposure or medical susceptibility. Support has emerged for the latter pathway, that is pathway 2 in : individuals of low SES may have impaired immune function due to nutritional or psychological stress, increasing their susceptibility of developing influenza (given exposure) and their likelihood of experiencing complications. A series of studies found that adults with lower SES were more likely to develop the common cold and influenza after being experimentally exposed (Cohen et al. Citation2004, Citation2008). Medical risks groups for severe influenza or Covid-19 are not homogenous biological entities, but are patterned by SES. For example, a Norwegian study showed that older age, lower education, and a weaker connection to work life (such as being on disability pension) were associated with higher risks of belonging to the medical risk group for severe influenza (Klüwer et al. Citationunder review). Effective vaccines or antiviral medications did not exist in 1918, and this was also the case for Covid-19 before the turn of the year 2020–21. However, issues include to what extent the vaccines will become available for low-income countries and whether social risk groups will be prioritized in addition to medical risk groups. An individual with higher SES may have stronger intentions to be vaccinated, perhaps due to greater health literacy or a more positive attitude toward healthcare providers (Howard et al. Citation2006; Maurer Citation2016). High SES also implies access to money, knowledge, and power, all of which likely impact actual vaccination uptake (Phelan et al. Citation2010). This would in turn lead to disparities in pandemic outcomes (pathway 2). An important field of research will be the impact of SES on Covid-19 vaccine uptake.
Finally, research has shown that the quality of healthcare and treatment options offered and availed of differ by social background (Fiscella et al. Citation2000), and this would translate into social disparities after the disease has developed (pathway 3). The three pathways of this framework could also be applied to racial disparities observed with Covid-19, as potential explanations include a higher prevalence of minority employees in essential services or occupations with more exposure and close proximity to others, reduced access to care, pre-existing health conditions, family size, multigenerational living situations, foreign-born or immigrant status, education level, public health awareness, and neighbourhood characteristics (see, for example, discussion in Abedi et al. Citation2021; Drefahl et al. Citation2020; Hawkins Citation2020).
The framework described in is suitable for explaining the mechanisms leading to social inequalities in pandemic outcomes in historical as well as contemporary pandemics, and in both high- and low-income countries. However, this approach is data-demanding, and access to high-quality linked data from hospital registers, administrative sources, and surveys may be better in contemporary and high-income settings. This has been clearly demonstrated by a systematic review and meta-analysis on the associations between SES and influenza pandemic outcomes (Mamelund et al. Citation2020). Out of 44 identified studies (nine from the 1918 influenza, 35 from the 2009 pandemic), almost all used data from high-income settings, few used data from Asia and South America, and none used data from Africa. As we discuss later, a broader paradigm shift is needed to address data and methodological concerns, as well as other challenges raised by transdisciplinary approaches to pandemic preparedness today and in the post-Covid-19 future.
Biomedical pandemic preparedness in the twentieth century
The 1918 influenza pandemic showed that most countries were ill-prepared for a devastating pandemic. Pandemic preparedness plans were therefore called for, but these calls and potential drafts of such plans may have been put away and forgotten—just as the 1918 pandemic was coined the ‘forgotten pandemic’ by Crosby (Citation2003). National pandemic influenza preparedness plans were therefore not in place when the H2N2 Asian influenza pandemic of 1957–58 and the H3N2 ‘Hong Kong flu’ pandemic of 1968–70 hit the world. The outbreak of H5N1 ‘bird flu’ in Hong Kong in 1997, where 18 were infected and six died, was a wake-up call. The fact that it had been 40 years since the previous pandemic and the fear that a highly lethal bird flu could cause the next big pandemic led to a call from the WHO in the late 1990s for each member country to make national pandemic influenza preparedness plans (Mamelund Citation2008). Additionally, the increased awareness that a new pandemic could occur any time also sparked renewed attention on medical, historical, and demographic studies of the 1918 influenza, in what has been labelled the second wave of this pandemic’s historiography (Phillips Citation2014). When the anticipated new pandemic came in 2009, it was caused by an H1N1 influenza strain and not H5N1, but for the first time in history, pandemic preparedness plans were in place in several countries, at least high-income ones.
A 2017 review of pandemic preparedness plans documented that social inequalities were not taken into account in such plans for the WHO, the European Union and its 28 member countries, Iceland, Norway, Switzerland, Turkey, Macedonia, the US, Canada, or Australia (Mamelund Citation2017). Risk groups were only medically defined, and socially defined risk groups were not mentioned in recommendations for vaccination or as something to be concerned about when thinking about the ability to comply with non-pharmaceutical measures. This absence or neglect of the social lessons from influenza was surprising in view of:
the critique from the social justice literature on pandemics of the lack of focus on social vulnerability, which was raised prior to the 2009 pandemic and many years before the Covid-19 pandemic (Kayman and Ablorh-Odjidja Citation2006; Uscher-Pines et al. Citation2007; Lee et al. Citation2008). Although some countries reviewed and revised their influenza pandemic plans after 2009, plans were not explicitly updated to include issues of social justice (Mamelund Citation2017);
the large social disparities in mortality in both the 1918 and 2009 pandemics;
rising income/wealth disparities (Piketty Citation2014); and
the United Nations (UN) Sustainable Development Goals (SDGs) of eradicating poverty, ensuring good health for all, and reducing inequalities by 2030.
Several reasons for the exclusion of social inequalities are plausible. For example, the ‘master status’ of biomedicine might distract political attention from the social lessons of influenza (Barrett Citation2006). The belief that influenza is socially neutral outside medically defined risk groups might persist. Perhaps public health research and pandemic planning in high-income countries tend to focus on those causes of death that take the most lives in modern, late-stage demographic and epidemiological transition societies (including non-communicable diseases such as cardiovascular diseases and cancer) at the expense of the infectious diseases more prevalent in low-income countries and pre/early transition societies. Similarly, prior to Covid-19 there might have been misperceptions that large pandemics belonged to history or low-income countries only. Perhaps the modern ‘just-in-time’ economy also prevents nations from building up preparedness (e.g. stockpiling large amounts of protective equipment or increasing capacity of intensive care units) for the ‘next big pandemic’ that might be thought of as improbable. It may also be quite normal for people not to comprehend worst-case scenarios for a pandemic.
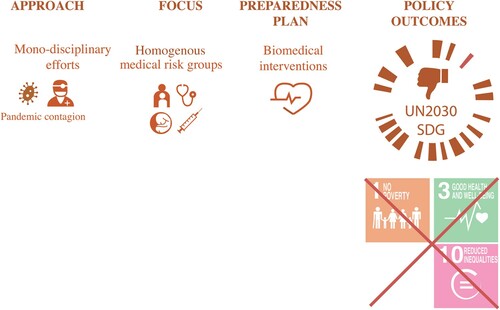
Further, the disciplinary or training backgrounds of those writing the preparedness plans likely matter. Just before the Covid-19 outbreak, out of the 22 people on the Epidemic and Pandemic committee in Norway, none had a background in social sciences and humanities (Folkehelseinstituttet Citation2018). A Guardian newspaper article revealed that the advisory group in the UK during Covid-19 in 2020 also contained few with such backgrounds (Sample Citation2020). A study also showed that of 115 Covid-19 response groups in 87 countries, only 3.5 per cent were gender balanced, while 85.2 per cent were male dominated (van Daalen et al. Citation2020). One of the features of the current paradigm () is that most of those who work on pandemic preparedness in national or international institutions of public health—such as the European Centre for Disease Prevention and Control, the US Centers for Disease Control and Prevention, and the WHO—are general practitioners or infection control officers with backgrounds in medicine, life sciences, biology, immunology, or vaccinology. The approaches in the preparedness plans are therefore mono-disciplinary with a focus on the pandemic contagion (the virus, mode of transmission, symptoms, immunology, etc.) as opposed to the pandemic configuration (historical context, events occurring at the same time, social structures, and social disparities) (Rosenberg Citation1992; Holmberg Citation2016; Mamelund Citation2017). The focus in the plans is on medical risk groups, such as those who are older (aged 65+), are pregnant, or have specific underlying health problems (e.g. chronic respiratory disease, chronic cardiovascular disease, liver or renal failure, chronic neurological disease or injury, diabetes mellitus, or severe obesity). In the plans, these medical risk groups are typically treated as homogenous biological entities; that is, everyone with the same medical conditions is equal across space and SES. The statistical models in the plans study the impact of prior immunity, non-pharmaceutical interventions (handwashing or mask use, environmental cleaning, social distancing, or travel restrictions), and pharmaceutical interventions (antiviral medications and vaccines) on pandemic outcomes without studying the potential social disparities in the outcomes. This mono-disciplinary medical focus leaves out potentially important preparedness lessons from other disciplines, such as the humanities and the social sciences. Models that do not focus on socio-economic vulnerability in addition to medical risk factors do not give the whole picture and would therefore have less potential for reducing pandemic outcomes and supporting the UN SDGs of eradicating poverty, ensuring good health for all, and reducing inequalities.
A transdisciplinary pandemic preparedness for the twenty-first century
We suggest that a paradigm shift in pandemic preparedness and thinking is necessary (). As part of such an initiative, infectious disease researchers and pandemic groups at international and national health institutions should collaborate with or recruit historians, demographers, and others in the social sciences and humanities who study pandemic issues. In other words, transdisciplinary pandemic preparedness plans are needed, with collaborative teams of people evaluating whether and how to recommend, impose, and lift public health interventions. An example of this approach can be seen with the German government, which unlike those of most other countries, has involved philosophers, historians, theologians, and jurists together with medical scientists in advising strategies for loosening the restrictions implemented during the Covid-19 pandemic (Matthews, Citation2020). Clearly, economists have important skills in evaluating the economic impacts of lockdowns and the costs and benefits of the pandemic burden vis-à-vis the burden of non-pharmaceutical interventions. Psychologists and psychiatrists are needed to evaluate the (combined) burden of the disease, unemployment, loneliness, and other factors on mental health, including suicide intentions and risks. Pedagogists are needed to evaluate the impact of homeschooling on students during lockdowns and are also important voices in decisions on when to close and open schools and how long schools should be closed for when the disease burden is high. Philosophers and ethicists bring important skills and insights for evaluating priorities related to (non-) pharmaceutical interventions and allocation of limited resources. Jurists are clearly needed as governments have made various regulations and laws in response to the Covid-19 pandemic. All of these disciplines are under-represented among pandemic planners, even though people with these varied backgrounds should play key roles in navigating the delicate balance of health, economics, equity, and freedom during pandemics. Further, because the poorest sections of societies, Indigenous people, immigrants, Black people, and other marginalized groups are clearly hardest affected by pandemics, non-academic stakeholders representing these groups should also work with public health planners to guide public health work during pandemics and also to guide revisions of pandemic preparedness plans. Social justice, gender, or other diversity perspectives in pandemic preparedness might be missed when those who write preparedness plans and are part of real-time pandemic response groups are dominated by men, non-disabled people, people of majority race or ethnic backgrounds, people of higher SES, and/or people from medical and life sciences backgrounds.
Figure 3 Approach and focus after a paradigm shift in pandemic preparedness plans and thinking
Source: As for .

Further, in order to conduct high-quality epidemiological research on the 1918 influenza or Covid-19 pandemics, or to use data from 1918 as a worst-case scenario for pandemic preparedness modelling, it is not enough just to have a good understanding of the virus, immunity, and virulence. Researchers also need to be aware of the historical context in which data were collected and produced, and to take into account how the events of the time might have affected pandemic outcomes. For example, the First World War might have affected the outcomes of the 1918 pandemic via increased exposure (movement of troops and displaced people), susceptibility (poorer nutrition), and reduced access to healthcare (in belligerent nations, most of the nurses and doctors were at the front, leaving the civilian population with poorer healthcare). For these reasons pandemic historians should also play a larger role in pandemic preparedness and planning.
A transdisciplinary paradigm would also recognize that individuals belonging to a medical risk group are not homogenous but heterogeneous (Klüwer et al. Citationunder review). Variation in prevalence of medical risk factors and co-/multi-morbidities, as well as how conditions intersect with sex, SES, and other social factors, must be considered. The chances of a pregnant woman or a man with a heart disease living in a low-income country surviving a pandemic infection are most likely lower than those of their counterparts living in high-income countries. Results from a systematic review also show that social factors explain variation in pandemic outcomes in 1918 and 2009 independent of medical risk factors (Mamelund et al. Citation2020), mirroring a study of Covid-19 documenting independent impacts of poverty, medical risk factors, and immigrant status (Williamson et al. Citation2020).
These findings indicate that recommendations for seasonal influenza vaccination and current and future pandemic preparedness should reflect patterns of social disparities in exposure and access to care, independent of chronic disease status (Blumenshine et al. Citation2008). Health authorities in most countries currently translate the international biomedical recommendations for seasonal influenza, Covid-19, and future pandemic vaccination schemes into their own national contexts. The social conditions for recommending vaccination also need to be investigated and determined nationally. For example, recommendations might be that vaccines during seasonal influenza and pandemics should be free and securely distributed to medical and social risk groups, to designated poverty areas in high-income countries, and to low-income countries. Prioritization of vaccines based on social indications such as living conditions, social determinants of health, immigrant status, or ethnicity should be framed in such a way to avoid stigmatization.
However, while a culture change is needed, it is likely to take time to adjust before a new pandemic or even during a pandemic. In Norway, it took some time before Covid-related information was published in several languages, four months (February to June 2020) before the risk management plans of the Norwegian Institute of Public Health included social vulnerability in addition to medical vulnerability, and nine months before comprehensive reports on the vulnerability of immigrants were published and a government-appointed group developed advice for lowering the pandemic outcome risks among immigrants (Folkehelseinstituttet Citation2020a, Citation2020b, Citation2020c; Indseth et al. Citation2020, Citation2021). Vaccines in Norway were first distributed to municipalities according to their share of population over 65 years, but during the spring of 2021, after most older people and those with the most severe comorbidities had been vaccinated, the government decided to give more vaccines to the areas most affected, including Oslo, in particular the eastern low-SES parishes and other surrounding cities. In addition, vaccines were distributed according to municipal population size rather than the share of the population over 65 years. This change in policy, including the geographical indication for distributing vaccines, indirectly protected the heavily affected eastern parts of Oslo with high shares of immigrants. But a better and more direct approach to address both social and medical vulnerabilities would have been to distribute the vaccines to municipalities at the very beginning based on social determinants of health indicators, in addition to comorbidity diagnosis and age profile.
As low-SES groups may hold less positive attitudes towards governments and their advice (Howard et al. Citation2006; Blake et al. Citation2010; Phelan et al. Citation2010; Maurer Citation2016), attitudinal campaigns might be useful. Fighting vaccine hesitancy, fake news, and conspiracy theories is important. In a paradigm shift, the influenza models in preparedness plans should also study anticipated social consequences of the policies. For example, a low-income single mother with no paid sick leave who will lose her job if she is unable to go to work will not be able to comply with the recommendation to stay at home with her children during a school closure. In addition to potential socio-economic consequences, this situation will also put her more at risk of contracting and spreading pandemic influenza and thus increase existing inequalities (Blake et al. Citation2010).
Further, transdisciplinary preparedness groups and plans will potentially give more robust and informed recommendations to reduce social inequalities, save lives, and reduce economic and social losses during pandemics and thus will also be more in line with the UN SDGs. Moreover, pandemic preparedness is or should be about ensuring fewer social disparities in health, wealth, and access to health information and healthcare before a pandemic occurs. As previous research has shown, cities with high pre-pandemic disparities also reported large disparities during the 1918 pandemic (Mamelund Citation2006; Grantz et al. Citation2016).
Social scientists are likely to contribute meaningfully to these and other aspects of pandemic preparedness, and there is a need for more research on the short- and long-term demographic and economic consequences of past pandemics and the related public health responses. Therefore, this might be the ideal time for demography departments to build up their research and teaching competencies in historical demography and pandemics, for history departments to develop and enhance skills in quantitative methods, and for these departments and related fields (e.g. economics) to pursue interdisciplinary collaborations and cross-cutting curricula on pandemic-related topics.
Summary
The myth that infectious disease pandemics, such as the 1918 influenza pandemic and Covid-19, are socially neutral is deeply rooted and persistent among the public, in popular literature, and even in academic literature and pandemic preparedness plans. We have shown that although the Covid-19 pandemic in 2020 might initially have been a ‘rich person’s virus’, with wealthy people on vacation contracting the infection first in some areas, the disease quickly turned into a ‘poor person’s disease’. The same pattern was observed in 1918. Although the rich and famous were infected as well as the poor, there were clear social disparities in pandemic outcomes. Therefore, pandemic preparedness needs to be readjusted to focus on reducing social inequalities in wealth and health before the next pandemic, while pandemic preparedness plans, prioritizing of vaccines, routine monitoring, and reporting of the impact of pandemics must all explicitly address social justice and equity (Schmidt et al. Citation2020).
Notes
1 Svenn-Erik Mamelund and Jessica Dimka are based at the Centre for Research on Pandemics & Society, Oslo Metropolitan University.
2 Please direct all correspondence to Svenn-Erik Mamelund, Centre for Research on Pandemics & Society, Oslo Metropolitan University, PO Box 4, St. Olavs Plass, 0130 Oslo, Norway; or by Email: [email protected]
3 This paper was written from research funded by two Research Council of Norway grants: (1) CorRisk—Early Covid-19 wave in Norway: Social inequality in morbidity, compliance to non-pharmaceutical interventions and labour market consequences (grant number 312716); and (2) PANRISK—Socio-economic risk groups, vaccination and pandemic influenza (grant number 302336).
References
- Abedi, V., O. Olulana, V. Avula, D. Chaudhary, A. Khan, S. Shahjouei, J. Li et al. 2021. Racial, economic, and health inequality and COVID-19 infection in the United States, Journal of Racial and Ethnic Health Disparities 8: 732–742. doi:https://doi.org/10.1007/s40615-020-00833-4
- Abrams, E. M. and S. J. Szefler. 2020. COVID-19 and the impact of social determinants of health, The Lancet Respiratory Medicine 8(7): 659–661. doi:https://doi.org/10.1016/s2213-2600(20)30234–4
- Alberti, P. M., P. M. Lantz, and C. H. Wilkins. 2020. Equitable pandemic preparedness and rapid response: Lessons from COVID-19 for pandemic health equity, Journal of Health Politics, Policy and Law 45(6): 921–935. doi:https://doi.org/10.1215/03616878-8641469
- Alfani, G. and M. Bonetti. 2019. A survival analysis of the last great European plagues: The case of Nonantola (Northern Italy) in 1630, Population Studies 73(1): 101–118. doi:https://doi.org/10.1080/00324728.2018.1457794
- Argoty-Pantoja, A. D., K. Robles-Rivera, B. Rivera-Paredez, and J. Salmeron. 2021. COVID-19 fatality in Mexico’s indigenous populations, Public Health 193: 69–75. doi:https://doi.org/10.1016/j.puhe.2021.01.023
- Arrazola, J., M. Masiello, S. Joshi et al. 2020. COVID-19 mortality among American Indian and Alaska Native persons—14 states, January–June 2020, MMWR. Morbidity and Mortality Weekly Report 69: 1853–1856. doi:https://doi.org/10.15585/mmwr.mm6949a3
- Baena-Diez, J. M., M. Barroso, S. I. Cordeiro-Coelho, J. L. Diaz, and M. Grau. 2020. Impact of COVID-19 outbreak by income: Hitting hardest the most deprived, Journal of Public Health 42(4): 698–703. doi:https://doi.org/10.1093/pubmed/fdaa136
- Bambra, C., M. Gibson, A. Sowden, K. Wright, M. Whitehead, and M. Petticrew. 2010. Tackling the wider social determinants of health and health inequalities: Evidence from systematic reviews, Journal of Epidemiology & Community Health 64(4): 284–291. doi:https://doi.org/10.1136/jech.2008.082743
- Baqui, P., I. Bica, V. Marra, A. Ercole, and M. van der Schaar. 2020. Ethnic and regional variations in hospital mortality from COVID-19 in Brazil: A cross-sectional observational study, The Lancet Global Health 8(8): e1018–e1026. doi:https://doi.org/10.1016/s2214-109x(20)30285-0
- Barrett, R. 2006. Dark winter and the spring of 1972: Deflecting the social lessons of smallpox, Medical Anthropology 25(2): 171–191. doi:https://doi.org/10.1080/01459740600686633
- Barry, J. M. 2005. The Great Influenza: The Story of the Deadliest Pandemic in History. London: Penguin Books.
- Batty, G. D., I. J. Deary, M. Luciano, D. M. Altschul, M. Kivimäki, and C. R. Gale. 2020. Psychosocial factors and hospitalisations for COVID-19: Prospective cohort study based on a community sample, Brain, Behavior, and Immunity 89: 569–578. doi:https://doi.org/10.1016/j.bbi.2020.06.021
- Baumer, T., E. Phillips, A. Dhadda, and T. Szakmany. 2020. Epidemiology of the first wave of COVID-19 ICU admissions in South Wales – The interplay between ethnicity and deprivation, Frontiers in Medicine 7: 569714. doi:https://doi.org/10.3389/fmed.2020.569714
- Beach, B., K. Clay, and M. H. Saavedra. 2020. The 1918 influenza pandemic and its lessons for COVID-19. NBER Working Paper Series, Issue. National Bureau of Economic Research.
- Beiner, G. 2006. Out in the cold and back: New-found interest in the great flu, Cultural and Social History 3(4): 496–505. doi:https://doi.org/10.1191/1478003806cs070ra
- Bengtsson, T., M. Dribe, and B. Eriksson. 2018. Social class and excess mortality in Sweden during the 1918 influenza pandemic, American Journal of Epidemiology 187(12): 2568–2576. doi:https://doi.org/10.1093/aje/kwy151
- Bertocchi, G. and A. Dimico. 2020. COVID-19, race and redlining. QUCEH Working Paper Series, Issue. Queen’s University Belfast, Queen’s University Centre for Economic History (QUCEH).
- Blake, K. D., R. J. Blendon, and K. Viswanath. 2010. Employment and compliance with pandemic influenza mitigation recommendations, Emerging Infectious Diseases 16(2): 212–218. doi:https://doi.org/10.3201/eid1602.090638
- Blumenshine, P., A. Reingold, S. Egerter, R. Mockenhaupt, P. Braveman, and J. Marks. 2008. Pandemic influenza planning in the United States from a health disparities perspective, Emerging Infectious Diseases 14(5): 709–715. doi:https://doi.org/10.3201/eid1405.071301
- Brandén, M., S. Aradhya, M. Kolk, J. Härkönen, S. Drefahl, B. Malmberg, M. Rostila et al. 2020. Residential context and COVID-19 mortality among adults aged 70 years and older in Stockholm: A population-based, observational study using individual-level data, The Lancet Healthy Longevity 1(2): e80–e88. doi:https://doi.org/10.1016/S2666-7568(20)30016-7
- Burstrom, B. and W. Tao. 2020. Social determinants of health and inequalities in COVID-19, European Journal of Public Health 30(4): 617–618. doi:https://doi.org/10.1093/eurpub/ckaa095
- Calderón-Larrañaga, A., D. L. Vetrano, D. Rizzuto, T. Bellander, L. Fratiglioni, and S. Dekhtyar. 2020. High excess mortality in areas with young and socially vulnerable populations during the COVID-19 outbreak in Stockholm region, Sweden, BMJ Global Health 5: e003595. doi:https://doi.org/10.1136/bmjgh-2020-003595
- Castrodale, L., J. McLaughlin, S. Imholte, K. Komatsu, E. Wells, M. Landen, D. Selvage et al. 2009. Deaths related to 2009 pandemic influenza A (H1N1) among American Indian/Alaska Natives – 12 states, 2009, MMWR: Morbidity and Mortality Weekly Report 58(48): 1341–1344. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5848a1.htm
- Chandra, S. 2013. Mortality from the influenza pandemic of 1918–19 in Indonesia, Population Studies 67(2): 185–193. doi:https://doi.org/10.1080/00324728.2012.754486
- Chandra, S., J. Chistensen, S.-E. Mamelund, and N. Paneth. 2018. Short-term birth sequelae of the 1918–20 influenza pandemic in the United States: State-level analysis, American Journal of Epidemiology 187(12): 2585–2595. doi:https://doi.org/10.1093/aje/kwy153
- Cohen, S., C. M. Alper, W. J. Doyle, N. Adler, J. J. Treanor, R. B. Turner et al. 2008. Objective and subjective socioeconomic status and susceptibility to the common cold, Health Psychology 27: 268–274. doi:https://doi.org/10.1037/0278-6133.27.2.268
- Cohen, S., W. J. Doyle, R. B. Turner, C. M. Alper, and D. P. Skoner. 2004. Childhood socioeconomic status and host resistance to infectious illness in adulthood, Psychosomatic Medicine 66(4): 553–558. doi:https://doi.org/10.1097/01.psy.0000126200.05189.d3
- Crosby, A. 1976. Epidemic and Peace, 1918. London: Greenwood Press.
- Crosby, A. W. 2003. America’s Forgotten Pandemic: The Influenza of 1918. Cambridge: Cambridge University Press.
- Crouse, Q. S., and K. Supriya. 2014. Health inequalities and infectious disease epidemics: A challenge for global health security, Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science 12(5): 263–273. doi:https://doi.org/10.1089/bsp.2014.0032
- Dahal, S., K. Mizumoto, R. Rothenberg, and G. Chowell. 2020. Investigating spatial variability in COVID-19 pandemic severity across 19 geographic areas, Spain, 2020, medRxiv. doi:https://doi.org/10.1101/2020.04.14.20065524
- de Lusignan, S., J. Dorward, A. Correa, N. Jones, O. Akinyemi, G. Amirthalingam, N. Andrews et al. 2020. Association of age, gender, deprivation, urbanicity, ethnicity, and smoking with a positive test for COVID-19 in an English primary care surveillance network: Cross sectional study of the first 500 cases, SSRN Electronic Journal. doi:https://doi.org/10.2139/ssrn.3578782
- Dimka, J., and S.-E. Mamelund. 2020. 1918 influenza outcomes among institutionalized Norwegian populations: Implications for disability-inclusive pandemic preparedness, Scandinavian Journal of Disability Research 22(1): 175–186. doi:https://doi.org/10.16993/sjdr.725
- Drefahl, S., M. Wallace, E. Mussino, S. Aradhya, M. Kolk, M. Brandén, B. Malmberg et al. 2020. A population-based cohort study of socio-demographic risk factors for COVID-19 deaths in Sweden, Nature Communications 11(1): 5097. doi:https://doi.org/10.1038/s41467-020-18926-3
- Euromomo. 2021. Available: https://www.euromomo.eu/.
- Figueroa, J. F., R. K. Wadhera, W. T. Mehtsun, K. Riley, J. Phelan, and A. K. Jha. 2021. Association of race, ethnicity, and community-level factors with COVID-19 cases and deaths across U.S. counties, Healthcare 9(1): 100495. doi:https://doi.org/10.1016/j.hjdsi.2020.100495
- Fiscella, K., P. Franks, M. R. Gold, and C. M. Clancy. 2000. Inequality in quality, JAMA 283(19): 2579–2584. doi:https://doi.org/10.1001/jama.283.19.2579
- Flint, S. M., J. S. Davis, J.-Y. Su, E. P. Oliver-Landry, B. A. Rogers, A. Goldstein, J. H. Thomas et al. 2010. Disproportionate impact of pandemic (H1N1) 2009 influenza on indigenous people in the top end of Australia’s northern territory, Medical Journal of Australia 192(10): 617–622. doi:https://doi.org/10.5694/j.1326-5377.2010.tb03654.x
- Folkehelseinstituttet [Norwegian National Institute of Public Health]. 2018. Pandemi- og epidemikomitéen [The Pandemic and Epidemic Committee]. Available: https://www.fhi.no/sv/influensa/influensapandemier/pandemi--og-epidemikomiteen/.
- Folkehelseinstituttet [Norwegian National Institute of Public Health]. 2020a. COVID-19-epidemien: Risikovurderinger [COVID-19 epidemic: Risk assessments]. Available: https://www.fhi.no/publ/2020/covid-19-epidemien-risikovurdering/.
- Folkehelseinstituttet [Norwegian National Institute of Public Health]. 2020b. Kunnskap, situasjon, prognose, risiko og respons i Norge etter uke 23 [Knowledge, situation, prognosis, risk, and response in Norway after week 23]. Available: https://www.fhi.no/contentassets/c9e459cd7cc24991810a0d28d7803bd0/vedlegg/notat-om-risiko-og-respons-2020–06–11.pdf.
- Folkehelseinstituttet [Norwegian National Institute of Public Health]. 2020c. Risikovurdering av og respons på 2019-nCoV-infeksjon i Norge [Risk assessment of and response to 2019-nCoV infection in Norway]. Available: https://www.fhi.no/contentassets/c9e459cd7cc24991810a0d28d7803bd0/vedlegg/risikovurdering-av-og-respons-pa-2019-ncov-infeksjon-i-norge-28.01.2020.pdf.
- Grantz, K. H., D. A. T. Cummings, G. E. Glass, M. S. Rane, H. Salje, and S. E. Schachterle. 2016. Disparities in influenza mortality and transmission related to sociodemographic factors within Chicago in the pandemic of 1918, Proceedings of the National Academy of Sciences 113(48): 13839–13844. doi:https://doi.org/10.1073/pnas.1612838113
- Great Britain Ministry of Health. 1920. Report on the 1918–19 Pandemic of Influenza. Reports on public health and medical subjects, No. 4. GBMH, London.
- Groom, A. V., T. W. Hennessy, R. J. Singleton, J. C. Butler, S. Holve, and J. E. Cheek. 2014. Pneumonia and influenza mortality among American Indian and Alaska Native people, 1990–2009, American Journal of Public Health 104(Suppl 3): S460–S469. doi:https://doi.org/10.2105/AJPH.2013.301740
- Groom, A. V., C. Jim, M. LaRoque, C. Mason, J. McLaughlin, L. Neel, T. Powell et al. 2009. Pandemic influenza preparedness and vulnerable populations in tribal communities, American Journal of Public Health 99(S2): S271–S278. doi:https://doi.org/10.2105/AJPH.2008.157453
- Gu, T., J. A. Mack, M. Salvatore, S. Prabhu Sankar, T. S. Valley, K. Singh, B. K. Nallamothu et al. 2020. Characteristics associated with racial/ethnic disparities in COVID-19 outcomes in an academic health care system, JAMA Network Open 3(10): e2025197. doi:https://doi.org/10.1001/jamanetworkopen.2020.25197
- Guarner, J. 2020. Three emerging coronaviruses in two decades, American Journal of Clinical Pathology 153(4): 420–421. doi:https://doi.org/10.1093/ajcp/aqaa029
- Han, Y., V. O. K. Li, J. C. K. Lam, P. Guo, R. Bai, and W. W. T. Fok. 2020. Who is more susceptible to Covid-19 infection and mortality in the States?, medRxiv. doi:https://doi.org/10.1101/2020.05.01.20087403
- Hatcher, S., C. Agnew-Brune, M. Anderson et al. 2020. COVID-19 among American Indian and Alaska native persons—23 states, January 31–July 3, 2020, MMWR. Morbidity and Mortality Weekly Report 69: 1166–1169. doi:https://doi.org/10.15585/mmwr.mm6934e1
- Hawkins, D. 2020. Differential occupational risk for COVID-19 and other infection exposure according to race and ethnicity, American Journal of Industrial Medicine 63(9): 817–820. doi:https://doi.org/10.1002/ajim.23145
- Hendryx, M. and J. Luo. 2020. COVID-19 prevalence and mortality rates in association with black race and segregation in the United States April 1 to April 15, 2020, SSRN Electronic Journal. doi:https://doi.org/10.2139/ssrn.3582857
- Herda, P. 2000. Disease and the colonial narrative. The 1918 influenza pandemic in Western Polynesia, New Zealand Journal of History 34(1): 133–144. http://www.nzjh.auckland.ac.nz/document/document/?wid=416
- Holmberg, M. 2016. The ghost of pandemics past: Revisiting two centuries of influenza in Sweden, Medical Humanities 43: 141–147. doi:https://doi.org/10.1136/medhum-2016-011023
- Horwood, P. F., A. Tarantola, C. Goarant, M. Matsui, E. Klement, M. Umezaki, S. Navarro et al. 2019. Health challenges of the Pacific region: Insights from history, geography, social determinants, genetics, and the microbiome, Frontiers in Immunology 10: 2184. doi:https://doi.org/10.3389/fimmu.2019.02184
- Howard, D. H., T. Sentell, and J. A. Gazmararian. 2006. Impact of health literacy on socioeconomic and racial differences in health in an elderly population, Journal of General Internal Medicine 21(8): 857–861. doi:https://doi.org/10.1111/j.1525-1497.2006.00530.x
- Indseth, T., I. H. Elgersma, B. H. Strand, K. Telle, A. S. Labberton, T. Arnesen, K. M. Nygård et al. 2021. Covid-19 blant personer født utenfor Norge, justert for yrke, trangboddhet, medisinsk risikogruppe, utdanning og inntekt [Covid-19 among people born outside Norway, adjusted for occupation, overcrowding, medical risk group, education, and income]. Folkehelseinstituttet [Norwegian National Institute of Public Health]. Available: https://www.fhi.no/publ/2021/covid-19-blant-personer-fodt-utenfor-norge-justert-for-yrke-trangboddhet-me/.
- Indseth, T., A. Godøy, M. Kjøllesdal, T. Arnesen, C. Jacobsen, M. Grøsland, and K. Telle. 2020. Covid-19 etter fødeland: Personer testet, bekreftet smittet og relaterte innleggelser og dødsfall [Covid-19 by country of birth: People tested, confirmed infected and related, hospitalizations and deaths]. Folkehelseinstituttet [Norwegian National Institute of Public Health]. Available: https://www.fhi.no/globalassets/dokumenterfiler/rapporter/2020/covid-19-etter-fodeland-personer-testet-bekreftet-smittet-og-relaterte-innleggelser-og-dodsfall-rapport-2020-v2.pdf.
- Iuliano, A. D., K. M. Roguski, H. H. Chang, D. J. Muscatello, R. Palekar, S. Tempia, C. Cohen et al. 2017. Estimates of global seasonal influenza-associated respiratory mortality: A modelling study, The Lancet 391(10127): 1285–1300. doi:https://doi.org/10.1016/S0140-6736(17)33293-2
- Johnson, N. 2006. Britain and the 1918–19 Influenza Pandemic. A Dark Epilogue. Routledge. doi:https://doi.org/10.4324/9780203018163
- Johnson, N. P. and J. Mueller. 2002. Updating the accounts: Global mortality of the 1918–1920 ‘Spanish’ influenza pandemic, Bulletin of the History of Medicine 76(1): 105–115. Available: http://muse.jhu.edu/article/4826. doi:https://doi.org/10.1353/bhm.2002.0022
- Kayman, H. and A. Ablorh-Odjidja. 2006. Revisiting public health preparedness, Journal of Public Health Management and Practice 12(4): 373–380. doi:https://doi.org/10.1097/00124784-200607000-00011
- Kelly H., G. N. Mercer, and A. C. Cheng. 2009. Quantifying the risk of pandemic influenza in pregnancy and indigenous people in Australia in 2009, Euro Surveillance 14(50): 19441. doi:https://doi.org/10.2807/ese.14.50.19441-en
- Kim, S. J. and W. Bostwick. 2020. Social vulnerability and racial inequality in COVID-19 deaths in Chicago, Health Education & Behavior 47(4): 509–513. doi:https://doi.org/10.1177/1090198120929677
- Klüwer, B., K. Rydland, I. Laake, M. Todd, L. Juvet, and S.-E. Mamelund. Under review. Socioeconomic patterns of the influenza risk group in Norway.
- La Ruche, G., A. Tarantola, P. Barboza, L. Vaillant, J. Gueguen, and M. Gastellu-Etchegorry. 2009. The 2009 pandemic H1N1 influenza and indigenous populations of the Americas and the Pacific, Eurosurveillance 14(42): 19366. doi:https://doi.org/10.2807/ese.14.42.19366-en
- Lauvrak, V. and L. Juvet. 2020. Social and Economic Vulnerable Groups During the COVID-19 Pandemic, Rapid Review 2020. Norwegian Institute of Public Health. https://www.fhi.no/globalassets/dokumenterfiler/rapporter/2020/social-and-economic-vulnerable-groups-during-the-covid-19-pandemic-report-2020-v3.pdf
- Lee, C., W. A. Rogers, and A. Braunack-Mayer. 2008. Social justice and pandemic influenza planning: The role of communication strategies, Public Health Ethics 1(3): 223–234. doi:https://doi.org/10.1093/phe/phn031
- Levin, A. T., W. P. Hanage, N. Owusu-Boaitey, K. B. Cochran, S. P. Walsh, and G. Meyerowitz-Katz. 2020. Assessing the age specificity of infection fatality rates for COVID-19: Systematic review, meta-analysis, and public policy implications, European Journal of Epidemiology 35: 1123–1138. doi:https://doi.org/10.1007/s10654-020-00698-1
- Liu, S. H., B. Liu, Y. Li, and A. Norbury. 2020. Time courses of COVID-19 infection and local variation in socioeconomic and health disparities in England, medRxiv. doi:https://doi.org/10.1101/2020.05.29.20116921
- Mackey, K., C. K. Ayers, K. K. Kondo, S. Saha, S. M. Advani, S. Young, H. Spencer et al. 2021. Racial and ethnic disparities in COVID-19-related infections, hospitalizations, and deaths: A systematic review, Annals of Internal Medicine 174(3): 362–373. doi:https://doi.org/10.7326/M20-6306
- Mamelund, S.-E. 2003. Spanish influenza mortality of ethnic minorities in Norway 1918–1919, European Journal of Population/ Revue Européenne de Démographie 19(1): 83–102. doi:https://doi.org/10.1023/A:1022179025843
- Mamelund, S.-E. 2004. Can the Spanish influenza pandemic of 1918 explain the baby boom of 1920 in neutral Norway?, Population 59(2): 229–260. doi:https://doi.org/10.2307/3654904
- Mamelund, S.-E. 2006. A socially neutral disease? Individual social class, household wealth and mortality from Spanish influenza in two socially contrasting parishes in Kristiania 1918–19, Social Science & Medicine 62(4): 923–940. doi:https://doi.org/10.1016/j.socscimed.2005.06.051
- Mamelund, S.-E. 2008. Influenza, historical, in International Encyclopedia of Public Health (Vol. 3). Academic Press, pp. 597–609. doi:https://doi.org/10.1016/B978-012373960-5.00372-5
- Mamelund, S.-E. 2011. Geography may explain adult mortality from the 1918–20 influenza pandemic, Epidemics 3(1): 46–60. doi:https://doi.org/10.1016/j.epidem.2011.02.001
- Mamelund, S. E. 2017. Social inequality – A forgotten factor in pandemic influenza preparedness, Tidsskrift for Den Norske Legeforening 12–13: 911–913. doi:https://doi.org/10.4045/tidsskr.17.0273
- Mamelund, S. E. 2018. 1918 pandemic morbidity: The first wave hits the poor, the second wave hits the rich, Influenza and Other Respiratory Viruses 12(3): 307–313. doi:https://doi.org/10.1111/irv.12541
- Mamelund, S.-E. and J. Dimka. 2019. Tuberculosis as a risk factor for 1918 influenza pandemic outcomes, Tropical Medicine and Infectious Disease 4(2): 74. doi:https://doi.org/10.3390/tropicalmed4020074
- Mamelund, S.-E., J. Dimka, and N. Zou Bakkeli. 2021. Social disparities in adopting non-pharmaceutical interventions during COVID-19, Journal of Developing Societies: 0169796X2199685, doi:https://doi.org/10.1177/0169796X21996858
- Mamelund, S. E., B. Haneberg, and S. Mjaaland. 2016. A missed summer wave of the 1918–1919 influenza pandemic: Evidence from household surveys in the United States and Norway, Open Forum Infectious Diseases 3(1): ofw040. doi:https://doi.org/10.1093/ofid/ofw040
- Mamelund, S. E., L. Sattenspiel, and J. Dimka. 2013. Influenza-associated mortality during the 1918–1919 influenza pandemic in Alaska and Labrador: A comparison, Social Science History 37(2): 177–229. doi:https://doi.org/10.1215/01455532-2074420
- Mamelund, S.-E., C. Shelley-Egan, and O. Rogeberg. 2020. The association between socioeconomic status and pandemic influenza: Systematic review and meta-analysis, medRxiv. doi:https://doi.org/10.1101/2020.12.09.20246496
- Marmot, M. 2005. Social determinants of health inequalities, The Lancet 365(9464): 1099–1104. doi:https://doi.org/10.1016/S0140-6736(05)71146-6
- Marmot, M. G. and R. Bell. 2009. Action on health disparities in the United States, JAMA 301(11): 1169–1171. doi:https://doi.org/10.1001/jama.2009.363
- Martins-Filho, P. R., A. A. de Souza Araujo, L. J. Quintans-Junior, and V. S. Santos. 2020. COVID-19 fatality rates related to social inequality in northeast Brazil: A neighbourhood-level analysis, Journal of Travel Medicine 27(7). doi:https://doi.org/10.1093/jtm/taaa128
- Matthews, D. 2020. German humanities scholars enlisted to end coronavirus lockdown. Available: https://www.timeshighereducation.com/news/german-humanities-scholars-enlisted-end-coronavirus-lockdown.
- Maurer, J. 2016. Inspecting the mechanism, Medical Decision Making 36(7): 887–899. doi:https://doi.org/10.1177/0272989x15608379
- Meyerowitz-Katz, G. and L. Merone. 2020. A systematic review and meta-analysis of published research data on COVID-19 infection-fatality rates, International Journal of Infectious Diseases 101: 138–148. doi:https://doi.org/10.1016/j.ijid.2020.09.1464
- Miller, H. 2020. Navajo nation reports more coronavirus cases per capital than all but 2 U.S. States. Available: https://www.huffpost.com/entry/navajo-nation-coronavirus-per-capita_n_5e94b532c5b6a50d4ae6d7e7.
- Murray, C. J., A. D. Lopez, B. Chin, D. Feehan, and K. H. Hill. 2007. Estimation of potential global pandemic influenza mortality on the basis of vital registry data from the 1918–20 pandemic: A quantitative analysis, The Lancet 368(9554): 2211–2218. doi:https://doi.org/10.1016/S0140-6736(06)69895-4
- Mutambudzi, M., C. Niedwiedz, E. B. Macdonald, A. Leyland, F. Mair, J. Anderson, C. Celis-Morales et al. 2020. Occupation and risk of severe COVID-19: Prospective cohort study of 120 075 UK biobank participants, Occupational and Environmental Medicine 78: 307–314. doi:https://doi.org/10.1136/oemed-2020-106731
- Nagle, R. 2020. Native Americans being left out of US coronavirus data and labelled as ‘other’. Available: https://www.theguardian.com/us-news/2020/apr/24/us-native-americans-left-out-coronavirus-data.
- Økland, H. and S.-E. Mamelund. 2019. Race and 1918 influenza pandemic in the United States: A review of the literature, International Journal of Environmental Research and Public Health 16(14): 2487. doi:https://doi.org/10.3390/ijerph16142487
- Okoi, O. and T. Bwawa. 2020. How health inequality affect responses to the COVID-19 pandemic in sub-Saharan Africa, World Development 135: 105067. doi:https://doi.org/10.1016/j.worlddev.2020.105067
- Olson, D. R., L. Simonsen, P. J. Edelson, and S. S. Morse. 2005. Epidemiological evidence of an early wave of the 1918 influenza pandemic in New York City, Proceedings of the National Academy of Sciences 102(31): 11059–11063. doi:https://doi.org/10.1073/pnas.0408290102
- Oxford, J. S. and D. Gill. 2018. Unanswered questions about the 1918 influenza pandemic: Origin, pathology, and the virus itself, The Lancet Infectious Diseases 18(11): e348–e354. doi:https://doi.org/10.1016/S1473-3099(18)30359-1
- Oxford, J. S., A. Sefton, R. Jackson, N. P. A. S. Johnson, and R. S. Daniels. 1999. Who’s that lady?, Nature Medicine 5(12): 1351–1352. doi:https://doi.org/10.1038/70913
- Patel, A. P., M. D. Paranjpe, N. P. Kathiresan, M. A. Rivas, and A. V. Khera. 2020. Race, socioeconomic deprivation, and hospitalization for COVID-19 in English participants of a national biobank, International Journal for Equity in Health 19(1): 114. doi:https://doi.org/10.1186/s12939-020-01227-y
- Phelan, J. C., B. G. Link, and P. Tehranifar. 2010. Social conditions as fundamental causes of health inequalities: Theory, evidence, and policy implications, Journal of Health and Social Behavior 51(1_suppl): S28–S40. doi:https://doi.org/10.1177/0022146510383498
- Phillips, H. 1984. Black October: The impact of the Spanish influenza epidemic of 1918 on South Africa. Unpublished PhD dissertation, University of Cape Town, South Africa.
- Phillips, H. 2014. The recent wave of ‘Spanish’ flu historiography, Social History of Medicine 27: 789–808. doi:https://doi.org/10.1093/shm/hku066
- Piketty, T. 2014. Capital in the Twenty-First Century. Cambridge, MA: Belknap Press of Harvard University Press.
- Plümper, T. and E. Neumayer. 2020. The pandemic predominantly hits poor neighbourhoods? SARS-CoV-2 infections and Covid-19 fatalities in German districts, European Journal of Public Health 30(6): 1176–1180. doi:https://doi.org/10.1093/eurpub/ckaa168
- Price-Haywood, E. G., J. Burton, D. Fort, and L. Seoane. 2020. Hospitalization and mortality among black patients and white patients with Covid-19, New England Journal of Medicine 382(26): 2534–2543. doi:https://doi.org/10.1056/NEJMsa2011686
- Public Health England. 2020. Disparities in the Risk and Outcomes of COVID-19. Available: https://www.gov.uk/government/publications/covid-19-review-of-disparities-in-risks-and-outcomes.
- Raphael, D. 2006. Social determinants of health: Present status, unanswered questions, and future directions, International Journal of Health Services 36(4): 651–677. doi:https://doi.org/10.2190/3MW4-1EK3-DGRQ-2CRF
- Rast, J., Y. C. Martinez, and L. H. Williams. 2020. Milwaukee’s Coronavirus Racial Divide: A Report on the Early Stages of COVID-19 Spread in Milwaukee County. Center for Economic Development Publications. https://dc.uwm.edu/cgi/viewcontent.cgi?article=1053&context=ced_pubs
- Rice, G. 1988. Black November: The 1918 Influenza Epidemic in New Zealand. Wellington: Allen & Unwin and Historical Branch, New Zealand Department of Internal Affairs.
- Rice, G. W. 2018. Influenza in New Zealand before 1918: A preliminary report, American Journal of Epidemiology 187(12): 2524–2529. doi:https://doi.org/10.1093/aje/kwy180
- Rosenberg, C. E. 1992. Explaining Epidemics and Other Studies in the History of Medicine. Cambridge: Cambridge University Press.
- Rostila, M., A. Cederström, M. Wallace, M. Brandén, B. Malmberg, and G. Andersson. 2020. Disparities in Covid-19 Deaths by Country of Birth in Stockholm, Sweden: A Total Population Based Cohort Study. Stockholm Research Reports in Demography.
- Ruggles, S. 2021. The revival of quantification: Reflections on old new histories, Social Science History 45: 1–25. doi:https://doi.org/10.1017/ssh.2020.44
- Ruggles, S. and D. L. Magnuson. 2020. The history of quantification in history: The JIH as a case study, Journal of Interdisciplinary History 3(Winter 2020): 363–381. doi:https://doi.org/10.1162/jinh_a_01446
- Sample, I. 2020. Who’s who on secret scientific group advising UK government?. Available: https://www.theguardian.com/world/2020/apr/24/coronavirus-whos-who-on-secret-scientific-group-advising-uk-government-sage.
- Schmidt, H., P. Pathak, T. Sönmez, and M. U. Ünver. 2020. Covid-19: How to prioritize worse-off populations in allocating safe and effective vaccines, BMJ 371: m3795. doi:https://doi.org/10.1136/bmj.m3795
- Semenza, J. C. 2010. Strategies to intervene on social determinants of infectious diseases, Eurosurveillance 15(27): 19611. doi:https://doi.org/10.2807/ese.15.27.19611-en
- Shortridge, K. F. 1999. The 1918 ‘Spanish’ flu: Pearls from swine?, Nature Medicine 5(4): 384–385. doi:https://doi.org/10.1038/7383
- Sohrabi, C., Z. Alsafi, N. O’Neill, M. Khan, A. Kerwan, A. Al-Jabir, C. Iosifidis et al. 2020. World Health Organization declares global emergency: A review of the 2019 novel coronavirus (COVID-19), International Journal of Surgery 76: 71–76. doi:https://doi.org/10.1016/j.ijsu.2020.02.034
- Steptoe, A., A. Shamaei-Tousi, Å Gylfe, B. Henderson, S. Bergström, and M. Marmot. 2007. Socioeconomic status, pathogen burden and cardiovascular disease risk, Heart 93(12): 1567–1570. doi:https://doi.org/10.1136/hrt.2006.113993
- Steyn, N., R. Binny, K. Hannah, S. Hendy, A. James, T. Kukutai, A. Lustig et al. 2020. Estimated inequities in COVID-19 infection fatality rates by ethnicity for Aotearoa New Zealand, New Zealand Medical Journal 133(1521): 28–39. https://assets-global.website-files.com/5e332a62c703f653182faf47/5f500878a2864b4765a25c10_Plank%20FINAL.pdf
- Stone, A. A., A. B. Krueger, A. Steptoe, and J. K. Harter. 2010. The socioeconomic gradient in daily colds and influenza, headaches, and pain, Archives of Internal Medicine 170(6): 570–572. doi:https://doi.org/10.1001/archinternmed.2010.20
- Summers, J. A., G. D. Shanks, M. G. Baker, and N. Wilson. 2013. Severe impact of the 1918–19 pandemic influenza in a national military force, The New Zealand Medical Journal 126(1378): 36–47.
- Summers, J. A., J. Stanley, M. G. Baker, and N. Wilson. 2014. Risk factors for death from pandemic influenza in 1918–1919: A case–control study, Influenza and Other Respiratory Viruses 8(3): 329–338. doi:https://doi.org/10.1111/irv.12228
- Summers, J. A., N. Wilson, M. G. Baker, and G. D. Shanks. 2010. Mortality risk factors for pandemic influenza on New Zealand troop ship, 1918, Emerging Infectious Diseases 16(12): 1931–1937. doi:https://doi.org/10.3201/eid1612.100429
- Sydenstricker, E. 1931. The incidence of influenza among persons of different economic status during the epidemic of 1918, Public Health Reports (1896–1970) 46(4): 154–170. doi:https://doi.org/10.2307/4579923
- Taubenberger, J. K. 2003. Genetic characterisation of the 1918 ‘Spanish’ influenza virus, in H. Phillips and D. Killingray (eds), The Spanish Influenza Pandemic of 1918–19: New Perspectives. London: Routledge, pp. 39–46.
- Taubenberger, J. K., A. H. Reid, T. A. Janczewski, and T. G. Fanning. 2001. Integrating historical, clinical and molecular genetic data in order to explain the origin and virulence of the 1918 Spanish influenza virus, Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences 356(1416): 1829–1839. doi:https://doi.org/10.1098/rstb.2001.1020
- Tomkins, S. M. 1992. The failure of expertise: Public health policy in Britain during the 1918–19 influenza epidemic, Social History of Medicine 5(3): 435–454. doi:https://doi.org/10.1093/shm/5.3.435
- Trauer, J. M., K. L. Laurie, J. McDonnell, A. Kelso, and P. G. Markey. 2011. Differential effects of pandemic (H1N1) 2009 on remote and indigenous groups; Northern Territory, Australia, 2009, Emerging Infectious Diseases 17(9): 1615–1623. doi:https://doi.org/10.3201/eid1709.101196
- Uscher-Pines, L., P. S. Duggan, J. P. Garoon, R. A. Karron, and R. R. Faden. 2007. Planning for an influenza pandemic: Social justice and disadvantaged groups, Hastings Center Report 37(4): 32–39. doi:https://doi.org/10.1353/hcr.2007.0064
- van Daalen, K. R., C. Bajnoczki, M. Chowdhury, S. Dada, P. Khorsand, A. Socha, A. Lal et al. 2020. Symptoms of a broken system: The gender gaps in COVID-19 decision-making, BMJ Global Health 5(10): e003549. doi:https://doi.org/10.1136/bmjgh-2020-003549
- Van Hartesveldt, F. R. 1992. The 1918–1919 Pandemic of Influenza: The Urban Impact in the Western World. Lewiston, NY: Edwin Mellen Press.
- Wadhera, R. K., P. Wadhera, P. Gaba, J. F. Figueroa, K. E. Joynt Maddox, R. W. Yeh, and C. Shen. 2020. Variation in COVID-19 hospitalizations and deaths across New York City boroughs, JAMA 323(21): 2192–2195. doi:https://doi.org/10.1001/jama.2020.7197
- Wastnedge, E. A. N., R. M. Reynolds, S. R. van Boeckel, S. J. Stock, F. C. Denison, J. A. Maybin, and H. O. D. Critchley. 2021. Pregnancy and COVID-19, Physiological Reviews 101(1): 303–318. doi:https://doi.org/10.1152/physrev.00024.2020
- Williamson, E. J., A. J. Walker, K. Bhaskaran, S. Baco, C. Bates, C. E. Morton, H. J. Curtis et al. 2020. Factors associated with Covid-19-related death using OpenSAFELY, Nature 584(7821): 430–436. doi:https://doi.org/10.1038/s41586-020-2521-4
- Wilson, N., L. T. Barnard, J. A. Summers, G. D. Shanks, and M. G. Baker. 2012. Differential mortality rates by ethnicity in 3 influenza pandemics over a century, New Zealand, Emerging Infectious Diseases 18(1): 71–77. doi:https://doi.org/10.3201/eid1801.110035
- Wilson, N., O. Mansoor, and M. Baker. 2018. The first analytic evidence for socio-economic gradients in 1918 pandemic influenza mortality rates for New Zealand, The New Zealand Medical Journal 131(1486): 50–53.
- Worldometer. 2021. COVID-19 Coronavirus Pandemic. Available: https://www.worldometers.info/coronavirus/.
- Wu, Y. C., C. S. Chen, and Y. J. Chan. 2020. The outbreak of COVID-19: An overview, Journal of the Chinese Medical Association 83(3): 217–220. doi:https://doi.org/10.1097/JCMA.0000000000000270
- Yang, T. C., S. W. Emily Choi, and F. Sun. 2021. COVID-19 cases in US counties: Roles of racial/ethnic density and residential segregation, Ethnicity & Health 26(1): 11–21. doi:https://doi.org/10.1080/13557858.2020.1830036
- Zelner, J., R. Trangucci, R. Naraharisetti, A. Cao, R. Malosh, K. Broen, N. Masters et al. 2021. Racial disparities in coronavirus disease 2019 (COVID-19) mortality are driven by unequal infection risks, Clinical Infectious Diseases 72(5): e88–e95. doi:https://doi.org/10.1093/cid/ciaa1723
- Zylberman, P. 2003. A holocaust in a holocaust: The Great War and the 1918 Spanish influenza epidemic in France, in H. Phillips and D. Killingray (eds), The Spanish Influenza Pandemic of 1918–19. New Perspectives. London: Routledge Social History of Medicine Series, pp. 191–201.