Abstract
Aims: Leading the growing international recognition of the need for sustainability in healthcare delivery, the UK medical regulator has mandated that newly qualified doctors must be able to apply the principles of sustainable healthcare to medical practice. This original research investigates how best to incorporate this new learning into the medical curriculum.
Methods: Data from multiple sources were triangulated to generate themes through grounded theory. Meetings were held with representatives of key stakeholder organizations, relevant documents were reviewed and semi-structured interviews were conducted with diverse medical educators who teach sustainable healthcare.
Results: There is continual pressure on space in the curriculum, and faculty lack the knowledge to teach this emerging subject, which is also difficult to examine. Students increasingly demand that sustainability be addressed in their education and future careers. Many sources of support and learning resources are available.
Conclusions: Practical recommendations for implementation in any medical school include: teaching sustainability as a cross-cutting theme rather than a topic, clinicians and students learning from each other in this developing field, and embedding into assessment the wider determinants of disease. Sustainable healthcare emphasizes prevention rather than late intervention, with benefits to the environment on which health depends, healthcare systems and patients.
Introduction
A new mandate for the field of medical education
As the international drive for healthcare professionals to embrace sustainability gains momentum, the UK has taken the lead. In the General Medical Council’s document Outcomes for graduates 2018 (“Outcomes”), the medical regulator has placed a new obligation on medical education (General Medical Council Citation2018). Doctors qualifying or registering in the UK will be required to understand and apply the principles of sustainable healthcare to medical practice. Teaching this is the responsibility of medical schools and of doctors who are involved in medical education. Yet sustainability is an emerging concept to many in the medical profession, although the increasingly unsustainable nature of the healthcare system and potential ways to address this may already be familiar.
Sustainable healthcare
Healthcare nationally and globally is responsible for one-tenth of economic activity and this proportion is growing (Sustainable Development Unit Citation2018; Xu et al. Citation2018). However, treatments do not always benefit the patients and can cause harm, and are increasingly technology-based and expensive, while the majority of healthcare budgets are spent on long-term conditions which are dependent on lifestyle and environmental factors (Crisp Citation2017; Montgomery et al. Citation2017). More emphasis on prevention is therefore necessary for better patient outcomes and to reduce pressure on services to improve their quality (Naylor and Appleby Citation2012; Hensher et al. Citation2017; Organisation for Economic Co-operation and Development Citation2017). The adverse impact of healthcare delivery on the environment also needs to be addressed (Roberts Citation2009).
Sustainable healthcare focuses on the improvement of health and better delivery of healthcare, rather than late intervention in disease, with resulting co-benefits to patients and to the environment on which human health depends. It would thus serve to provide high-quality healthcare now without compromising the ability to provide healthcare in the future.
A need for evidence
To implement this new learning, medical schools need evidence of best practice for embedding sustainability into the curriculum. As sustainable healthcare education has not been a requirement to date, the literature has understandably focused on making the case for teaching it rather than researching its implementation (Mortimer Citation2010; Gómez et al. Citation2013; Walpole et al. Citation2016). Where integration into the curriculum is addressed, opportunities have been identified and teaching methods suggested though not tested (Bell Citation2010; Maxwell and Blashki Citation2016; Walpole et al. Citation2017; Wellbery et al. Citation2018). An exception is a participatory action research study which evaluated collaboration and pedagogies, and its findings are explored in the analysis section (Walpole and Mortimer Citation2017). Specific teaching initiatives for student nurses have also been described (Richardson et al. Citation2014; Grose et al. Citation2015; Grose and Richardson Citation2016). An Australasian collaboration is developing curriculum to address the serious health threats from climate change (Madden et al. Citation2018), and the International Federation of Medical Student Associations has produced a well-structured climate and health training manual (Citation2016). An excellent resource is the book Sustainable Healthcare, which has a chapter on medical education (Schroeder et al. Citation2013). The literature review found a scarcity of evidence for best practice for embedding a new topic into the medical curriculum, and Grant emphasizes the role of purpose and context as principles of curriculum design (Bland et al. Citation2000; Grant Citation2014; Thomas et al. Citation2016). This study therefore addresses a need to determine how this new learning can best be embedded in the very diverse curricular structures of different medical schools both within the UK and more broadly.
Aim and objectives
The aim of this research is:
To make evidence-based recommendations on best practice for implementing the teaching and learning of sustainable healthcare in the medical education curriculum.
To do this, the main objectives are:
to review current practice in such teaching and relate it to the new mandate
to relate this teaching to its practical applications in healthcare delivery
to investigate educators’ experience of this teaching, and what worked well or not
to identify key barriers and enablers
to consider the best approaches to incorporating this into the medical curriculum.
Methodology
A qualitative exploratory approach was used, employing grounded theory to generate themes through the triangulation and analysis of multiple sources of data (Kennedy and Lingard Citation2006; Gibbs Citation2008; Bryman Citation2016). gives an overview of the research methods used and the specific objectives they were designed to meet.
Table 1. Methods used to meet research objectives.
Selection of contextual data sources
As primary data, the GMC Outcomes document which set out the requirement was reviewed in detail against its precursors to highlight the changes, and compared with its postgraduate equivalent the Generic Professional Capabilities Framework (General Medical Council Citation2015, Citation2017). In order to situate this new learning in the wider context of its practical application, the directors or representatives of key stakeholder organizations in the sustainable delivery of healthcare were interviewed: the Director of the Sustainable Development Unit (SDU) of the NHS/Public Health England; the Medical Director of the Centre for Sustainable Healthcare (CSH); and an NHS sustainability manager. Medical schools are part of universities, therefore to appreciate the current status of sustainability teaching and learning in higher education in general, the annual conference of the Environmental Association for Universities and Colleges (EAUC) was attended, and a meeting arranged with an Academic Sustainability Director. As these interviews were with organizations which have specific purposes they could not be anonymized or standardized.
Selection of medical educators for semi-structured interviews
Informed by the literature review and document analysis, questions were developed and used in anonymized semi-structured interviews with medical educators. Since sustainable healthcare education is an emerging concept, it is the few individuals who have been teaching this through their own interest who are expert in this field. With varying degrees of responsibility for the curriculum and seniority and specialty, these educators were from eight medical schools around the UK which have diverse approaches to curriculum structure, teaching methods and assessment. A few were schools known to the Sustainable Healthcare Education network (SHE) of the CSH to be currently teaching sustainable healthcare, others were identified by the author. As no new themes were constructed by the last interviews, this was felt to constitute sufficiency of purposive sampling.
Validity of data analysis
In order to identify the barriers, enablers, drivers, and benefits, open coding was used to identify initial key issues, followed by axial coding to explore and define the connections between categories. A reflexive open-minded approach to the meaning of the data was attempted throughout this iterative process. Insights from all the sources of data were triangulated and compared for convergence and divergence to develop theory and arrive at recommendations for practical educational innovations to meet the GMC’s new requirements. These recommendations are designed to be applicable in the wider context of all UK medical schools including those not involved in the study and potentially also in an international context as sustainability is increasingly embraced.
Ethical approval
This project was for a Masters research thesis (Tun Citation2018). Ethical approval was sought and obtained through the Imperial College Education Ethics Review Process.
Results and analysis – document analysis and interviews with key stakeholders
Document analysis of “Outcomes for graduates”
“Sustainable healthcare” appears as the headline requirement for one entire section of the 26 sections in Outcomes. This section, 25: Health promotion and illness prevention, is reproduced in with the additions and differences since the 2015 version highlighted.
Figure 1. Annotated copy of Outcomes for graduates 2018 section 25. Highlighting denotes the additions and differences since the 2015 version. Reproduced from Outcomes for graduates 2018 © 2018 General Medical Council.
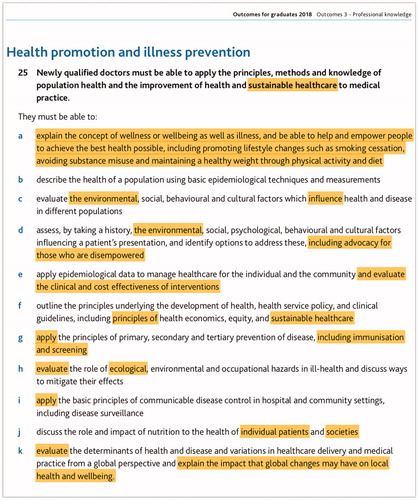
Paragraph 25a is entirely new, and focuses on health promotion, with wellness and wellbeing appearing as new concepts. The term “empower” is used, health risks are spelt out and a new reference to lifestyle changes lists healthy weight, physical activity, and diet, all of which had not been addressed before. Paragraphs 25c and 25d now include “environmental” factors and have separated out the factors which influence health and disease at a population level from similar factors influencing a patient’s presentation, and advocacy is required in the latter case. Doctors must now be able to evaluate the clinical and cost effectiveness of interventions (25e), and take into account cost effectiveness in selecting investigations (in a different section, 12–14e). The principles of sustainable healthcare are referred to again in 25f. Immunization and screening are new additions. In 25h “ecological” is mentioned for the first time, and “environmental” was previously only here, in the context of a hazard. Paragraph 25j refers to nutrition in relation to individual patients and societies which may give some scope within the teaching of sustainable healthcare. In 25k, where the impact of global changes has been added, there was a missed opportunity to mention climate change, despite the legal obligations on the NHS to reduce its carbon footprint (Great Britain Citation2008).
Other sections of Outcomes also carry scope for the teaching of sustainable healthcare. Section 5: Patient safety and quality improvement, contains “including seeking ways to continually improve the use and prioritization of resources.” Under section 6: Dealing with complexity and uncertainty, 6e is new, stating “recognise how treatment and care can place an additional burden on patients and make decisions to reduce this burden where appropriate, particularly where patients have multiple conditions or are approaching the end of life.” This mention of burden on patients is transformative, along with 12–14n in Diagnosis and medical management, “recognise the potential consequences of over-diagnosis and over-treatment.”
Centre for Sustainable Healthcare
Since 2015, the GMC has recognized the Priority Learning Outcomes (PLO) for educating for sustainable healthcare, produced by the SHE network of CSH (Thompson et al. Citation2014; Centre for Sustainable Healthcare Citation2015; Walpole et al. Citation2015). Developed through a multi-stage national consultation with UK medical schools and postgraduate organizations, the consensus PLOs were referenced in Outcomes for graduates 2015 (General Medical Council Citation2015) and were further tested in an action research project. This found that new learning could quickly be implemented but that students required a clear structure and goals, ideally with exposure to sustainability concepts early in the course to gain an understanding of the core concepts. A clinical focus was important to establish the relevance of sustainability to health outcomes and the role of the doctor (Walpole and Mortimer Citation2017). In the United States, these PLOs have been elaborated using a Delphi study, which concludes by proposing that physicians advocate for the sustainability of the healthcare systems in which they work (Teherani et al. Citation2017).
To build the confidence of faculty to teach sustainability, CSH holds training sessions to help educators to develop and embed this teaching, and its website contains a wealth of learning resources (Centre for Sustainable Healthcare Citation2019). CSH has also developed a framework for the inclusion of sustainability in quality improvement (QI) (Mortimer et al. Citation2018). Its Medical Director welcomed the potential to interweave this complex subject into areas beyond public health or health improvement, now that Outcomes includes sustainability:
Getting it into national requirements is incredibly helpful so that we can then engage with the institutions … Sustainability is now something that doctors have to know about.
NHS trust sustainability department/Sustainable Development Unit
It is in the interests of NHS trusts that clinicians are educated to understand and manage the use of resources appropriately. In addition, there are legal requirements. For instance in the UK, the National Health Service (NHS) has obligations to meet the carbon reduction targets of the Climate Change Act 2008 (Great Britain Citation2008).
If we look at the carbon footprint of the hospital, 60% of it is stuff we buy, and throw away. The energy piece is probably 20%, then waste and transport. (sustainability manager)
The SDU has an interest in the impact of medical activity, a key task being to “use the influence of the health sector … to normalise the innovative ways of improving environmental, social and economic health” (Pencheon Citation2017). Since the Public Services (Social Value) Act 2012 requires “public authorities to have regard to economic, social and environmental well-being in connection with public services contracts” (Great Britain Citation2012), sustainability would improve if these aspects were considered with the medical outcome:
Having that wider perspective would have a dramatic effect across the supply chain – we’re talking billions of pounds of purchasing … whether medicines or medical devices … sutures or scanners … pharmaceuticals are hugely energy intensive to produce. (sustainability manager)
Prescription drugs are responsible for a large proportion of the carbon footprint of healthcare. In the NHS, even unopened medicines stored in locked trolleys on the wards are thrown away when patients are discharged. It is accepted practice that an estimated £300 million of NHS prescribed medicines are wasted each year (Hazell and Robson Citation2015).
It is therefore important to these stakeholders to develop the outlook of medical students and clinicians to raise issues, and advocate for and implement change, in order for sustainability to become part of their practice and future leadership within the health system.
The higher education context
The move to teaching sustainability in higher education in general is reflected in the introduction of an academic stream at the annual conference of the EAUC, historically the sphere of the estates and facilities departments on campus. Two recurring themes in the conference were:
Students as leaders or partners of teaching
The strength of the relationship between employment and sustainability.
There is competition between universities to be seen as sustainable. It is therefore important to have consistent messaging from the highest levels of institutions that sustainability is a priority. Keele University, which hosted the conference, has a Director of Education for Sustainability, and sustainability is used as the context for generic skills development and as the core of interdisciplinary group projects.
We’ve got a number of senior appointments at Keele over the past 12 months who have partly come to Keele because of our sustainability agenda. … People are already seeing the links in those key places. I think it’s fantastically exciting at Keele. (director of education for sustainability)
Results and analysis – interviews with medical educators
The key themes identified from analysis of the semi-structured interviews with medical educators are summarized in .
Table 2. Key barriers, enablers, and drivers for implementing sustainable healthcare education.
Barriers to implementing sustainable healthcare education
1. Lack of knowledgeable teachers of sustainable healthcare: The most intractable problem emerging from the interviews was the lack of knowledgeable educators to teach healthcare sustainability. This was compounded by a perceived resistance from the established medical profession to this new concept.
The trouble is cardiologists will teach about stents and statins. They won’t teach you about sedentary lifestyles and about active transport and particulate pollution and all of these other things because they don’t know it themselves … if it was appearing in every single thing it wouldn’t take long before medical students are going ‘I seem to be hearing exactly the same thing in every subject – everything I’m hearing about the causes of cancer seems to be the same thing as causing lung disease which seems to be the same thing as causing coronary vascular disease and strokes – so why aren’t we doing something about that?’ (educator 3)
Informants stressed the need to find a number of colleagues who would be engaged and involved, and faculty development or “teaching the teacher” was needed.
2. Lack of space in the curriculum: There was consensus that the curriculum was already full or overcrowded, with staunchly defended teaching time contending with continual pressure to fit additional topics.
One of my colleagues talks about the 25 year undergraduate curriculum … if we actually taught all the things that everybody thinks that undergraduate students need to know about medicine before graduating. If we were to do justice to all the topics that we strongly feel that medics need to know we would never actually let them graduate. (educator 4)
3. Uncertainty of location in the curriculum: There was strong feeling that sustainable healthcare is not a topic but a theme akin to ethics, professionalism, or leadership that should spiral through all the years in the core curriculum. For later years, the topics of wastefulness and the clinical environment could be related to quality of care and patient safety:
Patient safety is quite a dominant energy. It’s hard to argue against and therefore things sometimes get too much priority, because they’re beating the patient safety drum so loudly and everyone’s afraid to argue against it … things like disposable curtains … when our students looked into it they couldn’t find any evidence for why we had to throw away our curtains every six months. (educator 6)
4. Need for learning resources: Informants suggested that a sustainable healthcare lead could be engaged to offer a coherent course, perhaps using current topics of debate:
… creating a suite of interesting and updated resources – the problem is having someone whose job it is to keep them updated. (educator 5)
Many proposed that learning resources such as recorded lectures, reading and e-learning material and slides should be pooled and widely disseminated between medical schools. Although there are unhelpful funding models and possible concerns about intellectual property, this approach was seen as more sustainable than for each medical school to produce its own resources, especially in a subject with few knowledgeable teachers.
5. Difficulty in assessing learning: Sustainable healthcare was seen as challenging to examine. In many informants’ and the author’s view, the metric of success would be attitudinal change and empowerment in the student and change in their future clinical practice. To achieve this, educators wanted every exam question to begin by asking about the extent to which environmental and lifestyle factors cause the disease in question. This may go some way to increasing awareness; however, current modalities of assessment do not fully lend themselves to detecting whether the learners have achieved the desired outcomes. As observed by Prideaux (Citation2007), “new content and new emphases in medical education require new methods of assessment.”
6. Emotional impact needing resilience: Sustainability is a challenging subject to handle emotionally, and there is a need to teach resilience alongside the large-scale thinking that the issue requires. It is important for both teachers and learners to keep a positive outlook, as the topic can be overwhelming:
Perhaps because of my position I only really get the politically aware students talking to me about this. And so I see a small wave of very depressed students, frustrated and – you know, like the rest of us, really – desperately hoping that – in the way that I probably did too when I was in my teens – hoping that somebody will just wade in and sort all of this out now please. (educator 4)
With growing understanding comes a sense of urgency, mission, and responsibility:
This is not my planet. It’s our planet, and there’s only one of them. When it’s gone, it’s gone. We’re burdened with financial constraints within the health service. This gave [the student] the opportunity to see this is real. (educator 2)
Learning for both educators and students needs to be supported to ensure emotional resilience, and the use of practical projects that result in change could improve morale.
Enablers and drivers for implementing sustainable healthcare education
1. Demand from students: Students were seen as a driver for sustainable healthcare education, with high achievers being some of the most interested:
We get very bright students, and then we don’t stretch them out of their comfort zone … it’s getting students to think through the solutions for the world in which they’re going to inhabit. (educator 5)
Retaining the highest quality candidates is important as medical schools face an expectation to act to help stem the loss of recently qualified doctors, who may leave through disillusionment with existing structures. Educators said that students valued reflecting on how the system could be different, and that feedback was overwhelmingly positive. One described how well their lectures are received by a cohort of approximately 300 students:
They’re all still there 45 minutes later asking questions, the whole lot [late on a Friday], no one leaves, they’re really engaged. (educator 3)
There was variability in prior awareness:
… interesting being a fly on the wall at these sessions – one or two students go ‘How is it our job to look at food?’ … considering the role of the doctor not just as mending patients and sending them on their way, but making them see things in a different way. (educator 1)
However, educators reported greatly enjoying practical sessions and students warmed to sustainability teaching quite rapidly:
At the beginning, a degree of scepticism … at the end of the module – six or eight sessions that we had together, and the word of one of them was ‘This was life changing.’ Those were his words. (educator 2)
2. The move in higher education to include sustainability: University-wide support can encourage innovative teaching of sustainability, which is seen to enhance both appeal to students and career opportunities for students:
The generation coming through want this … not just doctors, you talk to management consultants, you talk to Unilever, they all say the question you get asked by potential employees is ‘What’s your position on sustainability, what’s your position on global health? Because if you aren’t doing the right thing, I don’t want to work for you.’ (educator 3)
Educators saw a time of curriculum review as a good opportunity to introduce sustainability into core teaching, and institutional leadership and ethos are important.
3. A new legitimacy through GMC mandate: Many noted that prioritization in the headline signaled significant change in the subcategories.
… it’s actually a whole section of Outcomes for graduates. It’s incredibly powerful. It is without doubt the most helpful thing that’s come along in a long while – not just for sustainability but for loads of helpful things. (educator 6)
Just as for NHS trusts a key driver of change is the requirement to report on sustainability in the annual report, it is encouraging that complying with Outcomes is mandatory:
… the GMC do actually use this as the template for how they assess the medical schools. So you have to do a return – I think they have given us to 2020, but by 2020 we will have to explain how our curriculum delivers on these goals. (educator 6)
One aspect of the wording however brought out strongly held views among many educators, on the distinction between action on individual behaviors and on the wider determinants of health:
I hate this – ‘lifestyle changes’ – we are ignoring the weight of evidence around the constrained choices that some people have. That is fundamentally an individualistic conceptualisation compared with the old [Outcomes]. (educator 5)
We know targeting risk groups doesn’t work. What you need to do is shift the population mean, move the normal distribution down and then you get a huge change of scale. (educator 3)
… I feel a bit uneasy because a lot of the [changing] individual behaviours stuff is not as effective as changing the transportation system or how you design cities or challenge the food structures. (educator 7)
We can’t afford to keep treating people for the consequences of these problems, we have to find a better way. (educator 8)
4. Leadership from other stakeholders: In producing graduates, medical schools must consider the policy and strategy of other stakeholders in the practice of medicine. Medical education lags behind its counterparts in teaching sustainability not only in higher education generally but also in postgraduate medical training. Doctors in postgraduate training are now expected to design and implement QI projects, and understand how resources are managed and the importance of avoiding waste (General Medical Council Citation2017). Sustainability is one of the seven domains used by the Royal College of Physicians to define quality, and “must run through and moderate other domains. Healthcare should be considered not only in terms of what can be delivered to an individual today, but also to the population in general and the patient of the future” (Atkinson et al. Citation2010). One educator expressed this with clarity:
The ethical concept of sustainability is about unfairness across time. Health inequalities is typically about unfairness now across space. (educator 7)
The Royal College of General Practitioners’ position statement on quality in general practice also mentions sustainable delivery of healthcare, the avoidance of waste and the sustainable use of resources (Royal College of General Practitioners Citation2017). Apart from the financial constraints and the carbon emissions targets faced by NHS trusts and the SDU, there is the frustration of the clinicians themselves:
I think increasingly the more one does medicine the more one realises an awful lot of what one does doesn’t make any difference at all. Certainly on the [unit] I’m working on probably 13 out of 15 beds on any one day are occupied by diseases that are entirely preventable and they [the junior doctors] see that. (educator 3)
5. Sources of support and resources: Educators indicated many sources of support and learning resources, such as through the CSH, the websites of the medical Royal Colleges, and NHS trust Estates and Facilities departments’ sustainability teams where students may identify significant avenues for QI at the same time as savings. Many pedagogies were found to be suitable including: lectures, talks, or seminars; SSCs or practical projects ranging from a series of half days to a complete two-week to six-week block; essays based on an SSC; workshops and case-based scenarios with facilitated small group discussions; mini QI projects; as part of clinical placements within general practice or hospital trusts; and incorporation into public health and global health teaching. Educators reported that students were particularly positive when the teaching was clinically relevant to patient care, concerned with real issues in a local context such as energy use or waste management, used concrete examples such as carbon footprinting, involved a practical element in small group teaching or when a lecture was by a clinician seen to be thinking about sustainable healthcare.
Discussion
Developing theory from observation
provides a theoretical framework for the relationships between the barriers, enablers, solutions, and benefits identified through triangulation of data from the literature, documents, stakeholders, and semi-structured interviews.
Figure 2. Teaching and learning sustainable healthcare: Barriers (red), Enablers (light blue), Solutions (yellow highlight), and Benefits (black).
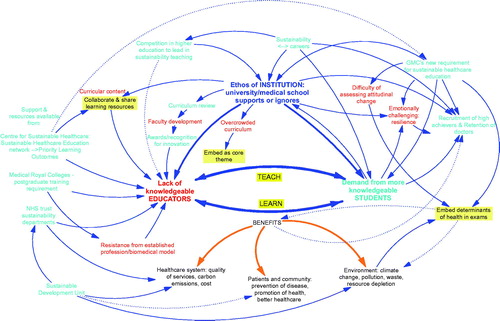
Given that the foremost problem is lack of knowledge of sustainability in educators, especially the clinicians who teach, and that the most desirable teaching is by these very people, a solution is that the teachers learn about sustainability at the same time that they are teaching it to students. This has been suggested in Sustainable Healthcare (Schroeder et al. Citation2013, p. 224):
… students often teem with ideas and initiatives, once given the freedom to express them. It is a pleasure to see how sustainability teaching often dissolves the usual academic hierarchies, where, due to this being a new field, students frequently teach as much as they learn.
Teaching faculty who are open enough to embrace sustainability may well value the concept of openly learning alongside the students they are meant to be teaching. This has been documented in health promotion education where GP tutors valued learning from the students and the fresh perspective that students brought to their practice (Wylie and Leedham-Green Citation2017). Indeed the first keynote speaker at the EAUC conference pointed out that the Welsh have only one word “dysgu” for both teaching and learning, and so: “I teach you, I’m learning from you. Who is expert, teacher, learner?” (Fazey Citation2018)
The international collaboration described by Walpole et al. (Citation2017) also suggested educator–student partnership, and there was consensus that sustainability should be integrated into a spiral curriculum that builds learning throughout the years of the course.
The questions of space and place in the curriculum can thus be addressed together by understanding that sustainability in healthcare is a core theme, as identified by the Royal College of Physicians (Atkinson et al. Citation2010).
The theoretical relationship developed through grounded theory is therefore as follows:
By embedding sustainability as a theme running through all of medical education, educators and students can teach and learn from each other at the same time as learning about sustainable healthcare, irrespective of specialization.
Strengths and limitations of the research
This study was able to access multiple sources of data by a range of methods to provide a holistic context. A wide range of medical educators who have developed expertise in teaching about sustainable healthcare all agreed to be interviewed and useful insights were garnered. Similarly, the directors and representatives of the key stakeholder organizations identified were interviewed and gave valuable input.
Of necessity, extrapolation is being attempted from the analysis of current practice, where there is no requirement to teach sustainability, to a context where there is a mandate for such teaching. As this is an emerging field there is a limited number of experts to access. The key informants in both the semi-structured and informal interviews were enthusiasts for sustainable healthcare education and this may have influenced the themes that were generated. An alternative approach could have been to elicit the perspective of educators who do not hold this view, in order to better illuminate the barriers in particular. While remaining aware of the need for reflexivity throughout the process, there may be bias in that the researcher also believes that doctors should be educated to act in a way that makes healthcare more sustainable. The student perspective was not sought as this has been addressed in other studies, and also a different ethics approval process would be required.
Conclusions and recommendations
The medical regulator’s new mandate for newly qualified doctors to be able to apply the principles, methods, and knowledge of sustainable healthcare to medical practice created the question of how best to embed this teaching in the very diverse curricular structures of medical schools. The focus of sustainable healthcare is on the improvement of health and better delivery of healthcare, rather than late intervention in disease. In Outcomes for graduates, the GMC has introduced to medical education the concepts of over-diagnosis and over-treatment, cost effectiveness, and treatment as a burden on patients. Wellness or wellbeing as well as illness, and their environmental determinants, now have to be studied, with advocacy for those who are disempowered. This research found a clear consensus from participants and the literature on the key barriers and enablers to implementing this new learning. These were holistically considered, resulting in 10 practical recommendations for implementing sustainable healthcare education in any medical school, as shown in the panel “Recommendations for implementation of sustainable healthcare education.”
It is important to bear in mind the benefits that will accrue: both to the health service and by way of health co-benefits for patients; by preparing doctors-to-be for the reality of their future practice; and not least through any influence on the culture of senior leaders new to teaching about sustainable healthcare.
Priorities for future work
Areas for future research include the following, once sustainable healthcare curricula are being piloted:
Evaluation of new teaching and learning of sustainable healthcare, especially in medical schools where this has not previously taken place, including situations where teachers are learning with and from students.
Research into suitable modalities of assessment of the impact of this learning on students’ perspective and practice.
Collaborations with the following key organizations are suggested to enhance the development of sustainable healthcare teaching:
Universities/medical schools: at institutional level and faculty level to facilitate the exchange of learning resources such as videos, recorded lectures, slides.
CSH/SHE: to develop a simplified QI framework for medical schools; and to collate sources of learning materials from various national and international organizations.
Medical Royal Colleges: to facilitate vertical integration with specialty training.
National and international student bodies interested in sustainable healthcare: to discuss future direction.
Recommendations for implementation of sustainable healthcare education
Educating new doctors to promote and practice sustainable healthcare may enhance satisfaction in clinical practice and has wider benefits for the healthcare system and the environment as well as for patients. Ten widely applicable recommendations were formulated from this research for medical schools wishing to embed the teaching of sustainable healthcare:
Timetable sustainability as a theme not a topic. This runs through all of medical education, so most faculty need to be informed and many educators should be involved.
Train the teachers alongside the learners. Build up staff teaching capacity in sessions where it is accepted that students may well be more knowledgeable, e.g. on climate change.
Involve clinicians as much as possible. Relating teaching to medical practice and clinical care of patients has the greatest impact on students.
Pool teaching resources to avoid duplication. As few educators are well versed in sustainable healthcare, share with other medical schools recorded material such as lectures, presentation slides, video film, online modules – in the spirit of sustainability.
Use other sources of support. Learning resources are available from CSH, the postgraduate medical Royal Colleges, World Health Organization, internationally developed Massive Open Online Courses. Hospital Trust sustainability managers can help with projects and benefit from the potential improvements that are identified.
Employ multiple pedagogies. After a basic grounding, include practical sessions to think about more sustainable options, have compulsory and optional projects, case-based scenarios – depending on the context in the curriculum.
Embed in assessment. Assessment modalities include: multiple choice questions for factual knowledge; as part of objective structured clinical exams to ensure integration into clinical practice; incorporation into written questions to emphasize the identification of preventable causes of disease.
Demand institutional backing. Consistent messaging from the highest levels which relates sustainability teaching to the university’s ethos and strategy can smooth progress in embedding teaching.
Plan to support emotional resilience. Addressing sustainability issues can cause strong or overwhelming reactions in staff or students, which need to be recognized and directed to relevant sources of support.
Evaluate the innovation. Plan, pilot, and evaluate as with any new teaching, bearing in mind the need for core teaching of the whole cohort, and the desirability of offering further optional projects.
Practice points
-
Sustainable healthcare is a cross-cutting core theme, not a stand-alone topic.
-
Educators and students can teach and learn from each other in this emerging field.
-
Relating teaching to clinical practice has the greatest impact on students’ learning.
-
Resources are available from the Centre for Sustainable Healthcare, WHO, postgraduate medical Royal Colleges, and internationally developed Massive Open Online Courses.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
Glossary
Sustainable healthcare: Focuses on the improvement of health and better delivery of healthcare, rather than late intervention in disease, with resulting benefits to patients and to the environment on which human health depends, thus serving to provide high-quality healthcare now without compromising the ability to meet the health needs of the future.
Acknowledgments
The author would like to sincerely thank William R. Sheate, who supervised the Masters research thesis on which this paper is based. Many thanks to all the participants who generously gave their time and insights in being interviewed, this study would not have been possible without them.
Disclosure statement
The author reports no conflicts of interest. The author alone is responsible for the content and writing of this article.
Additional information
Notes on contributors
SanYuMay Tun
SanYuMay Tun (May Sanyu Tun), MB BS, MSc, DIC, FHEA, is a medical educator and former General Practitioner who recently completed an MSc at the Centre for Environmental Policy, Imperial College London, specializing in Health and the Global Environment.
References
- Atkinson S , Ingham J , Cheshire M , Went S . 2010 . Defining quality and quality improvement . Clin Med . 10 : 537 – 539 .
- Bell EJ . 2010 . Climate change: what competencies and which medical education and training approaches? BMC Med Educ . 10 : 31 .
- Bland CJ , Starnaman S , Wersal L , Moorhead-Rosenberg L , Zonia S , Henry R . 2000 . Curricular change in medical schools: how to succeed . Acad Med . 75 : 575 – 594 .
- Bryman A . 2016 . Social research methods . 5th ed . Oxford : Oxford University Press .
- Centre for Sustainable Healthcare. 2015 . Educating for sustainable healthcare – expanded learning outcomes; [accessed 2019 Jan 25]. https://sustainablehealthcare.org.uk/educating-sustainable-healthcare-expanded-learning-outcomes .
- Centre for Sustainable Healthcare. 2019 . Resource library. Sustainable healthcare education; [accessed 2019 Jan 25]. https://networks.sustainablehealthcare.org.uk/resources?f%5B0%5D=og_group_ref%3A4074 .
- Crisp N . 2017 . What would a sustainable health and care system look like? BMJ . 358 : j3895 .
- Fazey I . 2018 . Keynote session. Environmental Association for Universities and Colleges . Keele : Keele University .
- General Medical Council . 2015 . Outcomes for graduates (Tomorrow's Doctors) . London : GMC .
- General Medical Council . 2017 . Generic professional capabilities framework . London : GMC .
- General Medical Council . 2018 . Outcomes for graduates 2018 . London : GMC .
- Gibbs GR . 2008 . Thematic coding and categorizing . London : SAGE, Analysing qualitative data ; p. 38 – 55 .
- Gómez A , Balsari S , Nusbaum J , Heerboth A , Lemery J . 2013 . Perspective: environment, biodiversity, and the education of the physician of the future . Acad Med . 88 : 168 .
- Grant J . 2014 . Principles of curriculum design . In: Swanwick T , editor. Understanding medical education: evidence, theory and practice . 2nd ed. Chichester : John Wiley & Sons, Ltd ; p. 31 – 46 .
- Great Britain . 2008 . Climate Change Act 2008: Elizabeth II . London : The Stationery Office . Chapter 27.
- Great Britain . 2012 . Public Services (Social Value) Act 2012: Elizabeth II . London : The Stationery Office .
- Grose J , Doman M , Kelsey J , Richardson J , Woods M . 2015 . Integrating sustainability education into nursing using an interdisciplinary approach . Local Econ . 30 : 342 – 351 .
- Grose J , Richardson J . 2016 . Can a sustainability and health scenario provide a realistic challenge to student nurses and provoke changes in practice? An evaluation of a training intervention . Nurs Health Sci . 18 : 256 – 261 .
- Hazell B , Robson R . 2015 . Pharmaceutical waste reduction in the NHS: a best practice compilation paper . London : NHS Business Services Authority .
- Hensher M , Tisdell J , Zimitat C . 2017 . “Too much medicine”: insights and explanations from economic theory and research” . Soc Sci Med . 176 : 77 – 84 .
- International Federation of Medical Students Associations . 2016 . Training manual: climate and health . IFMSA .
- Kennedy TJT , Lingard LA . 2006 . Making sense of grounded theory in medical education . Med Educ . 40 : 101 – 108 .
- Madden DL , McLean M , Horton GL . 2018 . Preparing medical graduates for the health effects of climate change: an Australasian collaboration . Med J Aust . 208 : 291 – 292 .
- Maxwell J , Blashki G . 2016 . Teaching about climate change in medical education: an opportunity . J Public Health Res . 5 : 673 .
- Montgomery HE , Haines A , Marlow N , Pearson G , Mythen MG , Grocott MPW , Swanton C . 2017 . The future of UK healthcare: problems and potential solutions to a system in crisis . Ann Oncol . 28 : 1751 – 1755 .
- Mortimer F , Isherwood J , Wilkinson A , Vaux E . 2018 . Sustainability in quality improvement: redefining value . Fut Healthc J . 5 : 88 – 93 .
- Mortimer F . 2010 . The sustainable physician . Clin Med (Lond) . 10 : 110 .
- Naylor C , Appleby J . 2012 . Sustainable health and social care: connecting environmental and financial performance . London : The King’s Fund .
- Organisation for Economic Co-operation and Development . 2017 . Tackling wasteful spending on health . Paris : OECD Publishing .
- Pencheon D . 2017 . Sustainable Development Unit business plan 2017/18 . Cambridge : Sustainable Development Unit .
- Prideaux D . 2007 . Curriculum development in medical education: from acronyms to dynamism . Teach Teach Educ . 23 : 294 – 302 .
- Richardson J , Grose J , Doman M , Kelsey J . 2014 . The use of evidence-informed sustainability scenarios in the nursing curriculum: development and evaluation of teaching methods . Nurse Educ Today . 34 : 490 – 493 .
- Roberts I . 2009 . The health co-benefits of climate change policies: doctors have a responsibility to future generations . Clin Med . 9 : 212 – 213 .
- Royal College of General Practitioners . 2017 . RCGP position statement on quality in general practice . London : RCGP .
- Schroeder K , Thompson T , Frith K , Pencheon D . 2013 . Sustainable healthcare . Chichester : John Wiley & Sons, Ltd .
- Sustainable Development Unit . 2018 . Sustainable development in the health and care system – health check 2018 . Cambridge : Sustainable Development Unit .
- Teherani A , Nishimura H , Apatira L , Newman T , Ryan S . 2017 . Identification of core objectives for teaching sustainable healthcare education . Med Educ Online . 22 : 1386042 .
- Thomas PA , Kern DE , Hughes MT , Chen BY . 2016 . Curriculum development for medical education: a six-step approach . 3rd ed . Baltimore : Johns Hopkins University Press .
- Thompson T , Walpole S , Braithwaite I , Inman A , Barna S , Mortimer F . 2014 . Learning objectives for sustainable health care . Lancet . 384 : 1924 – 1925 .
- Tun MS . 2018 . Fulfilling a new obligation: teaching and learning about sustainable healthcare in the UK medical school curriculum [master’s thesis]. London: Imperial College London.
- Walpole SC , Mortimer F , Inman A , Braithwaite I , Thompson T . 2015 . Exploring emerging learning needs: a UK-wide consultation on environmental sustainability learning objectives for medical education . Int J Med Educ . 6 : 191 – 200 .
- Walpole SC , Mortimer F . 2017 . Evaluation of a collaborative project to develop sustainable healthcare education in eight UK medical schools . Public Health . 150 : 134 – 148 .
- Walpole SC , Pearson D , Coad J , Barna S . 2016 . What do tomorrow's doctors need to learn about ecosystems? A BEME systematic review: BEME Guide No. 36 . Med Teach . 38 : 338 – 352 .
- Walpole SC , Vyas A , Maxwell J , Canny BJ , Woollard R , Wellbery C , Leedham-Green K , Musaeus P , Tufail-Hanif U , Pavão Patrício K , et al. 2017 . Building an environmentally accountable medical curriculum through international collaboration . Med Teach . 39 : 1040 – 1050 .
- Wellbery C , Sheffield P , Timmireddy K , Sarfaty M , Teherani A , Fallar R . 2018 . It's time for medical schools to introduce climate change into their curricula . Acad Med . 93 : 1774 – 1777 .
- Wylie A , Leedham-Green K . 2017 . Health promotion in medical education: lessons from a major undergraduate curriculum implementation . Educ Prim Care . 28 : 325 – 333 .
- Xu K , Soucat A , Kutzin J , Brindley C , Dale E , Van de Maele N , Roubal T , Indikadahena C , Toure H , Cherilova V . 2018 . New perspectives on global health spending for universal health coverage . Geneva : World Health Organization .
